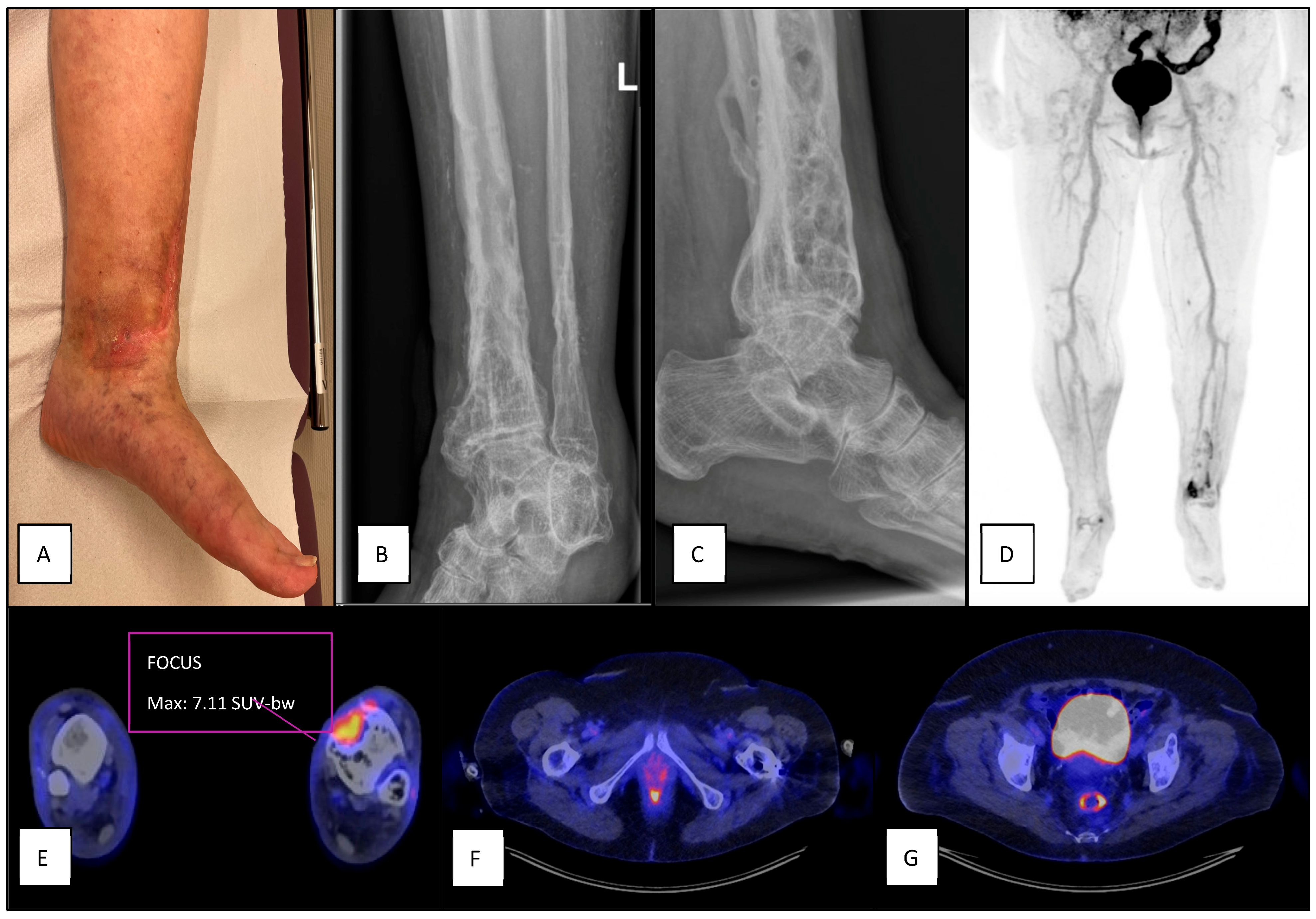
Diagnostic Value of Increased [18F]FDG Uptake in Locoregional Lymph Nodes on PET/CT in Patients with Suspected Fracture-Related Infection
Abstract
1. Introduction
2. Materials and Methods
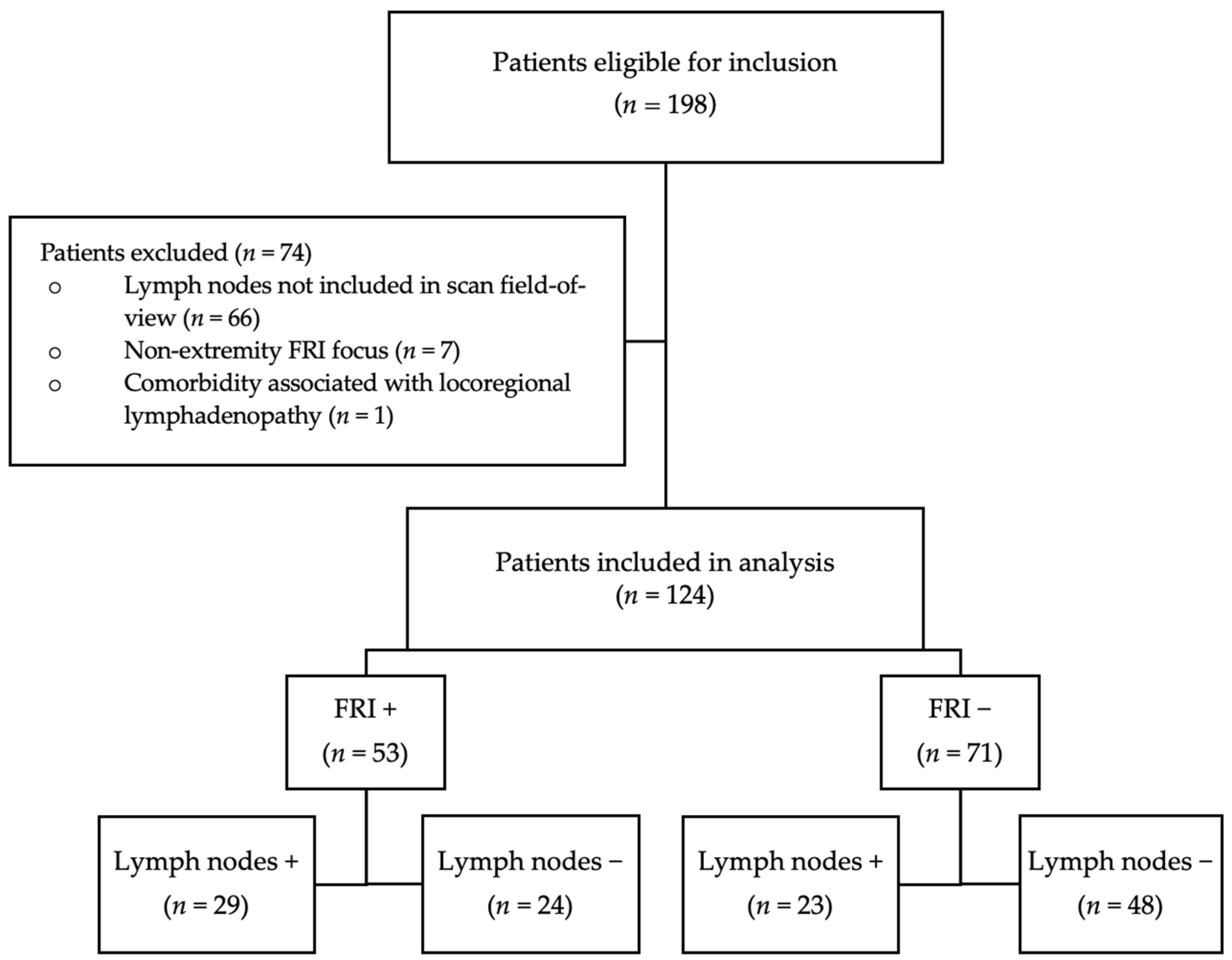
2.1. Study Design and Population
2.2. Exclusion Criteria
2.3. Patient Information
2.4. FDG-PET/CT Acquisition and Assessment
2.5. Reference Test
2.6. Statistical Analysis
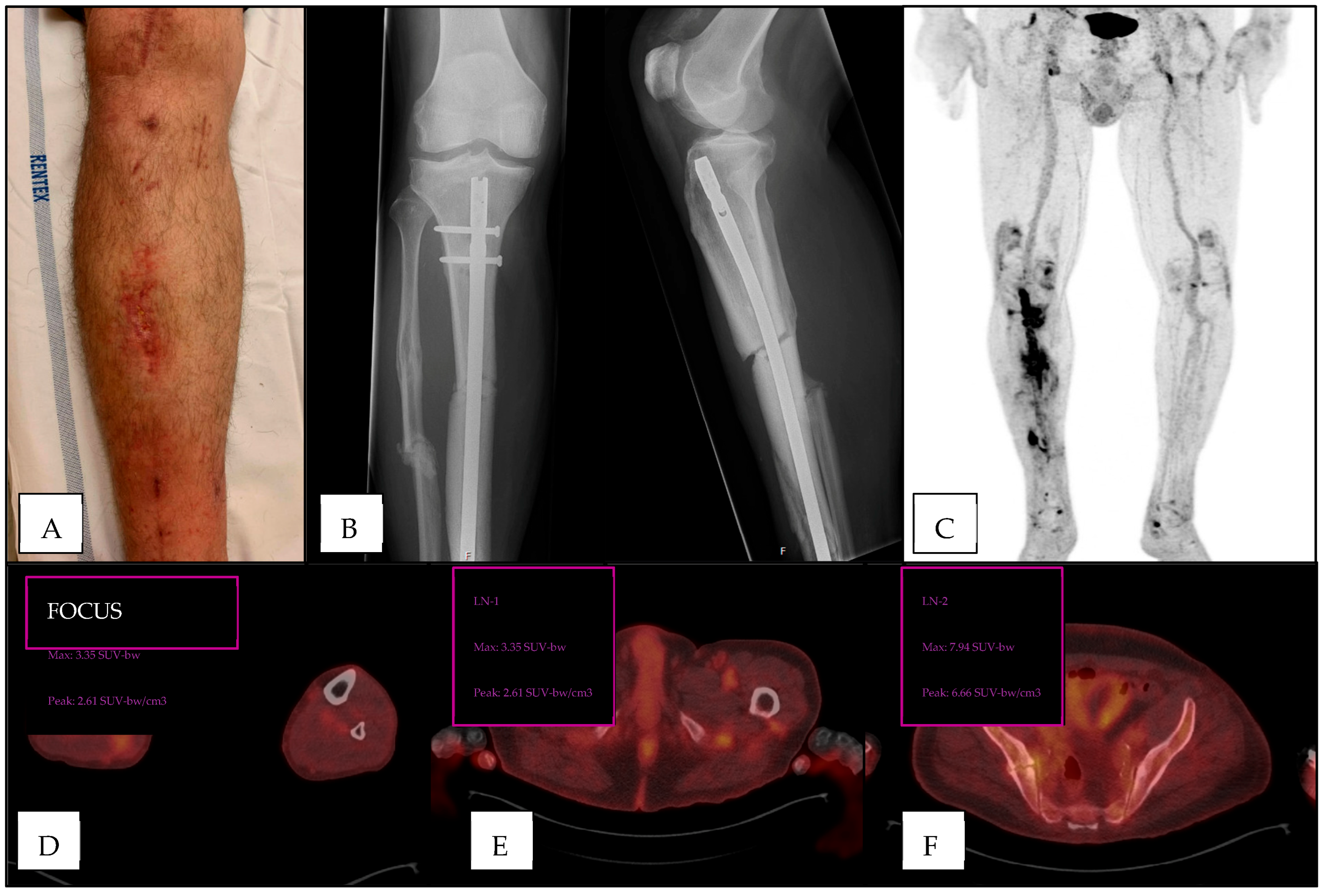
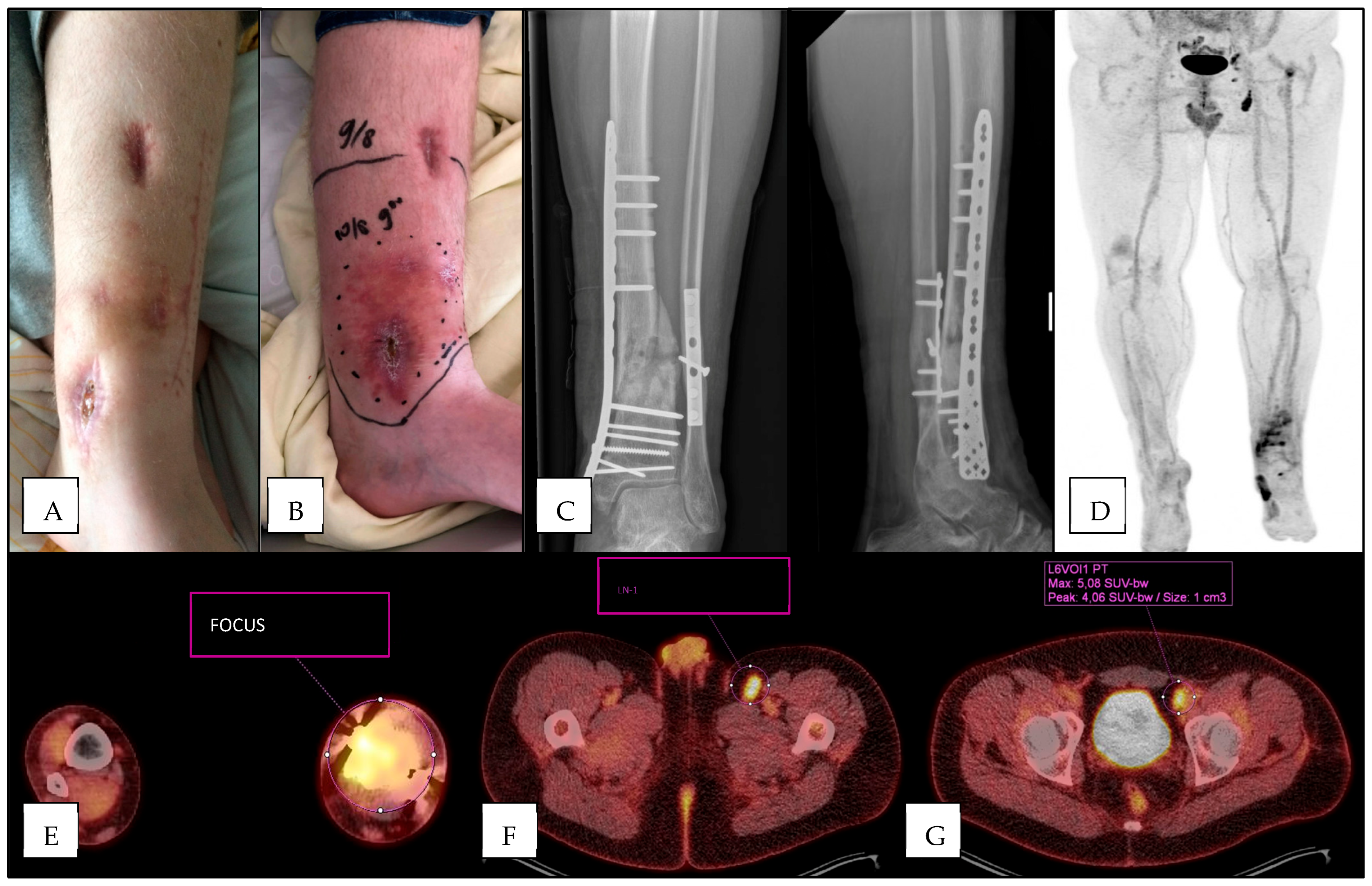
3. Results
3.1. Population Characteristics
3.2. FRI in Study Population
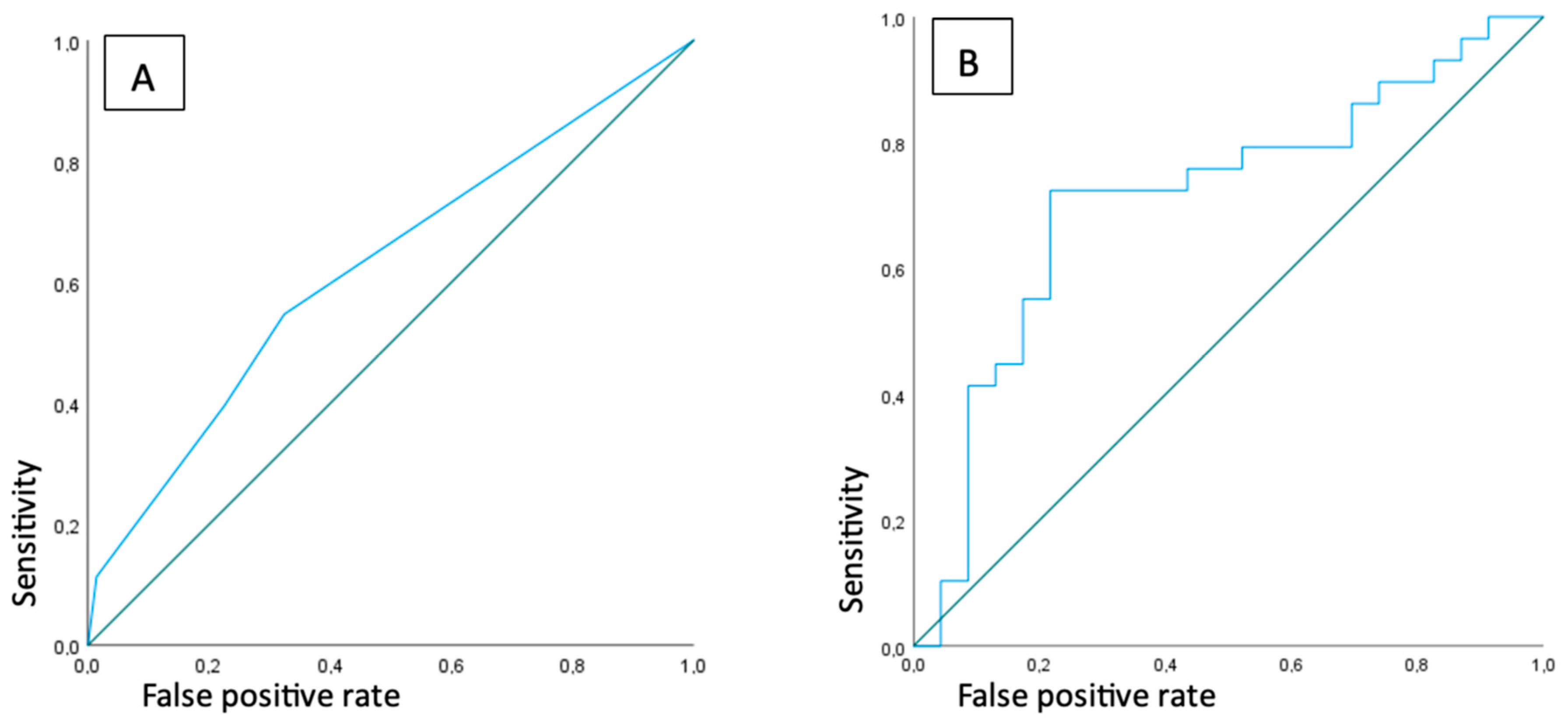
3.3. Diagnostic Accuracy of Standard Assessment Protocol
3.4. Diagnostic Accuracy of Presence and Number of FDG-Positive Lymph Nodes
3.5. Highest SUVmax
3.6. Added Value of Locoregional Lymph Node Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moriarty, T.F.; Metsemakers, W.J.; Morgenstern, M.; Hofstee, M.I.; Vallejo Diaz, A.; Cassat, J.E.; Wildemann, B.; Depypere, M.; Schwarz, E.M.; Richards, R.G. Fracture-related infection. Nat. Rev. Dis. Primers 2022, 8, 67. [Google Scholar] [CrossRef] [PubMed]
- Metsemakers, W.J.; Smeets, B.; Nijs, S.; Hoekstra, H. Infection after fracture fixation of the tibia: Analysis of healthcare utilization and related costs. Injury 2017, 48, 1204–1210. [Google Scholar] [CrossRef] [PubMed]
