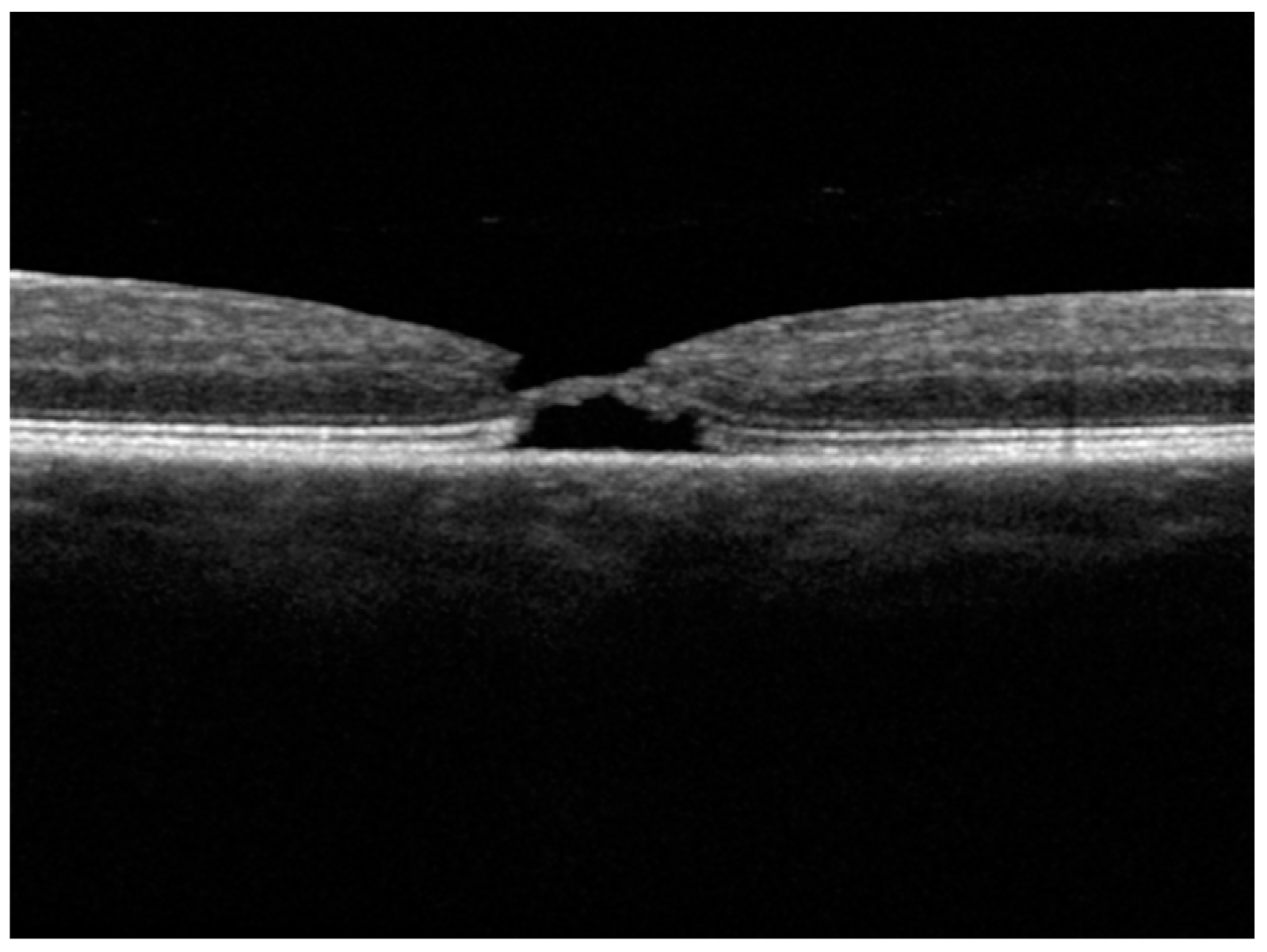
Spontaneously Opening and Closing Macular Holes with Lamellar Hole Epiretinal Proliferation: A Longitudinal Optical Coherence Tomography Analysis
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Case Reports
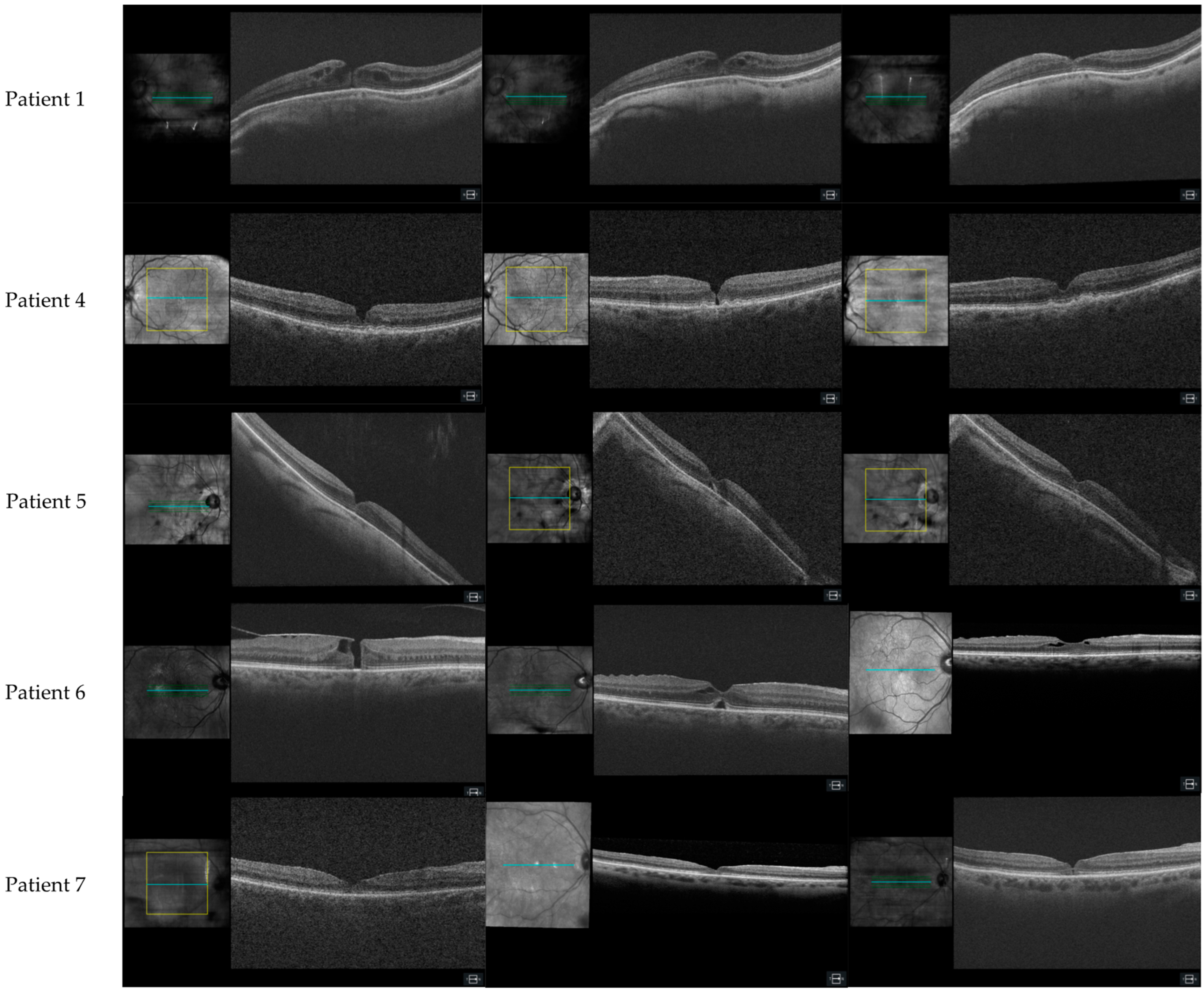
3.1.1. Patient 1, Left Eye
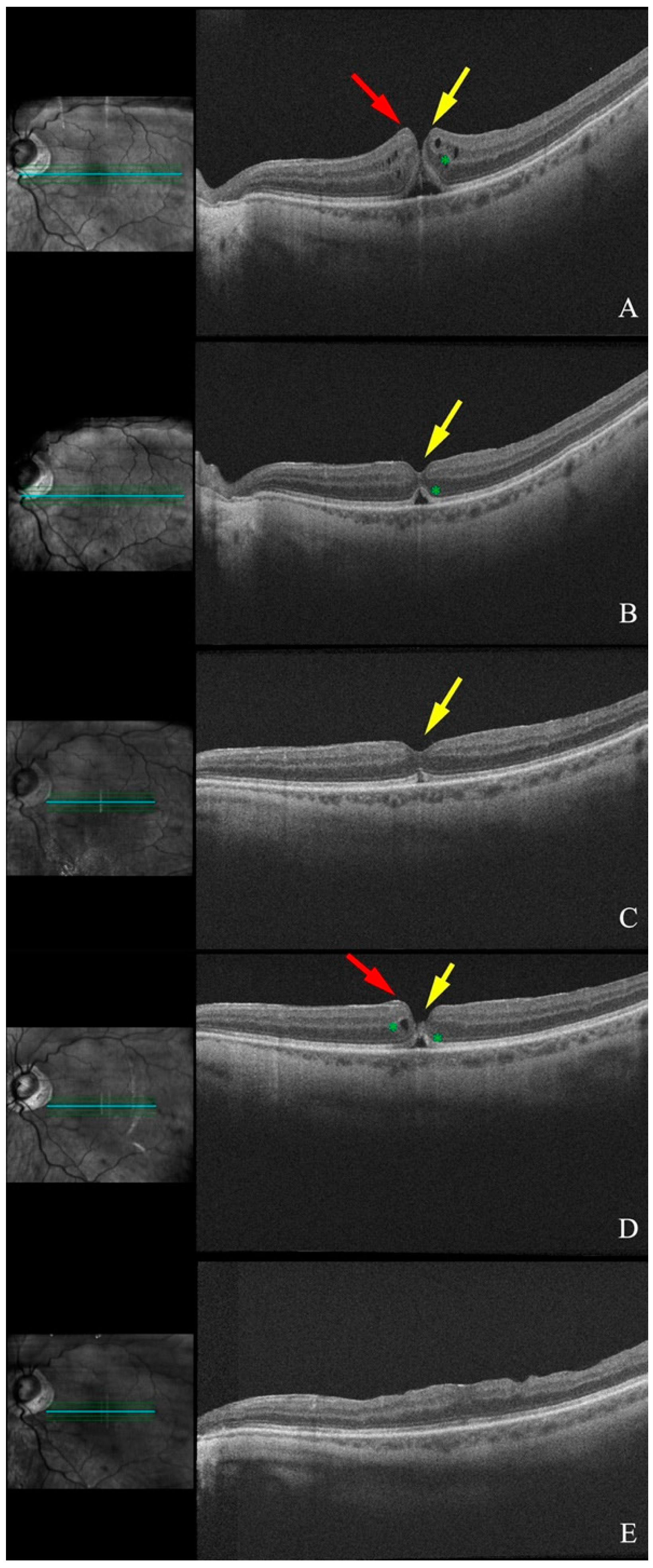
3.1.2. Patient 2, Left Eye
3.1.3. Patient 3, Left Eye
3.1.4. Patient 4, Left Eye
3.1.5. Patient 5, Right Eye
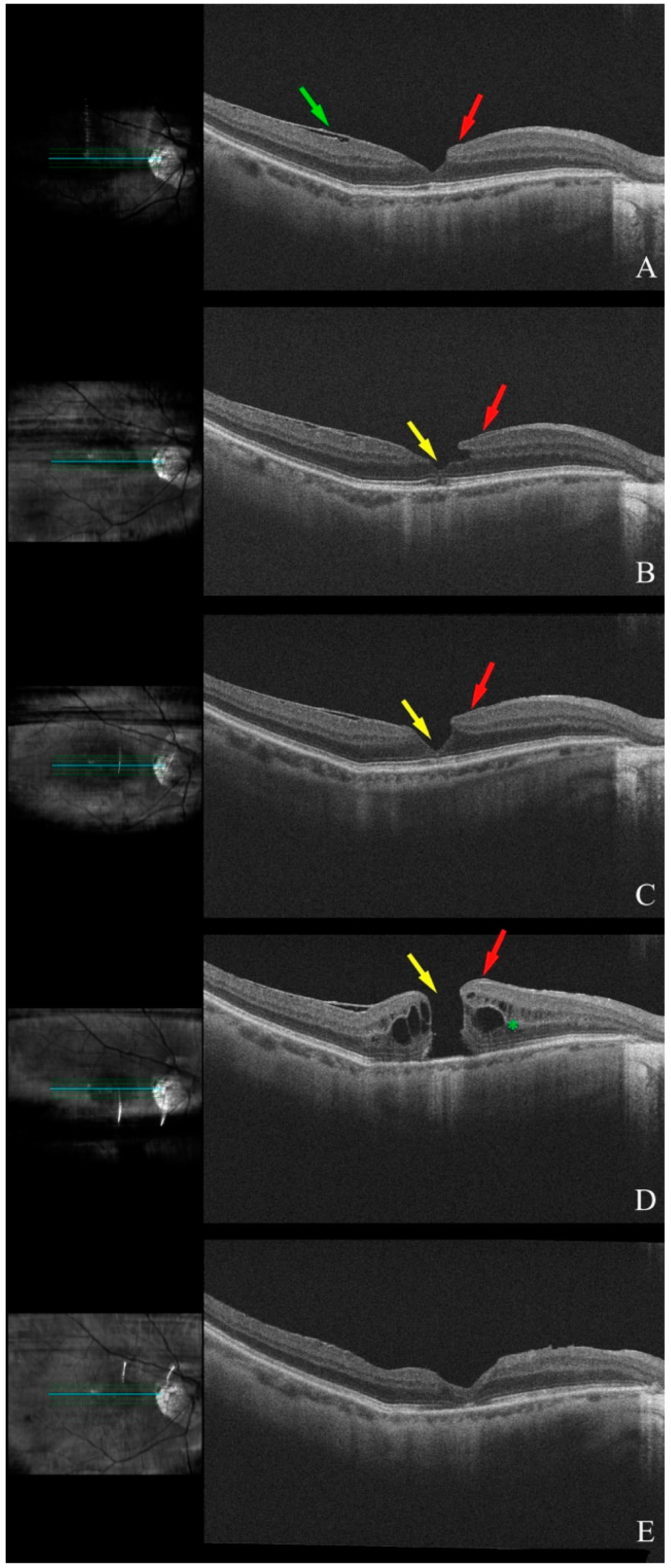
3.1.6. Patient 6, Right Eye
3.1.7. Patient 7, Right Eye
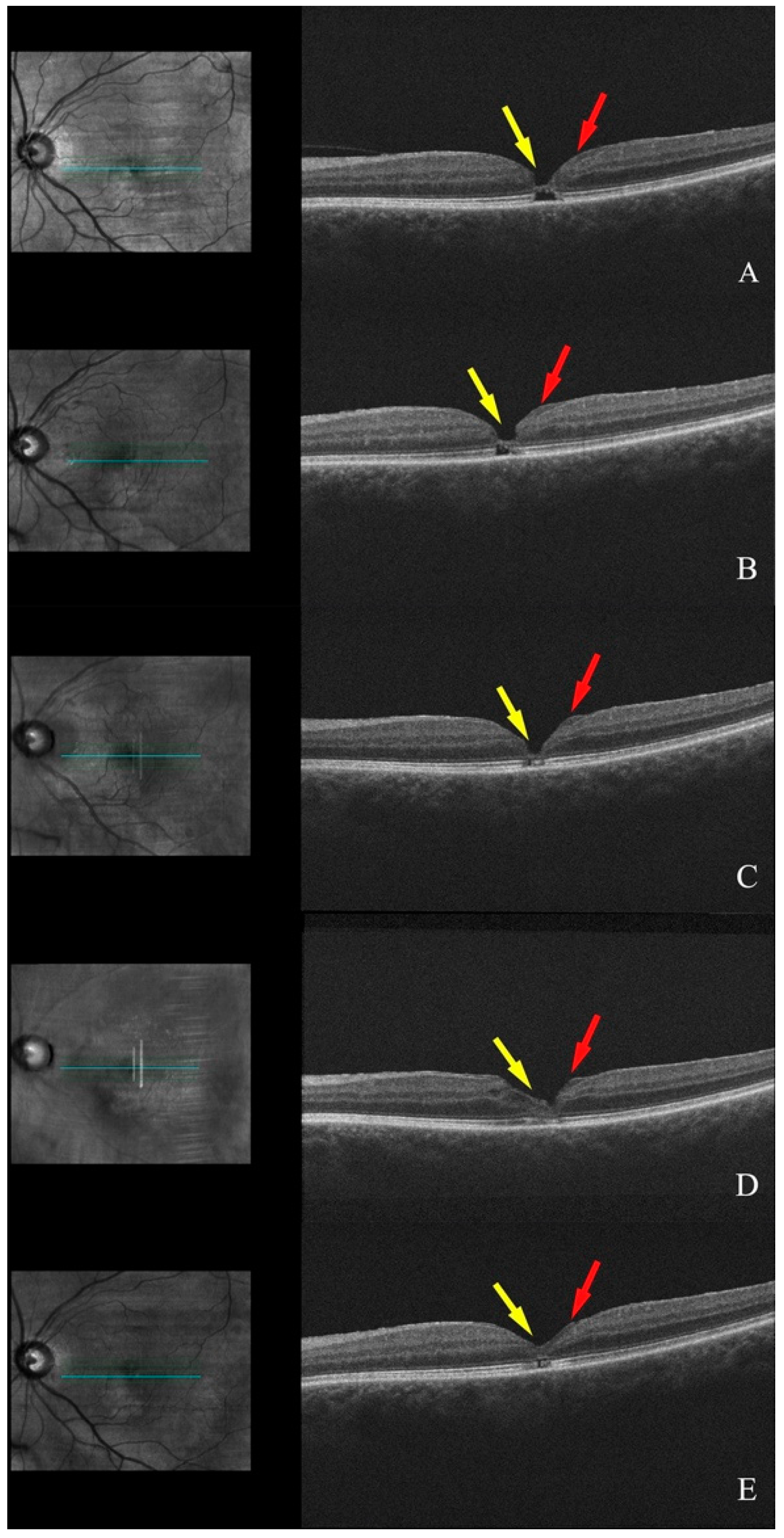
3.1.8. Patient 8, Right Eye
3.2. Analysis of Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LHEP | Lamellar hole epiretinal proliferation |
| FTMH | Full-thickness macular hole |
| LMH | Lamellar macular hole |
| VMT | Vitreomacular traction |
| ERM | Epiretinal membrane |
| SD-OCT | Spectral domain optical coherence tomography |
| CME | Cystoid macular edema |
| ELM | External limiting membrane |
| EZ | Ellipsoid zone |
| ONL | Outer nuclear layer |
| PVD | Posterior vitreous detachment |
| ILM | Inner limiting membrane |
| BCVA | Best-corrected visual acuity |
| OD | Right eye |
| OS | Left eye |
| POAG | Primary open angle glaucoma |
| CSR | Central serous retinopathy |
| AMD | Age-related macular degeneration |
