Correlation between Spot Sign and Intracranial Hemorrhage Expansion on Dual-Phase CT Angiography
Abstract
1. Introduction
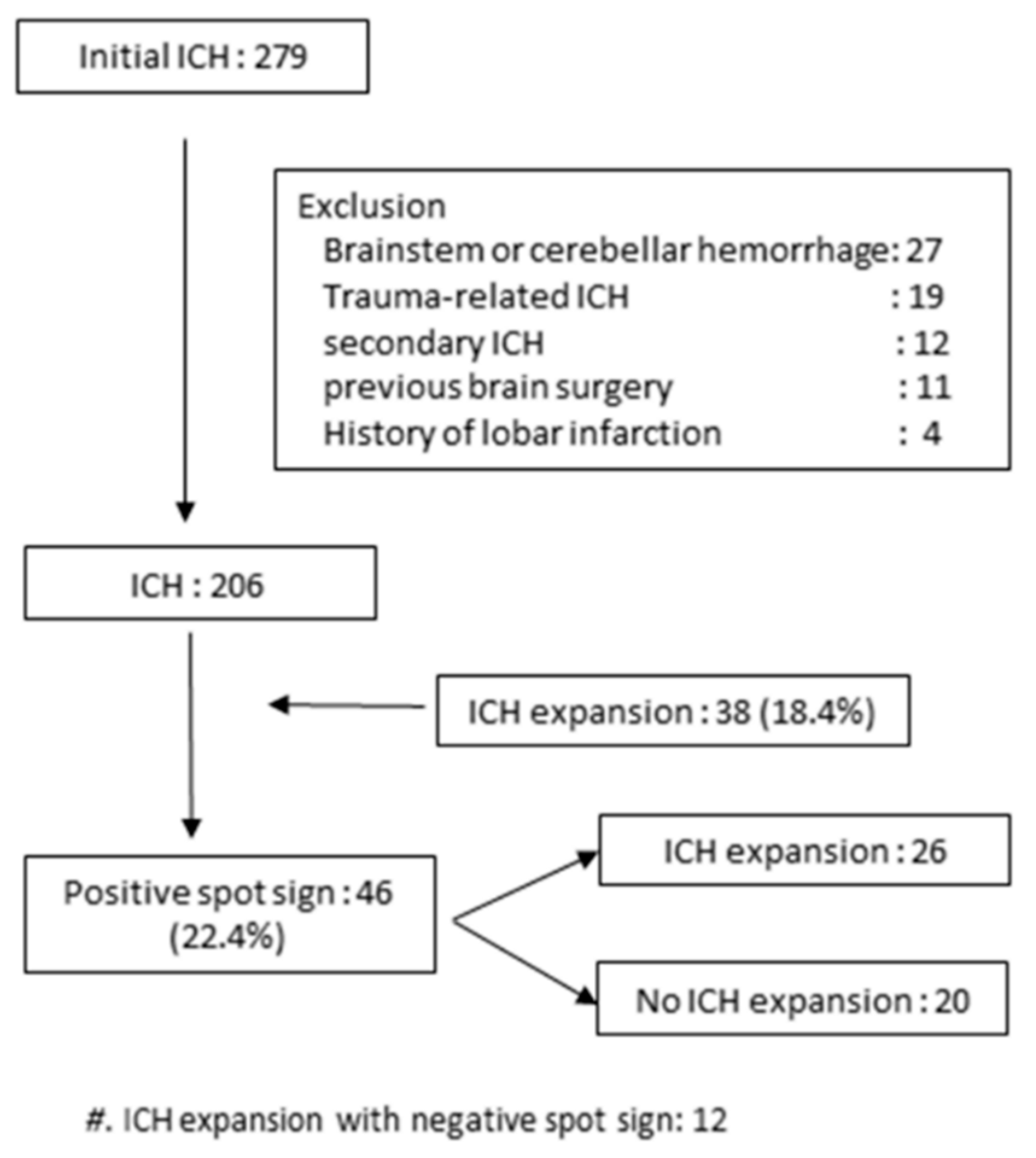
2. Methods
2.1. Patients
2.2. CT Acquisition
2.3. Clinical Data
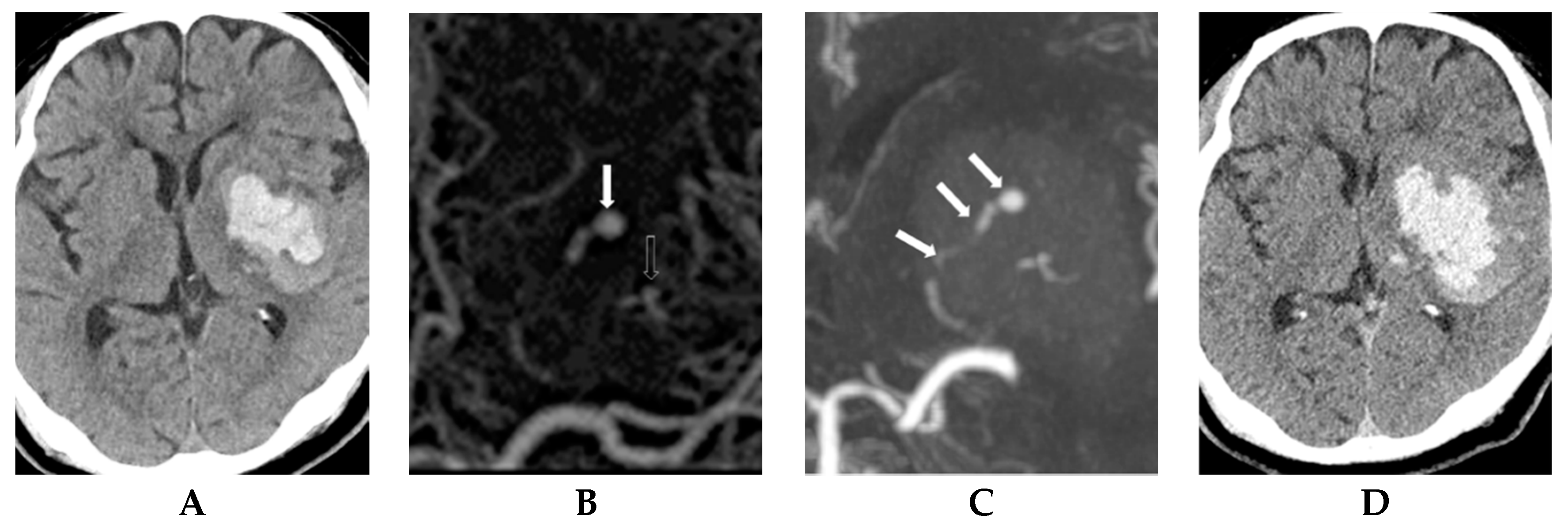
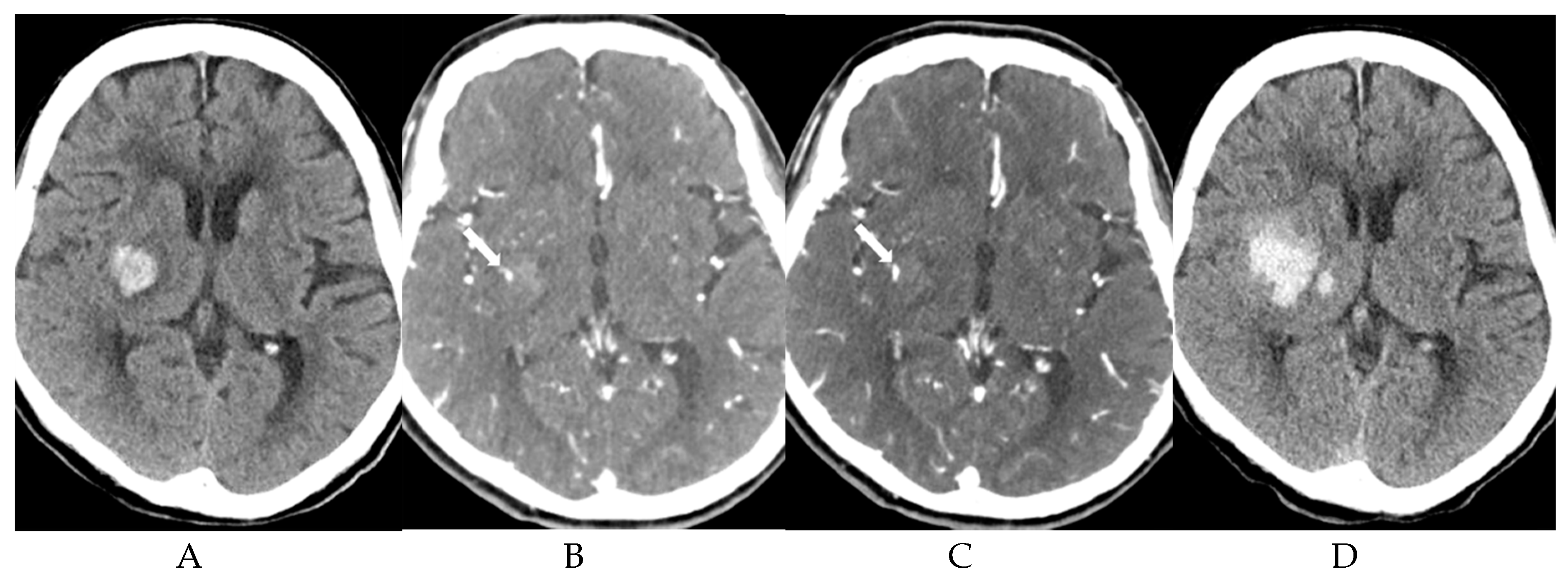
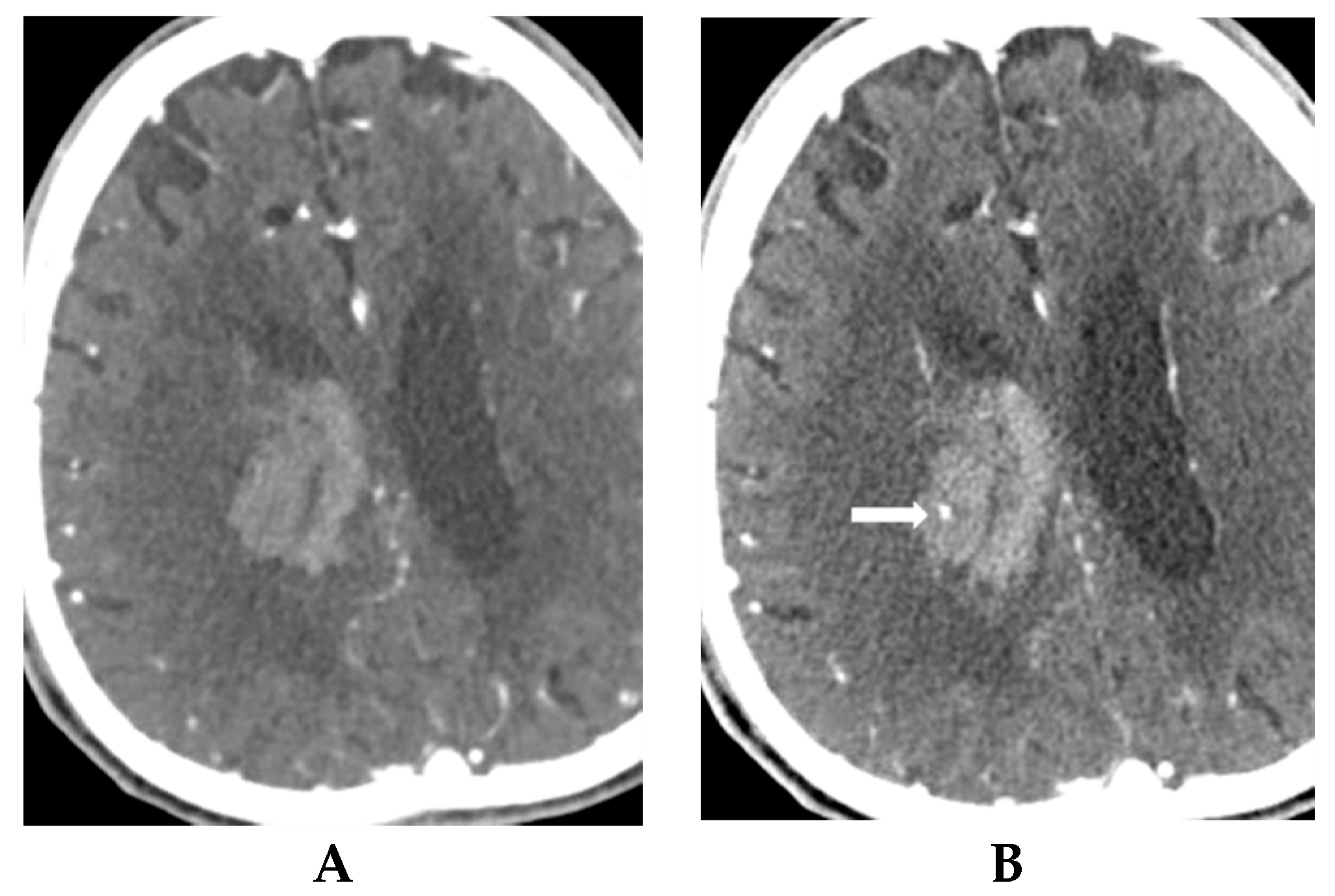
2.4. Image Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Peng, W.J.; Reis, C.; Reis, H.; Zhang, J.; Yang, J. Predictive Value of CTA Spot Sign on Hematoma Expansion in Intracerebral Hemorrhage Patients. BioMed Res. Int. 2017. [Google Scholar] [CrossRef] [PubMed]
- Wada, R.; Aviv, R.I.; Fox, A.J.; Sahlas, D.J.; Gladstone, D.J.; Tomlinson, G.; Symons, S.P. CT angiography “spot sign” predicts hematoma expansion in acute intracerebral hemorrhage. Stroke 2007, 38, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Broderick, J.P.; Brott, T.G.; Duldner, J.E.; Tomsick, T.; Huster, G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke 1993, 24, 987–993. [Google Scholar] [CrossRef] [PubMed]
- Han, J.H.; Lee, J.M.; Koh, E.J.; Choi, H.Y. The spot sign predicts hematoma expansion, outcome, and mortality in patients with primary intracerebral hemorrhage. J. Korean Neurosurg. Soc. 2014, 56, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zhang, J.; Yang, K.; Wang, Q.; Xu, B.; Chen, X. Accuracy of spot sign in predicting hematoma expansion and clinical outcome: A meta-analysis. Medicine 2018. [Google Scholar] [CrossRef]
