Development of a Pulmonary Nodule Service and Clinical Pathway: A Pragmatic Approach Addressing an Unmet Need
Abstract
1. Introduction
2. Materials and Methods
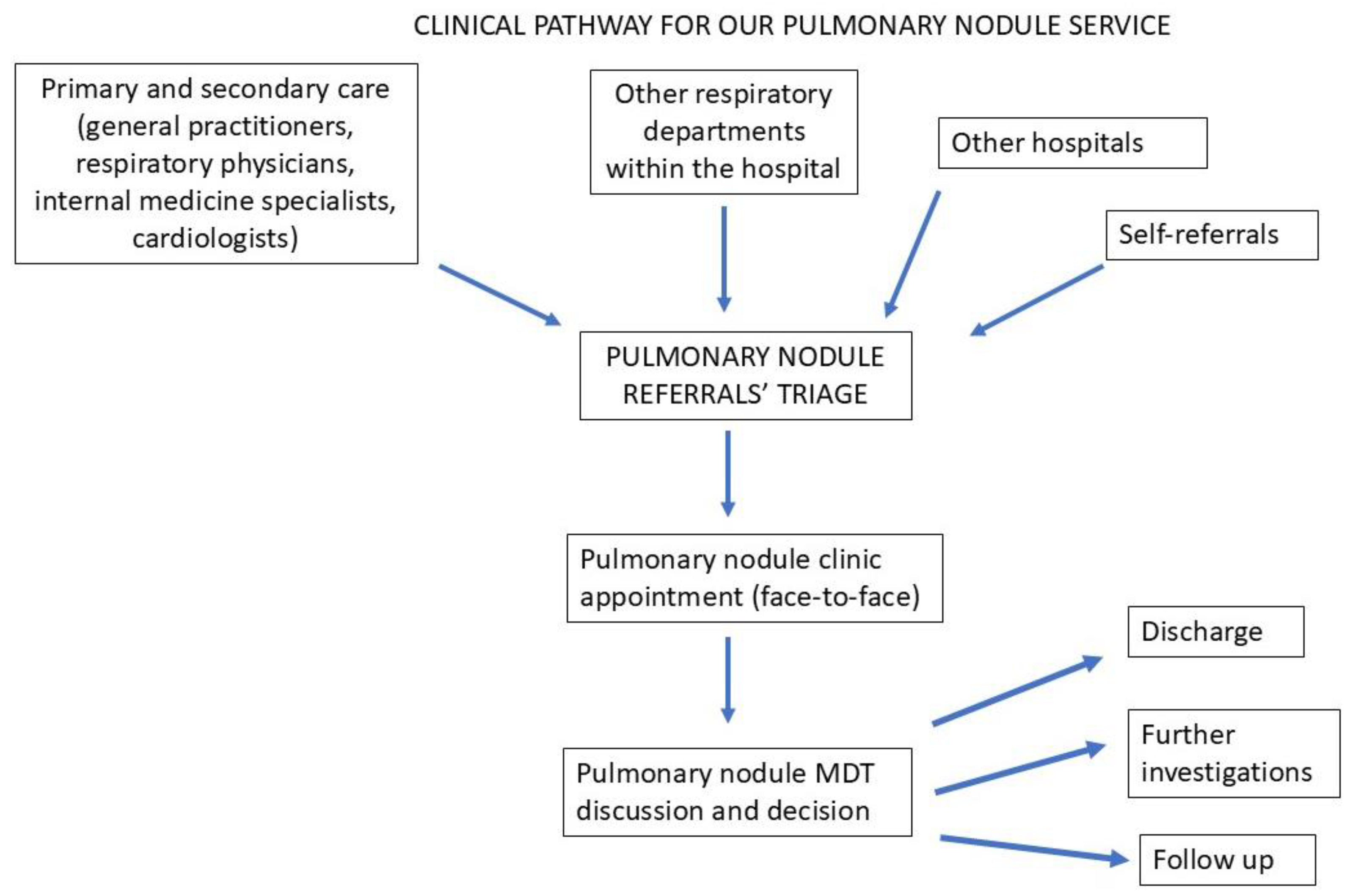
2.1. The Service
2.2. The Pathway
2.3. Referral Criteria
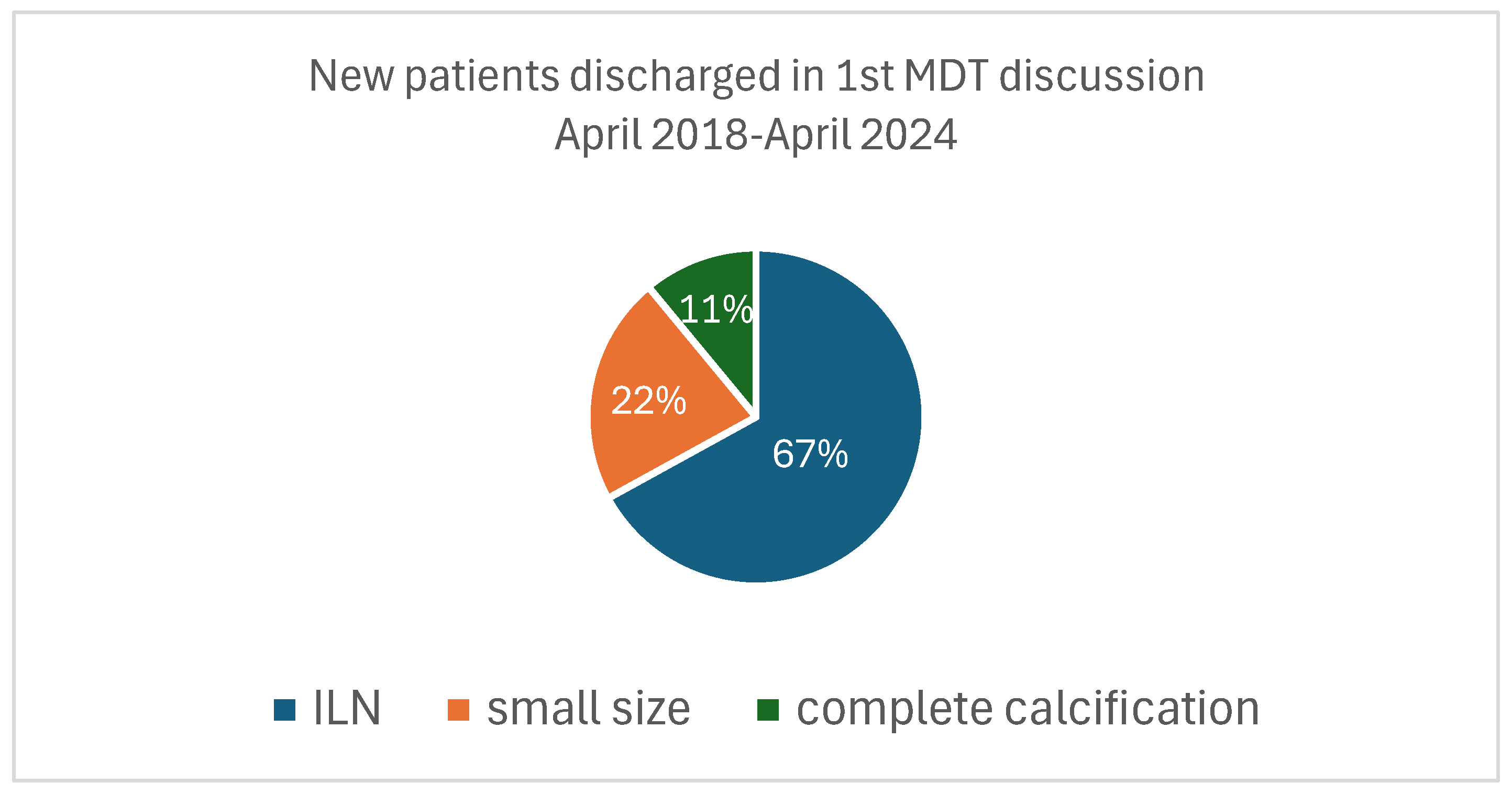
3. Results
4. Discussion
4.1. The Problem of Incidental Pulmonary Nodules and the Need for Dedicated Structured Clinical Services
4.2. The Importance of Safety Netting and Appropriate Follow-Up
4.3. Dedicated Specialized Personnel Improves Patient Management
4.4. Pulmonary Nodules’ Density and Radical Treatment
4.5. Additional Radiological Findings Beyond Incidental Pulmonary Nodules
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LDCT | Low dose computed tomography |
| PNS | Pulmonary nodule service |
| MDT | Multidisciplinary team |
| COPD | Chronic obstructive pulmonary disease |
| MTOS | Multidisciplinary thoracic oncology service |
| TB | Tuberculosis |
References
- Hall, W.B.; Truitt, S.G.; Scheunemann, L.P.; Shah, S.A.; Rivera, M.P.; Parker, L.A.; Carson, S.S. The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism. Arch. Intern. Med. 2009, 169, 1961–1965. [Google Scholar] [CrossRef] [PubMed]
- Kwan, J.L.; Yermak, D.; Markell, L.; Paul, N.S.; Shojania, K.G.; Cram, P. Follow Up of Incidental High-Risk Pulmonary Nodules on Computed Tomography Pulmonary Angiography at Care Transitions. J. Hosp. Med. 2019, 14, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Scholtz, J.E.; Lu, M.T.; Hedgire, S.; Meyersohn, N.M.; Oliveira, G.R.; Prabhakar, A.M.; Gupta, R.; Kalra, M.K.; Shepard, J.O.; Hoffmann, U.; et al. Incidental pulmonary nodules in emergent coronary CT angiography for suspected acute coronary syndrome: Impact of revised 2017 Fleischner Society Guidelines. J. Cardiovasc. Comput. Tomogr. 