Withings Body Cardio Versus Gold Standards of Pulse-Wave Velocity and Body Composition
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Materials and Methods
2.2.1. Body Cardio Assessment
2.2.2. SphygmoCor Assessment
2.2.3. Bod Pod Assessment
3. Statistical Analyses
4. Results
4.1. Participants
4.2. Comparison of Body Cardio PWV Measurements with SphygmoCor Determinations
4.3. Comparison of Body Cardio HR Measurements with SphygmoCor Determinations
4.4. Comparison of Body Cardio BM Measurements with Bod Pod Determinations
4.5. Comparison of Body Cardio FM Measurements with Bod Pod Determinations
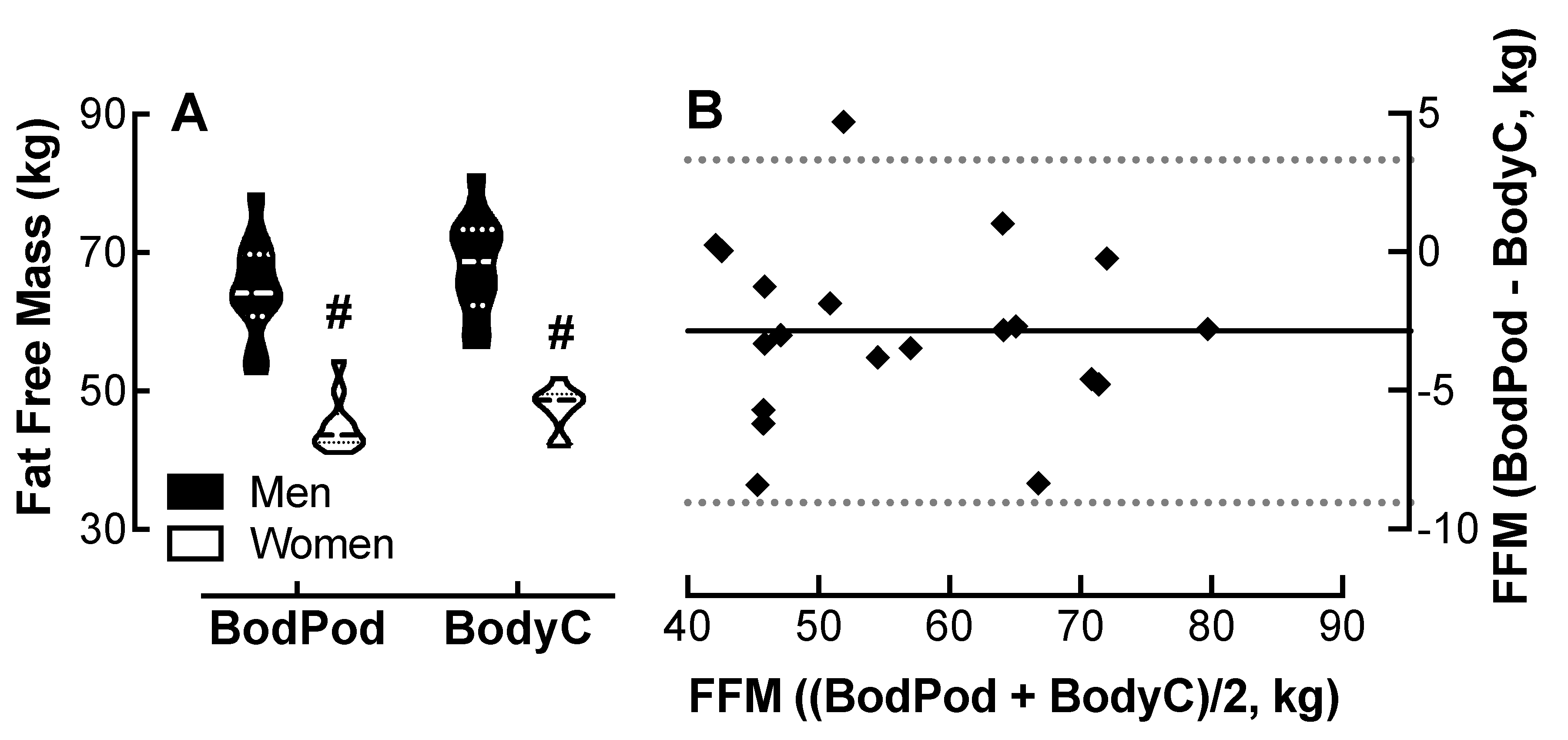
4.6. Comparison of Body Cardio FFM Measurements with Bod Pod Determinations
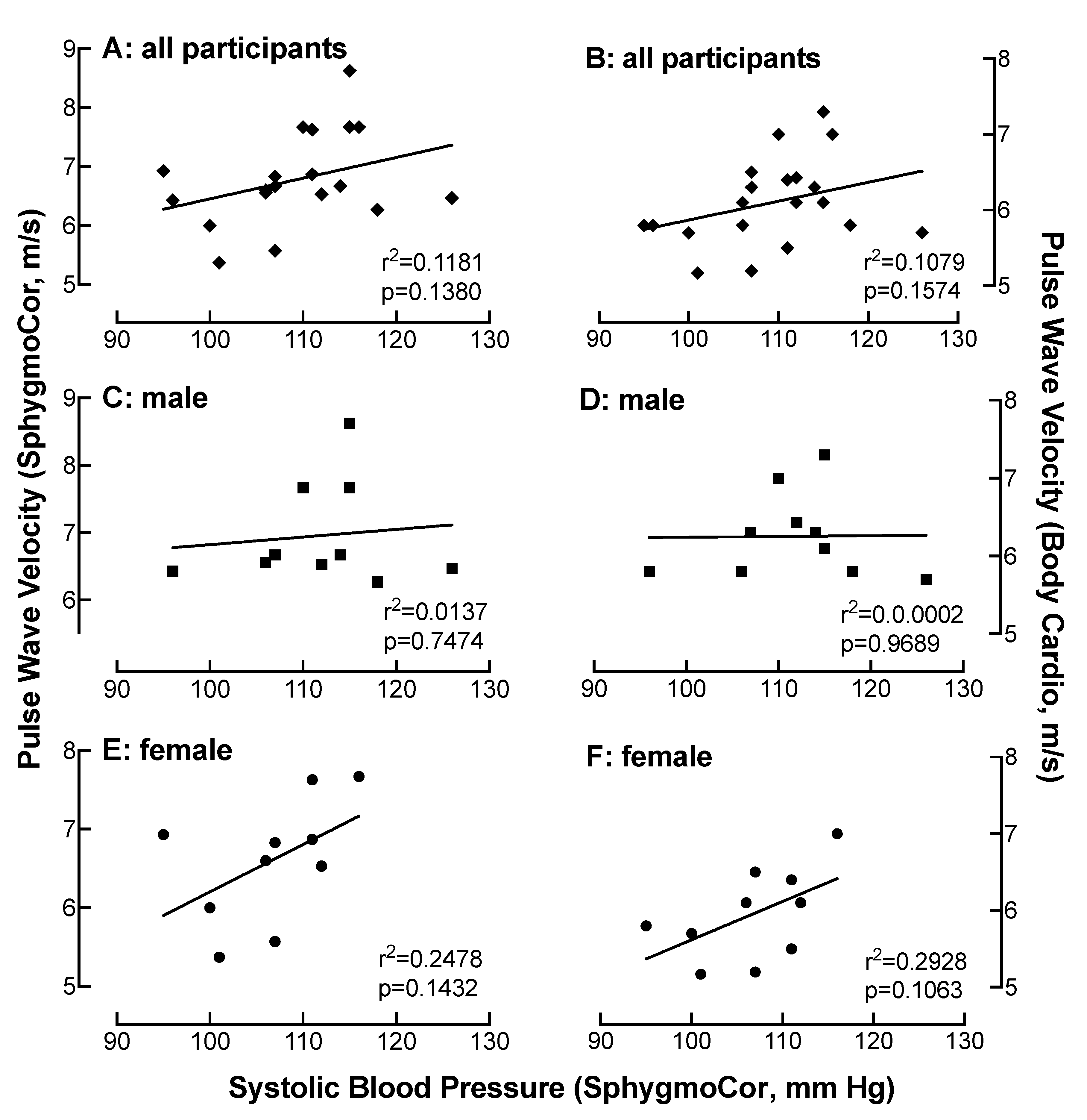
4.7. Relationship of SBP Measured on the SphygmoCor with PWV as a Function of Device
4.8. Relationship of HR Measured on the SphygmoCor with PWV as a Function of Device
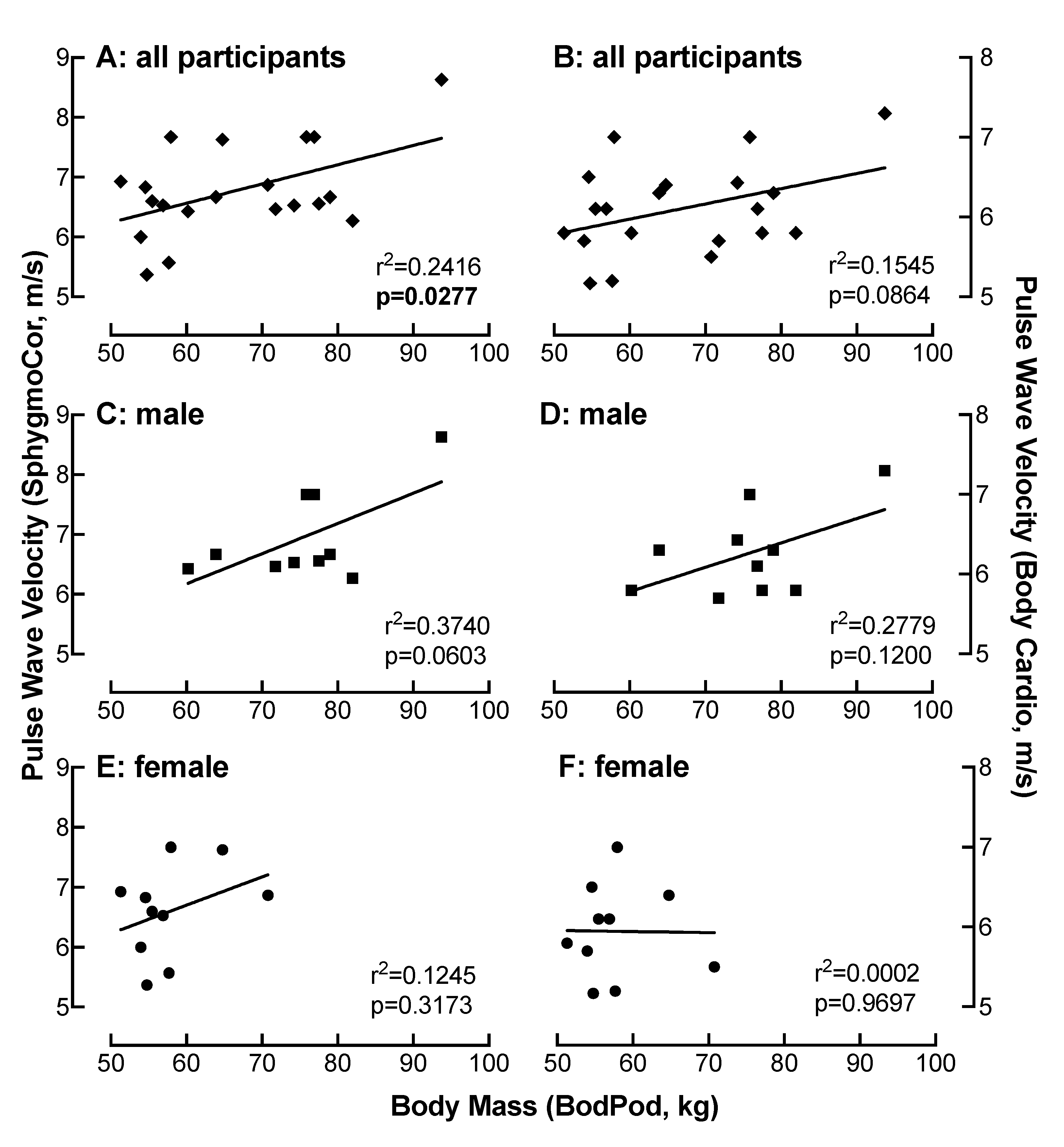
4.9. Relationship of BM Measured on the Bod Pod with PWV as a Function of Device
4.10. Relationship of FM Measured on the Bod Pod with PWV as a Function of Device
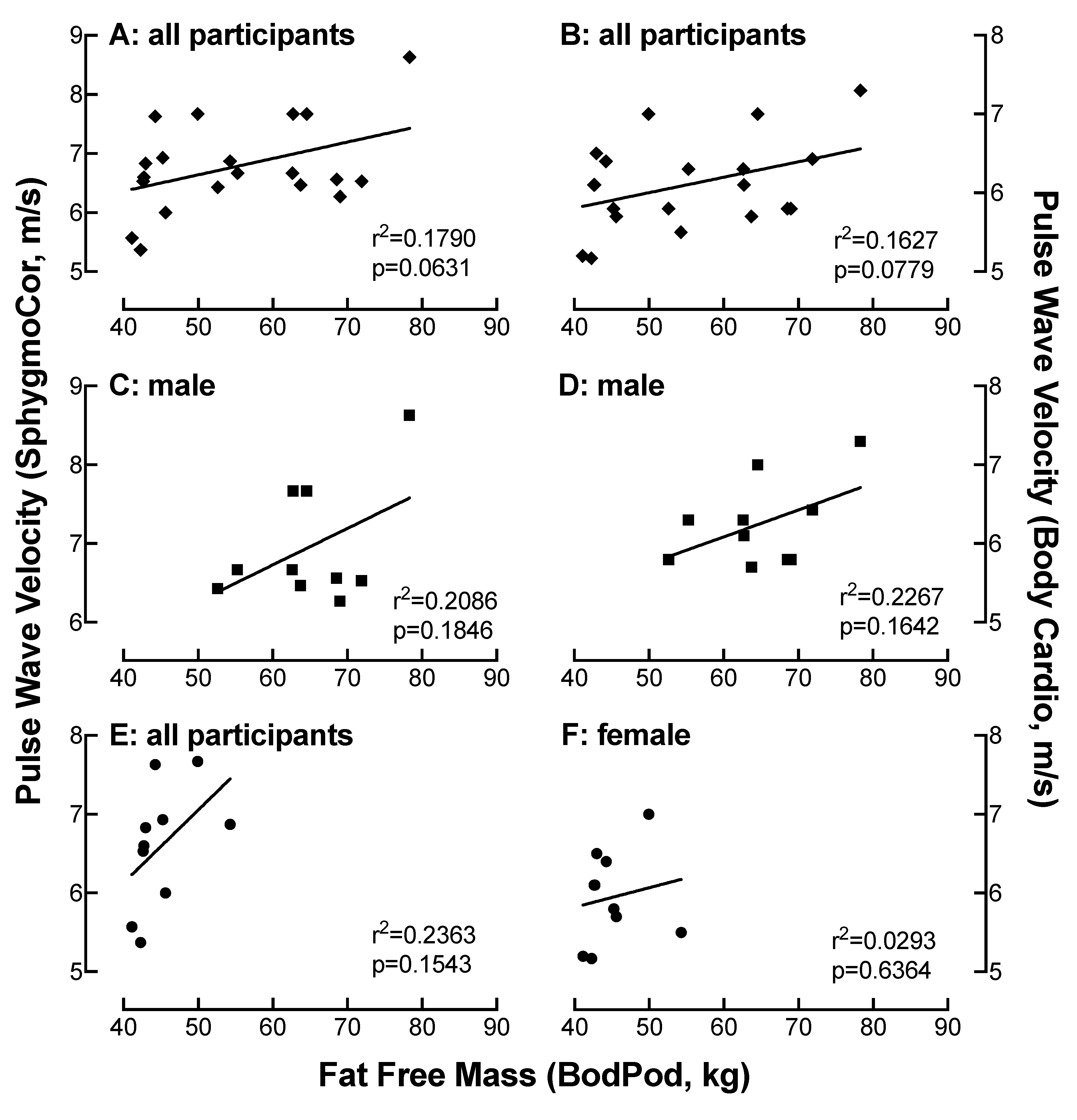
4.11. Relationship of FFM Measured on the Bod Pod with PWV as a Function of Device
5. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Butlin, M.; Qasem, A.; Battista, F.; Bozec, E.; McEniery, C.M.; Millet-Amaury, E.; Pucci, G.; Wilkinson, I.B.; Schillaci, G.; Boutouyrie, P. Carotid-femoral pulse wave velocity assessment using novel cuff-based techniques: Comparison with tonometric measurement. J. Hypertens 2013, 31, 2237–2243. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Kruszon-Moran, D.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA 2016, 315, 2284–2291. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Beydoun, M.A.; Liang, L.; Caballero, B.; Kumanyika, S.K. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008, 16, 2323–2330. [Google Scholar] [CrossRef]
- Bhupathiraju, S.N.; Hu, F.B. Epidemiology of Obesity and Diabetes and Their Cardiovascular Complications. Circ. Res. 2016, 118, 1723–1735. [Google Scholar] [CrossRef]
- Bozec, E.; McEniery, C.M.; Millet-Amaury, E.; Pucci, G.; Wilkinson, I.B.; Schillaci, G.; Boutouyrie, P. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann. Intern. Med. 2004, 140, 992–1000. [Google Scholar]
- Kuk, J.L.; Katzmarzyk, P.T.; Nichaman, M.Z.; Church, T.S.; Blair, S.N.; Ross, R. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring) 2006, 14, 336–341. [Google Scholar] [CrossRef]
- Nicklas, B.J.; Penninx, B.W.; Cesari, M.; Kritchevsky, S.B.; Newman, A.B.; Kanaya, A.M.; Pahor, M.; Ding, J.; Harris, T.B.; Health, A.. Association of visceral adipose tissue with incident myocardial infarction in older men and women: The Health, Aging and Body Composition Study. Am. J. Epidemiol. 2004, 160, 741–749. [Google Scholar] [CrossRef]
