Unexpected Increase in Benzodiazepine Prescriptions Related to the Introduction of an Electronic Prescribing Tool: Evidence from Multicenter Hospital Data
Abstract
1. Background
2. Methods
2.1. Setting, Study Population, and Design
2.2. Data Analysis
3. Results
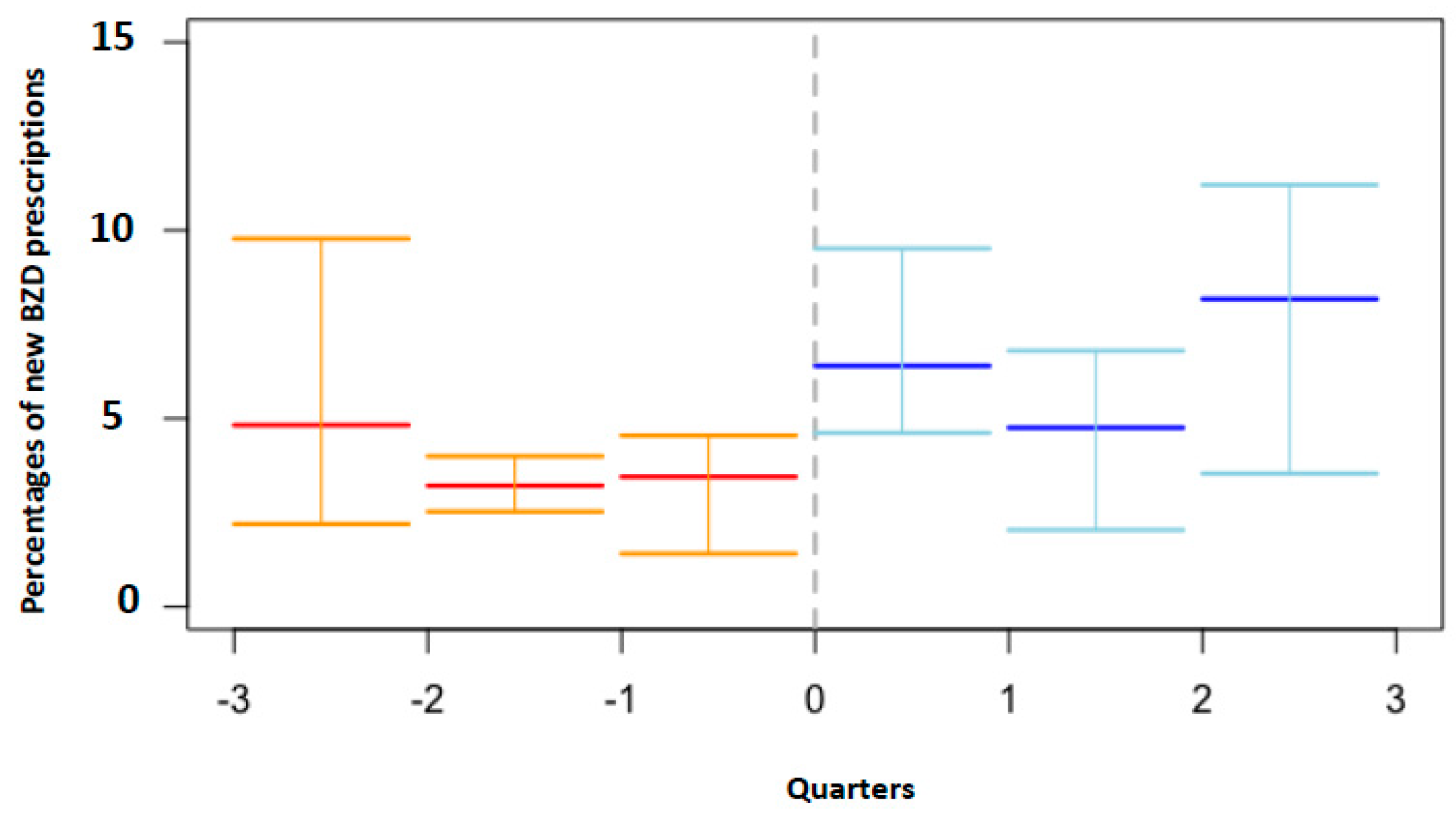
3.1. Descriptive and Interrupted Time Series Analyses
3.2. Fixed-Effects Regression Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| EOC | Ente Ospedaliero Cantonale |
| BZDs | benzodiazepines |
| e-prescribing | electronic prescribing systems |
| FE | fixed effect |
References
- van Doormaal, J.E.; van den Bemt, P.M.; Zaal, R.J.; Egberts, A.G.; Lenderink, B.W.; Kosterink, J.G.; Haaijier-Ruskamp, F.M. The influence that electronic prescribing has on medication errors and preventable adverse drug events: an interrupted time-series study. J. Am. Med. Inform. Assoc. 2009, 16, 816–825. [Google Scholar] [CrossRef]
- Franklin, B.D.; Puaar, S. What is the impact of introducing inpatient electronic prescribing on prescribing errors? A naturalistic stepped wedge study in an English teaching hospital. Health Inform. J. 2019, 460458219833112. [Google Scholar] [CrossRef]
- Ammenwerth, E.; Schnell-Inderst, P.; Machan, C.; Siebert, U. The Effect of Electronic Prescribing on Medication Errors and Adverse Drug Events: A Systematic Review. J. Am. Med. Inform. Assoc. 2008, 15, 585–600. [Google Scholar] [CrossRef]
- Wolfstadt, J.I.; Gurwitz, J.H.; Field, T.S.; Lee, M.; Kalkar, S.; Wu, W.; Rochon, P.A. The Effect of Computerized Physician Order Entry with Clinical Decision Support on the Rates of Adverse Drug Events: A Systematic Review. J. Gen. Intern. Med. 2008, 23, 451–458. [Google Scholar] [CrossRef]
- Chaudhry, B.; Wang, J.; Wu, S.; Maglione, M.; Mojica, W.; Roth, E.; Morton, S.C.; Shekelle, P.G. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann. Intern. Med. 2006, 144, 742–752. [Google Scholar] [CrossRef]
- Shamliyan, T.A.; Duval, S.; Du, J.; Kane, R.L. Just what the doctor ordered. Review of the evidence of the impact of computerized physician order entry system on medication errors. Health Serv. Res. 2008, 43, 32–53. [Google Scholar] [CrossRef]
