The Impact of Axial CT Level Selection on Grading Trochlear Dysplasia Using Dejour Classification
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Sample Size Calculation
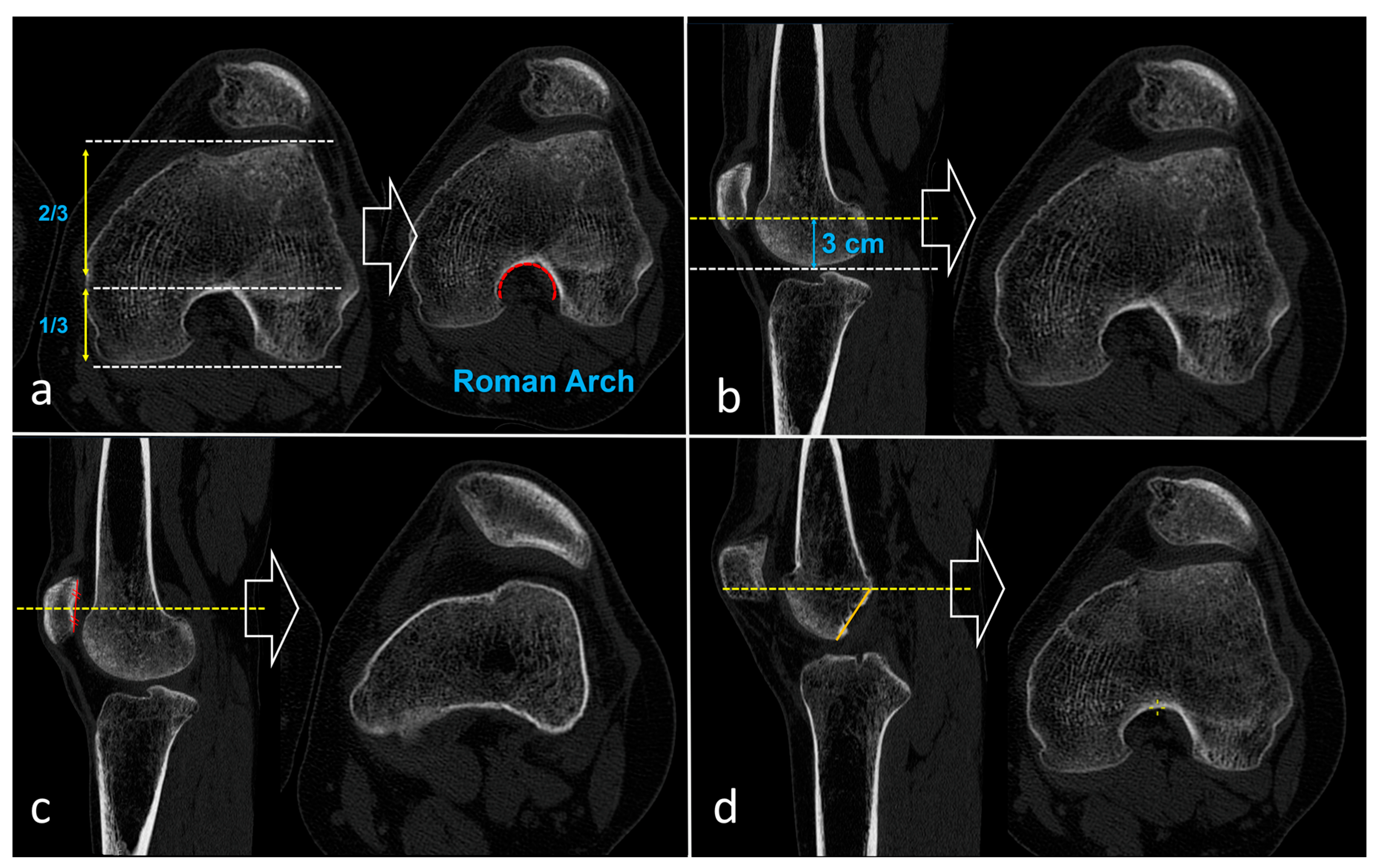
2.3. Imaging and Determination of CT Levels
2.4. Inter and Intra-Observer Reliability and Validity Assessments
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Participants
3.2. Reliability of the Dejour Classification
3.3. Diagnostic Accuracy According to Axial CT Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CI | Confidence interval |
| CT | Computed tomography |
| DICOM | Digital Imaging and Communications in Medicine |
| MPFL | Medial patellofemoral ligament |
| MRI | Magnetic resonance imaging |
| MPR | Multiplanar reconstruction |
| SD | Standard deviation |
| SPSS | Statistical Package for the Social Sciences |
| T1 | First reading/first time point |
| T2 | Second reading/second time point |
| TT–TG | Tibial tubercle–trochlear groove |
References
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and natural history of acute patellar dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef]
- Gravesen, K.S.; Kallemose, T.; Blønd, L.; Troelsen, A.; Barfod, K.W. High incidence of acute and recurrent patellar dislocations: A retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1204–1209. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Pareek, A.; Hewett, T.E.; Stuart, M.J.; Dahm, D.L.; Krych, A.J. Incidence of First-Time Lateral Patellar Dislocation: A 21-Year Population-Based Study. Sports Health 2018, 10, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Ricciuti, A.; Colosi, K.; Fitzsimmons, K.; Brown, M. Patellofemoral Instability in the Pediatric and Adolescent Population: From Causes to Treatments. Children 2024, 11, 1261. [Google Scholar] [CrossRef] [PubMed]
- Jayne, C.; Mavrommatis, S.; Shah, A.D.; Medina, G.; Paschos, N. Risk factors and treatment rationale for patellofemoral instability in the pediatric population. J. Pediatr. Soc. N. Am. 2024, 6, 100015. [Google Scholar] [CrossRef]
- Danielsen, O.; Poulsen, T.A.; Eysturoy, N.H.; Mortensen, E.S.; Hölmich, P.; Barfod, K.W. Trochlea dysplasia, increased TT-TG distance and patella alta are risk factors for developing first-time and recurrent patella dislocation: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3806–3846. [Google Scholar] [CrossRef]
- Pineda, T.; Dejour, D.H. ‘À la carte’ treatment algorithm for patellofemoral instability. Rev. Esp. Cir. Ortop. Traumatol. 2025, 69, T544–T550. [Google Scholar] [CrossRef]