2018, 12, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.; Nicholls, S.; Bardin, P.; Ptasznik, R.; Steinfort, D.; Miller, A. Incidental Pulmonary Nodules Are Common on CT Coronary Angiogram and Have a Significant Cost Impact. Heart Lung Circ. 2019, 28, 295–301. [Google Scholar] [CrossRef]
- Iribarren, C.; Hlatky, M.A.; Chandra, M.; Fair, J.M.; Rubin, G.D.; Go, A.S.; Burt, J.R.; Fortmann, S.P. Incidental pulmonary nodules on cardiac computed tomography: Prognosis and use. Am. J. Med. 2008, 121, 989–996. [Google Scholar] [CrossRef]
- Song, J.H.; Beland, M.D.; Mayo-Smith, W.W. Incidental clinically important extraurinary findings at MDCT urography for hematuria evaluation: Prevalence in 1209 consecutive examinations. Am. J. Roentgenol. 2012, 199, 616–622. [Google Scholar] [CrossRef]
- Hardavella, G.; Bisirtzoglou, D.; Stasinopoulou, M.; Agapitou, T.; Karampinis, I.; Kostoulas, A.; Lampaki, S.; Fili, E.; Zervas, E.; Gkiozos, I. National Lung Cancer Screening Programs Worldwide; An Emerging Call for Early Diagnosis. J. Respir. Dis. Treat. 2024, 5, 101. [Google Scholar]
- Frille, A.; Hardavella, G.; Lee, R. Lung cancer incidence and mortality with extended follow-up in the National LungScreening Trial. Breathe 2020, 16, 190322. [Google Scholar] [CrossRef]
- Hardavella, G.; Frille, A.; Sreter, K.B.; Atrafi, F.; Yousaf-Khan, U.; Beyaz, F.; Kyriakou, F.; Bellou, E.; Mullin, M.L.; Janes, S.M. Lung cancer screening: Where do we stand? Breathe 2024, 20, 230190. [Google Scholar] [CrossRef]
- Hardavella, G.; Frille, A.; Chalela, R.; Sreter, K.B.; Petersen, R.H.; Novoa, N.; de Koning, H.J. How will lung cancer screening and lung nodule management change the diagnostic and surgical lung cancer landscape? Eur. Respir. Rev. 2024, 33, 230232. [Google Scholar] [CrossRef]
