Arrhythmogenic Inflammatory Cardiomyopathy in Autoimmune Rheumatic Diseases: A Challenge for Cardio-Rheumatology
Abstract
1. Introduction
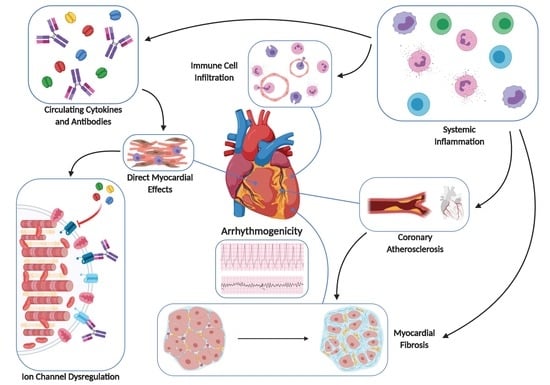
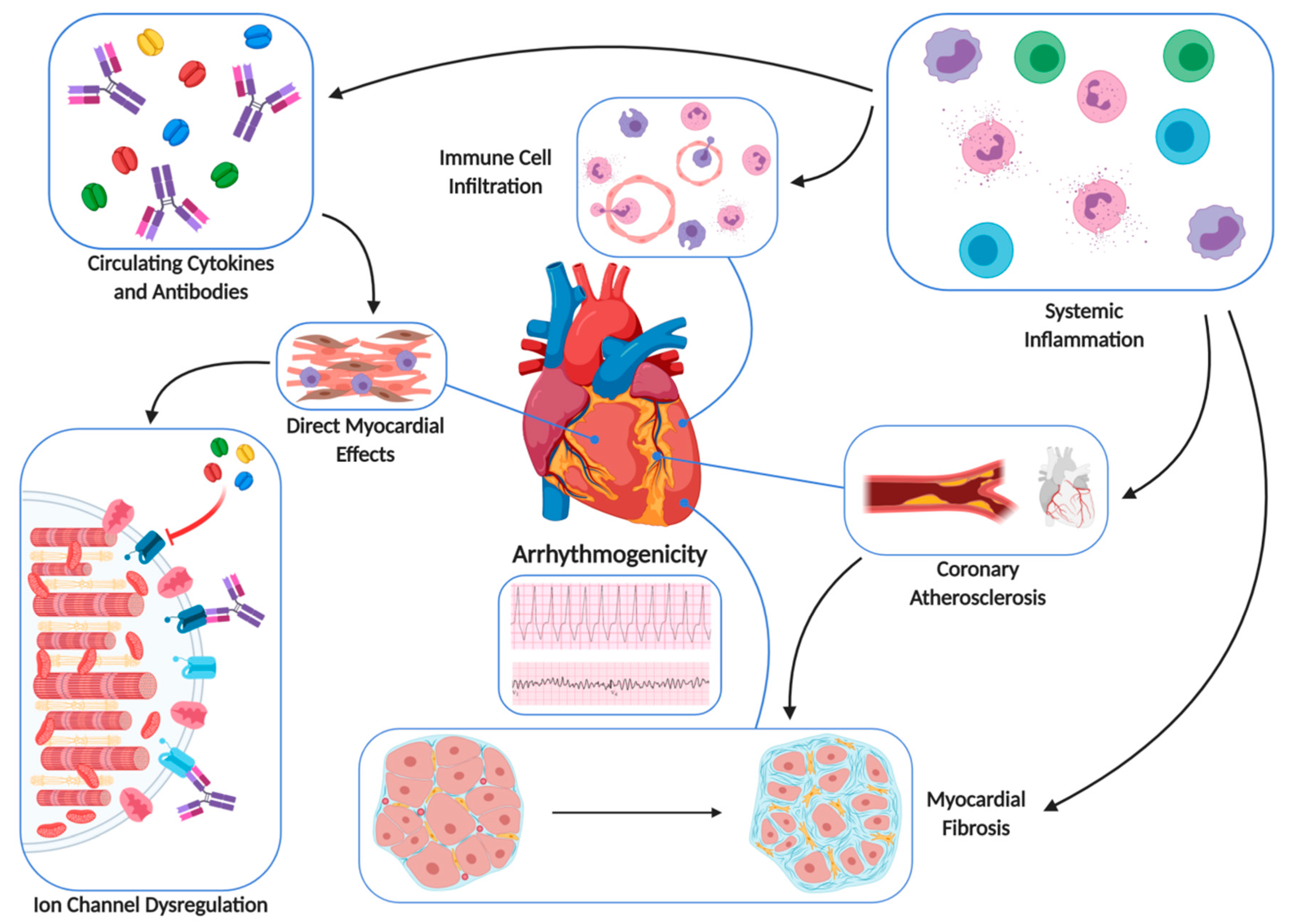
2. Pathophysiology of AIC in ARDs
2.1. Fibrotic Substrate
2.2. Inflammatory Substrate
2.3. Cardiac Channelopathy due to Specific Autoantibodies
3. AIC in ARD Patients
4. Clinical Manifestations of AIC in ARDs
5. Diagnostic Algorithm of AIC in ARDs
6. Role of Troponin
7. Treatment of AIC in ARDs
7.1. Cardiologic Pharmaceutical Approach
7.1.1. Beta Blockers Administration
7.1.2. ACE Inhibitors and/or ARBs
7.2. Aldosterone Antagonists
7.3. Cardiologic Interventional Approach
7.3.1. Implantable Cardioverter–Defibrillator Therapy
7.3.2. Ablation Therapy
7.3.3. Pharmacologic Treatment
7.4. Rheumatologic Pharmaceutical Approach
8. Conclusions
Funding
Conflicts of Interest
References
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2018, 138, e210–e271. [Google Scholar] [PubMed]
- Semsarian, C.; Ingles, J. Molecular autopsy in victims of inherited arrhythmias. J. Arrhythm. 2016, 32, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Seferović, P.M.; Ristić, A.D.; Maksimović, R.; Simeunović, D.S.; Ristić, G.G.; Radovanović, G.; Seferović, D.; Maisch, B.; Matucci-Cerinic, M. Cardiac arrhythmias and conduction disturbances in autoimmune rheumatic diseases. Rheumatology (Oxford) 2006, 45 (Suppl. 4), iv39–iv42. [Google Scholar] [CrossRef]
- Mavrogeni, S.I.; Sfikakis, P.P.; Markousis-Mavrogenis, G.; Bournia, V.K.; Poulos, G.; Koutsogeorgopoulou, L.; Karabela, G.; Stavropoulos, E.; Katsifis, G.; Boki, K.; et al. Cardiovascular magnetic resonance imaging pattern in patients with autoimmune rheumatic diseases and ventricular tachycardia with preserved ejection fraction. Int. J. Cardiol. 2019, 284, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Mavrogeni, S.I.; Sfikakis, P.P.; Dimitroulas, T.; Koutsogeorgopoulou, L.; Markousis-Mavrogenis, G.; Poulos, G.; Kolovou, G.; Theodorakis, G.; Kitas, G.D. Prospects of using cardiovascular magnetic resonance in the identification of arrhythmogenic substrate in autoimmune rheumatic diseases. Rheumatol. Int. 2018, 38, 1615–1621. [Google Scholar] [CrossRef] [PubMed]
- De Bakker, J.M.; van Capelle, F.J.; Janse, M.J.; Wilde, A.A.; Coronel, R.; Becker, A.E.; Hauer, R.N. Reentry as a cause of ventricular tachycardia in patients with chronic ischemic heart disease: Electrophysiologic and anatomic correlation. Circulation 1988, 77, 589–606. [Google Scholar] [CrossRef] [PubMed]
- De Bakker, J.M.; van Capelle, F.J.; Janse, M.J.; Tasseron, S.; Vermeulen, J.T.; de Jonge, N.; Lahpor, J.R. Fractionated electrograms in dilated cardiomyopathy: Origin and relation to abnormal conduction. J. Am. Coll. Cardiol. 1996, 27, 1071–1078. [Google Scholar] [CrossRef]