- Pauyo, T.; Park, J.P.; Bozzo, I.; Bernstein, M. Patellofemoral Instability Part I: Evaluation and Nonsurgical Treatment. J. Am. Acad. Orthop. Surg. 2022, 30, e1431–e1442. [Google Scholar] [CrossRef]
- Bollier, M.; Fulkerson, J.P. The role of trochlear dysplasia in patellofemoral instability. J. Am. Acad. Orthop. Surg. 2011, 19, 8–16. [Google Scholar] [CrossRef]
- Aljadaan, B.M.; Alhakbani, M.S.A.; Almonaie, S.H.; Cahusac, P.M.B. Outcomes of Surgical Interventions for Patellofemoral Instability in the Presence of Trochlear Dysplasia: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2025, 53, 1216–1230. [Google Scholar] [CrossRef]
- Hiemstra, L.A.; Kerslake, S.; Loewen, M.; Lafave, M. Effect of Trochlear Dysplasia on Outcomes After Isolated Soft Tissue Stabilization for Patellar Instability. Am. J. Sports Med. 2016, 44, 1515–1523. [Google Scholar] [CrossRef]
- Dejour, D.H.; Deroche, É. Trochleoplasty: Indications in patellar dislocation with high-grade dysplasia. Surgical technique. Orthop. Traumatol. Surg. Res. 2022, 108, 103160. [Google Scholar] [CrossRef]
- Malghem, J.; Maldague, B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: Relation to patellar dislocation. Radiology 1989, 170, 507–510. [Google Scholar] [CrossRef]
- Maldague, B.; Malghem, J. Apport du cliché de profil du genou dans le dépistage des instabilités rotuliennes. Rapport préliminaire [Significance of the radiograph of the knee profile in the detection of patellar instability. Preliminary report]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1985, 71, 5–13. [Google Scholar] [PubMed]
- Walch, G.; Dejour, H. Radiology in femoropatellar pathology. Acta Orthop. Belg 1989, 55, 371–380. [Google Scholar]
- Dejour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. Factors of patellar instability: An anatomic radiographic study. Knee Surg. Sports Traumatol. Arthrosc. 1994, 2, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Dejour, D.; Reynaud, P.; Lecoultre, B. Douleurs et instabilité rotulienne. Essai de classification. Med. Hyg. 1998, 56, 1466–1471. [Google Scholar]
- Dejour, H.; Walch, G.; Neyret, P.; Adeleine, P. Dysplasia of the femoral trochlea. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1990, 76, 45–54. (In French) [Google Scholar]
- Dejour, D.H.; Mesnard, G.; Giovannetti de Sanctis, E. Updated treatment guidelines for patellar instability: “un menu à la carte”. J. Exp. Orthop. 2021, 8, 109. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tscholl, P.M.; Wanivenhaus, F.; Fucentese, S.F. Conventional Radiographs and Magnetic Resonance Imaging for the Analysis of Trochlear Dysplasia: The Influence of Selected Levels on Magnetic Resonance Imaging. Am. J. Sports Med. 2017, 45, 1059–1065. [Google Scholar] [CrossRef]
