A Comparative Analysis of the Piezoelectric Ultrasonic Appliance and Trephine Bur for Apical Location: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
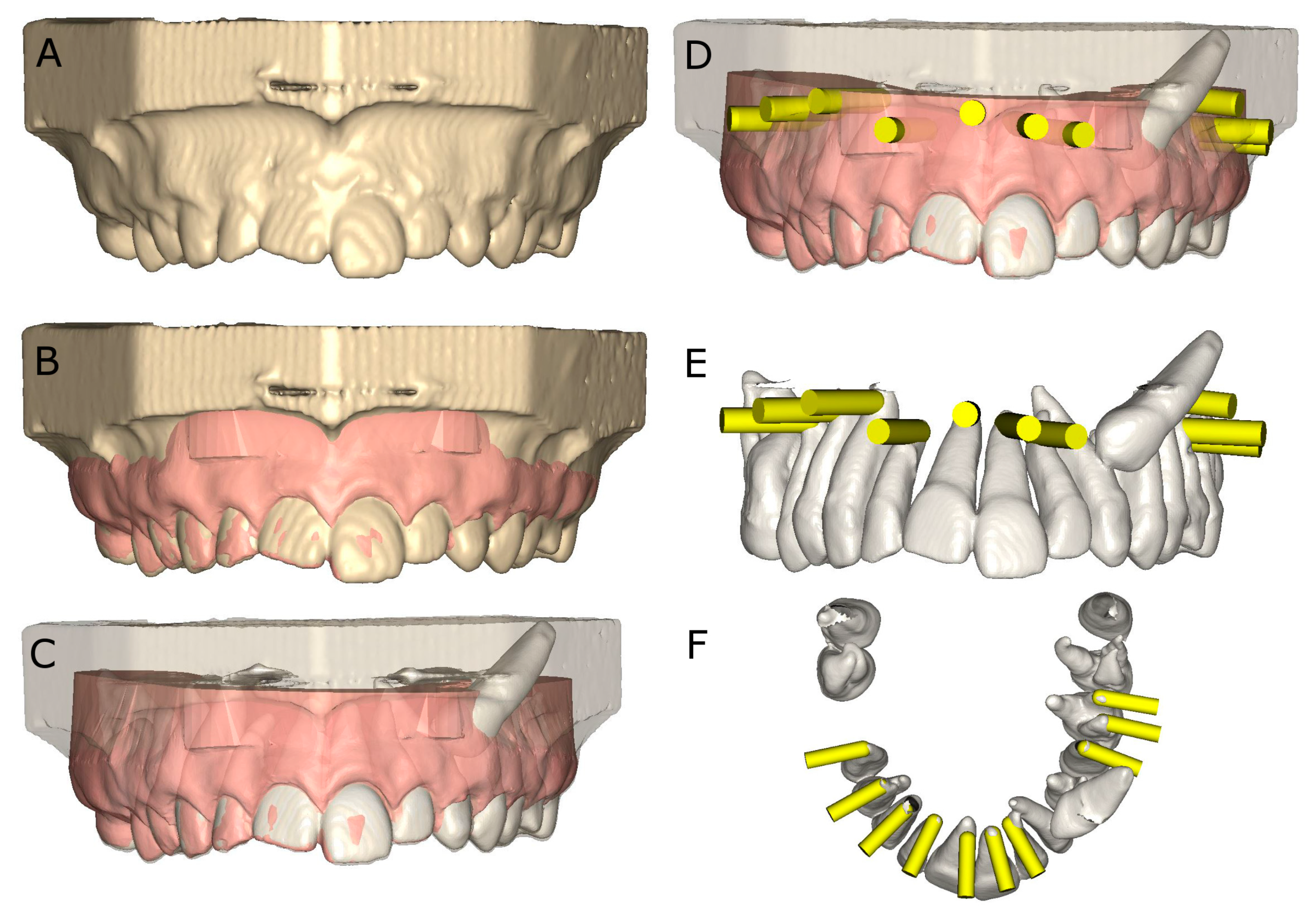
2.1. Study Design
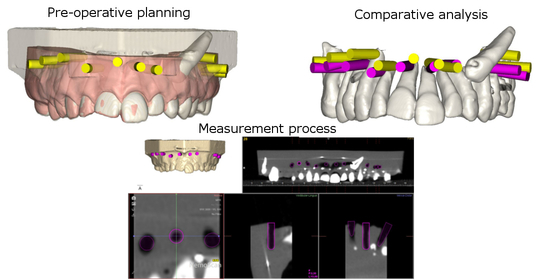
2.2. Experimental Procedure
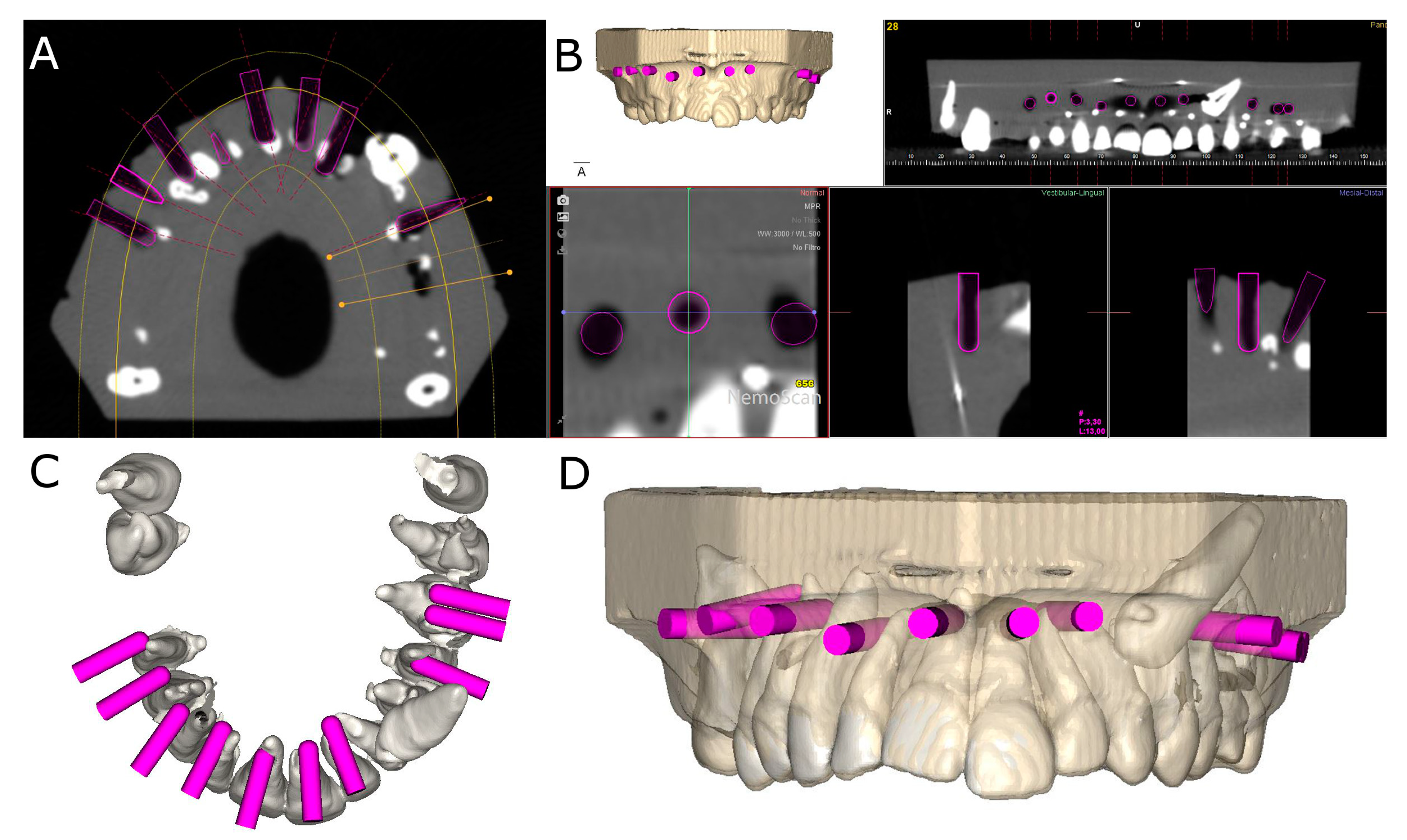
2.3. Measurement Procedure
2.4. Statistical Tests
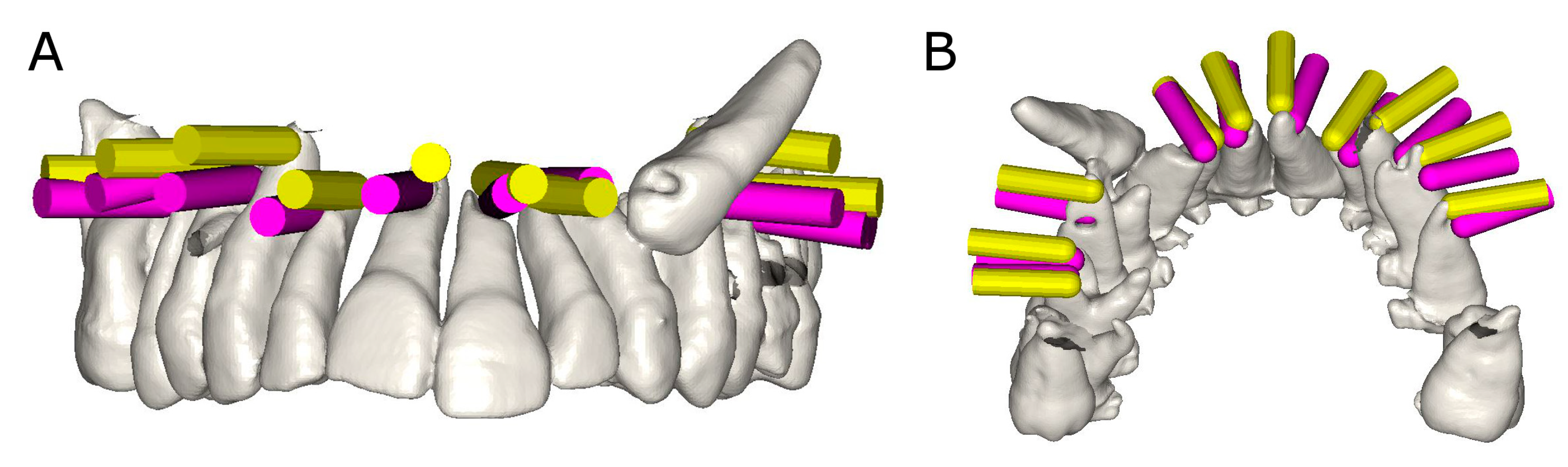
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Setzer, F.C.; Kohli, M.R.; Shah, S.B.; Karabucak, B.; Kim, S. Outcome of endodontic surgery: A meta-analysis of the literature-Part 2: Comparison of endodontic microsurgical techniques with and without the use of higher magnification. J. Endod. 2012, 38, 1–10. [Google Scholar] [CrossRef]
- Kohli, M.R.; Berenji, H.; Setzer, F.C.; Lee, S.M.; Karabucak, B. Outcome of Endodontic Surgery: A Meta-analysis of the Literature—Part 3: Comparison of Endodontic Microsurgical Techniques with 2 Different Root-end Filling Materials. J. Endod. 2018, 44, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Karabucak, B.; Bunes, A.; Chehoud, C.; Kohli, M.R.; Setzer, F. Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: A cone-beam computed tomography study. J. Endod. 2016, 42, 538–541. [Google Scholar] [CrossRef] [PubMed]