Appendix A
References
- Duker, J.S.; Kaiser, P.K.; Binder, S.; de Smet, M.D.; Gaudric, A.; Reichel, E.; Sadda, S.R.; Sebag, J.; Spaide, R.F.; Stalmans, P. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013, 120, 2611–2619. [Google Scholar] [CrossRef]
- Chen, Q.; Liu, Z.X.; Azzolini, C. Idiopathic Macular Hole: A Comprehensive Review of Its Pathogenesis and of Advanced Studies on Metamorphopsia. J. Ophthalmol. 2019, 2019, 7294952. [Google Scholar] [CrossRef]
- Freeman, W.R.; Azen, S.P.; Kim, J.W.; El-Haig, W.; Mishell Iii, D.R.; Bailey, I. Vitrectomy for the Treatment of Full-Thickness Stage 3 or 4 Macular Holes Results of a Multicentered Randomized Clinical Trial. Ophthalmology 1997, 115, 11–21. [Google Scholar]
- Ezra, E.; Gregor, Z.J. Surgery for Idiopathic Full-Thickness Macular Hole Two-Year Results of a Randomized Clinical Trial Comparing Natural History, Vitrectomy, and Vitrectomy Plus Autologous Serum: Moorfields Macular Hole Study Group Report No. 1. Arch. Ophthalmol. 2004, 122, 224–236. [Google Scholar] [CrossRef]
- Liang, X.; Liu, W.; Ohira, A. Characteristics and Risk Factors for Spontaneous Closure of Idiopathic Full-Thickness Macular Hole. J. Ophthalmol. 2019, 2019, 4793764. [Google Scholar] [CrossRef]
- Pang, C.E.; Spaide, R.F.; Freund, K.B. Epiretinal proliferation seen in association with lamellar macular holes: A distinct clinical entity. Retina 2014, 34, 1513–1523. [Google Scholar] [CrossRef]