- Pineda, T.; Dejour, D.; ReSurg. Inconsistent repeatability of the Dejour classification of trochlear dysplasia due to the variability of imaging modalities: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5707–5720. [Google Scholar] [CrossRef] [PubMed]
- Dejour, D.H.; de Sanctis, E.G.; Müller, J.H.; Deroche, E.; Pineda, T.; Guarino, A.; Toanen, C.; Patellofemoral Imaging Group. Adapting the Dejour classification of trochlear dysplasia from qualitative radiograph- and CT-based assessments to quantitative MRI-based measurements. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 2833–2846. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, M.F.; Maggini, E.; Vaisitti, N.; Pianelli, A.; Grava, G.; Cattaneo, S.; Milano, G. Sulcus Angle, Trochlear Depth, and Dejour’s Classification Can Be Reliably Applied to Evaluate Trochlear Dysplasia: A Systematic Review of Radiological Measurements. Arthroscopy 2023, 39, 549–568. [Google Scholar] [CrossRef] [PubMed]
- Dejour, H.; Walch, G. La pathologie fe’ moropatellaire. In 6èmes Journe es Lyonnaises de Chirurgie du Genou; University of Lyon: Lyon, France, 1987. [Google Scholar]
- Pfirrmann, C.W.; Zanetti, M.; Romero, J.; Hodler, J. Femoral trochlear dysplasia: MR findings. Radiology 2000, 216, 858–864. [Google Scholar] [CrossRef]
- Sharma, N.; Brown, A.; Bouras, T.; Kuiper, J.H.; Eldridge, J.; Barnett, A. The Oswestry-Bristol Classification. Bone Jt. J. 2020, 102, 102–107. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Walsh, J.M.; Credille, K.; Allahabadi, S.; Kaplan, D.J.; Darbandi, A.D.; Huddleston, H.P.; Hevesi, M.; Wang, Z.; Dandu, N.; Yanke, A.B. Biomechanical Properties and Kinematics of Medial Patellofemoral Ligament Reconstruction: A Systematic Review. Orthop. J. Sports Med. 2024, 12, 23259671241241537. [Google Scholar] [CrossRef]
- Chahla, J.; Smigielski, R.; LaPrade, R.F.; Fulkerson, J.P. An Updated Overview of the Anatomy and Function of the Proximal Medial Patellar Restraints (Medial Patellofemoral Ligament and the Medial Quadriceps Tendon Femoral Ligament). Sports Med. Arthrosc. Rev. 2019, 27, 136–142. [Google Scholar] [CrossRef]
- Kazley, J.M.; Banerjee, S. Classifications in Brief: The Dejour Classification of Trochlear Dysplasia. Clin. Orthop. Relat. Res. 2019, 477, 2380–2386. [Google Scholar] [CrossRef]
- Tanaka, M.J. Editorial Commentary: Trochlear Dysplasia Is Difficult to Measure, No Matter How You Slice It. Arthroscopy 2021, 37, 1212–1213. [Google Scholar] [CrossRef]
- Brumini, I.; Pranjkovic, T.; Veljkovic Vujaklija, D. Evaluation of MRI-Based Measurements for Patellar Dislocation: Reliability and Reproducibility. Diagnostics 2025, 15, 2647. [Google Scholar] [CrossRef]

