Predictors of Impaired Reperfusion in ST-Elevation Myocardial Infarction Treated with Primary PCI: Preliminary Results from COMA.NET Project
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Definitions and Outcome
2.3. Statistical Analyses
2.4. Ethical Considerations
3. Results
3.1. Baseline Characteristics
3.2. Procedural Data
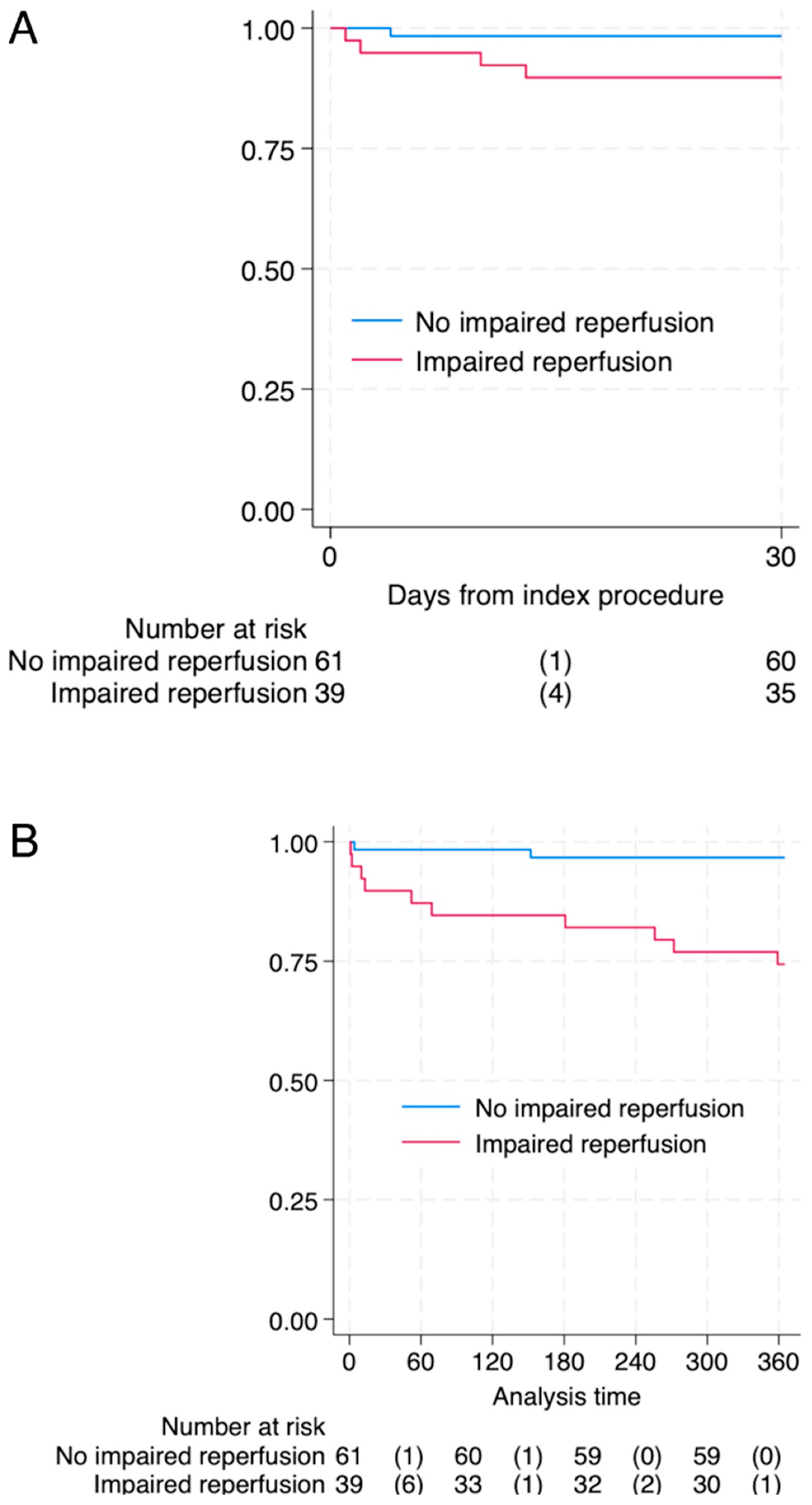
3.3. Follow-Up
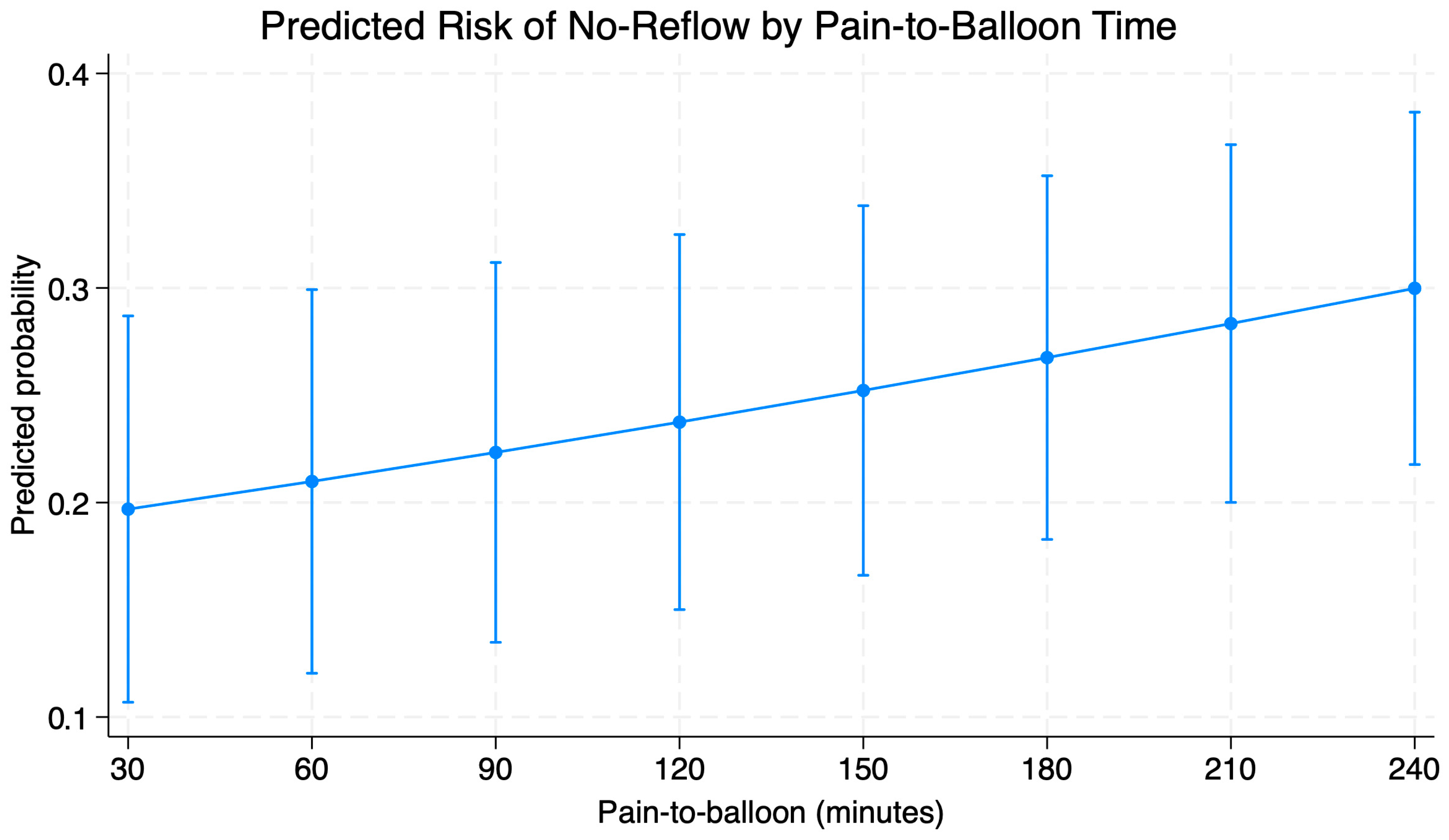
3.4. Predictors of Impaired Reperfusion
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nicolau, A.M.; Silva, P.G.; Mejía, H.P.G.; Granada, J.F.; Kaluza, G.L.; Burkhoff, D.; Abizaid, T.; Pileggi, B.; Freire, A.F.D.; Godinho, R.R.; et al. Molecular Mechanisms of Microvascular Obstruction and Dysfunction in Percutaneous Coronary Interventions: From Pathophysiology to Therapeutics—A Comprehensive Review. Int. J. Mol. Sci. 2025, 26, 6835. [Google Scholar] [CrossRef] [PubMed]
- Mignatti, A.; Echarte-Morales, J.; Sturla, M.; Latib, A. State of the Art of Primary PCI: Present and Future. J. Clin. Med. 2025, 14, 653. [Google Scholar] [CrossRef] [PubMed]
- Sokratous, S.; Mitsis, A.; Khattab, E.; Karelas, D.; Velidakis, N.; Kadoglou, N.P.E. Coronary Microvascular Disease Early After Myocardial Infarction: Diagnostic Approach and Prognostic Value—A Narrative Review. Biomedicines 2025, 13, 1289. [Google Scholar] [CrossRef]
- Annibali, G.; Scrocca, I.; Aranzulla, T.C.; Meliga, E.; Maiellaro, F.; Musumeci, G. “No-Reflow” Phenomenon: A Contemporary Review. J. Clin. Med. 2022, 11, 2233. [Google Scholar] [CrossRef] [PubMed]
- Feher, A.; Chen, S.Y.; Bagi, Z.; Arora, V. Prevention and treatment of no-reflow phenomenon by targeting the coronary microcirculation. Rev. Cardiovasc. Med. 2014, 15, 38–51. [Google Scholar] [CrossRef]
- Birdal, O.; Topçu, S.; Tanboğa, H.; Koza, Y.; Aksakal, E.; Gülcü, O.; Karakelleoğlu, S.; Şenocak, H.; Gündoğdu, F. The Relationship Between Clinical Outcomes and Calculated Thrombus Burden Before and After Initial Flow in Patients with ST-Segment Elevation Myocardial Infarction. Eurasian J. Med. 2022, 54, 145–149. [Google Scholar] [CrossRef]
- Chettibi, M.; Benghezel, S.; Bertal, S.; Nedjar, R.; Bouraghda, M.A.; Bouafia, M.T. No reflow: What are the predictors? Annales Cardiologie D’angeiologie 2015, 64, 472–480. [Google Scholar] [CrossRef]