- Molven, O.; Halse, A.; Grung, B. Incomplete healing (scar tissue) after periapical surgery-Radiographic findings 8 to 12 years after treatment. J. Endod. 1996, 22, 264–268. [Google Scholar] [CrossRef]
- de Chevigny, C.; Dao, T.T.; Basrani, B.R.; Marquis, V.; Farzaneh, M.; Abitbol, S.; Friedman, S. Treatment outcome in endodontics: The Toronto study-phase 4: Initial treatment. J. Endod. 2008, 34, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.; Jung, H.I.; Song, M.; Kim, S.Y.; Kim, H.-C.; Kim, E. Outcome of nonsurgical retreatment and endodontic microsurgery: A meta-analysis. Clin. Oral Investig. 2015, 19, 569–582. [Google Scholar] [CrossRef]
- Sreedevi, P.; Varghese, N.; Varugheese, J.M. Prognosis of periapical surgery using bonegrafts: A clinical study. J. Conserv. Dent. 2011, 14, 68–72. [Google Scholar] [CrossRef]
- Chong, B.S.; Rhodes, J.S. Endodontic surgery. Br. Dent. J. 2014, 216, 281–290. [Google Scholar] [CrossRef] [PubMed]
- von Arx, T. Apical surgery: A review of current techniques and outcome. Saudi Dent. J. 2011, 23, 9–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strbac, G.D.; Schnappauf, A.; Giannis, K.; Bertl, M.H.; Moritz, A.; Ulm, C. Guided Autotransplantation of Teeth: A Novel Method Using Virtually Planned 3-dimensional Templates. J. Endod. 2016, 42, 1844–1850. [Google Scholar] [CrossRef]