- Hardavella, G.; Sethi, T. Epidemiology: Development and perspectives. In Dingemans A-MC; Reck, M., Westeel, V., Eds.; Lung cancer; European Respiratory Society: Lausanne, Switzerland, 2015; pp. 1–11. [Google Scholar]
- Wolf, A.M.D.; Oeffinger, K.C.; Shih, T.Y.; Walter, L.C.; Church, T.R.; Fontham, E.T.H.; Elkin, E.B.; Etzioni, R.D.; Guerra, C.E.; Perkins, R.B.; et al. Screening for lung cancer: 2023 guideline update from the American Cancer Society. CA Cancer J. Clin. 2024, 74, 50–81. [Google Scholar] [CrossRef] [PubMed]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- de Koning, H.J.; van der Aalst, C.M.; de Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N.; et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Pastorino, U.; Silva, M.; Sestini, S.; Sabia, F.; Boeri, M.; Cantarutti, A.; Sverzellati, N.; Sozzi, G.; Corrao, G.; Marchianò, A. Prolonged lung cancer screening reduced 10-year mortality in the MILD trial: New confirmation of lung cancer screening efficacy. Ann. Oncol. 2019, 30, 1162–1169. [Google Scholar] [CrossRef]
- MacMahon, H.; Austin, J.H.; Gamsu, G.; Herold, C.J.; Jett, J.R.; Naidich, D.P.; Patz, E.F., Jr.; Swensen, S.J.; Fleischner Society. Guidelines for Management of Small Pulmonary Nodules Detected on CT Scans: A Statement from the Fleischner Society. Radiology 2005, 237, 395–400. [Google Scholar] [CrossRef]
- Gould, M.K.; Donington, J.; Lynch, W.R.; Mazzone, P.J.; Midthun, D.E.; Naidich, D.P.; Wiener, R.S. Evaluation of individuals with pulmonary nodules: When is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, e93S–e120S. [Google Scholar] [CrossRef]
- Callister, M.E.; Baldwin, D.R.; Akram, A.R.; Barnard, S.; Cane, P.; Draffan, J.; Franks, K.; Gleeson, F.; Graham, R.; Malhotra, P.; et al. British Thoracic Society Pulmonary Nodule Guideline Development Group; British Thoracic Society Standards of Care Committee. British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 2015, 70, ii1–ii54. [Google Scholar] [CrossRef]
