Association of Non-Carious Cervical Lesions with Oral Hygiene Habits and Dynamic Occlusal Parameters
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recordings and Measurements
2.2. T-scan Analysis
2.3. Statistical Analysis
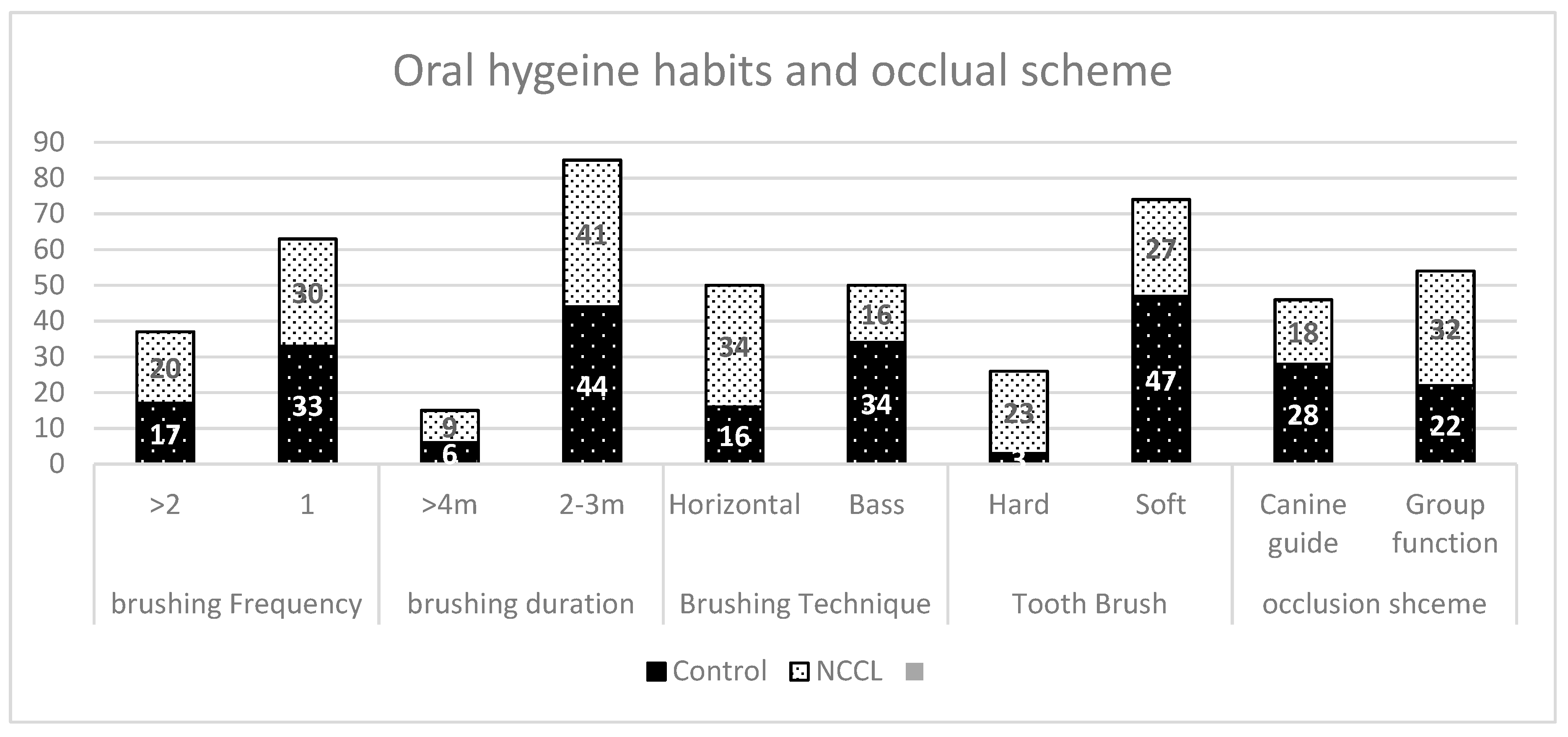
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Aw, T.C.; Lepe, X.; Johnson, G.H.; Mancl, L. Characteristics of noncarious cervical lesions: A clinical investigation. J. Am. Dent. Assoc. 2002, 133, 725–733. [Google Scholar] [CrossRef]
- Bartlett, D.W.; Shah, P. A critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J. Dent. Res. 2006, 85, 306–312. [Google Scholar] [CrossRef]
- Borcic, J.; Anic, I.; Urek, M.M.; Ferreri, S. The prevalence of non-carious cervical lesions in permanent dentition. J. Oral Rehabil. 2004, 31, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Bergstrom, J.; Eliasson, S. Cervical abrasion in relation to toothbrushing and periodontal health. Scand. J. Dent. Res. 1988, 96, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Hand, J.S.; Hunt, R.J.; Reinhardt, J.W. The prevalence and treatment implications of cervical abrasion in the elderly. Gerodontics 1986, 2, 167–170. [Google Scholar]
- Oginni, A.O.; Olusile, A.O.; Udoye, C.I. Non-carious cervical lesions in a Nigerian population: Abrasion or abfraction? Int. Dent. J. 2003, 53, 275–279. [Google Scholar] [PubMed]
- Michael, J.A.; Townsend, G.C.; Greenwood, L.F.; Kaidonis, J.A. Abfraction: Separating fact from fiction. Aust. Dent. J. 2009, 54, 2–8. [Google Scholar] [CrossRef]
- Nascimento, M.M.; Gordan, V.V.; Qvist, V.; Bader, J.D.; Rindal, D.B.; Williams, O.D.; Gewartowski, D.; Fellows, J.L.; Litaker, M.S.; Gilbert, G.H.; et al. Restoration of noncarious tooth defects by dentists in The Dental Practice-Based Research Network. J. Am. Dent. Assoc. 2011, 142, 1368–1375. [Google Scholar] [CrossRef] [PubMed]
- Grippo, J.O.; Simring, M.; Coleman, T.A. Abfraction, abrasion, biocorrosion, and the enigma of noncarious cervical lesions: A 20-year perspective. J. Esthet. Restor. Dent. 2012, 24, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Nayyer, M.; Zahid, S.; Hassan, S.H.; Mian, S.A.; Mehmood, S.; Khan, H.A.; Kaleem, M.; Zafar, M.S.; Khan, A.S. Comparative abrasive wear resistance and surface analysis of dental resin-based materials. Eur. J. Dent. 2018, 12, 57–66. [Google Scholar]
- Ahmed, N.; Zafar, M.S. Effects of wear on hardness and stiffness of restorative dental materials. Life Sci. J. 2014, 11, 11–18. [Google Scholar]
- Zafar, M.S. Wear behavior of various dental restorative materials. Mater. Technol. 2019, 34, 25–31. [Google Scholar] [CrossRef]