- Pang, C.E.; Maberley, D.A.; Bailey Freund, K.; White, V.A.; Rasmussen, S.; Matsubara, J.A. Clinicopathologic Correlation Lamellar Hole-associated epiretinal proliferation: A clinicopathologic correlation. Retina 2016, 36, 1408–1412. [Google Scholar] [CrossRef]
- Compera, D.; Schumann, R.G.; Cereda, M.G.; Acquistapace, A.; Lita, V.; Priglinger, S.G.; Staurenghi, G.; Bottoni, F. Progression of lamellar hole-associated epiretinal proliferation and retinal changes during long-term follow-up. Br. J. Ophthalmol. 2018, 102, 84–90. [Google Scholar] [CrossRef]
- Compera, D.; Entchev, E.; Haritoglou, C.; Mayer, W.J.; Hagenau, F.; Ziada, J.; Kampik, A.; Schumann, R.G. Correlative microscopy of lamellar hole-associated epiretinal proliferation. J. Ophthalmol. 2015, 2015, 450212. [Google Scholar] [CrossRef]
- Preti, R.C.; Zacharias, L.C.; Cunha, L.P.; Monteiro, M.L.R.; Sarraf, D. Spontaneous closure of degenerative lamellar macular hole with epiretinal membrane proliferation. Int. J. Retin. Vitr. 2021, 7, 64. [Google Scholar] [CrossRef]
- Watanabe, M.; Yokota, H.; Aso, H.; Hanazaki, H.; Hanaguri, J.; Yamagami, S.; Nagaoka, T. Development of Stage 4 Macular Hole after Spontaneous Closure in a Patient with Stage 2 Macular Hole and a Lamellar Macular Hole-Associated Epiretinal Proliferation. Case Rep. Ophthalmol. 2021, 12, 481–484. [Google Scholar] [CrossRef]