- MacMahon, H.; Naidich, D.P.; Goo, J.M.; Lee, K.S.; Leung, A.N.C.; Mayo, J.R.; Mehta, A.C.; Ohno, Y.; Powell, C.A.; Prokop, M.; et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017. Radiology 2017, 284, 161659. [Google Scholar] [CrossRef]
- Sethi, S.; Parrish, S. Incidental nodule management—Should there be a formal process? J. Thorac. Dis. 2016, 8 (Suppl. S6), S494–S497. [Google Scholar] [CrossRef]
- Digby, G.C.; Habert, J.; Sahota, J.; Zhu, L.; Manos, D. Incidental pulmonary nodule management in Canada: Exploring current state through a narrative literature review and expert interviews. J. Thorac. Dis. 2024, 16, 1537–1551. [Google Scholar] [CrossRef]
- Souliotis, K.; Golna, C.; Golnas, P. Establishing a Pulmonary Nodule Clinic Service for Early Diagnosis of Lung Cancer—Review of International Options and Considerations for Greece. Risk Manag. Healthc. Policy 2023, 16, 159–168. [Google Scholar] [CrossRef] [PubMed]
- O’Dowd, E.L.; Tietzova, I.; Bartlett, E.; Devaraj, A.; Biederer, J.; Brambilla, M.; Brunelli, A.; Chorostowska-Wynimko, J.; Decaluwe, H.; Deruysscher, D.; et al. ERS/ESTS/ESTRO/ESR/ESTI/EFOMP statement on management of incidental findings from low dose CT screening for lung cancer. Eur. Respir. J. 2023, 62, 2300533. [Google Scholar]
- Gulati, S.; Ivic-Pavlicic, T.; Joasil, J.; Flores, R.; Taioli, E. Outcomes in Incidentally Versus Screening Detected Stage I Lung Cancer Surgery Patients. J. Thorac. Oncol. 2024, 19, 581–588. [Google Scholar] [CrossRef]
- Interim Report in the Context of the Sector Inquiry into Private Health Services and Related Insurance Services, Under Art. 40 of L. 3959/2011. Available online: https://www.epant.gr/files/2023/health/Executive_Summary_Health_en.pdf (accessed on 27 April 2025).
