Individualized 3D-Printed Bone-Anchored Maxillary Protraction Device for Growth Modification in Skeletal Class III Malocclusion
Abstract
:1. Introduction
2. Methods
2.1. Study Sample
2.2. Data Acquisition
2.3. Preoperative Simulation
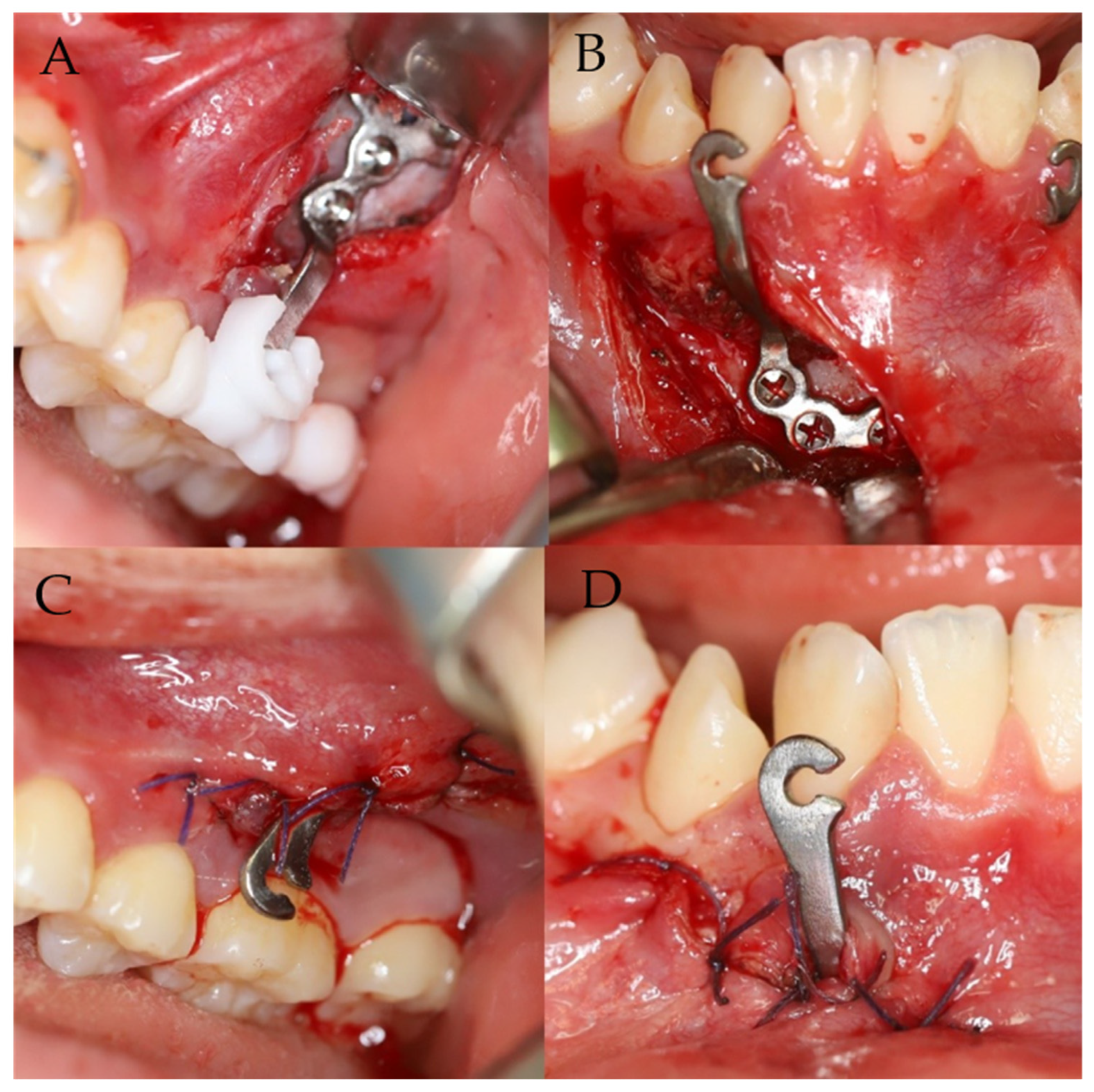
2.4. Surgical Procedure
2.5. Cephalometric and Superimposition Analysis
3. Results
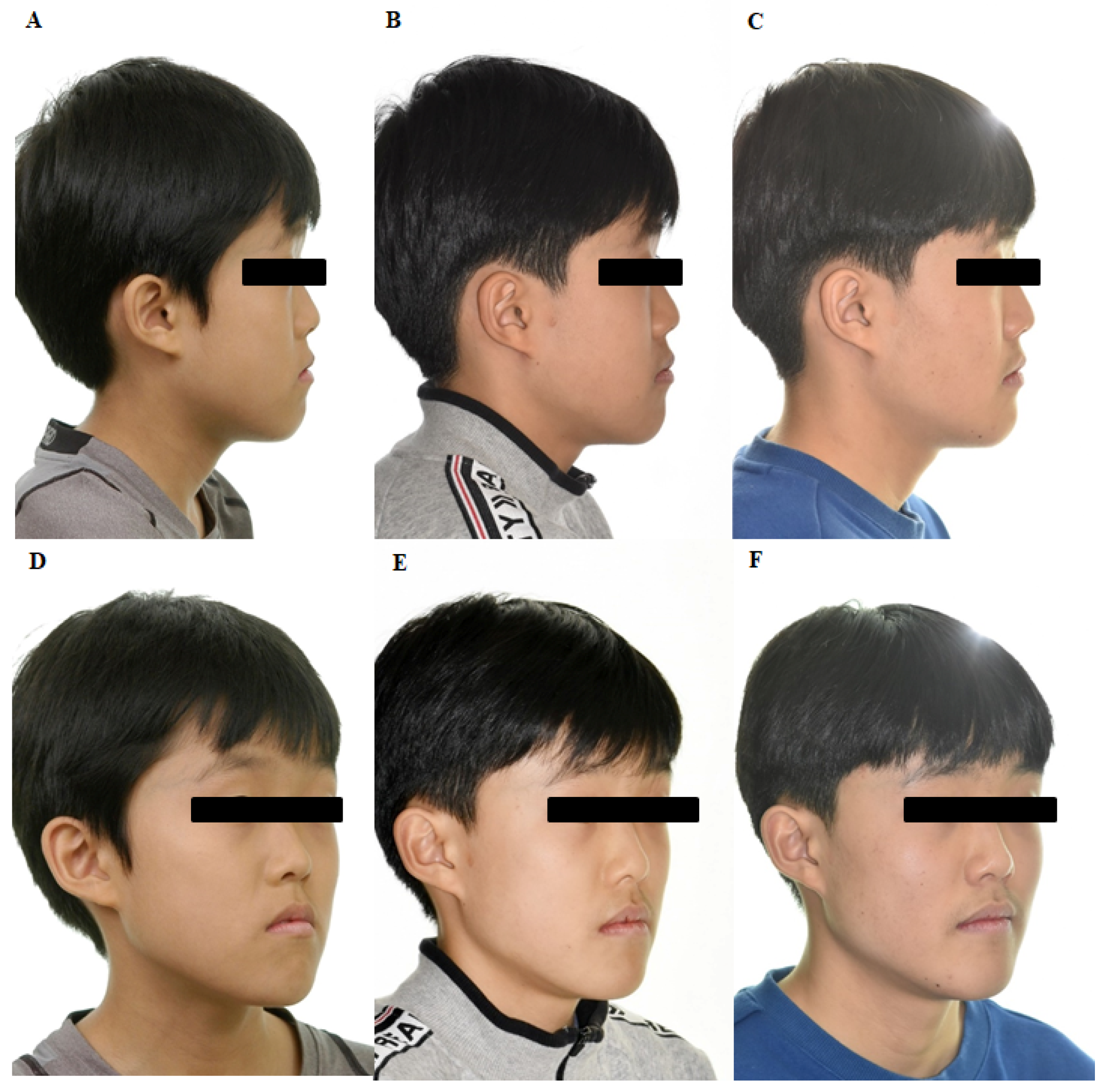
4. Case Presentation
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Proffit, W.R.; Fields, H.W., Jr.; Sarver, D.M. Contemporary Orthodontics; Elsevier Health Sciences: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Litton, S.F.; Ackermann, L.V.; Isaacson, R.J.; Shapiro, B.L. A genetic study of Class 3 malocclusion. Am. J. Orthod. 1970, 58, 565–577. [Google Scholar] [CrossRef]
- Borzabadi-Farahani, A.; Borzabadi-Farahani, A.; Eslamipour, F. Malocclusion and occlusal traits in an urban Iranian population. An epidemiological study of 11- to 14-year-old children. Eur. J. Orthod. 2009, 31, 477–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eslamian, L.; Borzabadi-Farahani, A.; Badiee, M.R.; Le, B.T. An Objective Assessment of Orthognathic Surgery Patients. J. Craniofac. Surg. 2019, 30, 2479–2482. [Google Scholar] [CrossRef]
- White, L. Early orthodontic intervention. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 24–28. [Google Scholar] [CrossRef]