- Wilkinson, I.B.; McEniery, C.M.; Schillaci, G.; Boutouyrie, P.; Segers, P.; Donald, A.; Chowienczyk, P.J. ARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: Part 1, arterial pulse wave velocity. Artery Res. 2010, 4, 34–40. [Google Scholar] [CrossRef]
- Butlin, M.; Shirbani, F.; Barin, E.; Tan, I.; Spronck, B.; Avolio, A.P. Cuffless Estimation of Blood Pressure: Importance of Variability in Blood Pressure Dependence of Arterial Stiffness Across Individuals and Measurement Sites. IEEE Trans. Biomed. Eng. 2018, 65, 2377–2383. [Google Scholar] [CrossRef]
- Schroeder, E.C.; Rosenberg, A.J.; Hilgenkamp, T.I.M.; White, D.W.; Baynard, T.; Fernhall, B. Effect of upper body position on arterial stiffness: Influence of hydrostatic pressure and autonomic function. J. Hypertens 2017, 35, 2454–2461. [Google Scholar] [CrossRef]
- Bramwell, J.C.; Hill, A.V. The velocity of the pulse wave in man. Proc. R. Soc. Lond. Ser. B 1922, 93, 298–306. [Google Scholar]
- Van Bortel, L.M.; Laurent, S.; Boutouyrie, P.; Chowienczyk, P.; Cruickshank, J.K.; De Backer, T.; Filipovsky, J.; Huybrechts, S.; Mattace-Raso, F.U.; Protogerou, A.D.; et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J. Hypertens 2012, 30, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, G.F.; Hwang, S.J.; Vasan, R.S.; Larson, M.G.; Pencina, M.J.; Hamburg, N.M.; Vita, J.A.; Levy, D.; Benjamin, E.J. Arterial stiffness and cardiovascular events: The Framingham Heart Study. Circulation 2010, 121, 505–511. [Google Scholar] [CrossRef] [PubMed]