- Okubo, A.; Unoki, K.; Yamakiri, K.; Sameshima, M.; Sakamoto, T. Early structural changes during spontaneous closure of idiopathic full-thickness macular hole determined by optical coherence tomography: A case report. BMC Res. Notes 2013, 6, 396. [Google Scholar] [CrossRef]
- Michalewska, Z.; Cisiecki, S.; Sikorski, B.; Michalewski, J.; Kałużny, J.J.; Wojtkowski, M.; Nawrocki, J. Spontaneous closure of stage III and IV idiopathic full-thickness macular holes—A two-case report. Graefes Arch. Clin. Exp. Ophthalmol. 2008, 246, 99–104. [Google Scholar] [CrossRef]
- Morawski, K.; Kubicka-trza, A.; Romanowska-dixon, Z. The analysis of spontaneous closure mechanisms and regeneration of retinal layers of a full-thickness macular hole; Relationship with visual acuity improvement. Retina 2016, 36, 2132–2139. [Google Scholar] [CrossRef]
- García Fernández, M.; Castro Navarro, J. Spontaneous closure of stage IV idiopathic full-thickness macular hole and late reopening as a lamellar macular hole: A case report. J. Med. Case Rep. 2012, 6, 169. [Google Scholar] [CrossRef]
- Yamada, H.; Sakai, A.; Yamada, E.; Nishimura, T.; Matsumura, M. Spontaneous Closure of Traumatic Macular Hole. Spontaneous Clos. Trauma. Macular Hole 2002, 234, 340347. [Google Scholar] [CrossRef]