- Lussi, A.; Schlueter, N.; Rakhmatullina, E.; Ganss, C. Dental erosion—An overview with emphasis on chemical and histopathological aspects. Caries Res. 2011, 45 (Suppl. 1), 2–12. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Cai, D.; Wang, F.; He, D.; Ma, L.; Jin, Y.; Que, K. Non-carious cervical lesions (NCCLs) in a random sampling community population and the association of NCCLs with occlusive wear. J. Oral Rehabil. 2016, 43, 960–966. [Google Scholar] [CrossRef]
- Rees, J.S. The effect of variation in occlusal loading on the development of abfraction lesions: A finite element study. J. Oral Rehabil. 2002, 29, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.C.; Eakle, W.S. Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J. Prosthet. Dent. 1984, 52, 374–380. [Google Scholar] [CrossRef]
- Hammadeh, M.; Rees, J.S. The erosive susceptibility of cervical versus occlusal enamel. Eur. J. Prosthodont. Restor. Dent. 2001, 9, 13–17. [Google Scholar] [PubMed]
- Litonjua, L.A.; Bush, P.J.; Andreana, S.; Tobias, T.S.; Cohen, R.E. Effects of occlusal load on cervical lesions. J. Oral Rehabil. 2004, 31, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Wiens, J.P.; Priebe, J.W. Occlusal stability. Dent. Clin. N. Am. 2014, 58, 19–43. [Google Scholar] [CrossRef]
- Suit, S.R.; Gibbs, C.H.; Benz, S.T. Study of gliding tooth contacts during mastication. J. Periodontol. 1976, 47, 331–334. [Google Scholar] [CrossRef]
- Kuroe, T.; Itoh, H.; Caputo, A.A.; Konuma, M. Biomechanics of cervical tooth structure lesions and their restoration. Quintessence Int. (Berl. Ger. 1985) 2000, 31, 267–274. [Google Scholar]
- Dejak, B.; Mlotkowski, A.; Romanowicz, M. Finite element analysis of mechanism of cervical lesion formation in simulated molars during mastication and parafunction. J. Prosthet. Dent. 2005, 94, 520–529. [Google Scholar] [CrossRef]
- Grenness, M.J.; Tyas, M.J.; Osborn, J.E. Mapping a non-carious cervical lesion using stereoimagery and dental casts incorporating optical texture. J. Dent. 2009, 37, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Smith, B.G.; Knight, J.K. An index for measuring the wear of teeth. Br. Dent. J. 1984, 156, 435–438. [Google Scholar] [CrossRef]
- Mannerberg, F. Appearance of tooth surfaces as observed in shadowed replicas, in various age groups: In long-term studies, after tooth-brushing, in cases of erosion and after exposure to citrus fruit juice. Odontol. Rev. 1960, 11 (Suppl. 6), 1–11. [Google Scholar]
- Brandini, D.A.; de Sousa, A.L.; Trevisan, C.I.; Pinelli, L.A.; do Couto Santos, S.C.; Pedrini, D.; Panzarini, S.R. Noncarious cervical lesions and their association with toothbrushing practices: In vivo evaluation. Oper. Dent. 2011, 36, 581–589. [Google Scholar] [CrossRef]
- Bizhang, M.; Riemer, K.; Arnold, W.H.; Domin, J.; Zimmer, S. Influence of Bristle Stiffness of Manual Toothbrushes on Eroded and Sound Human Dentin—An In Vitro Study. PLoS ONE 2016, 11, e0153250. [Google Scholar] [CrossRef]