- Haidari, S.; Buijs, M.A.S.; Plate, J.D.J.; Zomer, J.J.; IJpma, F.F.A.; Hietbrink, F.; Govaert, G.A.M. Cost of fracture-related infection: The impact on direct hospital costs and healthcare utilization. Eur. J. Trauma. Emerg. Surg. 2024, 50, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Lu, V.; Zhang, J.; Patel, R.; Zhou, A.K.; Thahir, A.; Krkovic, M. Fracture Related Infections and Their Risk Factors for Treatment Failure—A Major Trauma Centre Perspective. Diagnostics 2022, 12, 1289. [Google Scholar] [CrossRef]
- Marais, L.C.; Zalavras, C.G.; Moriarty, F.T.; Kühl, R.; Metsemakers, W.J.; Morgenstern, M. The surgical management of fracture-related infection. Surgical strategy selection and the need for early surgical intervention. J. Orthop. 2024, 50, 36–41. [Google Scholar] [CrossRef]
- Vanvelk, N.; Van Lieshout, E.M.M.; Onsea, J.; Sliepen, J.; Govaert, G.; Ijpma, F.F.A.; Depypere, M.; Ferguson, J.; McNally, M.; Obremskey, W.T.; et al. Diagnosis of fracture-related infection in patients without clinical confirmatory criteria: An international retrospective cohort study. J. Bone Joint Infect. 2023, 8, 133–142. [Google Scholar] [CrossRef]