- Kurtul, A.; Murat, S.N.; Yarlioglues, M.; Duran, M.; Celik, I.E.; Kilic, A. Mild to Moderate Renal Impairment Is Associated with No-Reflow Phenomenon After Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction. Angiology 2015, 66, 644–651. [Google Scholar] [CrossRef]
- Humphrey, S.M.; Gavin, J.B.; Herdson, P.B. Catecholamine-depletion and the no-reflow phenomenon in anoxic and ischaemic rat hearts. J. Mol. Cell. Cardiol. 1982, 14, 151–161. [Google Scholar] [CrossRef]
- Humphrey, S.M.; Seelye, R.N.; Gavin, J.B. The influence of adenosine on the no-reflow phenomenon in anoxic and ischaemic hearts. Pathology 1982, 14, 129–133. [Google Scholar] [CrossRef]
- Kuliczkowski, W.; Miszalski-Jamka, K.; Kaczmarski, J.; Pres, D.; Gąsior, M. No-reflow and platelet reactivity in diabetic patients with ST-segment elevation myocardial infarction: Is there a link? Postep. Kardiol. Interwencyjnej 2017, 13, 326–330. [Google Scholar] [CrossRef]
- Huczek, Z.; Filipiak, K.J.; Kochman, J.; Piatkowski, R.; Grabowski, M.; Roik, M.; Malek, L.A.; Jaworski, P.; Opolski, G. Baseline platelet reactivity in acute myocardial infarction treated with primary angioplasty--influence on myocardial reperfusion, left ventricular performance, and clinical events. Am. Heart J. 2007, 154, 62–70. [Google Scholar] [CrossRef]
- Yang, L.; Cong, H.; Lu, Y.; Chen, X.; Liu, Y. Prediction of no-reflow phenomenon in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Medicine 2020, 99, e20152. [Google Scholar] [CrossRef]
- Abdi, S.; Rafizadeh, O.; Peighambari, M.; Basiri, H.; Bakhshandeh, H. Evaluation of the Clinical and Procedural Predictive Factors of no-Reflow Phenomenon Following Primary Percutaneous Coronary Intervention. Res. Cardiovasc. Med. 2015, 4, e25414. [Google Scholar]
- Harrison, R.W.; Aggarwal, A.; Ou, F.S.; Klein, L.W.; Rumsfeld, J.S.; Roe, M.T.; Wang, T.Y.; American College of Cardiology National Cardiovascular Data Registry. Incidence and outcomes of no-reflow phenomenon during percutaneous coronary intervention among patients with acute myocardial infarction. Am. J. Cardiol. 2013, 111, 178–184. [Google Scholar] [CrossRef]