- Isber, N.; Restivo, M.; Gough, W.B.; Yang, H.; el-Sherif, N. Circus movement atrial flutter in the canine sterile pericarditis model: Cryothermal termination from the epicardial site of the slow zone of the reentrant circuit. Circulation 1993, 87, 1649–1660. [Google Scholar] [CrossRef]
- Ryu, K.; Li, L.; Khrestian, C.M.; Matsumoto, N.; Sahadevan, J.; Ruehr, M.L.; Van Wagoner, D.R.; Efimov, I.R.; Waldo, A.L. Effects of sterile pericarditis on connexins 40 and 43 in the atria: Correlation with abnormal conduction and atrial arrhythmias. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H1231–H1241. [Google Scholar] [CrossRef]
- Sadrpour, S.A.; Srinivasan, D.; Bhimani, A.A.; Lee, S.; Ryu, K.; Cakulev, I.; Khrestian, C.M.; Markowitz, A.H.; Waldo, A.L.; Sahadevan, J. Insights into new-onset atrial fibrillation following open heart surgery and implications for type II atrial flutter. Europace 2015, 17, 1834–1839. [Google Scholar] [CrossRef]
- Lazzerini, P.E.; Capecchi, P.L.; Guideri, F.; Acampa, M.; Galeazzi, M.; Laghi Pasini, F. Connective tissue diseases and cardiac rhythm disorders: An overview. Autoimmun. Rev. 2006, 5, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Capecchi, P.L.; Guideri, F.; Acampa, M.; Selvi, E.; Bisogno, S.; Galeazzi, M.; Laghi-Pasini, F. Autoantibody-mediated cardiac arrhythmias: Mechanisms and clinical implications. Basic Res. Cardiol. 2008, 103, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Korkmaz, S.; Zitron, E.; Bangert, A.; Seyler, C.; Li, S.; Heged€us, P.; Scherer, D.; Li, J.; Fink, T.; Schweizer, P.A.; et al. Provocation of an autoimmune response to cardiac voltage-gated sodiumchannel NaV1.5 induces cardiac conduction defects in rats. J. Am. Coll. Cardiol. 2013, 62, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Maguy, A.; Duverger, J.E.; Vigneault, P.; Comtois, P.; Shi, Y.; Tardif, J.C.; Thomas, D.; Nattel, S. Induced KCNQ1 autoimmunity accelerates cardiac repolarization in rabbits: Potential significance in arrhythmogenesis and antiarrhythmic therapy. Heart Rhythm. 2014, 11, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
- Fabris, F.; Yue, Y.; Qu, Y.; Chahine, M.; Sobie, E.; Lee, P.; Wieczorek, R.; Jiang, X.C.; Capecchi, P.L.; Laghi-Pasini, F.; et al. Induction of autoimmune response to the extracellular loop of the HERG channel pore induces QTc prolongation in guinea-pigs. J. Physiol. 2016, 594, 6175–6187. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Capecchi, P.L.; Laghi-Pasini, F.; Boutjdir, M. Autoimmune channelopathies as a novel mechanism in cardiac arrhythmias. Nat. Rev. Cardiol. 2017, 14, 521–535. [Google Scholar] [CrossRef]
- Lazzerini, P.E.; Capecchi, P.L.; Laghi-Pasini, F. Systemic inflammation and arrhythmic risk: Lessons from rheumatoid arthritis. Eur. Heart J. 2017, 38, 1717–1727. [Google Scholar] [CrossRef]