- Metsemakers, W.J.; Morgenstern, M.; McNally, M.A.; Moriarty, T.F.; McFadyen, I.; Scarborough, M.; Athanasou, N.; Ochsner, P.; Kuehl, R.; Raschke, M.; et al. Fracture-related infection: A consensus on definition from an international expert group. Injury 2018, 49, 505–510. [Google Scholar] [CrossRef]
- Lemans, J.V.; Hobbelink, M.G.; IJpma, F.F.; Plate, J.D.J.; van den Kieboom, J.; Bosch, P.; Leenen, L.P.H.; Kruyt, M.C.; Glaudemans, A.W.J.M.; Govaert, G.A.M. The diagnostic accuracy of 18F-FDG PET/CT in diagnosing fracture-related infections. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 999–1008. [Google Scholar] [CrossRef]
- Govaert, G.A.; IJpma, F.F.A.; McNally, M.; McNally, E.; Reininga, I.H.; Glaudemans, A.W. Accuracy of diagnostic imaging modalities for peripheral post-traumatic osteomyelitis—A systematic review of the recent literature. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1393–1407. [Google Scholar] [CrossRef]
- Govaert, G.A.; Bosch, P.; IJpma, F.F.; Glauche, J.; Jutte, P.C.; Lemans, J.V.; Wendt, K.; Reininga, I.; Glaudemans, A. High diagnostic accuracy of white blood cell scintigraphy for fracture related infections: Results of a large retrospective singlecenter study. Injury 2018, 49, 1085–1090. [Google Scholar] [CrossRef]
- Glaudemans, A.W.J.M.; Bosch, P.; Slart, R.H.J.A.; IJpma, F.F.A.; Govaert, G.A.M. Diagnosing fracture-related infections: Can we optimize our nuclear imaging techniques? Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1583–1587. [Google Scholar] [CrossRef] [PubMed]
