What the Radiologist Needs to Know About Sport Hernias: A Systematic Review of the Current Literature
Abstract
1. Introduction
- (1)
- Pinpoint tenderness during the palpation of the pubic tubercle at the conjoint tendon insertion.
- (2)
- Tenderness over the deep inguinal ring.
- (3)
- Pain and dilation of the external ring during the inspection maneuver in absence of a palpable hernia.
- (4)
- Pain during the palpation of the origin of the adductor longus tendon.
- (5)
- Dull, diffuse pain often radiating to the perineum, scrotum, and the inner thigh.
2. Material and Methods
2.1. Aim of the Current Systematic Review
2.2. Data Extraction and Quality Assessment
2.3. Search Strategy Items Details
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Statistical Analysis
2.7. Results of Systematic Review
2.8. Study Design
| Reference | Study Design | Level of Evidence | JBI Score | Risk of Bias | Synthesis of the Study |
|---|---|---|---|---|---|
| Bisciotti et al., 2023 [5] | Systematic review | I | 90/100 | Low | Groin Pain Syndrome Italian Consensus update 2023 |
| Paajanen et al., 2015 [6] | Systematic review | I | 78/100 | Low | Laparoscopic treatment of long-standing groin pain in athletic population |
| Jørgensen et al., 2019 [8] | Systematic review | I | 66/100 | Moderate | Treatment of longstanding groin pain syndrome |
| Kraeutler et al., 2021 [9] | Systematic review | I | 81/100 | Low | The difference in Terminology, Surgical Techniques, Preoperative Diagnostic Measures, and Geographic Differences in the Treatment of Athletic Pubalgia |
| Kopscik et al., 2023 [10] | Systematic review | I | 90/100 | Low | Sport hernia clinical approach |
| Bisciotti et al., 2016 [16] | Systematic review | I | 90/100 | Low | Groin Pain Syndrome Italian Consensus Conference on terminology, clinical evaluation, and imaging assessment in groin pain in athletes |
| Bisciotti et al., 2021 [19] | Systematic review | I | 89/100 | Low | The conservative treatment of longstanding adductor-related groin pain syndrome |
| Henriksen, 2016 [23] | Systematic review | I | 78/100 | Low | The systemic and local collagen turnover in hernia patients |
| Bracale et al., 2023 [25] | Systematic review | I | 90/100 | Low | The role of matrix metalloproteinases in the pathogenesis of inguinal hernias |
| Munegato et al., 2015 [28] | Systematic review | I | 65/100 | Moderate | The relationship between sports hernia and femoroacetabular impingement in athletes |
| Sheen et al., 2014 [29] | Systematic review | I | 81/100 | Low | The British Hernia Society’s 2014 position statement concerning the treatment of the sportsman’s groin’ based on the Manchester Consensus Conference |