- Radley, D.C.; Wasserman, M.R.; Olsho, L.E.; Shoemaker, S.J.; Spranca, M.D.; Bradshaw, B. Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems. J. Am. Med. Inform. Assoc. 2013, 20, 470–476. [Google Scholar] [CrossRef]
- Di Pentima, M.C.; Chan, S.; Eppes, S.C.; Klein, J.D. Antimicrobial prescription errors in hospitalized children: role of antimicrobial stewardshipprogram in detection and intervention. Clin. Pediatr. (Phila.) 2009, 48, 505–512. [Google Scholar] [CrossRef]
- Koppel, R.; Metlay, J.P.; Cohen, A.; Abaluck, B.; Localio, A.R.; Kimmel, S.E.; Strom, B.L. Role of Computerized Physician Order Entry Systems in Facilitating Medication Errors. JAMA 2005, 293, 1197. [Google Scholar] [CrossRef]
- Han, Y.Y.; Carcillo, J.A.; Venkataraman, S.T.; Clark, R.S.; Watson, R.S.; Nguyen, T.C.; Bayir, H.; Orr, R.A. Unexpected Increased Mortality After Implementation of a Commercially Sold Computerized Physician Order Entry System. Pediatrics 2005, 116, 1506–1512. [Google Scholar] [CrossRef]
- Ahmed, Z.; Barber, N.; Jani, Y.; Garfield, S.; Franklin, B.D.; Information, P.E.K.F.C. Economic impact of electronic prescribing in the hospital setting: A systematic review. Int. J. Med. Inform. 2016, 88, 1–7. [Google Scholar] [CrossRef]
- Frail, C.K.; Kline, M.; Snyder, M.E. Patient perceptions of e-prescribing and its impact on their relationships with providers: a qualitative analysis. J. Am. Pharm. Assoc. 2014, 54, 630–633. [Google Scholar] [CrossRef]
- Price, J.; Man, S.L.; Bartlett, S.; Taylor, K.; Dinwoodie, M.; Bowie, P. Repeat prescribing of medications: A system-centred risk management model for primary care organisations. J. Eval. Clin. Pract. 2017, 23, 779–796. [Google Scholar] [CrossRef]
- Del Giorno, R.; Greco, A.; Zasa, A.; Luca, C.; Michela, P.; Alessandro, C. Combining prescription monitoring, benchmarking, and educational interventions to reduce benzodiazepine prescriptions among internal medicine inpatients; a multicenter before and after study in a network of Swiss Public Hospitals. Postgrad Med. 2018, 130, 627–636. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2017, 335, 806–808. [Google Scholar] [CrossRef]
- Available online: http://www.kofam.ch/it/domanda-e-procedura/progetti-non-soggetti-allobbligodi autorizzazione/ (accessed on 15 June 2019).