- Hardavella, G.; Azhar, A.; Hussain, A.; Desai, S. Retrospective review of a novel clinical service and pathway for patients with pulmonary nodules. Eur. Respir. J. 2016, 48 (Suppl. S60), PA3078. [Google Scholar]
- Hardavella, G.; Desai, S. Development of a pulmonary nodule service & clinical pathway: A pragmatic approach addressing an unmet need. Eur. Respir. J. 2016, 48 (Suppl. S60), PA3079. [Google Scholar]
- O’Donnell, P.; O’Brien, F.; Valentine, L.; Telford, C. An assessment of nurse led follow up of pulmonary nodules. Eur. Respir. J. 2016, 48 (Suppl. S60), PA3080. [Google Scholar]
- Marcus, A.; Pittman, S.; Bloxham, H.; Storey, H.; Kohn, J.; Jallow, O.; Ncube, A.; Peacock, J. Use of Clinical Nurse Specialists in the Management of Incidental Pulmonary Nodules. Eur. Respir. J. 2021, 58 (Suppl. S65), PA1806. [Google Scholar]
- Gilbert, C.R.; Ely, R.; Fathi, J.T.; Louie, B.E.; Wilshire, C.L.; Modin, H.; Aye, R.W.; Farivar, A.S.; Vallières, E.; Gorden, J.A. The economic impact of a nurse practitioner-directed lung cancer screening, incidental pulmonary nodule, and tobacco-cessation clinic. J. Thorac. Cardiovasc. Surg. 2018, 155, 416–424. [Google Scholar] [CrossRef]
- Melton, N.; Lazar, J.F.; Moritz, T.A. A Community-based Pulmonary Nodule Clinic: Improving Lung Cancer Stage at Diagnosis. Cureus 2019, 11, e4226. [Google Scholar] [CrossRef]
- Simmons, J.; Gould, M.K.; Iaccarino, J.; Slatore, C.G.; Wiener, R.S. Systems-Level Resources for Pulmonary Nodule Evaluation in the United States: A National Survey. Am. J. Respir. Crit. Care Med. 2016, 193, 1063–1065. [Google Scholar] [CrossRef]
- Gould, M.K.; Tang, T.; Liu, I.L.; Lee, J.; Zheng, C.; Danforth, K.N.; Kosco, A.E.; Di Fiore, J.L.; Suh, D.E. Recent trends in the identification of incidental pulmonary nodules. Am. J. Respir. Crit. Care Med. 2015, 192, 1208–1214. [Google Scholar] [CrossRef] [PubMed]
- Tanner, N.T.; Aggarwal, J.; Gould, M.K.; Kearney, P.; Diette, G.; Vachani, A.; Fang, K.C.; Silvestri, G.A. Management of pulmonary nodules by community pulmonologists: A multicenter observational study. Chest 2015, 148, 1405–1414. [Google Scholar] [CrossRef] [PubMed]
- Wiener, R.S.; Gould, M.K.; Slatore, C.G.; Fincke, B.G.; Schwartz, L.M.; Woloshin, S. Resource use and guideline concordance in evaluation of pulmonary nodules for cancer: Too much and too little care. JAMA Intern. Med. 2014, 174, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Blagev, D.P.; Lloyd, J.F.; Conner, K.; Dickerson, J.; Adams, D.; Stevens, S.M.; Woller, S.C.; Evans, R.S.; Elliott, C.G. Follow-up of incidental pulmonary nodules and the radiology report. J. Am. Coll. Radiol. 2014, 11, 378–383. [Google Scholar] [CrossRef]
- Callen, J.L.; Westbrook, J.I.; Georgiou, A.; Li, J. Failure to follow-up test results for ambulatory patients: A systematic review. J. Gen. Intern. Med. 2012, 27, 1334–1348. [Google Scholar] [CrossRef]
- Golden, S.E.; Wiener, R.S.; Sullivan, D.; Ganzini, L.; Slatore, C.G. Primary care providers and a system problem: A qualitative study of clinicians caring for patients with incidental pulmonary nodules. Chest 2015, 148, 1422–1429. [Google Scholar] [CrossRef]