- Lazzerini, P.E.; Capecchi, P.L.; Laghi-Pasini, F. Long QT syndrome: An emerging role for inflammation and immunity. Front. Cardiovasc. Med. 2015, 2, 26. [Google Scholar] [CrossRef]
- Medenwald, D.; Kors, J.A.; Loppnow, H.; Thiery, J.; Kluttig, A.; Nuding, S.; Tiller, D.; Greiser, K.H.; Werdan, K.; Haerting, J. Inflammation and prolonged QT time: Results from the cardiovascular disease, living and ageing in Halle (CARLA) study. PLoS ONE 2014, 9, e95994. [Google Scholar] [CrossRef]
- Albert, C.M.; Ma, J.; Rifai, N.; Stampfer, M.J.; Ridker, P.M. Prospective study of C reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. Circulation 2002, 105, 2595–2599. [Google Scholar] [CrossRef]
- Ukena, C.; Mahfoud, F.; Kindermann, I.; Kandolf, R.; Kindermann, M.; B€ohm, M. Prognostic electrocardiographic parameters in patients with suspected myocarditis. Eur. J. Heart Fail. 2011, 13, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Pisoni, C.N.; Reina, S.; Arakaki, D.; Eimon, A.; Carrizo, C.; Borda, E. Elevated IL-1b levels in anti-Ro/SSA connective tissue diseases patients with prolonged corrected QTc interval. Clin. Exp. Rheumatol. 2015, 33, 715–720. [Google Scholar] [PubMed]
- Tisdale, J.E.; Jaynes, H.A.; Kingery, J.R.; Mourad, N.A.; Trujillo, T.N.; Overholser, B.R.; Kovacs, R.J. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ. Cardiovasc. Qual. Outcomes. 2013, 6, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Acampa, M.; Capecchi, P.L.; Fineschi, I.; Selvi, E.; Moscadelli, V.; Zimbone, S.; Gentile, D.; Galeazzi, M.; Laghi-Pasini, F. Antiarrhythmic potential of anticytokine therapy in rheumatoid arthritis: Tocilizumab reduces corrected QT interval by controlling systemic inflammation. Arthritis Care Res. (Hoboken) 2015, 67, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Cerrone, M.; Priori, S.G. Genetics of sudden death: Focus on inherited channelopathies. Eur. Heart J. 2011, 32, 2109–2118. [Google Scholar] [CrossRef] [PubMed]
- Yue, Y.; Castrichini, M.; Srivastava, U.; Fabris, F.; Shah, K.; Li, Z.; Qu, Y.; El-Sherif, N.; Zhou, Z.; January, C.; et al. Pathogenesis of the novel autoimmune-associated long-QT syndrome. Circulation 2015, 132, 230–240. [Google Scholar] [CrossRef]
- Boutjdir, M.; Lazzerini, P.E.; Capecchi, P.L.; Laghi-Pasini, F.; El-Sherif, N. Potassium channel block and novel autoimmune-associated long QT syndrome. Card Electrophysiol. Clin. 2016, 8, 373–384. [Google Scholar] [CrossRef]
- Hayashi, N.; Koshiba, M.; Nishimura, K.; Sugiyama, D.; Nakamura, T.; Morinobu, S.; Kawano, S.; Kumagai, S. Prevalence of disease-specific antinuclear antibodies in general population: Estimates from annual physical examinations of residents of a small town over a 5-year period. Mod. Rheumatol. 2008, 18, 153–160. [Google Scholar] [CrossRef]