- Dyer, D.; Addy, M.; Newcombe, R.G. Studies in vitro of abrasion by different manual toothbrush heads and a standard toothpaste. J. Clin. Periodontol. 2000, 27, 99–103. [Google Scholar] [CrossRef]
- Litonjua, L.A.; Andreana, S.; Bush, P.J.; Tobias, T.S.; Cohen, R.E. Wedged cervical lesions produced by toothbrushing. Am. J. Dent. 2004, 17, 237–240. [Google Scholar] [PubMed]
- Sabrah, A.H.; Turssi, C.P.; Lippert, F.; Eckert, G.J.; Kelly, A.B.; Hara, A.T. 3D-Image analysis of the impact of toothpaste abrasivity on the progression of simulated non-carious cervical lesions. J. Dent. 2018, 73, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Lussi, A.; Schaffner, M. Progression of and risk factors for dental erosion and wedge-shaped defects over a 6-year period. Caries Res. 2000, 34, 182–187. [Google Scholar] [CrossRef]
- Kerstein, R.B.; Grundset, K. Obtaining measurable bilateral simultaneous occlusal contacts with computer-analyzed and guided occlusal adjustments. Quintessence Int. 2001, 32, 7–18. [Google Scholar]
- Ma, F.F.; Hu, X.L.; Li, J.H.; Lin, Y. Normal occlusion study: Using T-Scan III occlusal analysis system. Zhonghua Kou Qiang Yi Xue Za Zhi 2013, 48, 363–367. [Google Scholar] [PubMed]
- Lin, P.T.; Jiao, Y.; Zhao, S.J.; Wang, F.; Li, L.; Yu, F.; Tian, M.; Yu, H.H.; Chen, J.H. Occlusion and Disocclusion Time Changes in Single Unit Crowns Designed by Functional Generated Path Technique: A Randomised Clinical Trial. Sci. Rep. 2017, 7, 388. [Google Scholar] [CrossRef]
- Haralur, S.B. Digital Evaluation of Functional Occlusion Parameters and their Association with Temporomandibular Disorders. J. Clin. Diagn. Res. JCDR 2013, 7, 1772–1775. [Google Scholar] [CrossRef]
- De Las Casas, E.B.; Cornacchia, T.P.; Gouvea, P.H.; Cimini, C.A., Jr. Abfraction and anisotropy—Effects of prism orientation on stress distribution. Comput. Methods Biomech. Biomed. Eng. 2003, 6, 65–73. [Google Scholar] [CrossRef]
- Zeola, L.F.; Pereira, F.A.; Machado, A.C.; Reis, B.R.; Kaidonis, J.; Xie, Z.; Townsend, G.C.; Ranjitkar, S.; Soares, P.V. Effects of non-carious cervical lesion size, occlusal loading and restoration on biomechanical behaviour of premolar teeth. Aust. Dent. J. 2016, 61, 408–417. [Google Scholar] [CrossRef]
- Soares, P.V.; Souza, L.V.; Verissimo, C.; Zeola, L.F.; Pereira, A.G.; Santos-Filho, P.C.; Fernandes-Neto, A.J. Effect of root morphology on biomechanical behaviour of premolars associated with abfraction lesions and different loading types. J. Oral Rehabil. 2014, 41, 108–114. [Google Scholar] [CrossRef]