- Woloshin, S.; Schwartz, L.M.; Dann, E.; Black, W.C. Using radiology reports to encourage evidence-based practice in the evaluation of small, incidentally detected pulmonary nodules: A preliminary study. Ann. Am. Thorac. Soc. 2014, 11, 211–214. [Google Scholar] [CrossRef]
- Hunnibell, L.S.; Slatore, C.G.; Ballard, E.A. Foundations for lung nodule management for nurse navigators. Clin. J. Oncol. Nurs. 2013, 17, 525–531. [Google Scholar] [CrossRef]
- Alsamarai, S.; Yao, X.; Cain, H.C.; Chang, B.W.; Chao, H.H.; Connery, D.M.; Deng, Y.; Garla, V.N.; Hunnibell, L.S.; Kim, A.W.; et al. The effect of a lung cancer care coordination program on timeliness of care. Clin. Lung Cancer 2013, 14, 527–534. [Google Scholar] [CrossRef]
- Slatore, C.G.; Horeweg, N.; Jett, J.R.; Midthun, D.E.; Powell, C.A.; Wiener, R.S.; Wisnivesky, J.P.; Gould, M.K.; on behalf of the ATS Ad Hoc Committee on Setting a Research Framework for Pulmonary Nodule Evaluation. An Official American Thoracic Society research statement: A research framework for pulmonary nodule evaluation and management. Am. J. Respir. Crit. Care Med. 2015, 192, 500–514. [Google Scholar] [CrossRef]
- Nair, A.; Bartlett, E.C.; Walsh, S.L.F.; Wells, A.U.; Navani, N.; Hardavella, G.; Bhalla, S.; Calandriello, L.; Devaraj, A.; Goo, J.M.; et al. Variable radiological lung nodule evaluation leads to divergent management recommendations. Eur. Respir. J. 2018, 52, 1801359. [Google Scholar] [CrossRef] [PubMed]
- Blum, T.G.; Morgan, R.L.; Durieux, V.; Chorostowska-Wynimko, J.; Baldwin, D.R.; Boyd, J.; Faivre-Finn, C.; Galateau-Salle, F.; Gamarra, F.; Grigoriu, B.; et al. European Respiratory Society guideline on various aspects of quality in lung cancer care. Eur. Respir. J. 2023, 61, 2103201. [Google Scholar] [CrossRef] [PubMed]
- Rich, A.L.; Baldwin, D.R.; Beckett, P.; Berghmans, T.; Boyd, J.; Faivre-Finn, C.; Galateau-Salle, F.; Gamarra, F.; Grigoriu, B.; Hansen, N.G.; et al. ERS statement on harmonised standards for lung cancer registration and lung cancer services in Europe. Eur. Respir. J. 2018, 52, 1800610. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, R.L.; Bankier, A.A.; Boiselle, P.M. Compliance with Fleischner Society guidelines for management of small lung nodules: A survey of 834 radiologists. Radiology 2010, 255, 218–224. [Google Scholar] [CrossRef]
- Esmaili, A.; Munden, R.F.; Mohammed, T.L. Small pulmonary nodule management: A survey of the members of the Society of Thoracic Radiology with comparison to the Fleischner Society guidelines. J. Thorac. Imaging 2011, 26, 27–31. [Google Scholar] [CrossRef]
- Hardavella, G.; Frille, A.; Theochari, C.; Keramida, E.; Bellou, E.; Fotineas, A.; Bracka, I.; Pappa, L.; Zagana, V.; Palamiotou, M.; et al. Multidisciplinary care models for patients with lung cancer. Breathe 2020, 16, 200076. [Google Scholar] [CrossRef]
- The Radiologist Shortage Conundrum. Available online: https://www.acr.org/Clinical-Resources/Publications-and-Research/ACR-Bulletin/The-Radiologist-Shortage-Conundrum (accessed on 27 April 2025).