- Suzuki, S.; Satoh, T.; Yasuoka, H.; Hamaguchi, Y.; Tanaka, K.; Kawakami, Y.; Suzuki, N.; Kuwana, M. Novel autoantibodies to a voltage-gated potassium channel Kv1.4 in a severe form of myasthenia gravis. J. Neuroimmunol. 2005, 170, 141–149. [Google Scholar] [CrossRef]
- Suzuki, S.; Baba, A.; Kaida, K.; Utsugisawa, K.; Kita, Y.; Tsugawa, J.; Ogawa, G.; Nagane, Y.; Kuwana, M.; Suzuki, N. Cardiac involvements in myasthenia gravis associated with anti-Kv1.4 antibodies. Eur. J. Neurol. 2014, 21, 223–230. [Google Scholar] [CrossRef]
- Borek, G.; Jenzer, H.R.; Frey, L.D.; Locher, J.T. Repetitive exercise induced ventricular tachycardia in a patient with rheumatoid arthritis taking low dose methotrexate. J. Rheumatol. 1992, 19, 1004–1005. [Google Scholar] [PubMed]
- Lazzerini, P.E.; Acampa, M.; Hammoud, M.; Maffei, S.; Capecchi, P.L.; Selvi, E.; Bisogno, S.; Guideri, F.; Galeazzi, M.; Pasini, F.L. Arrhythmic risk during acute infusion of infliximab: A prospective, single-blind, placebo-controlled, crossover study in patients with chronic arthritis. J. Rheumatol. 2008, 35, 1958–1965. [Google Scholar] [PubMed]
- Rosenstein, E.D.; Zucker, M.J.; Kramer, N. Giant cell myocarditis: Most fatal of autoimmune diseases. Semin. Arthritis Rheum. 2000, 30, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, R.A.; Borba, E.F.; Pedrosa, A.; Nishioka, S.; Viana, V.S.; Ramires, J.A.; Kalil-Filho, R.; Bonfá, E.; Martinelli Filho, M. Evidence for cardiac safety and antiarrhythmic potential of chloroquine in systemic lupus erythematosus. Europace 2014, 16, 887–892. [Google Scholar] [CrossRef]
- Huang, C.N.; Yu, H.H.; Chiu, S.N.; Lee, J.H.; Wang, L.C.; Yang, Y.H.; Chiang, B.L. Acute myocarditis and ventricular fibrillation as initial presentation of pediatric systemic lupus erythematosus. Rheumatol. Int. 2013, 33, 1093–1096. [Google Scholar] [CrossRef]
- Chen, C.Y.; Wang, F.L.; Lin, C.C. Chronic hydroxychloroquine use associated with QT prolongation and refractory ventricular arrhythmia. Clin. Toxicol. 2006, 44, 173–175. [Google Scholar] [CrossRef]
- Couto, N.; Ladeira, R.; Pimenta, J. Regression of tachycardiomyopathy after implant of pacemaker with antitachycardial function. Arq. Bras. Cardiol. 1993, 60, 31–33. [Google Scholar]
- Mavrogeni, S.; Gargani, L.; Pepe, A.; Monti, L.; Markousis-Mavrogenis, G.; De Santis, M.; De Marchi, D.; Koutsogeorgopoulou, L.; Karabela, G.; Guiducci, S.; et al. Cardiac Magnetic Resonance Predicts Ventricular Arrhythmias in Scleroderma: The Scleroderma Arrhythmia Clinical Utility Study [SAnCtUS] Rheumatology; Oxford Academic: Oxford, UK, 2019. (in press)