- Zhang, H.; Deng, F.; Wang, H.; Huang, Q.; Zhang, Y. Early orthodontic intervention followed by fixed appliance therapy in a patient with a severe Class III malocclusion and cleft lip and palate. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Azamian, Z.; Shirban, F. Treatment Options for Class III Malocclusion in Growing Patients with Emphasis on Maxillary Protraction. Sci. Cairo 2016, 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugawara, J.; Baik, U.B.; Umemori, M.; Takahashi, I.; Nagasaka, H.; Kawamura, H.; Mitani, H. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int. J. Adult Orthodon. Orthognath. Surg. 2002, 17, 243–253. [Google Scholar] [PubMed]
- De Clerck, H.; Cevidanes, L.; Baccetti, T. Dentofacial effects of bone-anchored maxillary protraction: A controlled study of consecutively treated Class III patients. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 577–581. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez de Guzmán-Barrera, J.; Sáez Martínez, C.; Boronat-Catalá, M.; Montiel-Company, J.M.; Paredes-Gallardo, V.; Gandía-Franco, J.L.; Almerich-Silla, J.M.; Bellot-Arcís, C. Effectiveness of interceptive treatment of class III malocclusions with skeletal anchorage: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0173875. [Google Scholar] [CrossRef] [PubMed]
- Cevidanes, L.; Baccetti, T.; Franchi, L.; McNamara, J.A., Jr.; De Clerck, H. Comparison of two protocols for maxillary protraction: Bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010, 80, 799–806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cornelis, M.A.; Scheffler, N.R.; Mahy, P.; Siciliano, S.; De