- d’Entremont, M.A.; Alazzoni, A.; Dzavik, V.; Sharma, V.; Overgaard, C.B.; Lemaire-Paquette, S.; Lamelas, P.; Cairns, J.A.; Mehta, S.R.; Natarajan, M.K.; et al. No-reflow after primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: An angiographic core laboratory analysis of the TOTAL Trial. EuroIntervention 2023, 19, e394–e401. [Google Scholar] [CrossRef] [PubMed]
- Desai, N.R.; Mega, J.L.; Jiang, S.; Cannon, C.P.; Sabatine, M.S. Interaction between cigarette smoking and clinical benefit of clopidogrel. J. Am. Coll. Cardiol. 2009, 53, 1273–1278. [Google Scholar] [CrossRef]
- Kodaira, M.; Miyata, H.; Numasawa, Y.; Ueda, I.; Maekawa, Y.; Sueyoshi, K.; Ishikawa, S.; Ohki, T.; Negishi, K.; Fukuda, K.; et al. Effect of Smoking Status on Clinical Outcome and Efficacy of Clopidogrel in Acute Coronary Syndrome. Circ. J. 2016, 80, 1590–1599. [Google Scholar] [CrossRef] [PubMed]
- Heusch, G.; Kleinbongard, P.; Böse, D.; Levkau, B.; Haude, M.; Schulz, R.; Erbel, R. Coronary microembolization: From bedside to bench and back to bedside. Circulation 2009, 120, 1822–1836. [Google Scholar] [CrossRef] [PubMed]
- Porto, I.; Biasucci, L.M.; De Maria, G.L.; Leone, A.M.; Niccoli, G.; Burzotta, F.; Trani, C.; Tritarelli, A.; Vergallo, R.; Liuzzo, G.; et al. Intracoronary microparticles and microvascular obstruction in patients with ST elevation myocardial infarction undergoing primary percutaneous intervention. Eur. Heart J. 2012, 33, 2928–2938. [Google Scholar] [CrossRef] [PubMed]
- Pachel, C.; Mathes, D.; Arias-Loza, A.P.; Heitzmann, W.; Nordbeck, P.; Deppermann, C.; Lorenz, V.; Hofmann, U.; Nieswandt, B.; Frantz, S. Inhibition of Platelet GPVI Protects Against Myocardial Ischemia-Reperfusion Injury. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 629–635. [Google Scholar] [CrossRef]
- Ziegler, M.; Wang, X.; Peter, K. Platelets in cardiac ischaemia/reperfusion injury: A promising therapeutic target. Cardiovasc. Res. 2019, 115, 1178–1188. [Google Scholar] [CrossRef] [PubMed]
