Vital Pulp Therapy in Permanent Teeth with Irreversible Pulpitis Caused by Caries: A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Design and Participants
2.3. Inclusion Criteria
- (1)
- Posterior teeth with deep caries exposing the pulp;
- (2)
- Posterior teeth with preoperative symptoms, such as referred pain, spontaneous pain or pain induced in thermal and cold sensitivity tests, which lasted from several seconds to even hours compared to the control teeth;
- (3)
- Posterior teeth with no prominent radiolucency at the periapical or furcation regions;
- (4)
- In order to ensure the independence of samples and the fitting of statistical models, one tooth was selected from each participant, with multiple teeth receiving VPT for analysis; the priority order was first premolar, second premolar, second molar and first molar.
2.4. Exclusion Criteria
- (1)
- Patients with general contraindications to dental treatment;
- (2)
- Teeth with completed RCT or VPT;
- (3)
- Teeth with external or internal resorption, prominent radiolucency at the periapical regions, or furcation;
- (4)
- Teeth with pulpitis caused by wedge-shaped defects, cracking, periodontitis or tooth fracture;
- (5)
- Teeth not responsive to vitality tests.
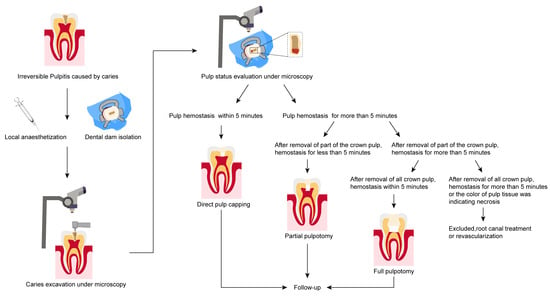
2.5. Interventions
2.6. Outcomes
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, J.S.; Jasani, B.; Patel, J.; Anthonappa, R.P.; King, N.M. Efficacy of Alternative Medicaments for Pulp Treatment in Primary Teeth in the Short Term: A Meta-analysis. J. Evid.-Based Dent. Pract. 2019, 19, 101309. [Google Scholar] [CrossRef]
- Silva, A.A.; Belladonna, F.G.; Rover, G.; Lopes, R.T.; Moreira, E.J.L.; De-Deus, G.; Silva, E. Does ultraconservative access affect the efficacy of root canal treatment and the fracture resistance of two-rooted maxillary premolars? Int. Endod. J. 2020, 53, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Dammaschke, T.; Leidinger, J.; Schäfer, E. Long-term evaluation of direct pulp capping--treatment outcomes over an average period of 6.1 years. Clin. Oral Investig. 2010, 14, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.M.; Ricucci, D.; Saoud, T.M.; Sigurdsson, A.; Kahler, B. Vital pulp therapy of mature permanent teeth with irreversible pulpitis from the perspective of pulp biology. Aust. Endod. J. 2020, 46, 154–166. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F., Jr.; Li, Y.; Tay, F.R. Vital pulp therapy: Histopathology and histobacteriology-based guidelines to treat teeth with deep caries and pulp exposure. J. Dent. 2019, 86, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Da Rosa, W.L.O.; Piva, E.; da Silva, A.F. Disclosing the physiology of pulp tissue for vital pulp therapy. Int. Endod. J. 2018, 51, 829–846. [Google Scholar] [CrossRef] [Green Version]
- Asgary, S.; Hassanizadeh, R.; Torabzadeh, H.; Eghbal, M.J. Treatment Outcomes of 4 Vital Pulp Therapies in Mature Molars. J. Endod. 2018, 44, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.M.; Pereira, J.F.; Marques, A.; Sequeira, D.B.; Friedman, S. Vital Pulp Therapy in Permanent Mature Posterior Teeth with Symptomatic Irreversible Pulpitis: A Systematic Review of Treatment Outcomes. Medicina 2021, 57, 573. [Google Scholar] [CrossRef]
- Li, Z.; Cao, L.; Fan, M.; Xu, Q. Direct Pulp Capping with Calcium Hydroxide or Mineral Trioxide Aggregate: A Meta-analysis. J. Endod. 2015, 41, 1412–1417. [Google Scholar] [CrossRef]