- Pijl, J.P.; Nienhuis, P.H.; Kwee, T.C.; Glaudemans, A.W.J.M.; Slart, R.H.J.A.; Gormsen, L.C. Limitations and Pitfalls of FDG-PET/CT in Infection and Inflammation. Semin. Nucl. Med. 2021, 51, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Casali, M.; Lauri, C.; Altini, C.; Bertagna, F.; Cassarino, G.; Cistaro, A.; Erba, A.P.; Ferrari, C.; Mainolfi, C.G.; Palucci, A.; et al. State of the art of 18F-FDG PET/CT application in inflammation and infection: A guide for image acquisition and interpretation. Clin. Transl. Imaging 2021, 9, 299–339. [Google Scholar] [CrossRef] [PubMed]
- van Rijsewijk, N.D.; Helthuis, J.H.G.; Glaudemans, A.W.J.M.; Wouthuyzen-Bakker, M.; Prakken, N.H.J.; Liesker, D.J.; Saleem, B.R.; Slart, R.H.J.A. Added Value of Abnormal Lymph Nodes Detected with FDG-PET/CT in Suspected Vascular Graft Infection. Biology 2023, 12, 251. [Google Scholar] [CrossRef]
- ten Hove, D.; Sinha, B.; Glaudemans, A.W.J.M.; Gomes, A.; Swart, L.R.; Tanis, W.; Budde, R.P.J.; Slart, R.H.J.A. 18F-FDG-Uptake in Mediastinal Lymph Nodes in Suspected Prosthetic Valve Endocarditis: Predictor or Confounder? Front. Cardiovasc. Med. 2021, 8, 717774. [Google Scholar]