- Aurigemma, C.; Scalone, G.; Tomai, F.; Altamura, L.; De Persio, G.; Stazi, A.; Lanza, G.A.; Crea, F. Persistent enhanced platelet activation in patients with acute myocardial infarction and coronary microvascular obstruction: Clinical implications. Thromb. Haemost. 2014, 111, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Mazhar, J.; Mashicharan, M.; Farshid, A. Predictors and outcome of no-reflow post primary percutaneous coronary intervention for ST elevation myocardial infarction. Int. J. Cardiol. Heart Vasc. 2016, 10, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Dudek, D.; Mielecki, W.; Burzotta, F.; Gasior, M.; Witkowski, A.; Horvath, I.G.; Legutko, J.; Ochala, A.; Rubartelli, P.; Wojdyla, R.M.; et al. Thrombus aspiration followed by direct stenting: A novel strategy of primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. Results of the Polish-Italian-Hungarian RAndomized ThrombEctomy Trial (PIHRATE Trial). Am. Heart J. 2010, 160, 966–972. [Google Scholar] [CrossRef]
- Tantawy, M.; Saad, M.; Hussien, S.; Selim, G.; Tamara, A. Predilation in Primary Percutaneous Coronary Intervention. Interv. Cardiol. 2025, 20, e15. [Google Scholar] [CrossRef]
- Zhou, S.S.; Tian, F.; Chen, Y.D.; Wang, J.; Sun, Z.J.; Guo, J.; Jin, Q.H. Combination therapy reduces the incidence of no-reflow after primary per-cutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction. J. Geriatr. Cardiol. 2015, 12, 135–142. [Google Scholar]
- Kandzari, D.E.; Tcheng, J.E.; Gersh, B.J.; Cox, D.A.; Stuckey, T.; Turco, M.; Mehran, R.; Garcia, E.; Zimetbaum, P.; McGlaughlin, M.G.; et al. Relationship between infarct artery location, epicardial flow, and myocardial perfusion after primary percutaneous revascularization in acute myocardial infarction. Am. Heart J. 2006, 151, 1288–1295. [Google Scholar] [CrossRef]
- Reindl, M.; Holzknecht, M.; Tiller, C.; Lechner, I.; Schiestl, M.; Simma, F.; Pamminger, M.; Henninger, B.; Mayr, A.; Klug, G.; et al. Impact of infarct location and size on clinical outcome after ST-elevation myocardial infarction treated by primary percutaneous coronary intervention. Int. J. Cardiol. 2020, 301, 14–20. [Google Scholar] [CrossRef]
- Tasar, O.; Karabay, A.K.; Oduncu, V.; Kirma, C. Predictors and outcomes of no-reflow phenomenon in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron. Artery Dis. 2019, 30, 270–276. [Google Scholar] [CrossRef]