- Jeganathan, S. The Growing Problem of Radiologist Shortages: Australia and New Zealand’s Perspective. Korean J. Radiol. 2023, 24, 1043–1045. [Google Scholar] [CrossRef]
- Lai, J.; Li, Q.; Fu, F.; Zhang, Y.; Li, Y.; Liu, Q.; Chen, H. Subsolid Lung Adenocarcinomas: Radiological, Clinical and Pathological Features and Outcomes. Semin. Thorac. Cardiovasc. Surg. 2022, 34, 702–710. [Google Scholar] [CrossRef]
- Chen, H.; Kim, A.W.; Hsin, M.; Shrager, J.B.; Prosper, A.E.; Wahidi, M.M.; Wigle, D.A.; Wu, C.C.; Huang, J.; Yasufuku, K. The 2023 American Association for Thoracic Surgery (AATS) Expert Consensus Document: Management of subsolid lung nodules. J. Thorac. Cardiovasc. Surg. 2024, 168, 631–647.e11. [Google Scholar] [CrossRef]
- Savitch, S.L.; Zheng, R.; Abdelsattar, Z.M.; Barta, J.A.; Okusanya, O.T.; Evans, N.R., III.; Grenda, T.R. Surgical Outcomes in the National Lung Screening Trial Compared With Contemporary Practice. Ann. Thorac. Surg. 2023, 115, 1369–1377. [Google Scholar] [CrossRef]
- Tisi, S.; Dickson, J.L.; Horst, C.; Quaife, S.L.; Hall, H.; Verghese, P.; Gyertson, K.; Bowyer, V.; Levermore, C.; Mullin, A.M.; et al. Detection of COPD in the SUMMIT Study lung cancer screening cohort using symptoms and spirometry. Eur. Respir. J. 2022, 60, 2200795. [Google Scholar] [CrossRef] [PubMed]
- de-Torres, J.P.; Alcaide, A.B.; Campo, A.; Zulueta, J.J.; Bastarrika, G.; Ezponda, A.; Mesa, M.; Murillo, D.; Rodriguez, M.; Del Mar Ocón, M. Lung Cancer Screening in People With COPD: The Pamplona-IELCAP Experience. Arch. Bronconeumol. 2024, 60, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Ravenel, J.G.; Nance, J.W. Coronary artery calcification in lung cancer screening. Transl. Lung Cancer Res. 2018, 7, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Pinsky, P.F. Lung cancer screening with low-dose CT: A world-wide view. Transl. Lung Cancer Res. 2018, 7, 234–242. [Google Scholar] [CrossRef]
- Robbins, H.A.; Zahed, H.; Lebrett, M.B.; Balata, H.; Johansson, M.; Sharman, A.; Evans, D.G.; Crosbie, E.J.; Booton, R.; Landy, R.; et al. Explaining differences in the frequency of lung cancer detection between the National Lung Screening Trial and community-based screening in Manchester, UK. Lung Cancer 2022, 171, 61–64. [Google Scholar] [CrossRef]
- Elia, S.; Loprete, S.; De Stefano, A.; Hardavella, G. Does aggressive management of solitary pulmonary nodules pay off? Breathe 2019, 15, 15–23. [Google Scholar] [CrossRef]
- Hardavella, G.; Carlea, F.; Karampinis, I.; Patirelis, A.; Athanasiadi, K.; Lioumpas, D.; Rei, J.; Hoyos, L.; Benakis, G.; Caruana, E.; et al. A scoping review of lung cancer surgery with curative intent: Workup, fitness assessment, clinical outcomes. Breathe 2024, 20, 240046. [Google Scholar] [CrossRef]

| Characteristics | Number of Patients (%) |
|---|---|
| Sex | |
| Female | 903 (41%) |
| Male | 1300 (59%) |
| Mean age (years) | 64 ± 19 |
| Smoking habit | |
| Current smoker | 1432 (65%) |
| Ex-smoker | 507 (23%) |
| Lifelong non-smoker | 264 (12%) |
| History of extrathoracic cancer (discharged from relevant services) | |
| Yes | 485 (22%) |
| No | 1718 (78%) |
| Asbestos exposure | |
| Yes | 176 (8%) |
| No | 2027 (92%) |
| Don’t know | - |
| History of TB * | |
| Yes | 110 (5%) |
| No | 2093 (95%) |
| Radiological evidence of emphysema | |
| Yes | 1586 (72%) |
| No | 617 (28%) |
| Radiological evidence of coronary calcification | |
| Yes | 705 (32%) |
| No | 1498 (68%) |
| MDTs April 2018–April 2024 | 132 |
|---|---|
| Patients | |
| Total number of patients discussed | 2203 |