- Glaudemans, A.W.J.M.; Jutte, P.C.; Cataldo, M.A.; Cassar-Pullicino, V.; Gheysens, O.; Borens, O.; Trampuz, A.; Wörtler, K.; Petrosillo, N.; Winkler, H.; et al. Consensus document for the diagnosis of peripheral bone infection in adults: A joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 957–970. [Google Scholar] [CrossRef]
- Kaalep, A.; Sera, T.; Oyen, W.; Krause, B.J.; Chiti, A.; Liu, Y.; Boellaard, R. EANM/EARL FDG-PET/CT accreditation—Summary results from the first 200 accredited imaging systems. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 412–422. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, Z.; Liang, X.; Shem, C. Inguinal draining-lymph node in 18F-FDG PET/CT images could be a new indicator for the diagnosis of fracture-related infection in the lower extremities. Front. Immumology 2023, 14, 1206682. [Google Scholar] [CrossRef]
- Hulsen, D.J.W.; Mitea, C.; Arts, J.J.; Loeffen, D.; Geurts, J. Diagnostic value of hybrid FDG-PET/MR imaging of chronic osteomyelitis. Eur. J. Hybrid. Imaging 2022, 6, 15. [Google Scholar] [CrossRef]
- López-Álvarez, M.; Heuker, M.; Sjollema, K.A.; van Dam, G.M.; van Dijl, J.M.; IJpma, F.F.; van Oosten, M. Bacteria-targeted fluorescence imaging of extracted osteosynthesis devices for rapid visualization of fracture-related infections. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2276–2289. [Google Scholar] [CrossRef]