- Jindal, G.; Singh, S.; Suri, D.; Rawat, A.; Rohit, M. Recurrent ventricular tachycardia in a child with juvenile dermatomyositis - an unusual association. Int. J. Rheum. Dis. 2012, 15, e26–e27. [Google Scholar] [CrossRef]
- Dilaveris, P.; Pietri, P.; Tsiachris, D.; Gatzoulis, K.; Stefanadis, C. Inducible ventricular tachycardia due to dermatomyositis-related cardiomyopathy in the era of implantable cardioverter-defibrillator therapy. Circulation 2012, 125, 967–969. [Google Scholar] [CrossRef][Green Version]
- Cuilleret, F.J.; Agraou, B.; Kyndt, X.; Cuilleret, V.; Agraou, H.; el Mansour, N.; Abolmaali, K.; Bodart, J.C.; Cattet, I.; Manouvrier, J.; et al. Cardiac effects of dermatomyositis. A case report. Arch. Mal. Coeur Vaiss. 2003, 96, 919–922. [Google Scholar]
- Adler, M.; Banerjeee, S.; Stratton, R. Ventricular tachycardia as a presenting feature of dermatomyositis. Heart 2002, 88, 443. [Google Scholar] [CrossRef][Green Version]
- Ishimaru, S.; Tsujino, I.; Takei, T.; Tsukamoto, E.; Sakaue, S.; Kamigaki, M.; Ito, N.; Ohira, H.; Ikeda, D.; Tamaki, N. Focal uptake on 18F-fluoro- 2-deoxyglucose positron emission tomography images indicates cardiac involvement of sarcoidosis. Eur. Heart J. 2005, 26, 1538–1543. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef]
- Mavrogeni, S.; Sfikakis, P.; Dimitroulas, T.; Kolovou, G.; Kitas, G.D. Edema and fibrosis imaging by cardiovascular magnetic resonance: How can the experience of Cardiology be best utilized in rheumatological practice? Semin. Arthritis Rheum. 2014, 44, 76–85. [Google Scholar] [CrossRef]
- Mavrogeni, S.I.; Kitas, G.D.; Dimitroulas, T.; Sfikakis, P.P.; Seo, P.; Gabriel, S.; Patel, A.R.; Gargani, L.; Bombardieri, S.; Matucci-Cerinic, M.; et al. Cardiovascular magnetic resonance in rheumatology: Current status and recommendations for use. Int. J. Cardiol. 2016, 217, 135–148. [Google Scholar] [CrossRef]
- McCarthy, R.E.; Boehmer, J.P.; Hruban, R.H.; Hutchins, G.M.; Kasper, E.K.; Hare, J.M.; Baughman, K.L. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N. Engl. J. Med. 2000, 342, 690–695. [Google Scholar] [CrossRef]
- Van Wijngaarden, S.E.; Ben Said-Bouyeri, S.; Ninaber, M.K.; Huizinga, T.W.; Schalij, M.J.; Bax, J.J.; Delgado, V.; de Vries-Bouwstra, J.K.; Marsan, N.A. Progression of Left Ventricular Myocardial Dysfunction in Systemic Sclerosis: A Speckle-tracking Strain Echocardiography Study. J. Rheumatol. 2019, 46, 405–415. [Google Scholar] [CrossRef]
- Nikdoust, F.; Bolouri, E.; Tabatabaei, S.A.; Goudarzvand, M.; Faezi, S.T. Early diagnosis of cardiac involvement in systemic lupus erythematosus via global longitudinal strain (GLS) by speckle tracking echocardiography. J. Cardiovasc. Thorac. Res. 2018, 10, 231–235. [Google Scholar] [CrossRef]
- Cooper, L.T., Jr. Myocarditis. N. Engl. J. Med. 2009, 360, 1526–1538. [Google Scholar] [CrossRef]