- ownsend, R.R.; Wilkinson, I.B.; Schiffrin, E.L.; Avolio, A.P.; Chirinos, J.A.; Cockcroft, J.R.; Heffernan, K.S.; Lakatta, E.G.; McEniery, C.M.; Mitchell, G.F.; et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness: A Scientific Statement From the American Heart Association. Hypertension 2015, 66, 698–722. [Google Scholar] [CrossRef]
- Ben-Shlomo, Y.; Spears, M.; Boustred, C.; May, M.; Anderson, S.G.; Benjamin, E.J.; Boutouyrie, P.; Cameron, J.; Chen, C.H.; Cruickshank, J.K.; et al. Aortic pulse wave velocity improves cardiovascular event prediction: An individual participant meta-analysis of prospective observational data from 17,635 subjects. J. Am. Coll. Cardiol. 2014, 63, 636–646. [Google Scholar] [CrossRef]
- Vlachopoulos, C.; Aznaouridis, K.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1318–1327. [Google Scholar] [CrossRef]
- Butlin, M.; Qasem, A. Large Artery Stiffness Assessment Using SphygmoCor Technology. Pulse (Basel) 2017, 4, 180–192. [Google Scholar] [CrossRef]
- Campo, D.; Khettab, H.; Yu, R.; Genain, N.; Edouard, P.; Buard, N.; Boutouyrie, P. Measurement of Aortic Pulse Wave Velocity With a Connected Bathroom Scale. Am. J. Hypertens 2017, 30, 876–883. [Google Scholar] [CrossRef]
- Wright, S.P.; Hall Brown, T.S.; Collier, S.R.; Sandberg, K. How consumer physical activity monitors could transform human physiology research. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2017, 312, R358–R367. [Google Scholar] [CrossRef]