- Abate, A.; Cavagnetto, D.; Rusconi, F.M.E.; Cressoni, P.; Esposito, L. Safety and Effects of the Rapid Maxillary Expander on Temporomandibular Joint in Subjects Affected by Juvenile Idiopathic Arthritis: A Retrospective Study. Children 2021, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kratchman, S. Modern Endodontic Surgery Concepts and Practice: A Review. J. Endod. 2006, 32, 601–623. [Google Scholar] [CrossRef]
- Sutter, E.; Lotz, M.; Rechenberg, D.-K.; Stadlinger, B.; Rücker, M.; Valdec, S. Guided apicoectomy using a CAD/CAM drilling template. Int. J. Comput. Dent. 2019, 22, 363–369. [Google Scholar] [PubMed]
- Antal, M.; Nagy, E.; Sanyó, L.; Braunitzer, G. Digitally planned root end surgery with static guide and custom trephine burs: A case report. Int. J. Med. Robot. Comput. Assist. Surg. 2020, 16, e2115. [Google Scholar] [CrossRef] [PubMed]
- Eszter, N.; Mark, F.; Mark, A. Guided modern endodontic microsurgery by use of a trephine bur. Orv. Hetil. 2020, 161, 1260–1265. [Google Scholar]
- Giacomino, C.M.; Ray, J.J.; Wealleans, J.A. Targeted Endodontic Microsurgery: A Novel Approach to Anatomically Challenging Scenarios Using 3-dimensional–printed Guides and Trephine Burs—A Report of 3 Cases. J. Endod. 