- Menon, B.K.; d’Esterre, C.D.; Qazi, E.M.; Almekhlafi, M.; Hahn, L.; Demchuk, A.M.; Goyal, M. Multiphase CT Angiography: A New Tool for the Imaging Triage of Patients with Acute Ischemic Stroke. Radiology 2015, 275, 510–520. [Google Scholar] [CrossRef]
- Koculym, A.; Huynh, T.J.; Jakubovic, R.; Zhang, L.; Aviv, R.I. CT perfusion spot sign improves sensitivity for prediction of outcome compared with CTA and postcontrast CT. Am. J. Neuroradiol. 2013, 34, 965–970. [Google Scholar] [CrossRef]
- Yang, C.Y.; Chen, Y.F.; Lee, C.W.; Huang, A.; Shen, Y.; Wei, C.; Liu, H.M. Multiphase CT angiography versus single-phase CT angiography: Comparison of image quality and radiation dose. Am. J. Neuroradiol. 2008, 29, 1288–1295. [Google Scholar] [CrossRef]
- Sun, S.J.; Gao, P.Y.; Sui, B.B.; Hou, X.Y.; Lin, Y.; Xue, J.; Zhai, R.Y. “Dynamic spot sign” on CT perfusion source images predicts haematoma expansion in acute intracerebral haemorrhage. Eur. Radiol. 2013, 23, 1846–1854. [Google Scholar] [CrossRef]
- Morotti, A.; Romero, J.M.; Jessel, M.J.; Brouwers, H.B.; Gupta, R.; Schwab, K.; Vashkevich, A.; Ayres, A.; Anderson, C.D.; Gurol, M.E.; et al. Effect of CTA Tube Current on Spot Sign Detection and Accuracy for Prediction of Intracerebral Hemorrhage Expansion. Am. J. Neuroradiol. 2016, 37, 1781–1786. [Google Scholar] [CrossRef]