- Dennert, R.H.; Crijns, J.; Heymans, S. Acute viral myocarditis. Eur. Heart J. 2008, 29, 2073–2082. [Google Scholar] [CrossRef]
- Tung, R.; Bauer, B.; Schelbert, H.; Lynch, J.P., 3rd; Auerbach, M.; Gupta, P.; Schiepers, C.; Chan, S.; Ferris, J.; Barrio, M.; et al. Incidence of abnormal positron emission tomography in patients with unexplained cardiomyopathy and ventricular arrhythmias: The potential role of occult inflammation in arrhythmogenesis. Heart Rhythm. 2015, 12, 2488–2498. [Google Scholar] [CrossRef]
- Bhatia, S.; Anstine, C.; Jaffe, A.S.; Gersh, B.J.; Chandrasekaran, K.; Foley, T.A.; Hodge, D.; Anavekar, N.S. Cardiac magnetic resonance in patients with elevated troponin and normal coronary angiography. Heart 2019, 105, 1231–1236. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Pak, K.; Kim, K. Diagnostic performance of F-18 FDG PET for detection of cardiac sarcoidosis; A systematic review and meta-analysis. J. Nucl. Cardiol. 2019, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Ha, F.J.; Agarwal, S.; Tweed, K.; Palmer, S.C.; Adams, H.S.; Thillai, M.; Williams, L. Imaging in Suspected Cardiac Sarcoidosis: A Diagnostic Challenge. Curr. Cardiol. Rev. 2019, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Z.; Shioji, K.; Kihara, Y.; Takenaka, H.; Onozawa, Y.; Kishimoto, C. Cardioprotective effects of carvedilol on acute autoimmune myocarditis: Anti-inflammatory effects associated with antioxidant property. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, H83–H90. [Google Scholar] [CrossRef] [PubMed]
- Exner, D.V.; Reiffel, J.A.; Epstein, A.E.; Ledingham, R.; Reiter, M.J.; Yao, Q.; Duff, H.J.; Follmann, D.; Schron, E.; Greene, H.L. Beta-blocker use and survival in patients with ventricular fibrillation or symptomatic ventricular tachycardia: The Antiarrhythmics Versus Implantable Defibrillators (AVID) trial. J. Am. Coll. Cardiol. 1999, 34, 325–333. [Google Scholar] [CrossRef]
- Moss, A.J.; Hall, W.J.; Cannom, D.S.; Daubert, J.P.; Higgins, S.L.; Klein, H.; Levine, J.H.; Saksena, S.; Waldo, A.L.; Wiber, D. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N. Engl. J. Med. 1996, 335, 1933–1940. [Google Scholar] [CrossRef]
- Moss, A.J.; Zareba, W.; Hall, W.J.; Klein, H.; Wiber, D.J.; Cannom, D.S.; Daubert, J.P.; Higgins, S.L.; Brown, M.W.; Andrews, M.L. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N. Engl. J. Med. 2002, 346, 877–883. [Google Scholar] [CrossRef]
- Bardy, G.H.; Lee, K.L.; Mark, D.B.; Poole, J.E.; Packer, D.L.; Boineau, R.; Domanski, M.; Troutman, C.; Anderson, J.; Johnson, G. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. Engl. J. Med. 2005, 352, 225–237. [Google Scholar] [CrossRef]