- Wooldridge, J.M. Econometric Analysis of Cross Section and Panel Data; MIT Press: Cambridge, MA, USA, 2010. [Google Scholar]
- Porterfield, A.; Engelbert, K.; Coustasse, A. Electronic Prescribing: Improving the Efficiency and Accuracy of Prescribing in the Ambulatory Care Setting. Perspect. Heal. Inf. Manag. 2014, 11. [Google Scholar]
- Schade, C.P.; Sullivan, F.M.; De Lusignan, S.; Madeley, J. e-Prescribing, Efficiency, Quality: Lessons from the Computerization of UK Family Practice. J. Am. Med. Inform. Assoc. 2006, 13, 470–475. [Google Scholar] [CrossRef]
- Dullabh, P.M.; Sondheimer, N.K.; Katsh, E.; Evans, M.A. How Patients Can Improve the Accuracy of their Medical Records. eGEMs 2014, 2, 10. [Google Scholar] [CrossRef]
- Donyai, P.; O’Grady, K.; Jacklin, A.; Barber, N.; Franklin, B.D. The effects of electronic prescribing on the quality of prescribing. Br. J. Clin. Pharmacol. 2008, 65, 230–237. [Google Scholar] [CrossRef]
- Pérez, T.; Moriarty, F.; Wallace, E.; McDowell, R.; Redmond, P.; Fahey, T. Prevalence of potentially inappropriate prescribing in older people in primary care and its association with hospital admission: longitudinal study. BMJ 2018, 363, k4524. [Google Scholar] [CrossRef]
- Dell’Osso, B.; Lader, M. Do benzodiazepines still deserve a major role in the treatment of psychiatric disorders? A critical reappraisal. Eur. Psychiatry 2013, 28, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Hartikainen, S.; Lönnroos, E.; Louhivuori, K. Medication as a risk factor for falls: critical systematic review. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2007, 62, 1172–1181. [Google Scholar] [CrossRef] [PubMed]
- Glass, J.; Lanctot, K.L.; Herrmann, N.; A Sproule, B.; E Busto, U. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 2005, 331, 1169. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.M.; Marshall, R.; Masci, C.; Coyne, J.C. Physicians’ Perspectives on Prescribing Benzodiazepines for Older Adults: A Qualitative Study. J. Gen. Intern. Med. 2007, 22, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Schedlbauer, A.; Prasad, V.; Mulvaney, C.; Phansalkar, S.; Stanton, W.; Avery, A.J. What Evidence Supports the Use of Computerized Alerts and Prompts to Improve Clinicians’ Prescribing Behavior? J. Am. Med. Inform. Assoc. 2009, 16, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Riedmann, D.; Jung, M.; O Hackl, W.; Ammenwerth, E. How to improve the delivery of medication alerts within computerized physician order entry systems: an international Delphi study. J. Am. Med. Inform. Assoc. 2011, 18, 760–766. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Malte, C.A.; Berger, D.; Saxon, A.J.; Hagedorn, H.J.; Achtmeyer, C.E.; Mariano, A.J.; Hawkins, E.J. Electronic Medical Record Alert Associated With Reduced Opioid and Benzodiazepine Coprescribing in High-risk Veteran Patients. Med. Care 2018, 56, 171–178. [Google Scholar] [CrossRef]
- Avery, A.J.; Savelyich, B.S.P.; Sheikh, A.; Cantrill, J.; Morris, C.J.; Fernando, B.; Bainbridge, M.; Horsfield, P.; Teasdale, S. Identifying and establishing consensus on the most important safety features of GP computer systems: e-Delphi study. Inform. Prim. Care 2005, 13, 3–11. [Google Scholar] [CrossRef][Green Version]