- Morotti, A.; Boulouis, G.; Charidimou, A.; Schwab, K.; Kourkoulis, C.; Anderson, C.D.; Gurol, M.E.; Viswanathan, A.; Romero, J.M.; Greenberg, S.M.; et al. Integration of Computed Tomographic Angiography Spot Sign and Noncontrast Computed Tomographic Hypodensities to Predict Hematoma Expansion. Stroke 2018, 49, 2067–2073. [Google Scholar] [CrossRef] [PubMed]
- Kothari, R.U.; Brott, T.; Broderick, J.P.; Barsan, W.G.; Sauerbeck, L.R.; Zuccarello, M.; Khoury, J. The ABCs of measuring intracerebral hemorrhage volumes. Stroke 1996, 27, 1304–1305. [Google Scholar] [CrossRef] [PubMed]
- Mayer, S.A.; Brun, N.C.; Begtrup, K.; Broderick, J.; Davis, S.; Diringer, M.N.; Skolnick, B.E.; Steiner, T. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N. Engl. J. Med. 2008, 358, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.F.; Meeker, M.; Holland, M.C. Acute traumatic intraparenchymal hemorrhage: Risk factors for progression in the early post-injury period. Neurosurgery 2006, 58, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, H.B.; Greenberg, S.M. Hematoma expansion following acute intracerebral hemorrhage. Cerebrovasc. Dis. 2013, 35, 195–201. [Google Scholar] [CrossRef]
- Davis, S.M.; Broderick, J.; Hennerici, M.; Brun, N.C.; Diringer, M.N.; Mayer, S.A.; Begtrup, K.; Steiner, T. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology 2006, 66, 1175–1181. [Google Scholar] [CrossRef]
- Brott, T.; Broderick, J.; Kothari, R.; Barsan, W.; Tomsick, T.; Sauerbeck, L.; Spilker, J.; Duldner, J.; Khoury, J. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke 1997, 28, 1–5. [Google Scholar] [CrossRef]