- Parolini, B.; Schumann, R.G.; Cereda, M.G.; Haritoglou, C.; Pertile, G. Lamellar Macular Hole: A Clinicopathologic Correlation of Surgically Excised Epiretinal Membranes. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9074. [Google Scholar] [CrossRef]
- Tadayoni, R.; Massin, P.; Haouchine, B.; Cohen, D.; Erginay, A.; Gaudric, A. Spontaneous resolution of small stage 3 and 4 full-thickness macular holes viewed by optical coherence tomography. Retina 2001, 21, 186–189. [Google Scholar] [CrossRef]
- Bringmann, A.; Duncker, T.; Jochmann, C.; Barth, T.; Duncker, G.I.W.; Wiedemann, P. Spontaneous closure of small full-thickness macular holes: Presumed role of Müller cells. Acta Ophthalmol. 2020, 98, e447–e456. [Google Scholar] [CrossRef]
- Bringmann, A.; Syrbe, S.; Görner, K.; Kacza, J.; Francke, M.; Wiedemann, P.; Reichenbach, A. The primate fovea: Structure, function and development. Prog. Retin. Eye Res. 2018, 66, 49–84. [Google Scholar] [CrossRef]
- Takahashi, H.; Kishi, S. Optical coherence tomography images of spontaneous macular hole closure. Am. J. Ophthalmol. 1999, 128, 519–520. [Google Scholar] [CrossRef]
- Preti, R.C.; Zacharias, L.C.; Cunha, L.P.; Monteiro, M.L.R.; Sarraf, D. Spontaneous macular hole closure after posterior vitreous detachment in an eye with hyperreflective OCT stress line. Am. J. Ophthalmol. Case Rep. 2020, 20, 100950. [Google Scholar] [CrossRef]