Clerck, H.J.; Tulloch, J.F. Modified miniplates for temporary skeletal anchorage in orthodontics: Placement and removal surgeries. J. Oral Maxillofac. Surg. 2008, 66, 1439–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.H.; Viana, M.A.; Graber, T.M.; Omerza, F.F.; BeGole, E.A. The effectiveness of protraction face mask therapy: A meta-analysis. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 675–685. [Google Scholar] [CrossRef]
- Sergl, H.G.; Klages, U.; Zentner, A. Functional and social discomfort during orthodontic treatment—Effects on compliance and prediction of patients’ adaptation by personality variables. Eur. J. Orthod. 2000, 22, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; Takano-Yamamoto, T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 373–378. [Google Scholar] [CrossRef]
- Cheng, S.J.; Tseng, I.Y.; Lee, J.J.; Kok, S.H. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int. J. Oral Maxillofac. Implant. 2004, 19, 100–106. [Google Scholar]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque-induced gingival conditions. J. Clin. Periodontol. 2018, 45, S17–S27. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Choi, Y.S.; Hwang, E.H.; Chung, K.R.; Kook, Y.A.; Nelson, G. Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S82–S89. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.J.; Kim, G.T.; Choi, Y.S.; Hwang, E.H.; Paek, J.; Kim, S.H.; Huang, J.C. Accuracy of a cone beam computed tomography-guided surgical stent for orthodontic mini-implant placement. Angle Orthod. 