- Spoelstra, G.B.; Blok, S.N.; Reali Nazario, L.; Noord, L.; Fu, Y.; Simeth, N.A.; IJpma, F.F.A.; van Oosten, M.; van Dijl, J.M.; Feringa, B.L.; et al. Synthesis and preclinical evaluation of novel 18F-vancomycin-based tracers for the detection of bacterial infections using positron emission tomography. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 2583–2596. [Google Scholar] [CrossRef] [PubMed]
- Spoelstra, G.B.; Braams, L.M.; IJpma, F.F.A.; van Oosten, M.; Feringa, B.L.; Szymanski, W.; van Dijl, J.M. Bacteria-targeted imaging using vancomycin-based positron emission tomography tracers can distinguish infection from sterile inflammation. Eur. J. Nucl. Med. Mol. Imaging 2024. [Google Scholar] [CrossRef] [PubMed]
| Sex | |
| Male | 88 (71%) |
| Female | 36 (29%) |
| Age (mean + SD, years) | 49 (SD 8.6) |
| Fracture location | |
| Humerus | 4 (2.5%) |
| Ulna/radius | 8 (6.5%) |
| Femur | 36 (29%) |
| Tibia | 69 (56%) |
| Foot | 7 (6%) |
| Fracture type | |
| Open | 71 (57%) |
| Closed | 53 (43%) |
| Injury/scan interval (mean + SD, months) | 79 (SD 11.7) |
| Last surgery/scan interval (mean + SD, months) | 29 (SD 48.6) |
| Confirmed FRI | 53 (43%) |
| Medical microbiology results | 41 (77%) |