- Ozgonul, C.; Besirli, C.G. Macular hole closure following spontaneous release of vitreomacular traction. BMJ Case Rep. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Privat, E.; Tadayoni, R.; Gaucher, D.; Haouchine, B.; Massin, P.; Gaudric, A. Residual Defect in the Foveal Photoreceptor Layer Detected by Optical Coherence Tomography in Eyes with Spontaneously Closed Macular Holes. Am. J. Ophthalmol. 2007, 143, 814–819. [Google Scholar] [CrossRef]
- Chehaibou, I.; Manoharan, N.; Govetto, A.; Tsui, I.; Hubschman, J.P. Spontaneous lamellar macular holes closure. Retin. Cases Brief Rep. 2022, 16, 397–400. [Google Scholar] [CrossRef]
- Lenkowski, J.R.; Raymond, P.A. Müller glia: Stem cells for generation and regeneration of retinal neurons in teleost fish. Prog. Retin. Eye Res. 2014, 40, 94–123. [Google Scholar] [CrossRef]
| Patient | Sex | Age | Eye | Initial BCVA | Final BCVA 1 | Lens (Phakic, Pseudophakic) | Ocular History |
|---|---|---|---|---|---|---|---|
| 1 | F | 71 | OS | 20/100 | 20/100 | Pseudophakic | POAG, myopia, FTMH OD |
| 2 | M | 77 | OS | 20/60 | 20/30 | Pseudophakic | Acute anterior uveitis, POAG, retinal detachment OD |
| 3 | F | 78 | OS | 20/20 | 20/20 | Phakic | Cataract, CSR, FTMH OD |