- Shi, S.; Bao, Z.F.; Liu, Y.; Zhang, D.D.; Chen, X.; Jiang, L.M.; Zhong, M. Comparison of in vivo dental pulp responses to capping with iRoot BP Plus and mineral trioxide aggregate. Int. Endod. J. 2016, 49, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Öncel Torun, Z.; Torun, D.; Demirkaya, K.; Yavuz, S.T.; Elçi, M.P.; Sarper, M.; Avcu, F. Effects of iRoot BP and white mineral trioxide aggregate on cell viability and the expression of genes associated with mineralization. Int. Endod. J. 2015, 48, 986–993. [Google Scholar] [CrossRef]
- Rao, Q.; Kuang, J.; Mao, C.; Dai, J.; Hu, L.; Lei, Z.; Song, G.; Yuan, G. Comparison of iRoot BP Plus and Calcium Hydroxide as Pulpotomy Materials in Permanent Incisors with Complicated Crown Fractures: A Retrospective Study. J. Endod. 2020, 46, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.G.; Law, A.S.; Holland, G.R.; Abbott, P.V.; Roda, R.S. Identify and define all diagnostic terms for pulpal health and disease states. J. Endod. 2009, 35, 1645–1657. [Google Scholar] [CrossRef]
- Tsze, D.S.; von Baeyer, C.L.; Pahalyants, V.; Dayan, P.S. Validity and Reliability of the Verbal Numerical Rating Scale for Children Aged 4 to 17 Years with Acute Pain. Ann. Emerg. Med. 2018, 71, 691–702.e3. [Google Scholar] [CrossRef]
- Linsuwanont, P.; Wimonsutthikul, K.; Pothimoke, U.; Santiwong, B. Treatment Outcomes of Mineral Trioxide Aggregate Pulpotomy in Vital Permanent Teeth with Carious Pulp Exposure: The Retrospective Study. J. Endod. 2017, 43, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Alqaderi, H.; Lee, C.T.; Borzangy, S.; Pagonis, T.C. Coronal pulpotomy for cariously exposed permanent posterior teeth with closed apices: A systematic review and meta-analysis. J. Dent. 2016, 44, 1–7. [Google Scholar] [CrossRef]
- Suhag, K.; Duhan, J.; Tewari, S.; Sangwan, P. Success of Direct Pulp Capping Using Mineral Trioxide Aggregate and Calcium Hydroxide in Mature Permanent Molars with Pulps Exposed during Carious Tissue Removal: 1-year Follow-up. J. Endod. 2019, 45, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Uesrichai, N.; Nirunsittirat, A.; Chuveera, P.; Srisuwan, T.; Sastraruji, T.; Chompu-Inwai, P. Partial pulpotomy with two bioactive cements in permanent teeth of 6- to 18-year-old patients with signs and symptoms indicative of irreversible pulpitis: A noninferiority randomized controlled trial. Int. Endod. J. 2019, 52, 749–759. [Google Scholar] [CrossRef]
- Asgary, S.; Eghbal, M.J.; Bagheban, A.A. Long-term outcomes of pulpotomy in permanent teeth with irreversible pulpitis: A multi-center randomized controlled trial. Am. J. Dent. 2017, 30, 151–155. [Google Scholar] [PubMed]
- Cushley, S.; Duncan, H.F.; Lappin, M.J.; Tomson, P.L.; Lundy, F.T.; Cooper, P.; Clarke, M.; El Karim, I.A. Pulpotomy for mature carious teeth with symptoms of irreversible pulpitis: A systematic review. J. Dent. 2019, 88, 103158. [Google Scholar] [CrossRef]
- Witherspoon, D.E.; Small, J.C.; Harris, G.Z. Mineral trioxide aggregate pulpotomies: A case series outcomes assessment. J. Am. Dent. Assoc. 2006, 137, 610–618. [Google Scholar] [CrossRef] [Green Version]