- Feldstein, A.; Simon, S.R.; Schneider, J.; Krall, M.; Laferriere, D.; Smith, D.H.; Sittig, D.F.; Soumerai, S.B. How to Design Computerized Alerts to Ensure Safe Prescribing Practices. Jt. Comm. J. Qual. Saf. 2004, 30, 602–613. [Google Scholar] [CrossRef]
- Krall, M.A.; Sittig, D.F. Subjective assessment of usefulness and appropriate presentation mode of alerts and reminders in the outpatient setting. In Proceedings of the AMIA Symposium, American Medical Informatics Association, Bethesda, MD, USA, 3–7 November 2001; pp. 334–338. [Google Scholar]
- Anjum, R.L.; Copeland, S.; Rocca, E. Medical scientists and philosophers worldwide appeal to EBM to expand the notion of ‘evidence’. BMJ Evid.-Based Med. 2018, 2018, 111092. [Google Scholar] [CrossRef]

| Before e-Prescribing Implementation | |||||
| Hospital A | Hospital B | Hospital C | Hospital D | Hospital E | |
| Admissions, n | 3947 | 3206 | 2654 | 4632 | 5758 |
| Age, median IQR | 76 (62–84) | 77 (67−85) | 73 (59−82) | 77 (65-84) | 75 (61-83) |
| Age groups, n (%) (admissions) | |||||
| <70 years | 1392 (35.3) | 910 (28.4) | 1105 (41.6) | 1506 (32.5) | 2180 (37.9) |
| ≥70 years | 2555 (64.7) | 2296 (71.6) | 1549 (58.4) | 3126 (67.5) | 3578 (62.1) |
| Gender, females (%) | 50.6 | 56.7 | 47.7 | 48.2 | 50.7 |
| Case-mix (median, Q1−Q3) | 0.72 (0.53−0.93) | 0.79 (0.59−1.00) | 0.67 (0.50−0.92) | 0.71 (0−52−0.93) | 0.67 (0.48−0.92) |
| BZD at admission, n (%) | 32.6 | 29.2 | 31.3 | 30.3 | 29.4 |
| New BZD prescriptions, % | 3.8 | 5.7 | 5.7 | 3.6 | 3.3 |
| After e-Prescribing Implementation | |||||
| Admissions, n | 4182 | 1937 | 7245 | 4733 | 4926 |
| Age, median IQR | 78 (67−85) | 80 (69−86) | 75 (62−83) | 77 (66−84) | 76 (63−84) |
| Age groups, (admissions) | |||||
| <70, y, n (%) | 1235 (29.5) | 489 (25.2) | 2704 (37.3) | 1461 (30.9) | 1745 (35.4) |
| ≥70, y, n (%) | 2947 (70.5) | 1448 (74.8) | 4541 (62.7) | 3272 (69.1) | 3181 (64.6) |
| Gender, females (%) | 51.2 | 56.9 | 47.54 | 49.4 | 50.0 |
| Case-mix (median, Q1−Q3) | 0.71 (0.52−0.96) | 0.75 (0.54−1.04) | 0.74 (0.51−1.01) | 0.72 (0.51−0.99) | 0.65 (0.48−0.90) |
| BZD at admission, (%) | 33.9 | 30.5 | 31.8 | 30.9 | 28.6 |
| New BZD prescriptions, (%) | 3.4 | 7.3 | 5.3 | 2.9 | 3.2 |
| Hospital A | β Coefficient | Standard Error | p-Value |
|---|---|---|---|
| Baseline level (β0) | 0.005 | 0.007 | 0.495 |
| Baseline trend of BZD prescriptions before e-prescribing (β1) | −0.002 | 0.004 | <0.001 * |
| Change in level at the implementation (β2) | 0.028 | 0.009 | <0.001 * |
| Trend change after the implementation (β3) | 0.002 | 0.0005 | <0.001 * |
| Hospital B | |||
| Baseline level (β0) | 0.047 | 0.005 | <0.001 * |
| Baseline trend of BZD prescriptions before e-prescribing (β1) | −0.0008 | 0.026 * | |
| Change in level at the implementation (β2) | −0.0389 | 0.0215 | 0.076 |
| Trend change after the implementation (β3) | 0.004 | 0.001 | <0.001 * |
| Hospital C | |||
| Baseline level (β0) | 0.097 | 0.024 | <0.001 * |
| Baseline trend of BZD prescriptions before e-prescribing (β1) | 0.001 | 0.001 | 0.096 |
| Change in level at the implementation (β2) | −0.038 | 0.025 | 0.017 * |
| Trend change after the implementation (β3) | −0.002 | 0.001 | 0.028 * |
| Hospital D | |||