- De Luca, G.; Gibson, C.M.; Huber, K.; Zeymer, U.; Dudek, D.; Cutlip, D.; Bellandi, F.; Noc, M.; Emre, A.; Zorman, S.; et al. Association between advanced Killip class at presentation and impaired myocardial perfusion among patients with ST-segment elevation myocardial infarction treated with primary angioplasty and adjunctive glycoprotein IIb-IIIa inhibitors. Am. Heart J. 2009, 158, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Ndrepepa, G.; Tiroch, K.; Fusaro, M.; Keta, D.; Seyfarth, M.; Byrne, R.A.; Pache, J.; Alger, P.; Mehilli, J.; Schömig, A.; et al. 5-year prognostic value of no-reflow phenomenon after percutaneous coronary intervention in patients with acute myocardial infarction. J. Am. Coll. Cardiol. 2010, 55, 2383–2389. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.C.; Cho, J.Y.; Jeong, H.C.; Lee, K.H.; Park, K.H.; Sim, D.S.; Yoon, N.S.; Youn, H.J.; Kim, K.H.; Hong, Y.J.; et al. Long-Term Clinical Outcomes of Transient and Persistent No Reflow Phenomena following Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction. Korean Circ. J. 2016, 46, 490–498. [Google Scholar] [CrossRef] [PubMed]
| Variable | Normal Reperfusion (61) | Impaired Reperfusion (39) | p-Value | |
|---|---|---|---|---|
| Baseline data | Age | 62.8 (11.6) | 70.6 (12.01) | 0.002 |
| Male sex | 45 (74%) | 22 (56%) | 0.07 | |
| Smoking | 35 (57.4%) | 9 (23.1%) | <0.001 | |
| Hypertension | 36 (59%) | 27 (69.2%) | 0.3 | |
| Diabetes | 11 (18%) | 9 (23.1%) | 0.54 | |
| Hyperlipidemia | 48 (78.7%) | 27 (69.2%) | 0.29 | |
| Atrial fibrillation | 5 (8.2%) | 8 (20.5%) | 0.07 | |
| eGFR (mL/min) | 86 (72–114) | 71 (51–92) | 0.005 | |
| Creatinine (mg/dL) | 0.86 (0.81–0.96) | 0.95 (0.82–1.18) | 0.07 | |
| Previous CAD | 9 (14.8%) | 10 (25.6%) | 0.18 | |
| Previous MI | 5 (8.2%) | 2 (5.1%) | 0.56 | |
| Previous revascularization | 5 (8.2%) | 1 (2.6%) | 0.25 | |
| EF (%) | 41.3 (7.9) | 34.3 (8.6) | <0.001 | |
| Pain time (min) | 163 (120–236) | 466 (103–771) | <0.001 | |
| Pain to drug (min) | 90 (60–172) | 360 (100–669) | <0.001 | |
| Pain to balloon (min) | 185 (147–271) | 505 (238–815) | <0.001 | |
| Duty hours | 23 (37.7%) | 10 (25.6%) | 0.21 | |
| Sudden cardiac arrest | 3 (4.9%) | 3 (7.7%) | 0.57 | |
| MI Location | Anterior MI | 25 (41%) | 29 (74.4%) | 0.004 |
| Inferior MI | 33 (54.1%) | 10 (25.6%) | ||
| Lateral MI | 3 (4.9%) | 0 (0%) | ||
| Platelet reactivity | ADP test on admission | 869 (609–1274) | 804 (419–1150) | 0.24 |