| Swan and Wolcott, 2007 [42] | Systematic review | I | 75/100 | Low | Athletic hernia clinical description |
| Serafim et al., 2022 [46] | Systematic review | I | 74/100 | Moderate | The return to sport after conservative versus surgical treatment for pubalgia in athletes |
| Revzin et al., 2016 [51] | Systematic review | I | 83/100 | Low | The US examination of the inguinal canal and its correlation with CT and MR imaging |
| Hernia Surge Group, 2018 [52] | Systematic review | I | 90/100 | Low | International guidelines for groin hernia management |
| Caudill et al., 2008 [53] | Systematic review | I | 63/100 | Moderate | Clinical aspect of sport hernia |
| Ng et al., 2008 [54] | Systematic review | I | 73/100 | Moderate | The role of herniography in hernia assessment |
| Bisciotti et al., 2024 [55] | Systematic review | I | 91/100 | Low | The anatomical factors in inguinal-pubic-adductor area that may contribute to gender difference in susceptibility to groin pain syndrome |
| Castle et al., 2021 [45] | Retrospective case–control study | III | 76/100 | Low | The return to play rate following surgical management of athletic pubalgia in the national basketball population |
| Meyers et al., 2008 [81] | Retrospective case–control study | III | 71/100 | Moderate | Clinical experience concerning sport hernia |
| Zoga et al., 2008 [82] | Retrospective case–control study | III | 70/100 | Moderate | MRI findings concerning athletic pubalgia and sport hernia |
| Vasileff et al., 2017 [83] | Case–control study | III | 86/100 | Low | The role of dynamic ultrasound in sport hernia assessment |
| Fournier and Richon, 1993 [2] | Case series | IV | 71/100 | Moderate | Description of 25 patients surgically treated for sport hernia with the Nesovic technique |
| Van Meirhaeghe et al., 2019 [3] | Case series | IV | 81/100 | Low | The results of 10-year of Nesovic surgical procedure combined with adductor release for groin pain in 33 competitive athletes |
| Orchard et al., 1998 [11] | Case series | IV | 72/100 | Moderate | The role of ultrasound in inguinal canal posterior wall deficiency |
| Malycha and Lovell, 1992 [14] | Case series | IV | 79/100 | Low | Inguinal surgery in athletes with chronic groin pain |
| Hackney, 1993 [15] | Case series | IV | 71/100 | Moderate | The sports hernia: as a cause of chronic groin pain |
| Spangen et al., 1988 [18] | Case series | IV | 78/100 | Low | Non palpable inguinal hernia in the female population |
| Bisciotti et al., 2022 [20] | Case series | IV | 90/100 | Low | Multidisciplinary assessment of long-standing groin pain syndrome in athletic women in keeping with the Italian Consensus Agreement |
| Jorgenson et al., 2015 [26] | Case series | IV | 90/100 | Low | Genomic association for susceptibility loci underlying inguinal hernia. |