| Comparisons | κ (95% CI) | Exact Agreement | Interpretation |
|---|---|---|---|
| Intra-observer A (T1 vs. T2) | 0.957 (95% CI 0.933–0.980) | 91% | Almost perfect |
| Intra-observer B (T1 vs. T2) | 0.838 (95% CI 0.767–0.909) | 84% | Almost perfect |
| Inter-observer (T1: A vs. B) | 0.717 (95% CI 0.623–0.811) | 72% | Substantial |
| Inter-observer (T2: A vs. B) | 0.784 (95% CI 0.706–0.860) | 73% | Substantial |
| Observer A vs. Consensus (T1) | 0.580 (95% CI 0.481–0.679) | 52% | Moderate |
| Observer A vs. Consensus (T2) | 0.574 (95% CI 0.473–0.674) | 52% | Moderate |
| Observer B vs. Consensus (T1) | 0.518 (95% CI 0.407–0.628) | 51% | Moderate |
| Observer B vs. Consensus (T2) | 0.534 (95% CI 0.424–0.643) | 52% | Moderate |
| CT Level | Comparisons | κ (95% CI) | Exact Agreement | Interpretation |
|---|---|---|---|---|
| Roman Arc | Intra-observer A (T1 vs. T2) | 0.958 (95% CI 0.897–0.991) | 92% | Almost perfect |
| Intra-observer B (T1 vs. T2) | 0.788 (95% CI 0.542–0.977) | 90% | Substantial | |
| Inter-observer (T1: A vs. B) | 0.760 (95% CI 0.545–0.934) | 84% | Substantial | |
| Inter-observer (T2: A vs. B) | 0.836 (95% CI 0.700–0.948) | 84% | Almost perfect | |
| Observer A vs. Consensus (T1) | 0.565 (95% CI 0.389–0.736) | 54% | Moderate | |
| Observer A vs. Consensus (T2) | 0.572 (95% CI 0.385–0.735) | 54% | Moderate | |
| Observer B vs. Consensus (T1) | 0.561 (95% CI 0.353–0.751) | 52% | Moderate | |
| Observer B vs. Consensus (T2) | 0.574 (95% CI 0.381–0.743) | 52% | Moderate | |
| 3 cm Above Joint Line | Intra-observer A (T1 vs. T2) | 0.969 (95% CI 0.928–0.993) | 92% | Almost perfect |
| Intra-observer B (T1 vs. T2) | 0.874 (95% CI 0.718–0.977) | 92% | Almost perfect | |
| Inter-observer (T1: A vs. B) | 0.688 (95% CI 0.486–0.863) | 70% | Substantial | |
| Inter-observer (T2: A vs. B) | 0.779 (95% CI 0.588–0.925) | 72% | Substantial | |
| Observer A vs. Consensus (T1) | 0.603 (95% CI 0.359–0.783) | 56% | Substantial | |
| Observer A vs. Consensus (T2) | 0.627 (95% CI 0.392–0.809) | 54% | Substantial | |
| Observer B vs. Consensus (T1) | 0.533 (95% CI 0.276–0.738) | 54% | Moderate | |
| Observer B vs. Consensus (T2) | 0.602 (95% CI 0.368–0.802) | 58% | Substantial | |
| Midpatellar Level | Intra-observer A (T1 vs. T2) | 0.921 (95% CI 0.848–0.974) | 86% | Almost perfect |
| Intra-observer B (T1 vs. T2) | 0.759 (95% CI 0.479–0.925) | 78% | Substantial | |
| Inter-observer (T1: A vs. B) | 0.475 (95% CI 0.197–0.727) | 54% | Moderate | |
| Inter-observer (T2: A vs. B) | 0.644 (95% CI 0.399–0.825) | 62% | Substantial | |