| 4 | F | 82 | OS | 20/30 | 20/20 | Phakic | Cataract, dry AMD, FTMH OD |
| 5 | M | 70 | OD | 20/60 | 20/40 | Pseudophakic | POAG, myopia |
| 6 | F | 73 | OD | 20/50 | 20/40 | Phakic | Narrow angle glaucoma |
| 7 | F | 72 | OD | 20/40 | 20/30 | Pseudophakic | Birdshot chorioretinopathy |
| 8 | F | 73 | OD | 20/40 | 20/40 | Pseudophakic | None |
| Patient | PVD Before Diagnosis | PVD After Diagnosis | VMT | ERM | LHEP | CME | Hole Type | Hole Width 1 (µm) | Closing Time (Weeks) | Time to Recurrence (Months) | ONL Bridge | ONL Integrity Reconstruction | ELM Integrity Reconstruction | EZ Integrity Reconstruction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | No | No | Yes | Yes | Yes | Yes | FTMH | 30 | 4 | - | Yes | Yes | No | No |
| 2 | Complete | - | No | Yes | Yes | Yes | FTMH | 50 | 24 | 12 | Yes | Yes | Yes | Yes |
| 3 | Partial | Complete | No | Yes | Yes | No | FTMH | 270 | 73 | - | Yes | Yes | No | No |
| 4 | Complete | - | No | Yes | Yes | No | FTMH | 230 | 24 | - | Yes | Yes | Yes | Yes |
| 5 | Complete | - | No | Yes | Yes | No | LMH | 180 | 5 | - | Yes | Yes | Yes | Yes |
| 6 | Partial | Complete | No | Yes | Yes | Yes | FTMH | 230 | 14 | - | Yes | Yes | Yes | Yes |
| 7 | Complete | - | No | Yes | Yes | No | LMH | 210 | 12 | 2 | No | Yes | Yes | No |