| Bisciotti et al., 2021 [33] | Case series | IV | 89/100 | Low | Multidisciplinary assessment of 320 athletes with long-standing groin pain syndrome in keeping with the Italian consensus agreement |
| Palumbo et al., 2022 [66] | Case series | IV | 74/100 | Moderate | Open surgery for sports |
| Robinson et al., 2006 [67] | Case series | IV | 80/100 | Low | Ultrasound examination for inguinal end femoral hernia |
| Ioffe et al., 2020 [68] | Case series | IV | 75/100 | Low | Magnetic resonance and ultrasound examination for sport hernia assessment in a football player population |
| van Wessem et al., 2003 [69] | Case series | IV | 81/100 | Low | The etiology of indirect inguinal hernias |
| van Veen et al., 2007 [70] | Case series | IV | 70/100 | Moderate | Patent processus vaginalis in the adult population as a risk factor for the indirect inguinal hernia |
| Wright et al., 2017 [71] | Case series | IV | 77/100 | Low | The neuropathy in primary inguinal hernia. |
| Meyers et al., 2000 [72] | Case series | IV | 73/100 | Moderate | Management of severe lower abdominal or inguinal pain in high-performance athletes. |
| Brennan et al., 2005 [73] | Case series | IV | 70/100 | Moderate | MRI assessment of secondary cleft sign as a marker of injury in athletes with groin pain syndrome |
| Falvey et al., 2016 [74] | Case series | IV | 77/100 | Low | Prospective anatomical diagnosis of 382 patients affected by athletic groin pain |
| Garner et al., 2006 [75] | Case series | IV | 73/100 | Moderate | The herniography examination in inguinal hernia assessment |
| Koch et al., 2005 [21] | Prospective study | IV | 85/100 | Low | Clinical evaluation of 6895 groin hernia repairs in women |
| Isik et al., 2017 [24] | Prospective study | IV | 89/100 | Low | The metalloproteinases inhibitors in patients with inguinal hernia |
| Dojčinović et al., 2012 [38] | Prospective study | IV | 84/100 | Low | Surgical treatment of chronic groin pain in athletes |
| Paajanen et al., 2011 [41] | Prospective study | IV | 90/100 | Low | Laparoscopic surgery for chronic groin pain in athletes compared to non-operative treatment |
| Robinson et al., 2015 [76] | Prospective study | IV | 72/100 | Moderate | MRI and ultrasound of the anterior pelvis and their correlation with clinical findings in a young football players population |
| Preskitt, 2011 [27] | Retrospective case series | IV | 65/100 | Moderate | The experience of Baylor University Medical Center of Dallas concerning sport hernia |
| Jain et al., 2010 [32] | Retrospective case series | IV | 80/100 | Low | Sport hernia in athletic population and its clinical presentation |