| ASPI test on admission | 210.5 (82–487) | 235 (138–379) | 0.6 | |
| ADP test on fifth day | 266.5 (175.5–484) | 349 (203–515) | 0.18 | |
| ASPI test on fifth day | 127 (76–191) | 139 (89–211) | 0.67 | |
| HTPR on admission (cut-off 416 AUC) | 49 (80.3%) | 25 (64.1%) | 0.15 | |
| HTPR of fifth day (cut-off 416 AUC) | 14 (23%) | 11 (28.2%) | 0.59 | |
| Clopidogrel resistance (>46 AU) | 27 (44.3%) | 23 (59%) | 0.15 | |
| Drugs on discharge | Clopidogrel | 61 (100%) | 38 (97.4%) | 1 |
| ASA | 61 (100%) | 38 (97.4%) | 1 | |
| ACEi | 60 (98.4%) | 32 (82.1%) | 0.008 | |
| B-blocker | 59 (96.7%) | 36 (92.3%) | 0.63 | |
| Statin | 59 (96.7%) | 36 (92.3%) | 0.63 | |
| MRA | 24 (39.3%) | 25 (64.1%) | 0.01 | |
| Diuretics | 22 (36.1%) | 28 (71.8%) | <0.001 | |
| PPI | 59 (96.7%) | 37 (94.9%) | 0.86 | |
| Follow-up | Death in 12 months | 2 (3.3%) | 10 (25.6%) | 0.001 |
| Death during hospitalization | 1 (1.6%) | 4 (10.3%) | 0.054 |
| Variable | Normal Reperfusion (61) | Impaired Reperfusion (39) | p-Value | |
|---|---|---|---|---|
| SYNTAX Score I | 17 (8) | 21 (9) | 0.04 | |
| TIMI flow before pPCI | 0 | 40 (65.6%) | 31 (79.5%) | 0.46 |
| 1 | 2 (3.3%) | 1 (2.6%) | ||
| 2 | 11 (18%) | 5 (12.8%) | ||
| 3 | 8 (13.1%) | 2 (5.1%) | ||
| Thrombectomy | 31 (50.1%) | 23 (60%) | 0.43 | |
| Predilation | 31 (50.1%) | 34 (87.2%) | <0.001 | |
| Number of stents | 0 | 0 (0%) | 1 (2.6%) | 0.43 |
| 1 | 46 (75%) | 32 (82.1%) | ||
| 2 | 12 (20%) | 4 (10.3%) | ||
| 3 | 2 (3.3%) | 2 (5.1%) | ||
| 4 | 1 (1.6%) | 0 (0%) | ||
| Stent data | Mean stent diameter | 3.5 (3–3.5) | 3.5 (3–3.5) | 0.51 |
| Mean stent length | 22 (16–28) | 22 (18–28) | 0.99 | |
| TIMI flow after pPCI | 0 | 0 (0%) | 0 (0%) | <0.001 |
| 1 | 0 (0%) | 3 (7.7%) | ||
| 2 | 0 (0%) | 22 (56.4%) | ||
| 3 | 61 (100%) | 14 (35.9%) | ||
| MBG after pPCI | 0 | 0 (0%) | 1 (2.6%) | <0.001 |
| 1 | 0 (0%) | 7 (17.9%) | ||
| 2 | 10 (16.4%) | 18 (46.2%) | ||
| 3 | 51 (83.6%) | 13 (33.3%) | ||
| TMPG after pPCI | 0 | 0 (0%) | 3 (7.7%) | <0.001 |
| 1 | 3 (4.9%) | 6 (15.4%) | ||
| 2 | 11 (18%) | 19 (48.7%) | ||
| 3 | 47 (77%) | 11 (28.2%) | ||
| cTFC after pPCI | 20 (15–27) | 43 (24–58) | <0.001 | |
| Time of procedure | 32 (25–48) | 40 (30–55) | 0.07 | |
| X-ray time (min) | 7.6 (5.1–10.5) | 10.3 (6.9–15.7) | 0.02 | |