2018, 44, 671–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zubizarreta-Macho, Á.; Muñoz, A.P.; Deglow, E.R.; Agustín-Panadero, R.; Álvarez, J.M. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Procedure for Endodontic Access Cavities: An in Vitro Study. J. Clin. Med. 2020, 9, 129. [Google Scholar] [CrossRef] [Green Version]
- Nagendrababu, V.; Murray, P.E.; Ordinola-Zapata, R.; Peters, O.A.; Rôças, I.N.; Siqueira, J.F., Jr.; Priya, E.; Jayaraman, J.; Pulikkotil, S.J.; Camilleri, J.; et al. PRILE 2021 guidelines for reporting laboratory studies in Endodontology: A consensus-based development. Int. Endod. J. 2021, 54, 1482–1490. [Google Scholar] [CrossRef] [PubMed]
- Nagendrababu, V.; Murray, P.E.; Ordinola-Zapata, R.; Peters, O.A.; Rôças, I.N.; Siqueira, J.F., Jr.; Priya, E.; Jayaraman, J.; Pulikkotil, S.J.; Suresh, N.; et al. PRILE 2021 guidelines for reporting laboratory studies in Endodontology: Explanation and elaboration. Int. Endod. J. 2021, 54, 1491–1515. [Google Scholar] [CrossRef]
- Van Assche, N.; Vercruyssen, M.; Coucke, W.; Teughels, W.; Jacobs, R.; Quirynen, M. Accuracy of computer-aided implant placement. Clin. Oral Implant. Res. 2012, 23, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Sicilia, A.; Botticelli, D. Computer-guided implant