| Steele et al., 2004 [39] | Retrospective case series | IV | 65/100 | Moderate | Surgery for posterior inguinal wall weakness in athletes |
| Kajetanek et al., 2018 [44] | Retrospective case series | IV | 67/100 | Moderate | Return to play after targeted surgery for sport hernia |
| Kim B et al., 2015 [77] | Retrospective case series | IV | 80/100 | Low | Ultrasound examination in sport hernia |
| Garvey and Hazard, 2014 [78] | Retrospective case series | IV | 85/100 | Low | Sports hernia or groin disruption injury? Chronic athletic groin pain: a retrospective study of 100 patients with long-term follow-up |
| Lee et al., 2017 [7] | Clinical review | IV | 82/100 | Low | Magnetic resonance and ultrasound imaging in groin pain syndrome |
| Kavanagh et al., 2006 [12] | Clinical review | IV | 75/100 | Low | Magnetic resonance imaging in athletes affected by groin pain syndrome |
| Koulouris, 2008 [13] | Clinical review | IV | 90/100 | Low | Anatomic approach of imaging in groin pain in an elite athletic population |
| Elattar et al., 2016 [22] | Clinical review | IV | 64/10 | Moderate | Return to play after groin pain syndrome in the athletic population |
| Bisciotti et al., 2017 [67] | Observational cross-sectional study | IV | 85/100 | Low | The relationship between Cam morphology and inguinal pathologies |
| Bisciotti et al., 2018 [80] | Observational cross-sectional study | IV | 86/90 | lOW | Potential magnetic resonance imaging findings associated with inguinal hernia and inguinal canal posterior wall weakness in athletes |
| Bisciotti et al., 2024 [84] | Case report | IV | 80/100 | Low | The use of botulinum toxin in pre-pubic aponeurotic complex injuries |
| Nesovic, 1987 [1] | Narrative review | V | Not applicable | Not applicable | Treatment of groin pain syndrome I athletes |
| Zuckerbraun et al., 2020 [4] | Narrative review | V | Not applicable | Not applicable | Clinical assessment of sport hernias |
| Brown Aet al., 2013 [17] | Narrative review | V | Not applicable | Not applicable | Clinical concept concerning sport hernias |
| Balconi, 2011 [30] | Narrative review | V | Not applicable | Not applicable | Ultrasound examination in groin pain syndrome |
| Patel and Wright, 2021 [31] | Narrative review | V | Not applicable | Not applicable | Clinical controversies in inguinal hernia clinical assessment |
| Bisciotti et al., 2022 [34] | Narrative review | V | Not applicable | Not applicable | The prepubic aponeurotic complex injuries |
| Thorborg, 2023 [35] | Narrative review | V | Not applicable | Not applicable | Clinical concepts for adductor strains and long-standing adductor-related groin pain |
| Via et al., 2018 [36] | Narrative review | V | Not applicable | Not applicable | Management of osteitis pubis in athletes |