- Chen, S.; Zhao, B.; Wang, W.; Shi, L.; Reis, C.; Zhang, J. Predictors of hematoma expansion predictors after intracerebral hemorrhage. Oncotarget 2017, 8, 89348–89363. [Google Scholar] [CrossRef]
- Park, B.K.; Kwak, H.S.; Chung, G.H.; Hwang, S.B. Diagnostic value of swirl sign on noncontrast computed tomography and spot sign on computed tomographic angiography to predict intracranial hemorrhage expansion. Clin. Neurol. Neurosurg. 2019, 182, 130–135. [Google Scholar] [CrossRef]
- Sporns, P.B.; Kemmling, A.; Schwake, M.; Minnerup, J.; Nawabi, J.; Broocks, G.; Wildgruber, M.; Fiehler, J.; Heindel, W.; Hanning, U. Triage of 5 Noncontrast Computed Tomography Markers and Spot Sign for Outcome Prediction After Intracerebral Hemorrhage. Stroke 2018, 49, 2317–2322. [Google Scholar] [CrossRef]
- Sporns, P.B.; Schwake, M.; Kemmling, A.; Minnerup, J.; Schwindt, W.; Niederstadt, T.; Schmidt, R.; Hanning, U. Comparison of Spot Sign, Blend Sign and Black Hole Sign for Outcome Prediction in Patients with Intracerebral Hemorrhage. J. Stroke 2017, 19, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Sporns, P.B.; Schwake, M.; Schmidt, R.; Kemmling, A.; Minnerup, J.; Schwindt, W.; Cnyrim, C.; Zoubi, T.; Heindel, W.; Niederstadt, T.; et al. Computed Tomographic Blend Sign Is Associated With Computed Tomographic Angiography Spot Sign and Predicts Secondary Neurological Deterioration After Intracerebral Hemorrhage. Stroke 2017, 48, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Luna, D.; Coscojuela, P.; Rodriguez-Villatoro, N.; Juega, J.M.; Boned, S.; Muchada, M.; Pagola, J.; Rubiera, M.; Ribo, M.; Tomasello, A.; et al. Multiphase CT Angiography Improves Prediction of Intracerebral Hemorrhage Expansion. Radiology 2017, 285, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Shin, N.Y.; Kim, K.E.; Park, M.; Kim, Y.D.; Kim, D.J.; Ahn, S.J.; Heo, J.H.; Lee, S.K. Dual-phase CT collateral score: A predictor of clinical outcome in patients with acute ischemic stroke. PLoS ONE 2014. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.L.; Kosior, J.C.; Gladstone, D.J.; Hopyan, J.J.; Symons, S.P.; Romero, F.; Dzialowski, I.; Roy, J.; Demchuk, A.M.; Aviv, R.I. Defining the CT angiography “spot sign” in primary intracerebral hemorrhage. Can. J. Neurol. Sci. 2009, 36, 456–461. [Google Scholar] [CrossRef] [PubMed]
| ICH Expansion (n = 38) | No ICH Expansion (n = 168) | p | |
|---|---|---|---|
| Age | 64.7 ± 14.3 | 66.5 ± 12.9 | 0.448 |
| Male (%) | 21 (55.3) | 112 (67.2) | 0.166 |
| Hypertension (%) | 18 (47.4) | 79 (47.0) | 0.965 |
| Diabetes (%) | 11 (28.9) | 58 (34.5) | 0.510 |
| Chronic renal disease (%) | 3 (7.9) | 9 (5.4) | 0.555 |
| Liver disease (%) | 6 (15.8) | 18 (10.7) | 0.377 |
| Cardiac disease (%) | 5 (13.5) | 31 (18.5) | 0.466 |
| Current smoking, (%) | 6 (15.8) | 39 (23.2) | 0.320 |
| Alcoholic, (%) | 15 (39.5) | 51 (30.4) | 0.279 |
| Antiplatelet drug (%) | 5 (13.5) | 17 (10.1) | 0.542 |
| Anticoagulant drug (%) | 3 (7.9) | 8 (4.8) | 0.445 |