therapy and soft- and hard-tissue aspects. The Third EAOConsensus Conference 2012. Clin. Oral Implant. Res. 2012, 23, 157–161. [Google Scholar]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402.e6. [Google Scholar] [CrossRef] [PubMed]
- Zubizarreta-Macho, Á.; Castillo-Amature, C.; Montiel-Company, J.M.; Mena-Álvarez, J. Efficacy of Computer-Aided Static Navigation Technique on the Accuracy of Endodontic Microsurgery. A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 313. [Google Scholar] [CrossRef] [PubMed]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assited implant surgery in single tooth space: A randomized controlled trial. Clin. Oral. Implant. Res. 2019, 30, 505–514. [Google Scholar]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implant. 2019, 34, 205–213. [Google Scholar] [CrossRef]
- Guzmán, A.M.; Deglow, E.R.; Zubizarreta-Macho, Á.; Agustín-Panadero, R.; Montero, S.H. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Navigation for Dental Implants Placement: An In Vitro Study. J. Clin. Med. 2019, 8, 2123. [Google Scholar] [CrossRef] [Green Version]
- Block, M.; Emery, R.; Lank, K.; Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral Maxillofac. Implant. 2017, 32, 92–99. [Google Scholar] [CrossRef]
- Chong, B.S.; Dhesi, M.; Makdissi, J. Computer-aided dynamic navigation: A novel method for guided endodontics. Quintessence Int. 2019, 50, 196–202. [Google Scholar]
- Jain, S.D.; Carrico, C.K.; Bermanis, I. 3-Dimensional Accuracy of Dynamic Navigation Technology in Locating Calcified Canals. J. Endod. 2020, 46, 839–845. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Valle Castaño, S.; Montiel-Company, J.M.; Mena-Álvarez, J. Effect of Computer-Aided Navigation Techniques on the Accuracy of Endodontic Access Cavities: A Systematic Review and Meta-Analysis. Biology 2021, 10, 212. [Google Scholar] [CrossRef]

| n | Mean | SD | Minimum | Maximum | ||
|---|---|---|---|---|---|---|
| Coronal | TB | 69 | 1.99 a | 1.03 | 0.30 | 3.50 |
| PUI | 69 | 3.43 b | 1.21 | 1.70 | 5.10 | |
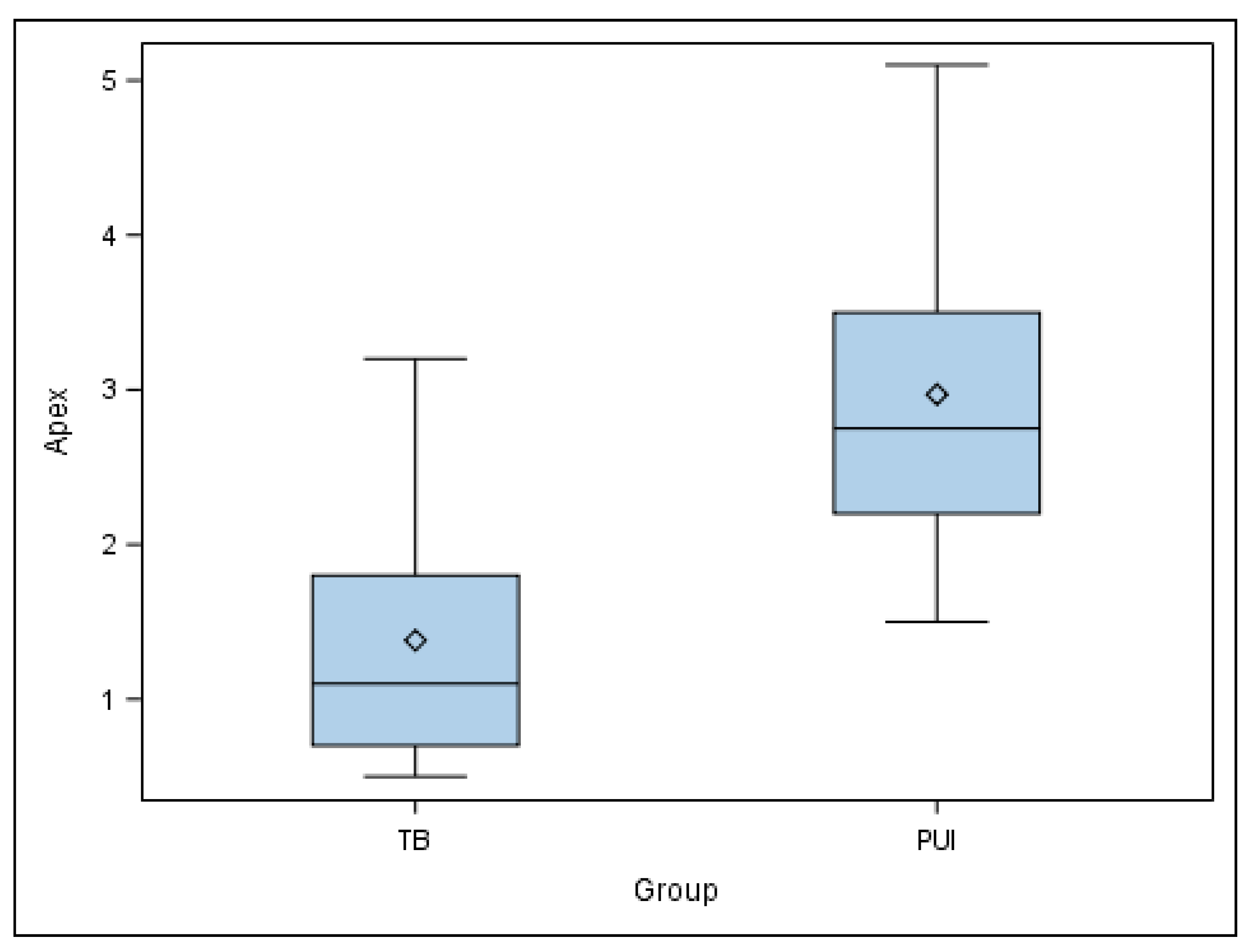
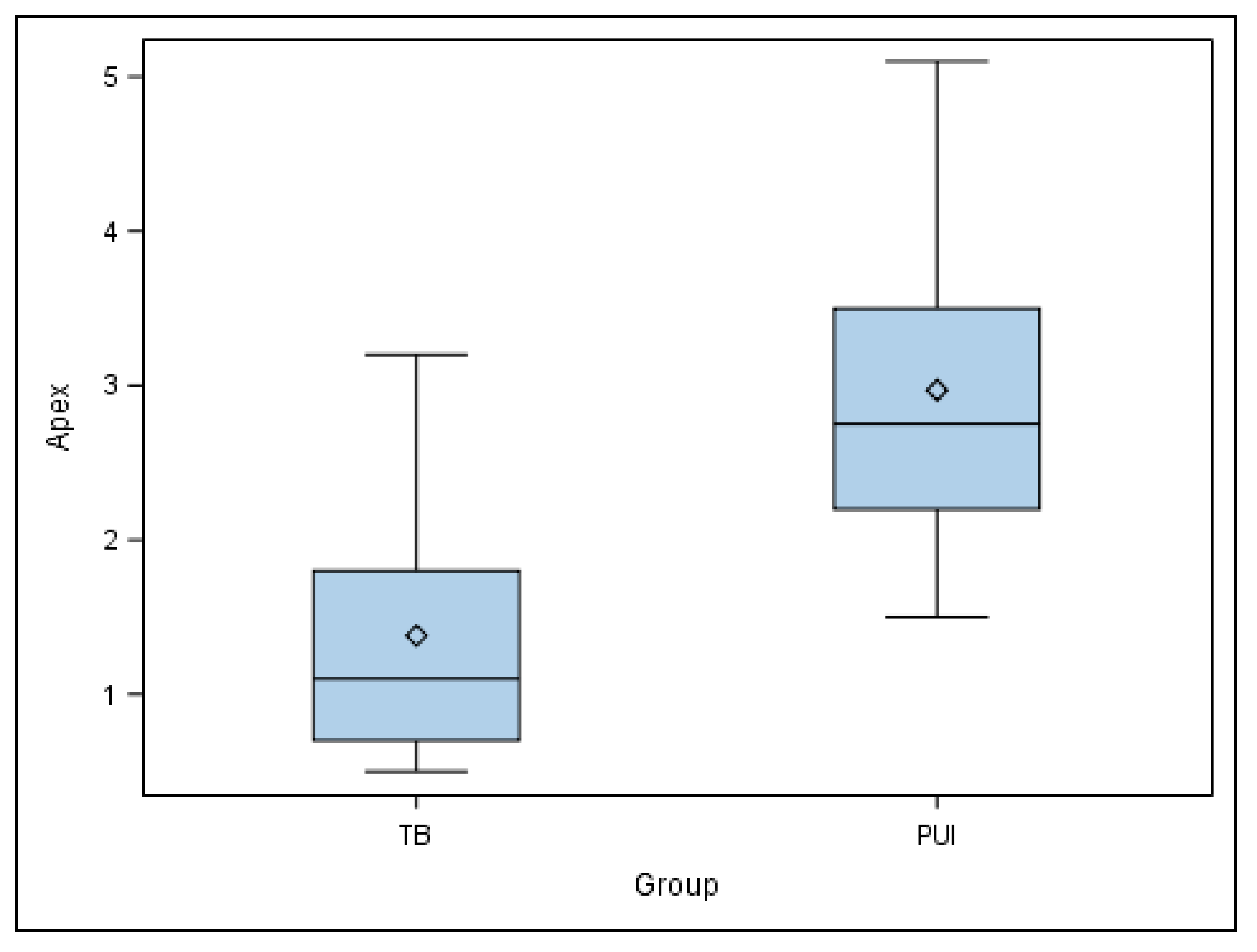
| Apical | TB | 69 | 1.38 a | 0.87 | 0.50 | 3.20 |
| PUI | 69 | 2.97 b | 1.26 | 1.50 | 5.10 | |
| Angular | TB | 69 | 10.96 a | 4.23 | 2.30 | 16.60 |
| PUI | 69 | 9.02 a | 4.07 | 2.80 | 15.50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cáceres Madroño, E.; Rodríguez Torres, P.; Oussama, S.; Zubizarreta-Macho, Á.; Bufalá Pérez, M.; Mena-Álvarez, J.; Riad Deglow, E.; Hernández Montero, S. A Comparative Analysis of the Piezoelectric Ultrasonic Appliance and Trephine Bur for Apical Location: An In Vitro Study. J. Pers. Med. 2021, 11, 1034. https://doi.org/10.3390/jpm11101034