| Anderson, 2016 [37] | Narrative review | V | Not applicable | Not applicable | Diagnosis and treatment of iliopsoas: pathology |
| Minnich et al., 2011 [40] | Narrative review | V | Not applicable | Not applicable | The minimal surgical repair technique for sport hernias |
| Choi et al., 2016 [43] | Narrative review | V | Not applicable | Not applicable | Return to play after sports hernia surgery |
| Bisciotti et al., 2024 [47] | Narrative review | V | Not applicable | Not applicable | The role of magnetic resonance imaging in groin pain syndrome in athletes |
| Bou Antoun et al., 2018 [56] | Narrative review | V | Not applicable | Not applicable | The role of imaging in inguinal-related groin pain in athletes |
| Gamborg et al., 2019 [57] | Narrative review | V | Not applicable | Not applicable | Anatomical and clinical differences between inguinal hernia and sport hernia |
| Dimitrakopoulou and, Schilders, 2016 [58] | Narrative review | V | Not applicable | Not applicable | Anatomical and clinical definition of sport hernia |
| Omar et al., 2008 [59] | Narrative review | V | Not applicable | Not applicable | MRI assessment of athletes affected by athletic pubalgia and sport hernia |
| Shortt et al. 2008 [60] | Narrative review | V | Not applicable | Not applicable | Anatomy, pathology, and MRI assessment in subjects affected by sport hernia |
| Rabe and Gretchen, 2010 [61] | Narrative review | V | Not applicable | Not applicable | Treatment and prevention of athletic pubalgia |
| Mullens et al., 2012 [62] | Narrative review | V | Not applicable | Not applicable | MRI technique in athletic pubalgia and sport hernia |
| Palisch et al., 2013 [63] | Narrative review | V | Not applicable | Not applicable | Clinical and therapeutic correlations between imaging and core injuries |
| Moeller, 2007 [64] | Narrative review | V | Not applicable | Not applicable | Clinical concept concerning sport hernia |
| Chopra and Robinson, 2016 [65] | Narrative review | V | Not applicable | Not applicable | The role of imaging in groin pain syndrome in athletic population |
3. Results
3.1. Definition of the Term Sport Hernia
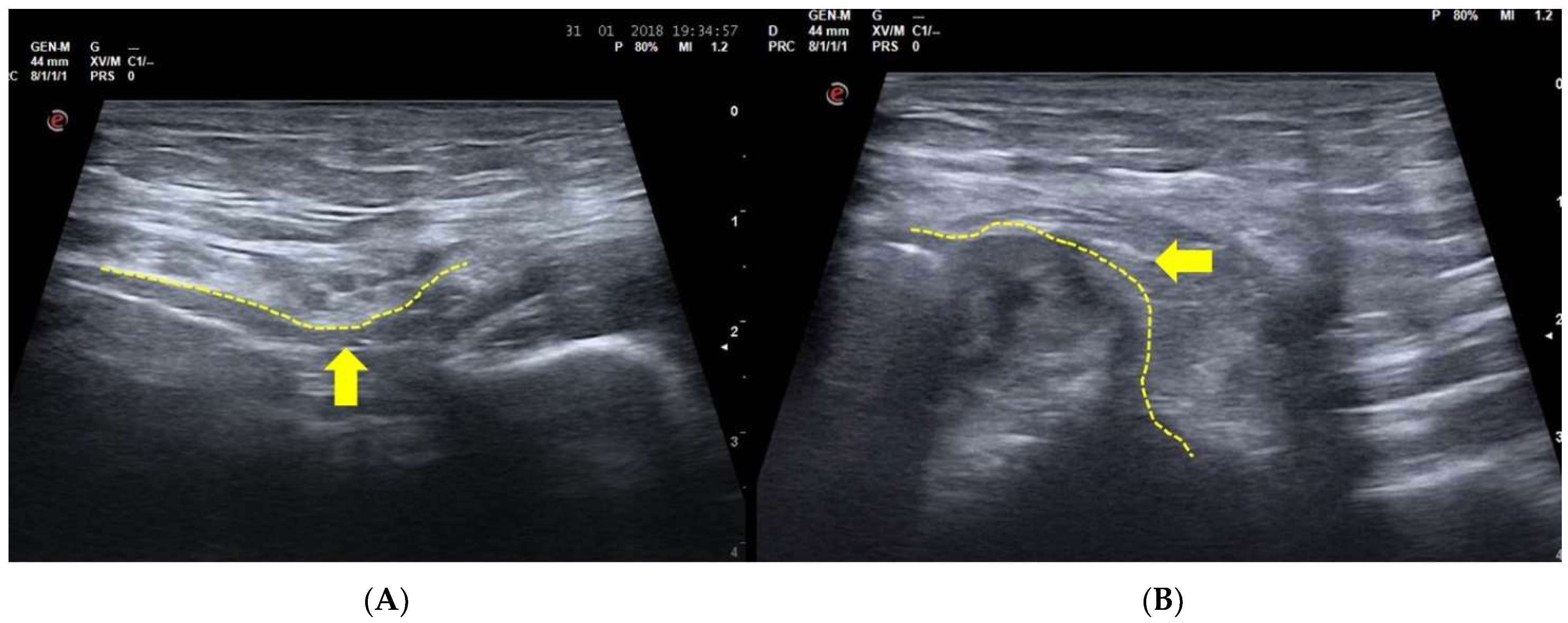
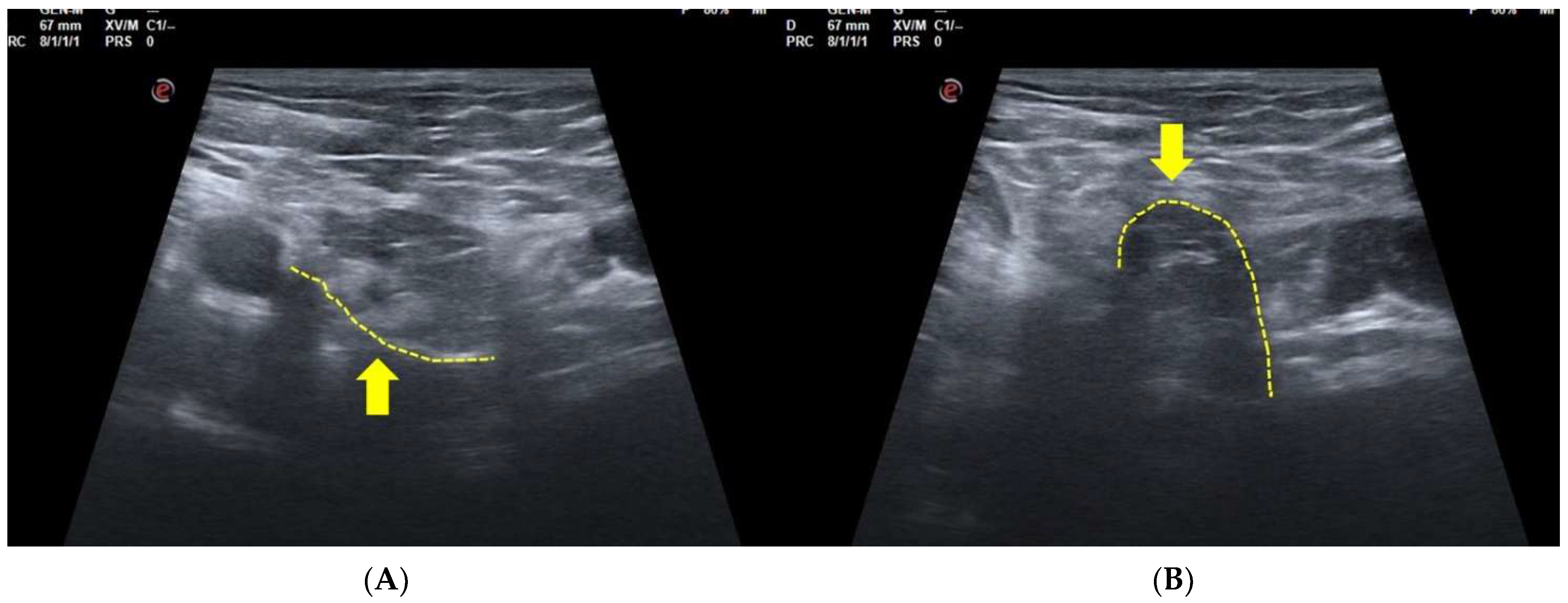
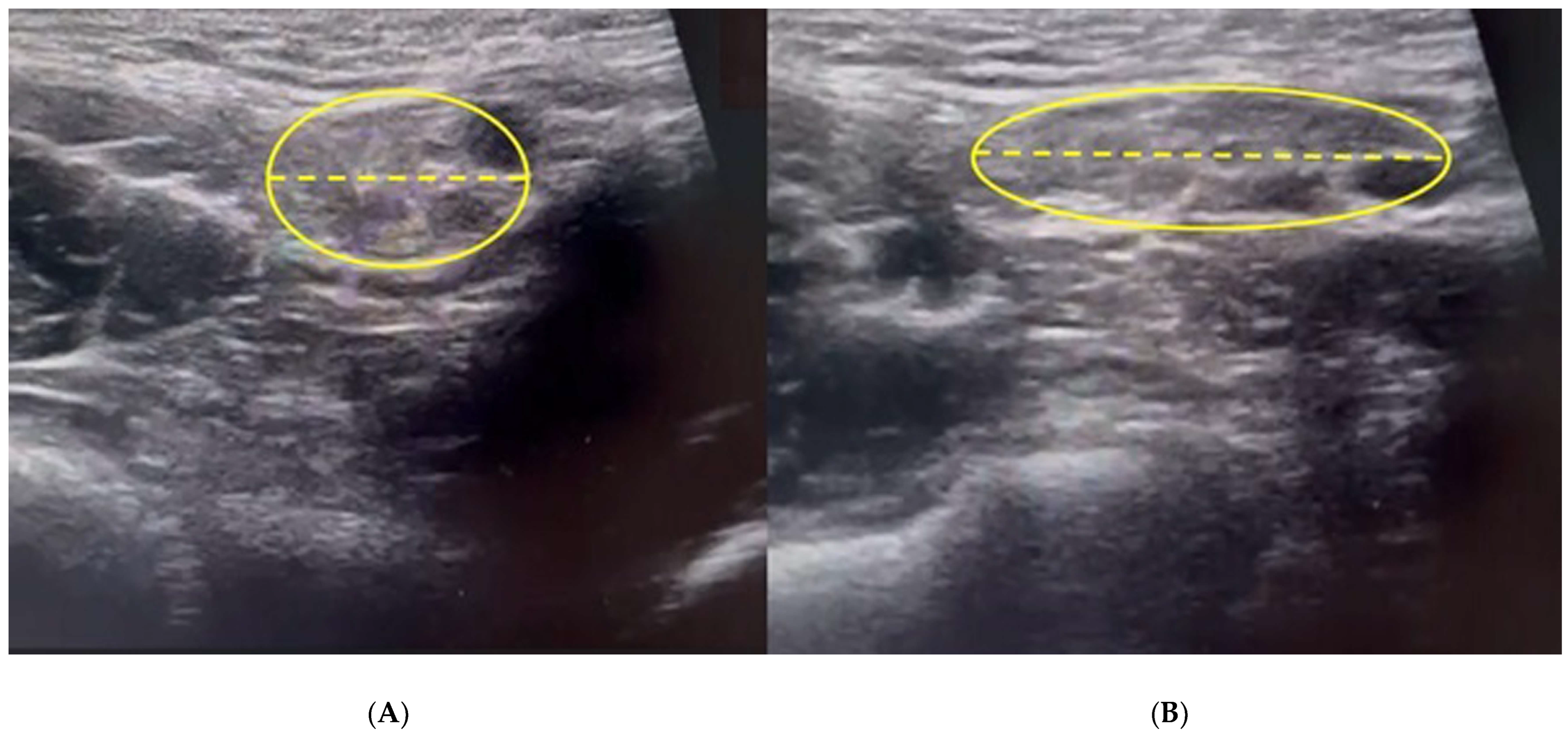
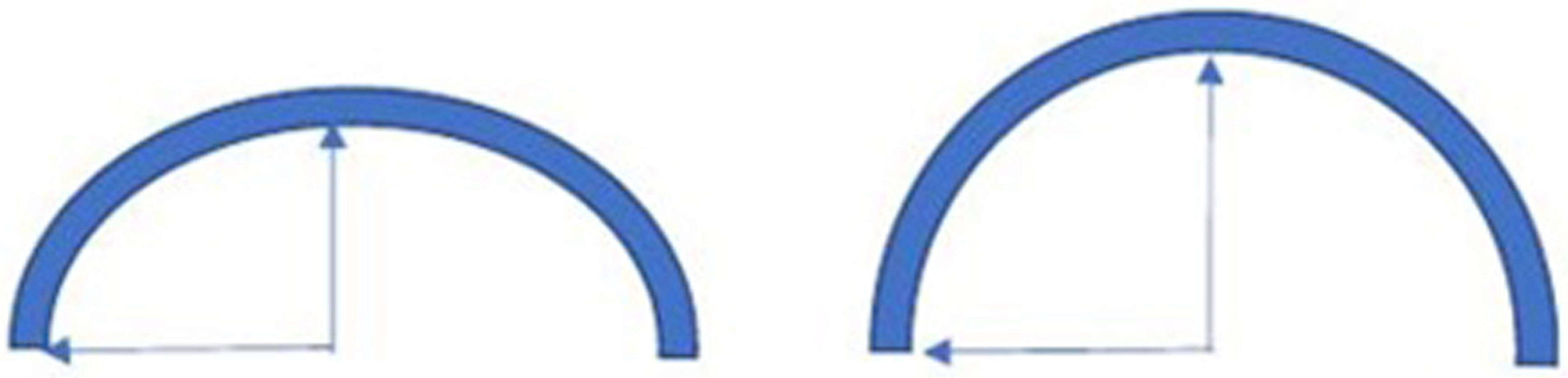
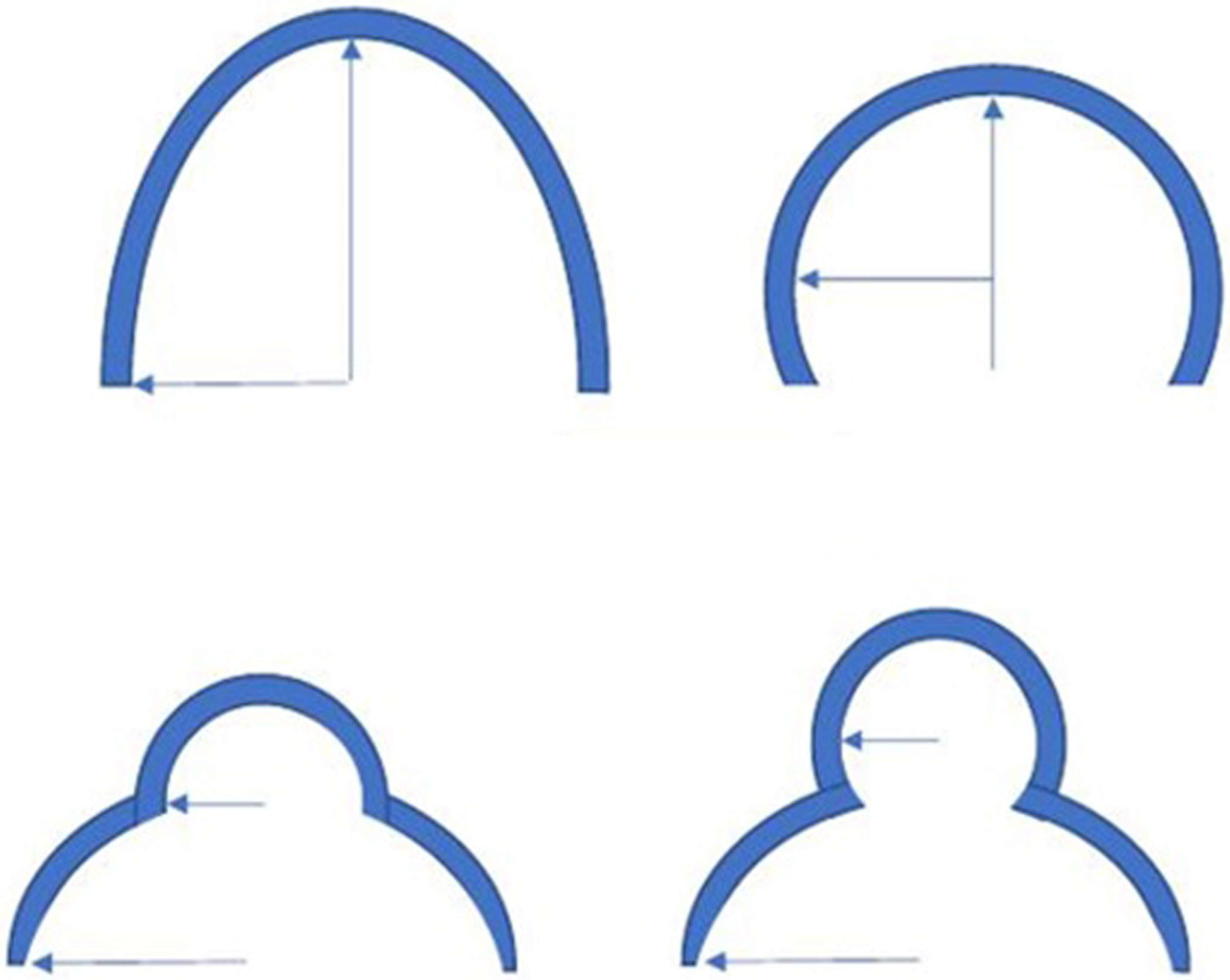
3.2. Dynamic Ultrasonography Examination
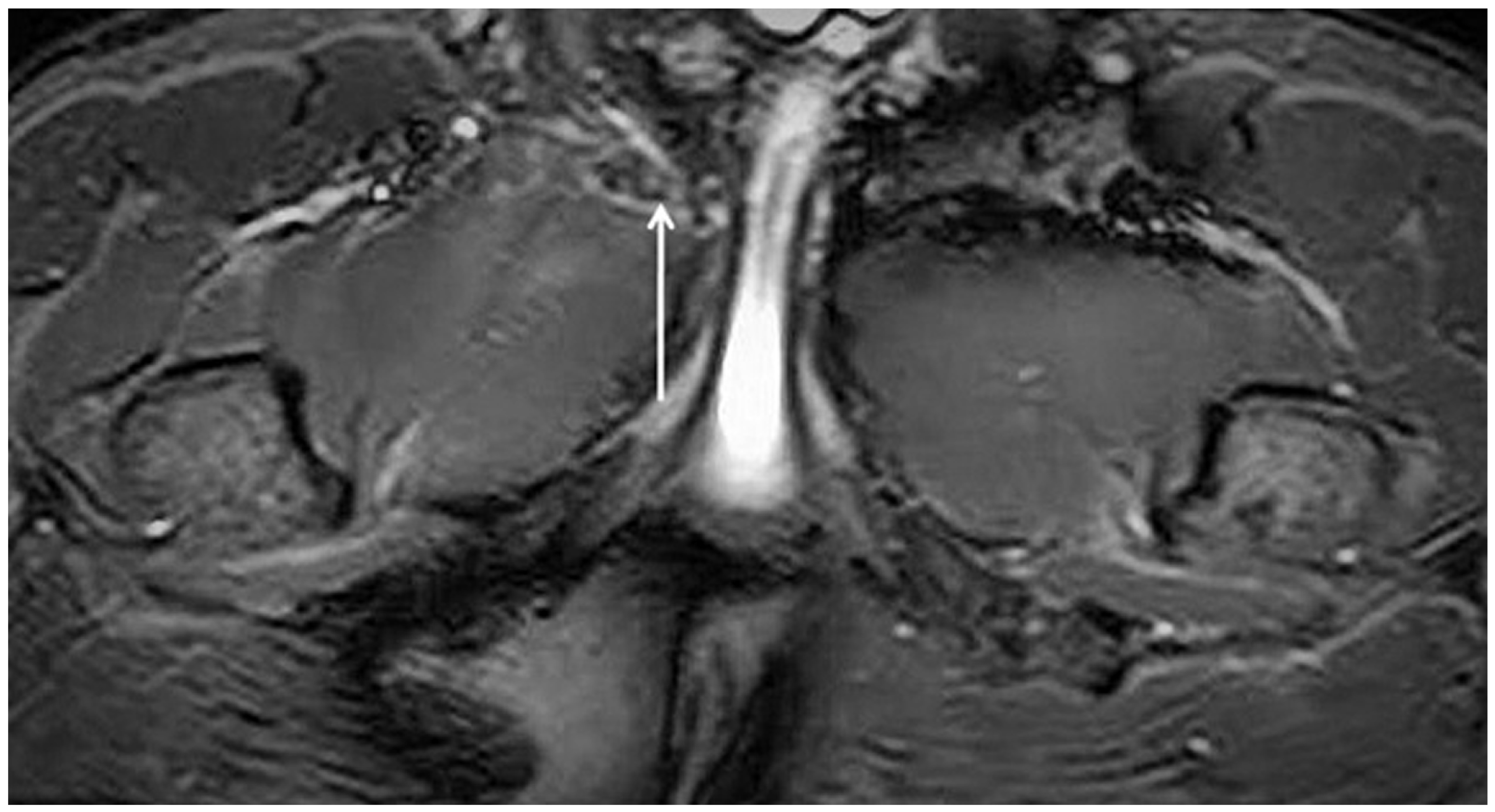
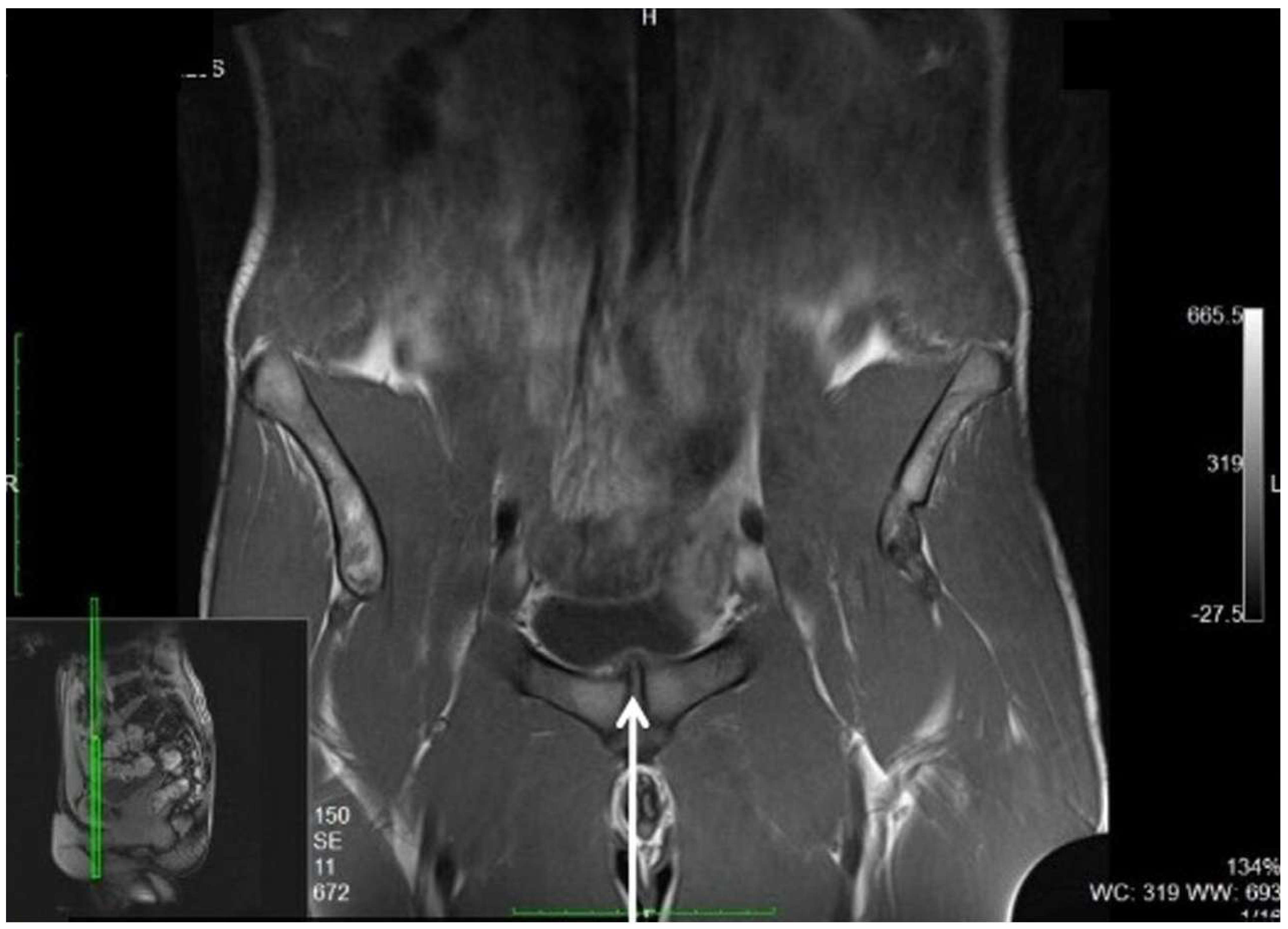
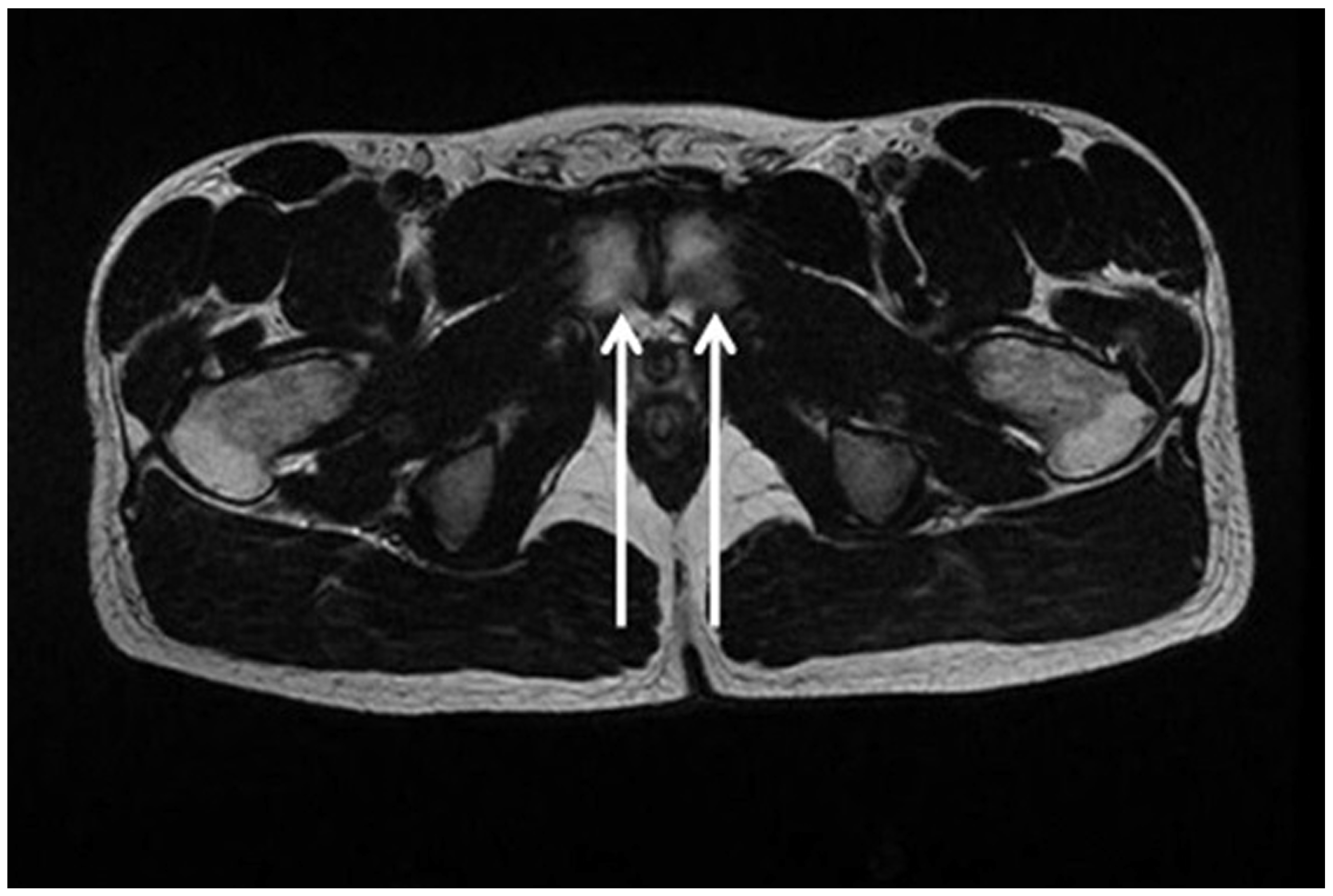
3.3. Magnetic Resonance Imaging
- (i)
- (ii)
- (iii)
- (i)
- The poor validity of MRI in the diagnosis of inguinal hernias and SH due to problems inherent to the Valsalva maneuver [56].