2012, 82, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, H.H.; Borzabadi-Farahani, A.; Fotovat, M.; Kim, S.H. Vestibular Incision Subperiosteal Tunnel Access (VISTA) for Surgically Facilitated Orthodontic Therapy (SFOT). Contemp. Clin. Dent. 2019, 10, 548. [Google Scholar] [PubMed]


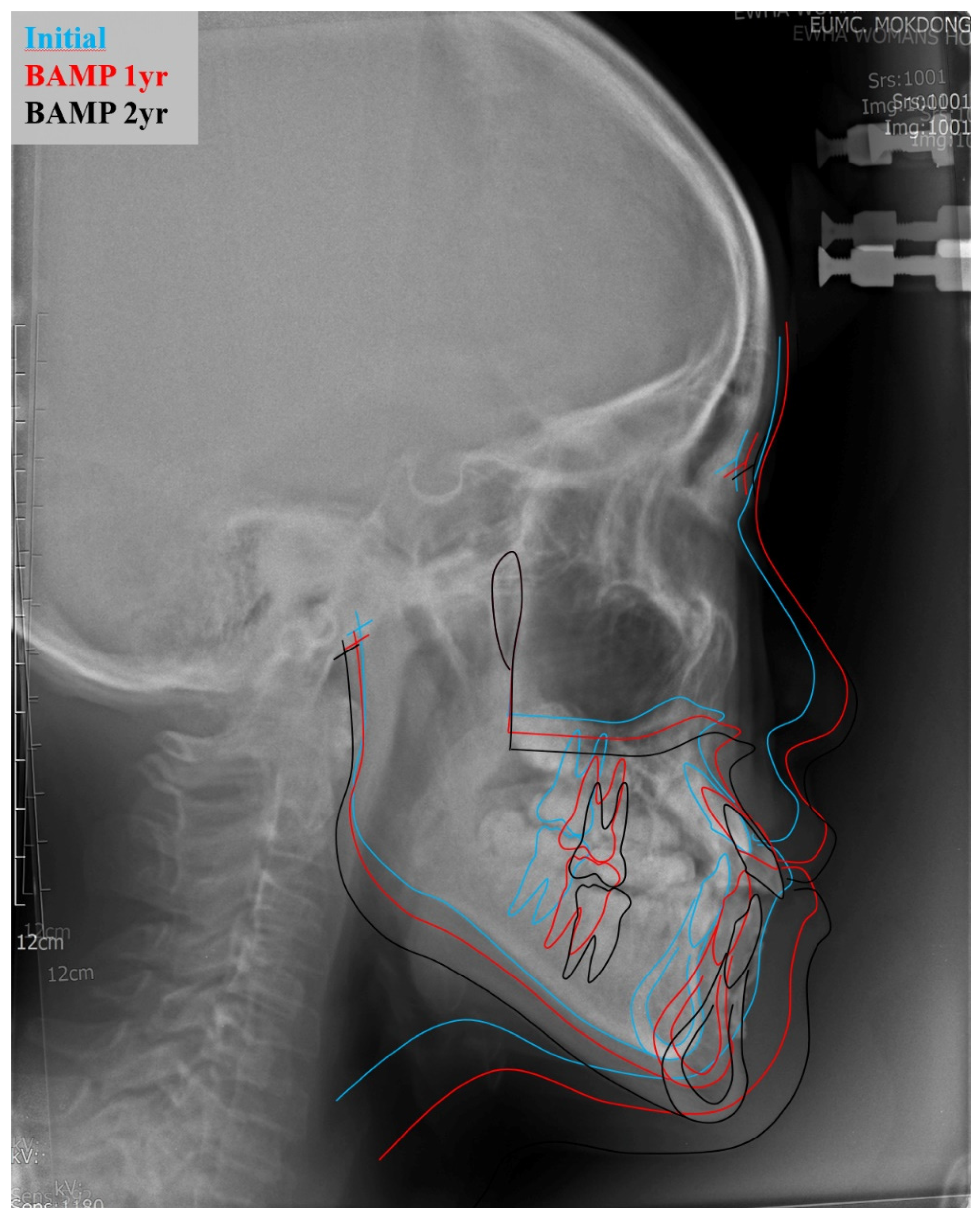
| Measurement | Reference Value | Preoperative | Postoperative 24 Months |
|---|---|---|---|
| Maxillo-mandibular measurement | |||
| SNA | 81.6 (3.1) | 77.98 | 84.63 |
| SNB | 79.1 (3.0) | 82.54 | 85.72 |
| ANB difference | 2.4 (1.8) | −4.56 | −1.09 |
| Wits appraisal | −2.7 (2.4) | −7.52 | −3.26 |
| Angular measurement | |||
| FMA | 29.63 (5.66) | 30.34 | 28.98 |
| SN-GoMe | 36 (4) | 37.1 | 32.72 |
| A point—N Perpend | 0.4 (2.3) | −5.37 | −1.86 |
| Facial height measurement | |||
| Facial Height Ratio | 65 (9) | 61.7 | 66.37 |
| Posterior Facial Height | 85 (5.5) | 76.84 | 90.76 |
| Anterior Facial Height | 127.4 (5.6) | 124.52 | 136.74 |
| Dentoalveolar measurement | |||
| U1 to SN | 107 (6) | 123.45 | 120.62 |
| IMPA | 95.9 (6.3) | 78.2 | 78.3 |
| Interincisal angle | 124 (8.3) | 121.2 | 128.32 |
| Soft tissue measurement | |||
| Upper Lip E-plane | 0.1 (2) | 0.44 | −1.58 |
| Lower Lip E-plane | 0.1 (2) | 2.69 | 0.26 |
| Nasolabial angle | 84.9 (5) | 93.86 | 101.9 |
| Linear Deviation | ||||
|---|---|---|---|---|
| x-Axis (Lateral/Medial) | y-Axis (Anterior/Posterior) | z-Axis (Cranial/Caudal) | Distance Difference | |