- Ball, S.D.; Altena, T.S. Comparison of the Bod Pod and dual energy x-ray absorptiometry in men. Physiol. Meas. 2004, 25, 671–678. [Google Scholar] [CrossRef]
- Higgins, J.P. Smartphone Applications for Patients’ Health and Fitness. Am. J. Med. 2016, 129, 11–19. [Google Scholar] [CrossRef]
- Zheng, Y.; Klem, M.L.; Sereika, S.M.; Danford, C.A.; Ewing, L.J.; Burke, L.E. Self-weighing in weight management: A systematic literature review. Obesity 2015, 23, 256–265. [Google Scholar] [CrossRef]
- Buffa, R.; Mereu, E.; Comandini, O.; Ibanez, M.E.; Marini, E. Bioelectrical impedance vector analysis (BIVA) for the assessment of two-compartment body composition. Eur. J. Clin. Nutr. 2014, 68, 1234–1240. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gomez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis--part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Manuel Gomez, J.; Lilienthal Heitmann, B.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis-part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Andreoli, A.; Matthie, J.; Withers, P. Predicting body cell mass with bioimpedance by using theoretical methods: A technological review. J. Appl. Physiol. 1997, 82, 1542–1558. [Google Scholar] [CrossRef]
- Ackland, T.R.; Lohman, T.G.; Sundgot-Borgen, J.; Maughan, R.J.; Meyer, N.L.; Stewart, A.D.; Muller, W. Current status of body composition assessment in sport: Review and position statement on behalf of the ad hoc research working group on body composition health and performance, under the auspices of the I.O.C. Medical Commission. Sports Med. 2012, 42, 227–249. [Google Scholar] [CrossRef]
- Tucker, L.A.; Lecheminant, J.D.; Bailey, B.W. Test-retest reliability of the Bod Pod: The effect of multiple assessments. Percept. Mot. Skills 2014, 118, 563–570. [Google Scholar] [CrossRef]
- Dewit, O.; Fuller, N.J.; Fewtrell, M.S.; Elia, M.; Wells, J.C. Whole body air displacement plethysmography compared with hydrodensitometry for body composition analysis. Arch. Dis. Child. 2000, 82, 159–164. [Google Scholar] [CrossRef]
- Palmer, B.F.; Clegg, D.J. The sexual dimorphism of obesity. Mol. Cell. Endocrinol. 2015, 402, 113–119. [Google Scholar] [CrossRef]
- Arner, P.; Lithell, H.; Wahrenberg, H.; Bronnegard, M. Expression of lipoprotein lipase in different human subcutaneous adipose tissue regions. J. Lipid Res. 1991, 32, 423–429. [Google Scholar] [PubMed]
- Ramirez, M.E.; McMurry, M.P.; Wiebke, G.A.; Felten, K.J.; Ren, K.; Meikle, A.W.; Iverius, P.H. Evidence for sex steroid inhibition of lipoprotein lipase in men: Comparison of abdominal and femoral adipose tissue. Metabolism 1997, 46, 179–185. [Google Scholar] [CrossRef]