- (ii)
- (iii)
- The different diagnostic approaches to GPS shown by different authors can be explained, at least partially, both by the fact that the diagnostic approach was performed on different sporting cohorts and/or graphical populations, and by the notable difference in the interpretation of the clinical examinations [74].
3.4. Herniography
3.5. Other Imaging Techniques
3.6. What Does the Radiologist Look for to Define SH and GPS?
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nesovic, B. Bolni sindrom simfeze kod sportista i mogucnosti njegovog lecenja. In: Povrede u sportu i njihovo lecenje. In Zdravstvena Kimosija SFKJ; Nacionalna i Univerzitetski Biblioteka: Bosna i Hercegovina, Sarajevo, 1987. [Google Scholar]
- Fournier, J.Y.; Richon, C.A. Revue critique de 25 patients traités pour pubalgie par myorraphie inguinale (opération de Nesovic) [Critical review of 25 patients treated for pubic pain with inguinal myorrhaphy (Nesovic operation)]. Helv. Chir. Acta. 1993, 59, 775–778. (In French) [Google Scholar] [PubMed]
- Van Meirhaeghe, J.P.; Vanden Berghe, A.; Houben, R.; Petre, D. 10-year results of the Nesovic procedure combined with adductor release for groin pain in 33 competitive athletes. Acta Orthop. Belg. 2019, 85, 169–181. [Google Scholar] [PubMed]
- Zuckerbraun, B.S.; Cyr, A.R.; Mauro, C.S. Groin Pain Syndrome Known as Sports Hernia: A Review. JAMA Surg. 2020, 155, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Bisciotti, G.N.; Zini, R.; Aluigi, M.; Aprato, A.; Auci, A.; Bellinzona, E.; Benelli, P.; Bigoni, M.; Bisciotti, A.; Bisciotti, A.; et al. Groin Pain Syndrome Italian Consensus Conference update 2023. J. Sports Med. Phys. Fit. 2024, 64, 402–414. [Google Scholar] [CrossRef] [PubMed]
- Paajanen, H.; Montgomery, A.; Simon, T.; Sheen, A.J. Systematic review: Laparoscopic treatment of long-standing groin pain in athletes. Br. J. Sports Med. 2015, 49, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Endo, Y.; Potter, H.G. Imaging of Groin Pain: Magnetic Resonance and Ultrasound Imaging Features. Sports Health 2017, 9, 428–435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jørgensen, S.G.; Öberg, S.; Rosenberg, J. Treatment of longstanding groin pain: A systematic review. Hernia 2019, 23, 1035–1044. [Google Scholar] [CrossRef] [PubMed]
- Kraeutler, M.J.; Mei-Dan, O.; Belk, J.W.; Larson, C.M.; Talishinskiy, T.; Scillia, A.J. A Systematic Review Shows High Variation in Terminology, Surgical Techniques, Preoperative Diagnostic Measures, and Geographic Differences in the Treatment of Athletic Pubalgia/Sports Hernia/Core Muscle Injury/Inguinal Disruption. Arthroscopy 2021, 37, 2377–2390.e2. [Google Scholar] [CrossRef] [PubMed]
- Kopscik, M.; Crisman, J.L.; Lomasney, L.; Smith, S.; Jadidi, S. Sports Hernias: A Comprehensive Review for Clinicians. Cureus 2023, 15, e43283. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Orchard, J.W.; Read, J.W.; Neophyton, J.; Garlick, D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br. J. Sports Med. 1998, 32, 134–139. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kavanagh, E.C.; Koulouris, G.; Ford, S.; McMahon, P.; Johnson, C.; Eustace, S.J. MR imaging of groin pain in the athlete. Semin. Musculoskelet. Radiol. 2006, 10, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Koulouris, G. Imaging review of groin pain in elite athletes: An anatomic approach to imaging findings. Am. J. Roentgenol. 2008, 191, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Malycha, P.; Lovell, G. Inguinal surgery in athletes with chronic groin pain: The ‘sportsman’s’ hernia. Astralian New Zealand J. Surg. 1992, 62, 123–125. [Google Scholar] [CrossRef] [PubMed]
- Hackney, R.G. The sports hernia: A cause of chronic groin pain. Br. J. Sports Med. 1993, 27, 58–62. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bisciotti, G.N.; Volpi, P.; Zini, R.; Auci, A.; Aprato, A.; Belli, A.; Bellistri, G.; Benelli, P.; Bona, S.; Bonaiuti, D.; et al. Groin Pain Syndrome Italian Consensus Conference on terminology, clinical evaluation and imaging assessment in groin pain in athlete. BMJ Open Sport Exerc. Med. 2016, 2, e000142, Erratum in BMJ Open Sport Exerc. Med. 2017, 2, e000142corr1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brown, A.; Abrahams, S.; Remedios, D.; Chadwick, S.J. Sports hernia: A clinical update. Br. J. Gen. Pract. 2013, 63, e235–e237. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Spangen, L.; Andersson, R.; Ohlsson, L. Non-palpable inguinal-hernia in the female. Am. Surg. 1988, 54, 574–577. [Google Scholar] [PubMed]
- Bisciotti, G.N.; Chamari, K.; Cena, E.; Garcia, G.R.; Vuckovic, Z.; Bisciotti, A.; Bisciotti, A.; Zini, R.; Corsini, A.; Volpi, P. The conservative treatment of longstanding adductor-related groin pain syndrome: A critical and systematic review. Biol. Sport 2021, 38, 45–63. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bisciotti, G.N.; Auci, A.; Bona, S.; Bisciotti, A.; Bisciotti, A.; Cassaghi, G.; DI Marzo, F.; DI Pietto, F.; Eirale, C.; Panascì, M.; et al. Long-standing groin pain syndrome in athletic women: A multidisciplinary assessment in keeping with the Italian Consensus Agreement. J. Sports Med. Phys. Fit. 2022, 62, 1199–1210. [Google Scholar] [CrossRef] [PubMed]
- Koch, A.; Edwards, A.; Haapaniemi, S.; Nordin, P.; Kald, A. Prospective evaluation of 6895 groin hernia repairs in women. Br. J. Surg. 2005, 92, 1553–1558. [Google Scholar] [CrossRef] [PubMed]
- Elattar, O.; Choi, H.-R.; Dills, V.D.; Busconi, B. Groin Injuries (Athletic Pubalgia) and Return to Play. Sports Health 2016, 8, 313–323. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Henriksen, N.A. Systemic and local collagen turnover in hernia patients. Dan. Med. J. 2016, 63, B5265. [Google Scholar] [PubMed]
- Isik, A.; Gursul, C.; Peker, K.; Aydın, M.; Fırat, D.; Yılmaz, I. Metalloproteinases and Their Inhibitors in Patients with Inguinal Hernia. World J. Surg. 2017, 41, 1259–1266. [Google Scholar] [CrossRef] [PubMed]