- Qudeimat, M.A.; Alyahya, A.; Hasan, A.A. Mineral trioxide aggregate pulpotomy for permanent molars with clinical signs indicative of irreversible pulpitis: A preliminary study. Int. Endod. J. 2017, 50, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Taha, N.A.; Abdulkhader, S.Z. Full Pulpotomy with Biodentine in Symptomatic Young Permanent Teeth with Carious Exposure. J. Endod. 2018, 44, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Taha, N.A.; Al-Khatib, H. Four years follow up of full pulpotomy in symptomatic mature permanent teeth with carious pulp exposure using a stain-proof calcium silicate based material. J. Endod. 2021, 21, S0099-2399. [Google Scholar] [CrossRef]
- Santos, J.M.; Marques, J.A.; Diogo, P.; Messias, A.; Sousa, V.; Sequeira, D.; Palma, P.J. Influence of Preoperative Pulp Inflammation in the Outcome of Full Pulpotomy Using a Dog Model. J. Endod. 2021, 47, 1417–1426. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K. Changes in the pulpal vasculature during inflammation. J. Endod. 1990, 16, 92–97. [Google Scholar] [CrossRef]
- Liu, S.Y.; Gong, W.Y.; Liu, M.Q.; Long, Y.Z.; Dong, Y.M. Clinical efficacy observation of direct pulp capping using iRoot BP Plus therapy in mature permanent teeth with carious pulp exposure. Chin. J. Stomatol. 2020, 55, 945–951. [Google Scholar] [CrossRef]
- Ricucci, D.; Loghin, S.; Siqueira, J.F., Jr. Correlation between clinical and histologic pulp diagnoses. J. Endod. 2014, 40, 1932–1939. [Google Scholar] [CrossRef]
- Rossi, H.L.; See, L.P.; Foster, W.; Pitake, S.; Gibbs, J.; Schmidt, B.; Mitchell, C.H.; Abdus-Saboor, I. Evoked and spontaneous pain assessment during tooth pulp injury. Sci. Rep. 2020, 10, 2759. [Google Scholar] [CrossRef] [Green Version]
- Kundzina, R.; Stangvaltaite, L.; Eriksen, H.M.; Kerosuo, E. Capping carious exposures in adults: A randomized controlled trial investigating mineral trioxide aggregate versus calcium hydroxide. Int. Endod. J. 2017, 50, 924–932. [Google Scholar] [CrossRef]
- Pigg, M.; Nixdorf, D.R.; Nguyen, R.H.; Law, A.S. Validity of Preoperative Clinical Findings to Identify Dental Pulp Status: A National Dental Practice-Based Research Network Study. J. Endod. 2016, 42, 935–942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taha, N.A.; About, I.; Sedgley, C.M.; Messer, H.H. Conservative Management of Mature Permanent Teeth with Carious Pulp Exposure. J. Endod. 2020, 46, S33–S41. [Google Scholar] [CrossRef]
- Alghaithy, R.A.; Qualtrough, A.J. Pulp sensibility and vitality tests for diagnosing pulpal health in permanent teeth: A critical review. Int. Endod. J. 2017, 50, 135–142. [Google Scholar] [CrossRef] [Green Version]
- Stashenko, P.; Teles, R.; D’Souza, R. Periapical inflammatory responses and their modulation. Crit. Rev. Oral Biol. Med. 1998, 9, 498–521. [Google Scholar] [CrossRef]
- Pak, J.G.; White, S.N. Pain prevalence and severity before, during, and after root canal treatment: A systematic review. J. Endod. 2011, 37, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Khayat, B.G.; Byers, M.R.; Taylor, P.E.; Mecifi, K.; Kimberly, C.L. Responses of nerve fibers to pulpal inflammation and periapical lesions in rat molars demonstrated by calcitonin gene-related peptide immunocytochemistry. J. Endod. 1988, 14, 577–587. [Google Scholar] [CrossRef]
- Camilleri, J.; Montesin, F.E.; Papaioannou, S.; McDonald, F.; Pitt Ford, T.R. Biocompatibility of two commercial forms of mineral trioxide aggregate. Int. Endod. J. 2004, 37, 699–704. [Google Scholar] [CrossRef]