- Tchoukalova, Y.D.; Koutsari, C.; Votruba, S.B.; Tchkonia, T.; Giorgadze, N.; Thomou, T.; Kirkland, J.L.; Jensen, M.D. Sex- and depot-dependent differences in adipogenesis in normal-weight humans. Obesity (Silver Spring) 2010, 18, 1875–1880. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.A.; Tao, C.; Gupta, R.K.; Scherer, P.E. Tracking adipogenesis during white adipose tissue development, expansion and regeneration. Nat. Med. 2013, 19, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Maloberti, A.; Vallerio, P.; Triglione, N.; Occhi, L.; Panzeri, F.; Bassi, I.; Pansera, F.; Piccinelli, E.; Peretti, A.; Garatti, L.; et al. Vascular Aging and Disease of the Large Vessels: Role of Inflammation. High Blood Press. Cardiovasc. Prev. 2019, 26, 175–182. [Google Scholar] [CrossRef]
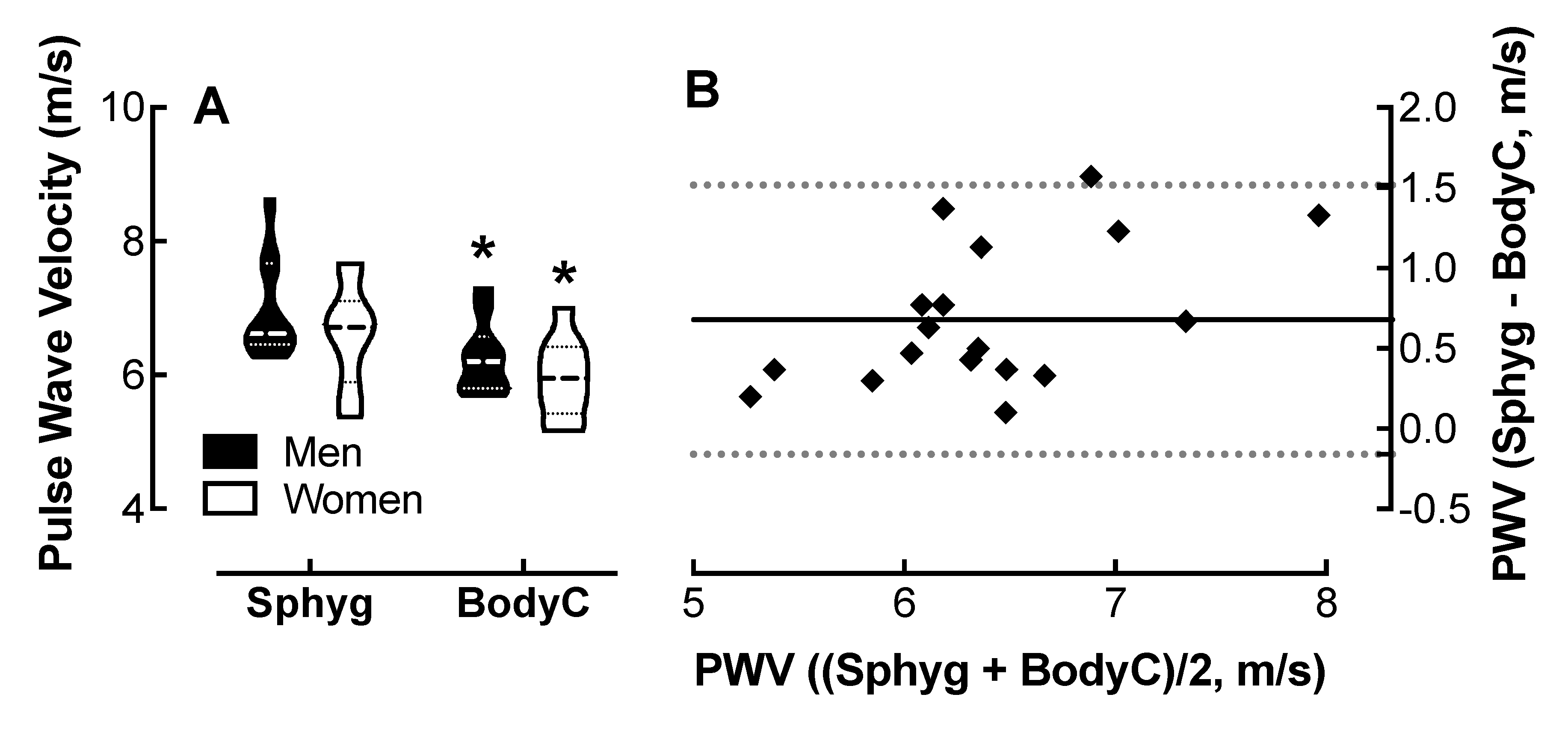
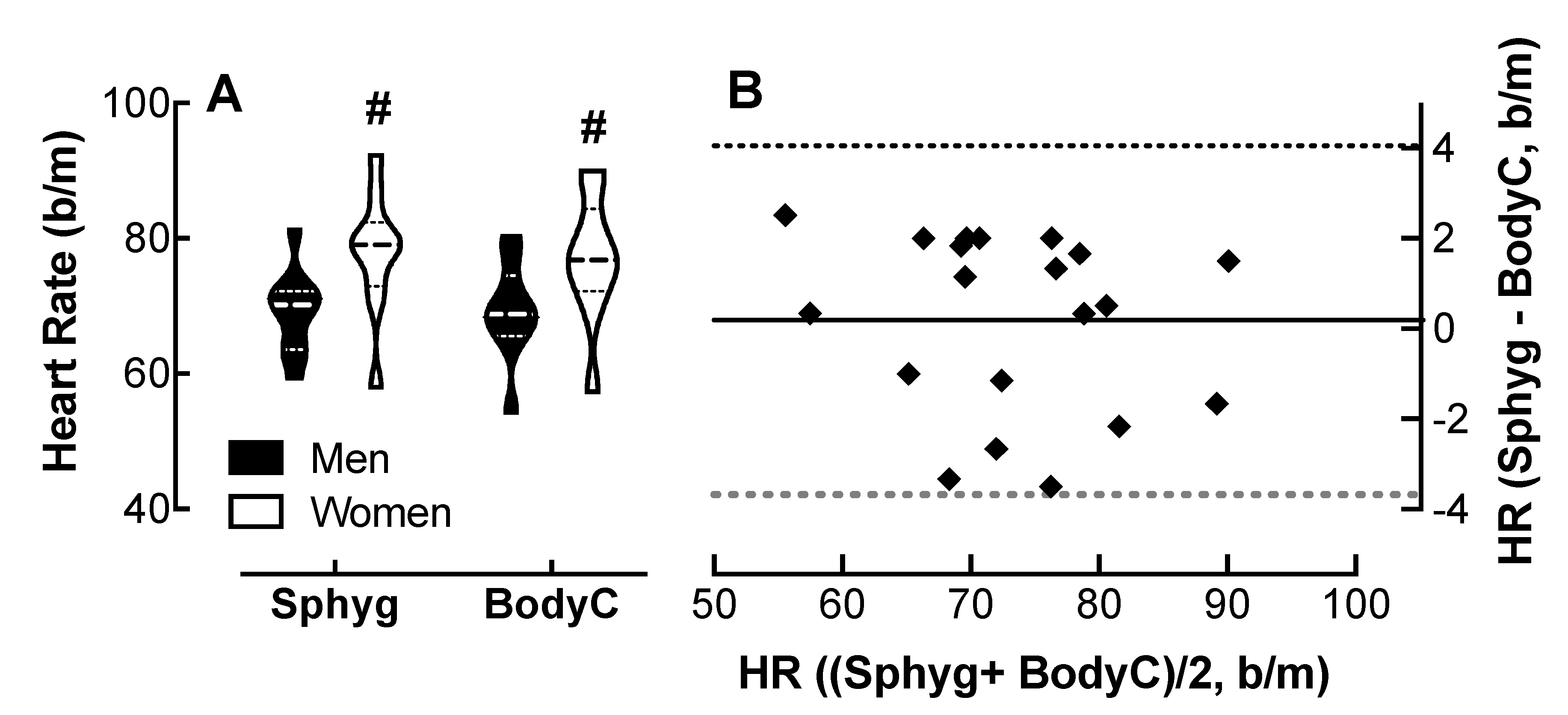
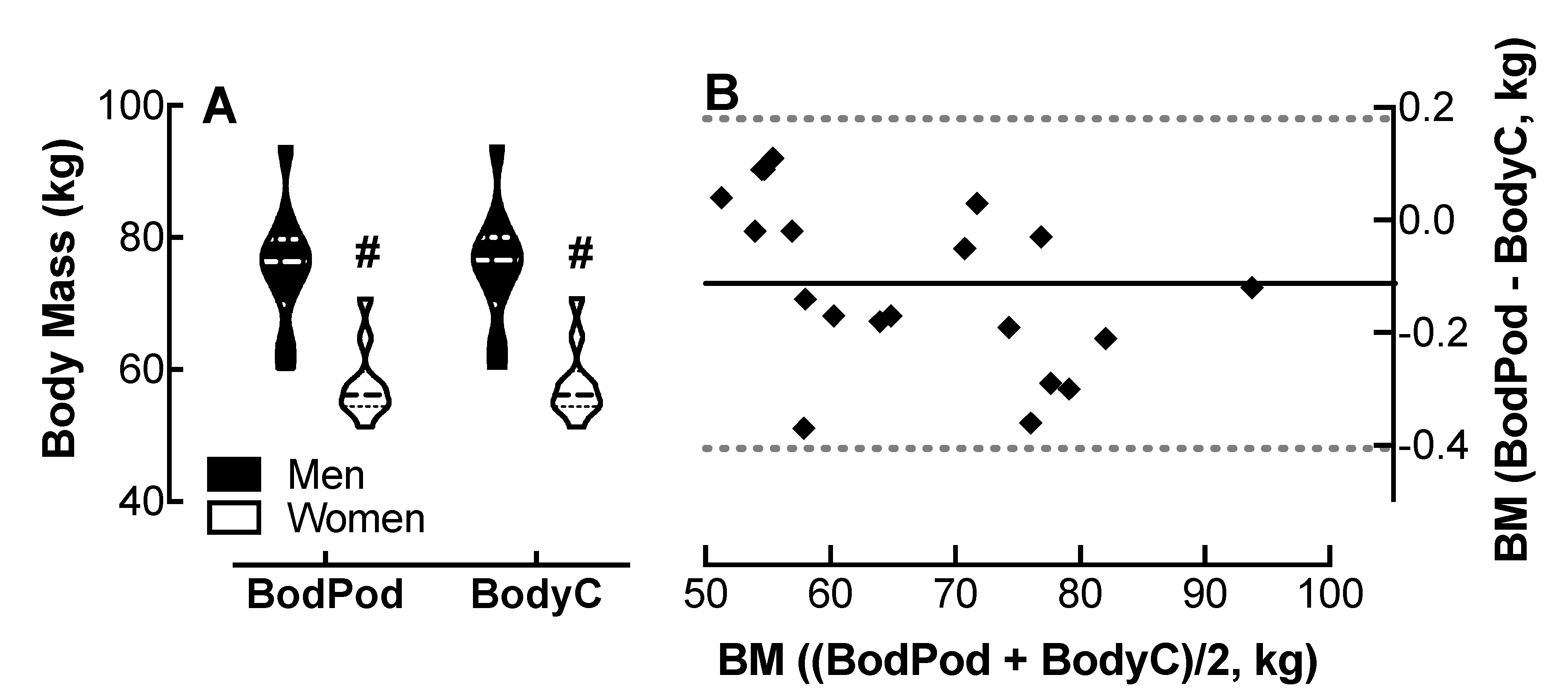
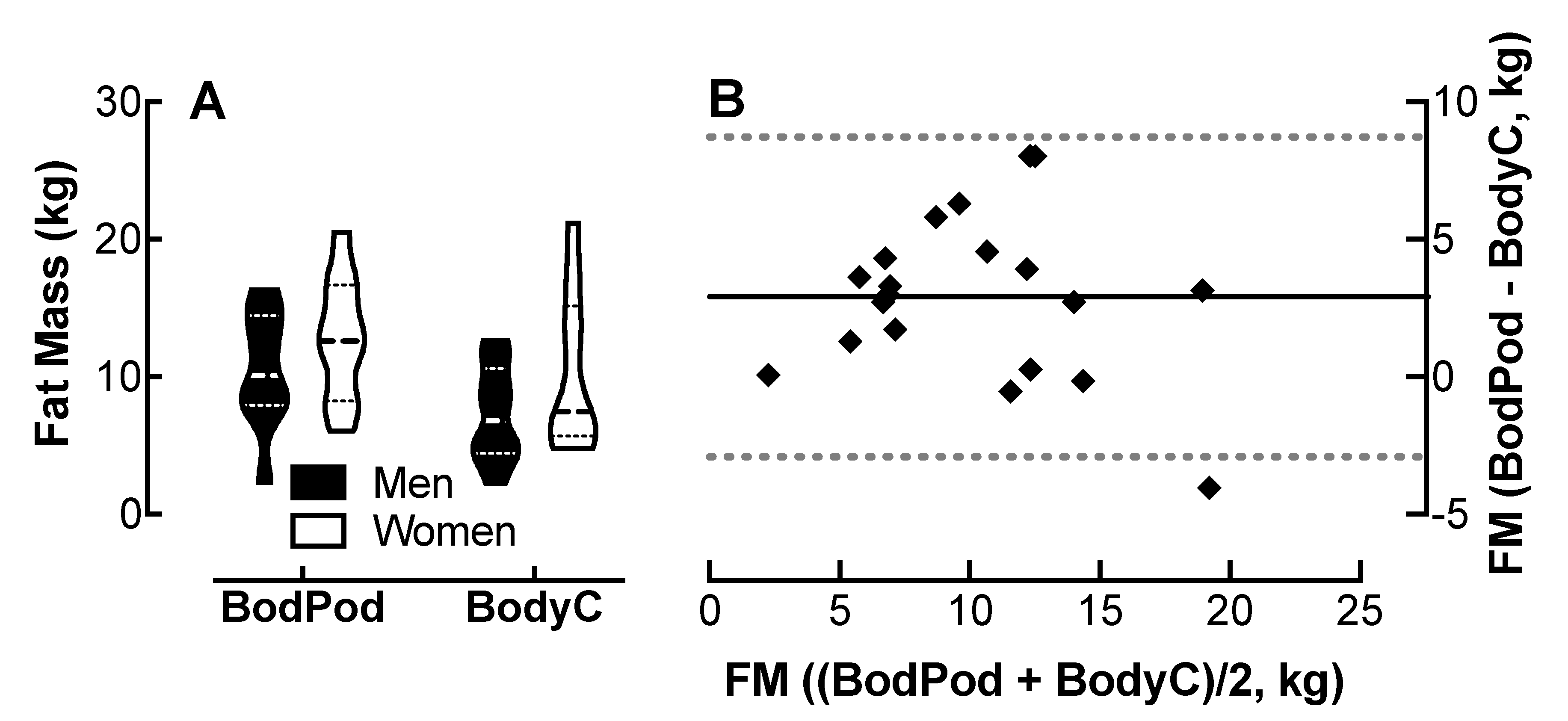

| Parameter | Cohort | Bias ± SD | 95% Limits of Agreement |
|---|---|---|---|
| PWV | Men + Women | 0.68 ± 0.43 | −0.16 to 1.50 |
| Men only | 0.71 ± 0.44 | −0.17 to 1.58 | |
| Women only | 0.65 ± 0.43 | −0.19 to 1.50 | |
| HR | Men + Women | 0.18 ± 1.97 | −3.68 to 4.05 |
| Men only | −0.05 ± 2.37 | −4.70 to 4.60 | |
| Women only | 0.42 ± 1.57 | −2.65 to 3.49 | |
| BM | Men + Women | −0.11 ± 0.15 | −0.41 to 0.18 |
| Men only | −0.18 ± 0.12 | −0.42 to 0.05 | |
| Women only | −1.04 ± 0.15 | −0.34 to 0.25 | |
| FM | Men + Women | 2.91 ± 2.97 | −2.91 to 8.73 |
| Men only | 3.28 ± 2.39 | −1.41 to 7.97 | |