- Bracale, U.; Peltrini, R.; Iacone, B.; Martirani, M.; Sannino, D.; Gargiulo, A.; Corcione, F.; Serra, R.; Bracale, U.M. A Systematic Review on the Role of Matrix Metalloproteinases in the Pathogenesis of Inguinal Hernias. Biomolecules 2023, 13, 1123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jorgenson, E.; Makki, N.; Shen, L.; Chen, D.C.; Tian, C.; Eckalbar, W.L.; Hinds, D.; Ahituv, N.; Avins, A. A genome-wide association study identifies four novel susceptibility loci underlying inguinal hernia. Nat. Commun. 2015, 6, 10130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Preskitt, J.T. Sports hernia: The experience of Baylor University Medical Center at Dallas. Proc. (Bayl. Univ. Med. Cent) 2011, 24, 89–91. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Munegato, D.; Bigoni, M.; Gridavilla, G.; Olmi, S.; Cesana, G.; Zatti, G. Sports hernia and femoroacetabular impingement in athletes: A systematic review. World J. Clin. Cases 2015, 3, 823–830. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sheen, A.J.; Stephenson, B.M.; Lloyd, D.M.; Robinson, P.; Fevre, D.; Paajanen, H.; de Beaux, A.; Kingsnorth, A.; Gilmore, O.J.; Bennett, D.; et al. ‘Treatment of the sportsman’s groin’: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. Br. J. Sports Med. 2013, 48, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Balconi, G. US in pubalgia. J. Ultrasound 2011, 14, 157–166. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, V.H.; Wright, A.S. Controversies in Inguinal Hernia. Surg. Clin. N. Am. 2021, 101, 1067–1079. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Tantia, O.; Sasmal, P.; Khanna, S.; Sen, B. Chronic Groin Pain in Athletes: Sportsman’s Hernia with Bilateral Femoral Hernia. Indian J. Surg. 2010, 72, 343–346. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bisciotti, G.N.; Auci, A.; Bona, S.; Bisciotti, A.; Bisciotti, A.; Cassaghi, G.; DI Marzo, F.; DI Pietto, F.; Eirale, C.; Panascì, M.; et al. A multidisciplinary assessment of 320 athletes with long-standing groin pain syndrome in keeping with the Italian consensus agreement: The high incidence and the multiple causes of inguinal and hip pathologies and pubic osteopathy. J. Sports Med. Phys. Fit. 2021, 61, 960–970. [Google Scholar] [CrossRef] [PubMed]
- Bisciotti, A.; Bisciotti, G.N.; Eirale, C.; Bisciotti, A.; Auci, A.; Bona, S.; Zini, R. Prepubic aponeurotic complex injuries: A structured narrative review. J. Sports Med. Phys. Fit. 2022, 62, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Thorborg, K. Current Clinical Concepts: Exercise and Load Management of Adductor Strains, Adductor Ruptures, and Long-Standing Adductor-Related Groin Pain. J. Athl. Train. 2023, 58, 589–601. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Via, A.G.; Frizziero, A.; Finotti, P.; Oliva, F.; Randelli, F.; Maffulli, N. Management of osteitis pubis in athletes: Rehabilitation and return to training—A review of the most recent literature. Open Access J. Sports Med. 2018, 10, 1–10. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anderson, C.N. Iliopsoas: Pathology, Diagnosis, and Treatment. Clin. Sports Med. 2016, 35, 419–433. [Google Scholar] [CrossRef] [PubMed]
- Dojčinović, B.; Šebečić, B.; Starešinić, M.; Janković, S.; Japjec, M.; Čuljak, V. Surgical treatment of chronic groin pain in athletes. Int. Orthop. 2012, 36, 2361–2365. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Steele, P.; Annear, P.; Grove, J.R. Surgery for posterior inguinal wall deficiency in athletes. J. Sci. Med. Sport 2004, 7, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Minnich, J.M.; Hanks, J.B.; Muschaweck, U.; Brunt, L.M.; Diduch, D.R. Sports hernia: Diagnosis and treatment highlighting a minimal repair surgical technique. Am. J. Sports Med. 2011, 39, 1341–1349. [Google Scholar] [CrossRef] [PubMed]
- Paajanen, H.; Brinck, T.; Hermunen, H.; Airo, I. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: A randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia). Surgery 2011, 150, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Swan, K.G.; Wolcott, M. The athletic hernia: A systematic review. Clin. Orthop. Relat. Res. 2007, 455, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.R.; Elattar, O.; Dills, V.D.; Busconi, B. Return to Play After Sports Hernia Surgery. Clin. Sports Med. 2016, 35, 621–636. [Google Scholar] [CrossRef] [PubMed]
- Kajetanek, C.; Benoît, O.; Granger, B.; Menegaux, F.; Chereau, N.; Pascal-Mousselard, H.; Khiami, F. Athletic pubalgia: Return to play after targeted surgery. Orthop. Traumatol. Surg. Res. 2018, 104, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Castle, J.P.; Kessler, A.; Abbas, M.J.; Wager, S.; Khalil, L.S.; Okoroha, K.R.; Mehran, N. High Return to Play Rate and Reduced Career Longevity Following Surgical Management of Athletic Pubalgia in National Basketball Association Players. Arthrosc. Sports Med. Rehabil. 2021, 3, e1359–e1365. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Serafim, T.T.; Oliveira, E.S.; Migliorini, F.; Maffulli, N.; Okubo, R. Return to sport after conservative versus surgical treatment for pubalgia in athletes: A systematic review. J. Orthop. Surg. Res. 2022, 17, 484. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bisciotti, G.N.; Di Pietto, F.; Rusconi, G.; Bisciotti, A.; Auci, A.; Zappia, M.; Romano, S. The Role of MRI in Groin Pain Syndrome in Athletes. Diagnostics 2024, 14, 814. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barker, T.H.; Stone, J.C.; Sears, K.; Klugar, M.; Leonardi-Bee, J.; Tufanaru, C.; Aromataris, E.; Munn, Z. Revising the JBI quantitative critical appraisal tools to improve their applicability: An overview of methods and the development process. JBI Evid. Synth. 2023, 21, 478–493. [Google Scholar] [CrossRef] [PubMed]
- Schiavenato, M.; Chu, F. PICO: What it is and what it is not. Nurse Educ. Pract. 2021, 56, 103194. [Google Scholar] [CrossRef] [PubMed]
- Dimitrakopoulou, A.; Schilders, E. Sportsman’s hernia? An ambiguous term. J. Hip Preserv. Surg. 2016, 3, 16–22. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mullens, F.E.; Zoga, A.C.; Morrison, W.B.; Meyers, W.C. Review of MRI technique and imaging findings in athletic pubalgia and the “sports hernia”. Eur. J. Radiol. 2012, 81, 3780–3792. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.; Hensor, E.; Lansdown, M.J.; Ambrose, N.S.; Chapman, A.H. Inguinofemoral hernia: Accuracy of sonography in patients with indeterminate clinical features. Am. J. Roentgenol. 2006, 187, 1168–1178. [Google Scholar] [CrossRef] [PubMed]
- Bisciotti, G.N.; Di Marzo, F.; Auci, A.; Parra, F.; Cassaghi, G.; Corsini, A.; Petrera, M.; Volpi, P.; Vuckovic, Z.; Panascì, M.; et al. Cam morphology and inguinal pathologies: Is there a possible connection? J. Orthop. Traumatol. 2017, 18, 439–450. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zoga, A.C.; Kavanagh, E.C.; Omar, I.M.; Morrison, W.B.; Koulouris, G.; Lopez, H.; Chaabra, A.; Domesek, J.; Meyers, W.C. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology 2008, 247, 797–807. [Google Scholar] [CrossRef] [PubMed]
- Revzin, M.V.; Ersahin, D.; Israel, G.M.; Kirsch, J.D.; Mathur, M.; Bokhari, J.; Scoutt, L.M. US of the Inguinal Canal: Comprehensive Review of Pathologic Processes with CT and MR Imaging Correlation. RadioGraphics 2016, 36, 2028–2048. [Google Scholar] [CrossRef] [PubMed]
- Caudill, P.; Nyland, J.; Smith, C.; Yerasimides, J.; Lach, J. Sports hernias: A systematic literature review. Br. J. Sports Med. 2008, 42, 954–964. [Google Scholar] [CrossRef] [PubMed]
- Omar, I.M.; Zoga, A.C.; Kavanagh, E.C.; Koulouris, G.; Bergin, D.; Gopez, A.G.; Morrison, W.B.; Meyers, W.C. Athletic pubalgia and “sports hernia”: Optimal MR imaging technique and findings. RadioGraphics 2008, 28, 1415–1438. [Google Scholar] [CrossRef] [PubMed]