- Emara, R.; Elhennawy, K.; Schwendicke, F. Effects of calcium silicate cements on dental pulp cells: A systematic review. J. Dent. 2018, 77, 18–36. [Google Scholar] [CrossRef]


| Variable Name | Variable Description | Assignment | Variable Name | Variable Description | Assignment |
|---|---|---|---|---|---|
| Sex | Male Female | 1 2 | Age | [5,10] [10,15] [15,16] | 1 2 3 |
| Root maturation | Open Closed | 0 1 | Cave shape | Occlusal Surface Only Proximal Surface Involved | 1 2 |
| Spontaneous pain | No Yes | 0 1 | Nocturnal pain | No Yes | 0 1 |
| Referred pain | No Yes | 0 1 | Cold test | Tenderness without delaying pain Tenderness with delaying pain <30 s Tenderness with delaying pain ≥30 s | 0 1 2 |
| Pain level of cold test | <5 ≥5 | 0 1 | Heat test | Tenderness without delaying pain Tenderness with delaying pain <30 s Tenderness with delaying pain ≥30 s Normal | 0 1 2 3 |
| Pain level of heat test | <5 ≥5 | 0 1 | Electrical vitality test difference | <10 ≥10 | 0 1 |
| Percussion sensitivity | (−) (+) | 0 1 | VPT type | Partial pulpotomy Full pulpotomy Direct pulp capping | 1 2 3 |
| Influencing Factors | B | S.E. | Waild | Sig. | Exp (B) |
|---|---|---|---|---|---|
| Sex (1) | 1.172 | 2.186 | 0.288 | 0.592 | 3.228 |
| Age | −4.084 | 2.919 | 1.958 | 0.162 | 0.017 |
| Root maturation (1) | 5.588 | 4.915 | 1.293 | 0.256 | 3.326 |
| Cave shape (1) | −0.536 | 2.325 | 0.053 | 0.818 | 0.585 |
| Spontaneous pain (1) | −4.958 | 1.956 | 0.000 | 0.999 | 0.000 |
| Nocturnal pain (1) | −2.260 | 1.837 | 1.515 | 0.218 | 0.104 |
| Referred pain (1) | −0.891 | 2.515 | 0.125 | 0.723 | 0.410 |
| Cold test | 2.134 | 2.972 | 0.516 | 0.473 | 3.446 |
| Pain level of cold test | 2.020 | 2.253 | 0.804 | 0.370 | 3.540 |
| Heat test | 0.411 | 0.659 | 0.389 | 0.533 | 1.508 |
| Pain level of heat test | 9.817 | 1.036 | 0.000 | 0.999 | 4.826 |
| Electrical vitality test difference | 3.205 | 1.886 | 0.000 | 0.998 | 1.121 |
| Percussion sensitivity (1) | −6.208 | 1.714 | 2.794 | 0.095 | 0.002 |
| VPT type | 1.980 | 0.372 | |||
| VPT type (1) | −2.097 | 2.793 | 0.564 | 0.453 | 0.123 |
| VPT type (2) | 0.797 | 2.382 | 0.112 | 0.738 | 2.219 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guan, X.; Zhou, Y.; Yang, Q.; Zhu, T.; Chen, X.; Deng, S.; Zhang, D. Vital Pulp Therapy in Permanent Teeth with Irreversible Pulpitis Caused by Caries: A Prospective Cohort Study. J. Pers. Med. 2021, 11, 1125. https://doi.org/10.3390/jpm11111125
Guan X, Zhou Y, Yang Q, Zhu T, Chen X, Deng S, Zhang D. Vital Pulp Therapy in Permanent Teeth with Irreversible Pulpitis Caused by Caries: A Prospective Cohort Study. Journal of Personalized Medicine. 2021; 11(11):1125. https://doi.org/10.3390/jpm11111125
Chicago/Turabian StyleGuan, Xiaoxu, Yi Zhou, Qingxia Yang, Tianer Zhu, Xuepeng Chen, Shuli Deng, and Denghui Zhang. 2021. "Vital Pulp Therapy in Permanent Teeth with Irreversible Pulpitis Caused by Caries: A Prospective Cohort Study" Journal of Personalized Medicine 11, no. 11: 1125. https://doi.org/10.3390/jpm11111125
APA StyleGuan, X., Zhou, Y., Yang, Q., Zhu, T., Chen, X., Deng, S., & Zhang, D. (2021). Vital Pulp Therapy in Permanent Teeth with Irreversible Pulpitis Caused by Caries: A Prospective Cohort Study. Journal of Personalized Medicine, 11(11), 1125. https://doi.org/10.3390/jpm11111125