| Women only | 2.54 ± 3.55 | −4.42 to 9.50 | |
| FFM | Men + Women | −2.87 ± 3.15 | −9.05 to 3.31 |
| Men only | −3.26 ± 2.55 | −8.25 to 1.74 | |
| Women only | −2.48 ± 3.76 | −9.86 to 4.89 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collier, S.R.; McCraw, C.; Campany, M.; Lubkemann, A.; StClair, P.; Ji, H.; Sandberg, K.; Morgan, J.W.; Smith, C.J. Withings Body Cardio Versus Gold Standards of Pulse-Wave Velocity and Body Composition. J. Pers. Med. 2020, 10, 17. https://doi.org/10.3390/jpm10010017
Collier SR, McCraw C, Campany M, Lubkemann A, StClair P, Ji H, Sandberg K, Morgan JW, Smith CJ. Withings Body Cardio Versus Gold Standards of Pulse-Wave Velocity and Body Composition. Journal of Personalized Medicine. 2020; 10(1):17. https://doi.org/10.3390/jpm10010017
Chicago/Turabian StyleCollier, Scott R., Conner McCraw, Megan Campany, Austin Lubkemann, Price StClair, Hong Ji, Kathryn Sandberg, Joseph W. Morgan, and Caroline J. Smith. 2020. "Withings Body Cardio Versus Gold Standards of Pulse-Wave Velocity and Body Composition" Journal of Personalized Medicine 10, no. 1: 17. https://doi.org/10.3390/jpm10010017
APA StyleCollier, S. R., McCraw, C., Campany, M., Lubkemann, A., StClair, P., Ji, H., Sandberg, K., Morgan, J. W., & Smith, C. J. (2020). Withings Body Cardio Versus Gold Standards of Pulse-Wave Velocity and Body Composition. Journal of Personalized Medicine, 10(1), 17. https://doi.org/10.3390/jpm10010017