Cáceres Madroño E, Rodríguez Torres P, Oussama S, Zubizarreta-Macho Á, Bufalá Pérez M, Mena-Álvarez J, Riad Deglow E, Hernández Montero S. A Comparative Analysis of the Piezoelectric Ultrasonic Appliance and Trephine Bur for Apical Location: An In Vitro Study. Journal of Personalized Medicine. 2021; 11(10):1034. https://doi.org/10.3390/jpm11101034
Chicago/Turabian StyleCáceres Madroño, Esther, Paulina Rodríguez Torres, Soraya Oussama, Álvaro Zubizarreta-Macho, María Bufalá Pérez, Jesús Mena-Álvarez, Elena Riad Deglow, and Sofía Hernández Montero. 2021. "A Comparative Analysis of the Piezoelectric Ultrasonic Appliance and Trephine Bur for Apical Location: An In Vitro Study" Journal of Personalized Medicine 11, no. 10: 1034. https://doi.org/10.3390/jpm11101034
APA StyleCáceres Madroño, E., Rodríguez Torres, P., Oussama, S., Zubizarreta-Macho, Á., Bufalá Pérez, M., Mena-Álvarez, J., Riad Deglow, E., & Hernández Montero, S. (2021). A Comparative Analysis of the Piezoelectric Ultrasonic Appliance and Trephine Bur for Apical Location: An In Vitro Study. Journal of Personalized Medicine, 11(10), 1034. https://doi.org/10.3390/jpm11101034