- Kober, L.; Thune, J.J.; Nielsen, J.J.; Haarbo, J.; Videbek, L.; Korup, E.; Jensen, G.; Hildebrandt, P.; Steffensen, F.H.; Bruun, N.E. Defibrillator implantation in patients with nonischemic systolic heart failure. N. Engl. J. Med. 2016, 375, 1221–1230. [Google Scholar] [CrossRef] [PubMed]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2017, 72, e91–e220. [Google Scholar]
- Agoston-Coldea, L.; Kouaho, S.; Sacre, K.; Dossier, A.; Escoubet, B.; Chillon, S.; Laissy, J.P.; Rouzet, F.; Kutty, S.; Extramiana, F.; et al. High mass (>18g) of late gadolinium enhancement on CMR imaging is associated with major cardiac events on long-term outcome in patients with biopsy-proven extracardiac sarcoidosis. Int. J. Cardiol. 2016, 222, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Ise, T.; Hasegawa, T.; Morita, Y.; Yamada, N.; Funada, A.; Takahama, H.; Amaki, M.; Kanzaki, H.; Okamura, H.; Kamakura, S.; et al. Extensive late gadolinium enhancement on cardiovascular magnetic resonance predicts adverse outcomes and lack of improvement in LV function after steroid therapy in cardiac sarcoidosis. Heart 2014, 100, 1165–1172. [Google Scholar] [CrossRef] [PubMed]
- Smedema, J.P.; van Geuns, R.J.; Ector, J.; Heidbuchel, H.; Ainslie, G.; Crijns, H.J.G.M. Right ventricular involvement and the extent of left ventricular enhancement with magnetic resonance predict adverse outcome in pulmonary sarcoidosis. ESC Heart Fail. 2018, 5, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Crawford, T.; Mueller, G.; Sarsam, S.; Prasitdumrong, H.; Chaiyen, N.; Gu, X.; Schuller, J.; Kron, J.; Nour, K.A.; Cheng, A.; et al. Magnetic resonance imaging for identifying patients with cardiac sarcoidosis and preserved or mildly reduced left ventricular function at risk of ventricular arrhythmias. Circ. Arrhythm. Electrophysiol. 2014, 7, 1109–1115. [Google Scholar] [CrossRef]
- Kumar, S.; Barbhaiya, C.; Nagashima, K.; Choi, E.K.; Epstein, L.M.; John, R.M.; Maytin, M.; Albert, S.M.; Miller, A.L.; Koplan, B.A. Ventricular tachycardia in cardiac sarcoidosis: Characterization of ventricular substrate and outcomes of catheter ablation. Circ. Arrhythm. Electrophysiol. 2015, 8, 87–93. [Google Scholar] [CrossRef]
- Malik, A.H.; Aronow, W.S. Prevention of Recurrent Ventricular Tachycardia in Patients With Implantable Cardioverter Defibrillators-A Network Meta-analysis. Am. J. Ther. 2019, 26, e469–e480. [Google Scholar] [CrossRef]
- Wijetunga, M.; Rockson, S. Myocarditis in systemic lupus erythematosus. Am. J. Med. 2002, 113, 419–423. [Google Scholar] [CrossRef]
- Zhang, L.; Zhu, Y.L.; Li, M.T.; Gao, N.; You, X.; Wu, Q.J.; Su, J.M.; Shen, M.; Zhao, L.D.; Liu, J.J. Lupus myocarditis: A case-control study from China. Chin. Med. J. 2015, 128, 2588–2594. [Google Scholar] [CrossRef]
- Barnado, A.; Kamen, D.L. Myocarditis successfully treated with intravenous immunoglobulin in a patient with systemic lupus erythematous and myositis. Am. J. Med. Sci. 2014, 347, 256–257. [Google Scholar] [CrossRef] [PubMed]