- Romeed, S.A.; Malik, R.; Dunne, S.M. Stress analysis of occlusal forces in canine teeth and their role in the development of non-carious cervical lesions: Abfraction. Int. J. Dent. 2012, 2012, 234845. [Google Scholar] [CrossRef]
- Brandini, D.A.; Trevisan, C.L.; Panzarini, S.R.; Pedrini, D. Clinical evaluation of the association between noncarious cervical lesions and occlusal forces. J. Prosthet. Dent. 2012, 108, 298–303. [Google Scholar] [CrossRef]
- Senawongse, P.; Pongprueksa, P.; Tagami, J. The effect of the elastic modulus of low-viscosity resins on the microleakage of Class V resin composite restorations under occlusal loading. Dent. Mater. J. 2010, 29, 324–329. [Google Scholar] [CrossRef] [PubMed]
| Variable | NCCL | ||
|---|---|---|---|
| B | SE B | β | |
| Brushing frequency | −0.029 | 0.098 | −0.028 |
| Brushing duration | 0.015 | 0.135 | 0.011 |
| Brushing technique | −0.176 | 0.100 | −0.176 |
| Tooth brush hardness | −0.427 | 0.115 | −0.375 ** |
| Occlusion scheme | 0.154 | 0.093 | 0.154 |
| R2 | 0.266 | ||
| F | 6.806 |
| Groups Score Versus | Control (s) | NCCL (s) | Pearson Correlation | p Value |
|---|---|---|---|---|
| Occlusion time | 0.516 | 0.727 | 0.455 | 0.001 ** |
| Rt Disocclusion Time | 0.642 | 1.144 | 0.661 | 0.001 ** |
| Lt Disocclusion Time | 0.686 | 1.228 | 0.642 | 0.001 ** |
| Pro Disocclusion Time | 0.655 | 1.06 | 0.534 | 0.001 ** |
| Predictor | B | SE B | OR (eB) |
|---|---|---|---|
| Initial contact | −1.055 | 0.833 | 0.348 |
| Occlusion Time | 4.253 * | 2.293 | 70.295 |
| Rt Disocclusion Time | 3.738 * | 2.197 | 42.033 |
| Lt Disocclusion Time | 5.381 * | 2.302 | 217.327 |
| Pro Disocclusion Time | 1.193 | 1.270 | 3.296 |
| Centre of Force | 1.484 | 0.957 | 4.410 |
| Tooth brush hardness | −3.110 * | 1.070 | 0.045 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haralur, S.B.; Alqahtani, A.S.; AlMazni, M.S.; Alqahtani, M.K. Association of Non-Carious Cervical Lesions with Oral Hygiene Habits and Dynamic Occlusal Parameters. Diagnostics 2019, 9, 43. https://doi.org/10.3390/diagnostics9020043
Haralur SB, Alqahtani AS, AlMazni MS, Alqahtani MK. Association of Non-Carious Cervical Lesions with Oral Hygiene Habits and Dynamic Occlusal Parameters. Diagnostics. 2019; 9(2):43. https://doi.org/10.3390/diagnostics9020043
Chicago/Turabian StyleHaralur, Satheesh B., Abdulrahman Saad Alqahtani, Mohammed Shaya AlMazni, and Mohammad Khalid Alqahtani. 2019. "Association of Non-Carious Cervical Lesions with Oral Hygiene Habits and Dynamic Occlusal Parameters" Diagnostics 9, no. 2: 43. https://doi.org/10.3390/diagnostics9020043
APA StyleHaralur, S. B., Alqahtani, A. S., AlMazni, M. S., & Alqahtani, M. K. (2019). Association of Non-Carious Cervical Lesions with Oral Hygiene Habits and Dynamic Occlusal Parameters. Diagnostics, 9(2), 43. https://doi.org/10.3390/diagnostics9020043