| ICH volume | 27.6 ± 23.9 | 23.2 ± 14.8 | 0.147 |
| IVH presence, (%) | 16 (42.1) | 81 (48.2) | 0.497 |
| Spot Sign | ICH Expansion (n = 26) | No ICH Expansion (n = 20) | p |
|---|---|---|---|
| First phase visualization | 25 (96.2) | 10 (50.0) | <0.001 |
| Increased size on second phase | 25 (96.2) | 10 (50.0) | <0.001 |
| First visualization on second phase | 1 (3.8) | 10 (50.0) | <0.001 |
| Linear pattern | 14 (53.8) | 9 (45.0) | 0.675 |
| Dot-like pattern | 12 (52.6) | 11 (55.0) | 0.675 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Goo, J.H.; Kwak, H.S.; Hwang, S.B.; Chung, G.H. Correlation between Spot Sign and Intracranial Hemorrhage Expansion on Dual-Phase CT Angiography. Diagnostics 2019, 9, 215. https://doi.org/10.3390/diagnostics9040215
Kim H, Goo JH, Kwak HS, Hwang SB, Chung GH. Correlation between Spot Sign and Intracranial Hemorrhage Expansion on Dual-Phase CT Angiography. Diagnostics. 2019; 9(4):215. https://doi.org/10.3390/diagnostics9040215
Chicago/Turabian StyleKim, Hyesoo, Ja Hong Goo, Hyo Sung Kwak, Seung Bae Hwang, and Gyung Ho Chung. 2019. "Correlation between Spot Sign and Intracranial Hemorrhage Expansion on Dual-Phase CT Angiography" Diagnostics 9, no. 4: 215. https://doi.org/10.3390/diagnostics9040215
APA StyleKim, H., Goo, J. H., Kwak, H. S., Hwang, S. B., & Chung, G. H. (2019). Correlation between Spot Sign and Intracranial Hemorrhage Expansion on Dual-Phase CT Angiography. Diagnostics, 9(4), 215. https://doi.org/10.3390/diagnostics9040215