| N | 20 | 20 | 20 | 20 |
| Median | −0.0154 | −0.0946 | 0.0579 | 0.1081 |
| Range | −0.1729–0.2448 | −1.1643–1.5076 | −0.9189–0.7126 | 0.0211–1.3772 |
| SD | 0.1463 | 0.9012 | 0.5515 | 0.5074 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Li, J.; Kim, S.; Kim, W.; Kim, S.-H.; Lee, S.-M.; Park, Y.L.; Yang, S.; Kim, J.-W. Individualized 3D-Printed Bone-Anchored Maxillary Protraction Device for Growth Modification in Skeletal Class III Malocclusion. J. Pers. Med. 2021, 11, 1087. https://doi.org/10.3390/jpm11111087
Kim M, Li J, Kim S, Kim W, Kim S-H, Lee S-M, Park YL, Yang S, Kim J-W. Individualized 3D-Printed Bone-Anchored Maxillary Protraction Device for Growth Modification in Skeletal Class III Malocclusion. Journal of Personalized Medicine. 2021; 11(11):1087. https://doi.org/10.3390/jpm11111087
Chicago/Turabian StyleKim, Minji, Jingwen Li, Sehyang Kim, Wonho Kim, Sun-Hyun Kim, Sung-Min Lee, Young Long Park, Sook Yang, and Jin-Woo Kim. 2021. "Individualized 3D-Printed Bone-Anchored Maxillary Protraction Device for Growth Modification in Skeletal Class III Malocclusion" Journal of Personalized Medicine 11, no. 11: 1087. https://doi.org/10.3390/jpm11111087
APA StyleKim, M., Li, J., Kim, S., Kim, W., Kim, S.-H., Lee, S.-M., Park, Y. L., Yang, S., & Kim, J.-W. (2021). Individualized 3D-Printed Bone-Anchored Maxillary Protraction Device for Growth Modification in Skeletal Class III Malocclusion. Journal of Personalized Medicine, 11(11), 1087. https://doi.org/10.3390/jpm11111087