| 8 | Complete | - | No | Yes | Yes | Yes | LMH | 370 | 4 | 4 | No | Yes | No | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moussa, O.; Golebka, J.; Gomide, G.; Koenigstein, D.; Shih, H.; Chen, R.W.S. Spontaneously Opening and Closing Macular Holes with Lamellar Hole Epiretinal Proliferation: A Longitudinal Optical Coherence Tomography Analysis. Diagnostics 2025, 15, 759. https://doi.org/10.3390/diagnostics15060759
Moussa O, Golebka J, Gomide G, Koenigstein D, Shih H, Chen RWS. Spontaneously Opening and Closing Macular Holes with Lamellar Hole Epiretinal Proliferation: A Longitudinal Optical Coherence Tomography Analysis. Diagnostics. 2025; 15(6):759. https://doi.org/10.3390/diagnostics15060759
Chicago/Turabian StyleMoussa, Omar, Jedrzej Golebka, Gabriel Gomide, Dvir Koenigstein, Hueyjong Shih, and Royce W. S. Chen. 2025. "Spontaneously Opening and Closing Macular Holes with Lamellar Hole Epiretinal Proliferation: A Longitudinal Optical Coherence Tomography Analysis" Diagnostics 15, no. 6: 759. https://doi.org/10.3390/diagnostics15060759
APA StyleMoussa, O., Golebka, J., Gomide, G., Koenigstein, D., Shih, H., & Chen, R. W. S. (2025). Spontaneously Opening and Closing Macular Holes with Lamellar Hole Epiretinal Proliferation: A Longitudinal Optical Coherence Tomography Analysis. Diagnostics, 15(6), 759. https://doi.org/10.3390/diagnostics15060759