- Tariq, S.; Garg, A.; Gass, A.; Aronow, W.S. Myocarditis due to systemic lupus erythematosus associated with cardiogenic shock. Arch. Med. Sci. 2018, 14, 460–462. [Google Scholar] [CrossRef] [PubMed]
- Raffeiner, B.; Botsios, C.; Dinarello, C.; Ometto, F.; Punzi, L.; Ramonda, R. Adult-onset Still’s disease with myocarditis successfully treated with the interleukin-1 receptor antagonist anakinra. Joint Bone Spine 2011, 78, 100–101. [Google Scholar] [CrossRef] [PubMed]
- Farrah, T.E.; Basu, N.; Dweck, M.; Fayad, Z.A.; Dhaun, N. Advances in Therapies and Imaging for Systemic Vasculitis. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1520–1541. [Google Scholar] [CrossRef] [PubMed]
- Stack, J.; McLaughlin, P.; Sinnot, C. Successful control of scleroderma myocarditis using a combination of cyclophosphamide and methylprednisolone. Scand J. Rheumatol. 2010, 39, 349–350. [Google Scholar] [CrossRef] [PubMed]
- Antoniades, L.; Sfikakis, P.P.; Mavrikakis, M. Glucocorticoid effects on myocardial performance in patients with systemic sclerosis. Clin. Exp. Rheumatol. 2001, 19, 431–437. [Google Scholar]
| Spatial Resolution | RV Assessment | Radiation | Availability | Cost | |
|---|---|---|---|---|---|
| Echo | +++ | + | _ | +++ | + |
| PET | + | + | +++ | + | +++ |
| CMR | +++ | +++ | _ | ++ | ++ |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mavrogeni, S.I.; Markousis-Mavrogenis, G.; Aggeli, C.; Tousoulis, D.; Kitas, G.D.; Kolovou, G.; Iliodromitis, E.K.; Sfikakis, P.P. Arrhythmogenic Inflammatory Cardiomyopathy in Autoimmune Rheumatic Diseases: A Challenge for Cardio-Rheumatology. Diagnostics 2019, 9, 217. https://doi.org/10.3390/diagnostics9040217
Mavrogeni SI, Markousis-Mavrogenis G, Aggeli C, Tousoulis D, Kitas GD, Kolovou G, Iliodromitis EK, Sfikakis PP. Arrhythmogenic Inflammatory Cardiomyopathy in Autoimmune Rheumatic Diseases: A Challenge for Cardio-Rheumatology. Diagnostics. 2019; 9(4):217. https://doi.org/10.3390/diagnostics9040217
Chicago/Turabian StyleMavrogeni, Sophie I., George Markousis-Mavrogenis, Constantina Aggeli, Dimitris Tousoulis, George D. Kitas, Genovefa Kolovou, Efstathios K. Iliodromitis, and Petros P. Sfikakis. 2019. "Arrhythmogenic Inflammatory Cardiomyopathy in Autoimmune Rheumatic Diseases: A Challenge for Cardio-Rheumatology" Diagnostics 9, no. 4: 217. https://doi.org/10.3390/diagnostics9040217
APA StyleMavrogeni, S. I., Markousis-Mavrogenis, G., Aggeli, C., Tousoulis, D., Kitas, G. D., Kolovou, G., Iliodromitis, E. K., & Sfikakis, P. P. (2019). Arrhythmogenic Inflammatory Cardiomyopathy in Autoimmune Rheumatic Diseases: A Challenge for Cardio-Rheumatology. Diagnostics, 9(4), 217. https://doi.org/10.3390/diagnostics9040217