| Radiation dose (mGy) | 1211 (775–1639) | 1340 (834–2138) | 0.27 | |
| Contrast dye (mL) | 150 (120–170) | 170 (140–220) | 0.07 | |
| Use of GP IIb/IIIa inhibitors | 23 (37.7%) | 18 (46.2%) | 0.4 | |
| No early post-pPCI ST resolution (<50% reduction of elevation) | 0 (0%) | 29 (74.4%) | <0.001 |
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Male sex | 0.77 (0.2–3.01) | 0.71 |
| Pain to balloon (per increase in 10 min) | 1.05 (1.02–1.07) | <0.001 |
| Anterior MI | 5.05 (1.14–22.38) | 0.03 |
| Predilation | 7.66 (1.78–32.9) | 0.006 |
| SYNTAX score I (per increase in 1 point) | 0.94 (0.87–1.02) | 0.13 |
| Killip–Kimball Class (per increase in 1 class) | 7.69 (1.88–31.38) | 0.004 |
| Smoking | 0.3 (0.08–1.1) | 0.07 |
| Atrial fibrillation | 0.37 (0.05–2.87) | 0.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Południewski, M.; Dąbrowski, E.J.; Pogorzelski, P.; Łuczaj, M.; Kobylińska, J.; Kruszyńska, J.; Kożuch, M.; Dobrzycki, S. Predictors of Impaired Reperfusion in ST-Elevation Myocardial Infarction Treated with Primary PCI: Preliminary Results from COMA.NET Project. Diagnostics 2026, 16, 149. https://doi.org/10.3390/diagnostics16010149
Południewski M, Dąbrowski EJ, Pogorzelski P, Łuczaj M, Kobylińska J, Kruszyńska J, Kożuch M, Dobrzycki S. Predictors of Impaired Reperfusion in ST-Elevation Myocardial Infarction Treated with Primary PCI: Preliminary Results from COMA.NET Project. Diagnostics. 2026; 16(1):149. https://doi.org/10.3390/diagnostics16010149
Chicago/Turabian StylePołudniewski, Maciej, Emil Julian Dąbrowski, Piotr Pogorzelski, Michał Łuczaj, Julia Kobylińska, Joanna Kruszyńska, Marcin Kożuch, and Sławomir Dobrzycki. 2026. "Predictors of Impaired Reperfusion in ST-Elevation Myocardial Infarction Treated with Primary PCI: Preliminary Results from COMA.NET Project" Diagnostics 16, no. 1: 149. https://doi.org/10.3390/diagnostics16010149
APA StylePołudniewski, M., Dąbrowski, E. J., Pogorzelski, P., Łuczaj, M., Kobylińska, J., Kruszyńska, J., Kożuch, M., & Dobrzycki, S. (2026). Predictors of Impaired Reperfusion in ST-Elevation Myocardial Infarction Treated with Primary PCI: Preliminary Results from COMA.NET Project. Diagnostics, 16(1), 149. https://doi.org/10.3390/diagnostics16010149