| New patients | 1365 (62%) |
| Follow-up patients | 838 (38%) |
| Patients with solid nodules | 1851 (84%) |
| Patients with subsolid nodules | 352 (16%) |
| Discharges | |
| New patients discharged in the first clinic appointment | 368/1365 (27%) |
| Intrapulmonary lymph nodes | 246/368 (67%) |
| Small size | 81/368 (22%) |
| Calcified nodule | 41/368 (11%) |
| Referral | |
| Patients referred to MTOS | 246/2203 (11%) |
| Patients referred to MTOS and discharged | 92/246 (37%) |
| Lung cancer diagnosis rate | 154/2203 (7%) |
| Adenocarcinoma | 100/154 (65%) |
| Squamous cell carcinoma | 46/154 (29.8%) |
| Typical carcinoid | 1/154 (0.65%) |
| Large cell carcinoma | 3/154 (1.95%) |
| Adenosquamous cell carcinoma | 4/154 (2.6%) |
| Stage I at diagnosis (T1a-c N0, eighth TNM edition) | 145/154 (94.15%) |
| Stage II at diagnosis (T1a-c N1, eighth TNM edition) | 9/154 (5.85%) |
| Histological Diagnosis | Nodule Density | ||
|---|---|---|---|
| Solid | Part-Solid | Pure Ground-Glass | |
| Adenocarcinoma (100/154) | 32 (32%) | 68 (68%) | 0 |
| Squamous cell carcinoma (46/154) | 45 (98%) | 1 (2%) | 0 |
| Typical carcinoid (1/154) | 1 (100%) | 0 | 0 |
| Large cell carcinoma (3/154) | 3 (100%) | 0 | 0 |
| Adenosquamous cell carcinoma (4/154) | 3 (75%) | 1 (25%) | 0 |
| N (100%) | Type of Resection | |||
|---|---|---|---|---|
| Pathology Staging | Wedge Resection | Segmentectomy | Lobectomy | |
| pT1aN0 | 38 | 20/38 (52.6%) | 17/38 (44.8%) | 1/38 (2.6%) |
| pT1bN0 | 78 | 0 | 29 (37.2%) | 49 (62.8%) |
| pT1cN0 | 29 | 0 | 0 | 29 (100%) |
| pT1aN1 | 1 | 0 | 1 (100%) | 0 |
| pT1bN1 | 2 | 0 | 1 (50%) | 1 (50%) |
| pT1cN1 | 6 | 0 | 0 | 6 (100%) |
| Surgical Modality | ||||
|---|---|---|---|---|
| Type of Resection N | VATS (Video-Assisted Thoracic Surgery) | Open Thoracotomy | VATS Converted to Open Thoracotomy | |
| Wedge | 20 | 13 (65%) | 5 (25%) | 2 (10%) |
| Segmentectomy | 48 | 30 (62.5%) | 13 (27%) | 5 (10.5%) |
| Lobectomy | 86 | 54 (62.8%) | 25 (29%) | 7 (8.2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hardavella, G.; Karampinis, I.; Anastasiou, N.; Stefanidis, K.; Tavernaraki, K.; Arapostathi, S.; Sidiropoulou, N.; Filippousis, P.; Patirelis, A.; Pompeo, E.; et al. Development of a Pulmonary Nodule Service and Clinical Pathway: A Pragmatic Approach Addressing an Unmet Need. Diagnostics 2025, 15, 1162. https://doi.org/10.3390/diagnostics15091162
Hardavella G, Karampinis I, Anastasiou N, Stefanidis K, Tavernaraki K, Arapostathi S, Sidiropoulou N, Filippousis P, Patirelis A, Pompeo E, et al. Development of a Pulmonary Nodule Service and Clinical Pathway: A Pragmatic Approach Addressing an Unmet Need. Diagnostics. 2025; 15(9):1162. https://doi.org/10.3390/diagnostics15091162
Chicago/Turabian StyleHardavella, Georgia, Ioannis Karampinis, Nikolaos Anastasiou, Konstantinos Stefanidis, Kyriaki Tavernaraki, Styliani Arapostathi, Nektaria Sidiropoulou, Petros Filippousis, Alexandro Patirelis, Eugenio Pompeo, and et al. 2025. "Development of a Pulmonary Nodule Service and Clinical Pathway: A Pragmatic Approach Addressing an Unmet Need" Diagnostics 15, no. 9: 1162. https://doi.org/10.3390/diagnostics15091162
APA StyleHardavella, G., Karampinis, I., Anastasiou, N., Stefanidis, K., Tavernaraki, K., Arapostathi, S., Sidiropoulou, N., Filippousis, P., Patirelis, A., Pompeo, E., Demertzis, P., & Elia, S. (2025). Development of a Pulmonary Nodule Service and Clinical Pathway: A Pragmatic Approach Addressing an Unmet Need. Diagnostics, 15(9), 1162. https://doi.org/10.3390/diagnostics15091162