| Baseline level (β0) | 0.029 | 0.005 | <0.001 * |
| Baseline trend of BZD prescriptions before e-prescribing (β1) | −0.0004 | 0.0003 | 0.204 |
| Change in level at the implementation (β2) | 0.007 | 0.007 | 0.336 |
| Trend change after the implementation (β3) | −0.000025 | 0.0004 | 0.958 |
| Hospital E | |||
| Baseline level (β0) | 0.037 | 0.004 | <0.001 * |
| Baseline trend of BZD prescriptions before e-prescribing (β1) | 0.0002 | 0.0002 | 0.316 |
| Change in level at the implementation (β2) | −0.0008 | 0.007 | 0.902 |
| Trend change after the implementation (β3) | −0.0005 | 0.0004 | 0.206 |
| Fixed Effect Model 1 | ||||||||||
| Entire sample | <70 years | ≥70 years | Males | Females | ||||||
| Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | |
| Effect of e-prescribing on new BZD prescriptions | 0.015 (0.005) | <0.001 * | 0.007 (0.010) | 0.459 | 0.016 (0.006) | 0.010 * | 0.023 (0.007) | <0.001 * | 0.018 (0.007) | 0.010 * |
| Intercept | 0.035 | 0.056 | 0.027 | 0.035 | 0.031 | |||||
| R2 | 0.0279 | 0.002 | 0.028 | 0.0405 | 0.0297 | |||||
| Fixed Effect Model 2 | ||||||||||
| Entire sample | <70 years | ≥70 years | Males | Females | ||||||
| Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | |
| Effect of e-prescribing on new BZD prescriptions | 0.014 (0.008) | 0.007 | 0.089 (0.014) | 0.527 | 0.028 (0.007) | <0.001 * | 0.020 (0.009) | 0.035 * | 0.004 (0.009) | 0.891 |
| Case mix × new BZD prescriptions | −0.004 (0.005) | 0.363 | −0.008 (0.006) | 0.202 | 0.003 (0.004) | 0.477 | −0.003 (0.004) | 0.544 | −0.008 (0.004) | 0.006 |
| e-prescribing on New BZD prescriptions × case mix | 0.006 (0.005) | 0.251 | 0.006 (0.008) | 0.448 | −0.003 (0.004) | −0.002 (0.005) | 0.978 | 0.008 (0.005) | 0.063 | |
| Intercept | 0.038 | 0.066 | 0.022 | 0.035 | 0.045 | |||||
| R2 | 0.068 | 0.021 | 0.082 | 0.036 | 0.031 | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Giorno, R.; Schneiders, C.; Stefanelli, K.; Ceschi, A.; Gyoerik-Lora, S.; Aletto, I.; Gabutti, L. Unexpected Increase in Benzodiazepine Prescriptions Related to the Introduction of an Electronic Prescribing Tool: Evidence from Multicenter Hospital Data. Diagnostics 2019, 9, 190. https://doi.org/10.3390/diagnostics9040190
Del Giorno R, Schneiders C, Stefanelli K, Ceschi A, Gyoerik-Lora S, Aletto I, Gabutti L. Unexpected Increase in Benzodiazepine Prescriptions Related to the Introduction of an Electronic Prescribing Tool: Evidence from Multicenter Hospital Data. Diagnostics. 2019; 9(4):190. https://doi.org/10.3390/diagnostics9040190
Chicago/Turabian StyleDel Giorno, Rosaria, Carmen Schneiders, Kevyn Stefanelli, Alessandro Ceschi, Sandor Gyoerik-Lora, Irene Aletto, and Luca Gabutti. 2019. "Unexpected Increase in Benzodiazepine Prescriptions Related to the Introduction of an Electronic Prescribing Tool: Evidence from Multicenter Hospital Data" Diagnostics 9, no. 4: 190. https://doi.org/10.3390/diagnostics9040190
APA StyleDel Giorno, R., Schneiders, C., Stefanelli, K., Ceschi, A., Gyoerik-Lora, S., Aletto, I., & Gabutti, L. (2019). Unexpected Increase in Benzodiazepine Prescriptions Related to the Introduction of an Electronic Prescribing Tool: Evidence from Multicenter Hospital Data. Diagnostics, 9(4), 190. https://doi.org/10.3390/diagnostics9040190