| Observer A vs. Consensus (T1) | 0.421 (95% CI 0.222–0.606) | 34% | Moderate | |
| Observer A vs. Consensus (T2) | 0.394 (95% CI 0.190–0.576) | 38% | Fair | |
| Observer B vs. Consensus (T1) | 0.322 (95% CI 0.139–0.496) | 40% | Fair | |
| Observer B vs. Consensus (T2) | 0.315 (95% CI 0.130–0.488) | 40% | Fair | |
| Top of Blumensaat Line | Intra-observer A (T1 vs. T2) | 0.952 (95% CI 0.856–1.000) | 94% | Almost perfect |
| Intra-observer B (T1 vs. T2) | 0.766 (95% CI 0.600–0.894) | 76% | Substantial | |
| Inter-observer (T1: A vs. B) | 0.760 (95% CI 0.561–0.919) | 80% | Substantial | |
| Inter-observer (T2: A vs. B) | 0.719 (95% CI 0.520–0.880) | 74% | Substantial | |
| Observer A vs. Consensus (T1) | 0.727 (95% CI 0.567–0.848) | 64% | Substantial | |
| Observer A vs. Consensus (T2) | 0.692 (95% CI 0.486–0.840) | 62% | Substantial | |
| Observer B vs. Consensus (T1) | 0.674 (95% CI 0.471–0.823) | 58% | Substantial | |
| Observer B vs. Consensus (T2) | 0.674 (95% CI 0.472–0.822) | 58% | Substantial |
| Comparison | Roman Arc (%, 95% CI) | 3 cm Above the Joint Line (%, 95% CI) | Midpatellar Level (%, 95% CI) | Top of Blumensaat Line (%, 95% CI) | p-Value * |
|---|---|---|---|---|---|
| Observer A, T1 | 54% (40–68) | 56% (42–70) | 34% (20–48) | 64% (50–78) | 0.010 |
| Observer A, T2 | 54% (40–68) | 54% (40–68) | 38% (24–52) | 62% (48–76) | 0.075 |
| Observer B, T1 | 52% (38–66) | 54% (40–68) | 40% (26–54) | 58% (44–70) | 0.277 |
| Observer B, T2 | 52% (38–66) | 58% (44–72) | 40% (26–54) | 58% (44–70) | 0.190 |
| Pooled # | 53% (40–66) | 56% (44–68) | 38% (7–50) | 61% (49–72) | — |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Kılıc, K.K.; Ertan, M.B.; Selcuk, H.; Kirtis, T.; Uslu, O.; Kose, O. The Impact of Axial CT Level Selection on Grading Trochlear Dysplasia Using Dejour Classification. Diagnostics 2026, 16, 77. https://doi.org/10.3390/diagnostics16010077
Kılıc KK, Ertan MB, Selcuk H, Kirtis T, Uslu O, Kose O. The Impact of Axial CT Level Selection on Grading Trochlear Dysplasia Using Dejour Classification. Diagnostics. 2026; 16(1):77. https://doi.org/10.3390/diagnostics16010077
Chicago/Turabian StyleKılıc, Koray Kaya, Mehmet Baris Ertan, Huseyin Selcuk, Tolga Kirtis, Oguzhan Uslu, and Ozkan Kose. 2026. "The Impact of Axial CT Level Selection on Grading Trochlear Dysplasia Using Dejour Classification" Diagnostics 16, no. 1: 77. https://doi.org/10.3390/diagnostics16010077
APA StyleKılıc, K. K., Ertan, M. B., Selcuk, H., Kirtis, T., Uslu, O., & Kose, O. (2026). The Impact of Axial CT Level Selection on Grading Trochlear Dysplasia Using Dejour Classification. Diagnostics, 16(1), 77. https://doi.org/10.3390/diagnostics16010077