- Meyers, W.C.; Foley, D.P.; Garrett, W.E.; Lohnes, J.H.; Mandlebaum, B.R. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am. J. Sports Med. 2000, 28, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Falvey, É.C.; King, E.; Kinsella, S.; Franklyn-Miller, A. Athletic groin pain (part 1): A prospective anatomical diagnosis of 382 patients—clinical findings, MRI findings and patient-reported outcome measures at baseline. Br. J. Sports Med. 2016, 50, 423–430. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garner, J.P.; Patel, S.; Glaves, J.; Ravi, K. Is herniography useful? Hernia 2006, 10, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.; Grainger, A.J.; Hensor, E.M.; Batt, M.E.; O’Connor, P.J. Do MRI and ultrasound of the anterior pelvis correlate with, or predict, young football players’ clinical findings? A 4-year prospective study of elite academy soccer players. Br. J. Sports Med. 2015, 49, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Robinson, P.; Modi, H.; Gupta, H.; Horgan, K.; Achuthan, R. Evaluation of the usage and influence of groin ultrasound in primary and secondary healthcare settings. Hernia 2015, 19, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Meyers, W.C.; McKechnie, A.; Philippon, M.J.; Horner, M.A.; Zoga, A.C.; Devon, O.N. Experience with “sports hernia” spanning two decades. Ann. Surg. 2008, 248, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Bisciotti, G.N.; Alessio, A.; Bisciotti, A.; Bisciotti, A. The Use of Botulinum Toxin in Pre-Pubic Aponeurotic Complex Injuries: A Case Report. J. Orthop. Case Rep. 2024, 14, 60–66. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hernia Surge Group. International guidelines for groin hernia management. Hernia 2018, 22, 1–165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bisciotti, G.N.; Bisciotti, A.; Auci, A.; Bisciotti, A.; Volpi, P. Anatomical Features in Inguinal-Pubic-Adductor Area That May Contribute to Gender Difference in Susceptibility to Groin Pain Syndrome. J. Pers. Med. 2024, 14, 860. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shortt, C.P.; Zoga, A.C.; Kavanagh, E.C.; Meyers, W.C. Anatomy, pathology, and MRI findings in the sports hernia. Semin. Musculoskelet. Radiol. 2008, 12, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Palisch, A.; Zoga, A.C.; Meyers, W.C. Imaging of athletic pubalgia and core muscle injuries: Clinical and therapeutic correlations. Clin. Sports Med. 2013, 32, 427–447. [Google Scholar] [CrossRef] [PubMed]
- Moeller, J.L. Sportsman’s hernia. Curr. Sports Med. Rep. 2007, 6, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Chopra, A.; Robinson, P. Imaging Athletic Groin Pain. Radiol. Clin. N. Am. 2016, 54, 865–873. [Google Scholar] [CrossRef] [PubMed]
- van Wessem, K.J.P.; Simons, M.P.; Plaisier, P.W.; Lange, J.F. The etiology of indirect inguinal hernias: Congenital and/or acquired? Hernia 2003, 7, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.; Born, D.E.; D’souza, N.; Hurd, L.; Gill, R.; Wright, D. Pain and compression neuropathy in primary inguinal hernia. Hernia 2017, 21, 715–722. [Google Scholar] [CrossRef] [PubMed]
- Garvey, J.F.; Hazard, H. Sports hernia or groin disruption injury? Chronic athletic groin pain: A retrospective study of 100 patients with long-term follow-up. Hernia 2014, 18, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Bisciotti, G.N.; Auci, A.; Cena, E.; Corsini, A.; Bisciotti, A.; Zini, R.; Eirale, C.; Parra, F.; Gassaghi, G.; Di Marzo, F.; et al. Potential MRI findings associated with inguinal hernia and inguinal canal posterior wall weakness in athletes. Muscles Ligaments Tendons J. 2018, 8, 290–304. [Google Scholar]
- Bou Antoun, M.B.; Reboul, G.; Ronot, M.; Crombe, A.; Poussange, N.; Pesquer, L. Imaging of inguinal-related groin pain in athletes. Br. J. Radiol. 2018, 91, 20170856. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gamborg, S.; Öberg, S.; Hölmich, P.; Skjoldby, B.; Rosenberg, J. [Sports hernia is not a hernia]. Ugeskr Laeger. 2019, 181, V01190018. (In Danish) [Google Scholar] [PubMed]
- Palumbo, P.; Massimi, F.; Lucchese, S.; Grimaldi, S.; Vernaccini, N.; Cirocchi, R.; Sorrenti, S.; Usai, S.; Intini, S.G. Open Surgery for Sportsman’s Hernia a Retrospective Study. Front. Surg. 2022, 9, 893390. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ng, T.T.; Hamlin, J.A.; Kahn, A.M. Herniography: Analysis of its role and limitations. Hernia 2009, 13, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Ioffe, O.Y.; Negria, N.M.; Omelchenko, A.V.; Stetsenko, O.P.; Dibrova, Y.A.; Kryvopustov, M.S.; Tsiura, Y.P.; Tarasiuk, T.V. Mri and ultrasound criteria for the diagnosis of a sports hernia in football players. Wiad Lek. 2020, 73, 755–760. [Google Scholar] [CrossRef] [PubMed]
- van Veen, R.N.; van Wessem, K.J.P.; Halm, J.A.; Simons, M.P.; Plaisier, P.W.; Jeekel, J.; Lange, J.F. Patent processus vaginalis in the adult as a risk factor for the occurrence of indirect inguinal hernia. Surg. Endosc. 2007, 21, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Brennan, D.; O’Connell, M.J.; Ryan, M.; Cunningham, P.; Taylor, D.; Cronin, C.; O’Neill, P.; Eustace, S. Secondary cleft sign as a marker of injury in athletes with groin pain: MR image appearance and interpretation. Radiology 2005, 235, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Rabe, S.B.; Gretchen, D.O. Athletic pubalgia: Recognition, treatment, and prevention: A review of the literature. Athl. Train. Sports Health Care 2010, 2, 25–30. [Google Scholar] [CrossRef]
- Vasileff, W.K.; Nekhline, M.; Kolowich, P.A.; Talpos, G.B.; Eyler, W.R.; van Holsbeeck, M. Inguinal Hernia in Athletes: Role of Dynamic Ultrasound. Sports Health 2017, 9, 414–421. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bisciotti, G.N.; Bisciotti, A.; Bisciotti, A.; Auci, A. What the Radiologist Needs to Know About Sport Hernias: A Systematic Review of the Current Literature. Diagnostics 2025, 15, 785. https://doi.org/10.3390/diagnostics15060785
Bisciotti GN, Bisciotti A, Bisciotti A, Auci A. What the Radiologist Needs to Know About Sport Hernias: A Systematic Review of the Current Literature. Diagnostics. 2025; 15(6):785. https://doi.org/10.3390/diagnostics15060785
Chicago/Turabian StyleBisciotti, Gian Nicola, Andrea Bisciotti, Alessandro Bisciotti, and Alessio Auci. 2025. "What the Radiologist Needs to Know About Sport Hernias: A Systematic Review of the Current Literature" Diagnostics 15, no. 6: 785. https://doi.org/10.3390/diagnostics15060785
APA StyleBisciotti, G. N., Bisciotti, A., Bisciotti, A., & Auci, A. (2025). What the Radiologist Needs to Know About Sport Hernias: A Systematic Review of the Current Literature. Diagnostics, 15(6), 785. https://doi.org/10.3390/diagnostics15060785