| Clinical follow up | 12 (23%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bosch, P.; Glaudemans, A.W.J.M.; de Vries, J.-P.P.M.; van Snick, J.H.; Lemans, J.V.C.; van den Kieboom, J.; Hobbelink, M.G.G.; Govaert, G.A.M.; IJpma, F.F.A. Diagnostic Value of Increased [18F]FDG Uptake in Locoregional Lymph Nodes on PET/CT in Patients with Suspected Fracture-Related Infection. Diagnostics 2025, 15, 616. https://doi.org/10.3390/diagnostics15050616
Bosch P, Glaudemans AWJM, de Vries J-PPM, van Snick JH, Lemans JVC, van den Kieboom J, Hobbelink MGG, Govaert GAM, IJpma FFA. Diagnostic Value of Increased [18F]FDG Uptake in Locoregional Lymph Nodes on PET/CT in Patients with Suspected Fracture-Related Infection. Diagnostics. 2025; 15(5):616. https://doi.org/10.3390/diagnostics15050616
Chicago/Turabian StyleBosch, Paul, Andor W. J. M. Glaudemans, Jean-Paul P. M. de Vries, Johannes H. van Snick, Justin V. C. Lemans, Janna van den Kieboom, Monique G. G. Hobbelink, Geertje A. M. Govaert, and Frank F. A. IJpma. 2025. "Diagnostic Value of Increased [18F]FDG Uptake in Locoregional Lymph Nodes on PET/CT in Patients with Suspected Fracture-Related Infection" Diagnostics 15, no. 5: 616. https://doi.org/10.3390/diagnostics15050616
APA StyleBosch, P., Glaudemans, A. W. J. M., de Vries, J.-P. P. M., van Snick, J. H., Lemans, J. V. C., van den Kieboom, J., Hobbelink, M. G. G., Govaert, G. A. M., & IJpma, F. F. A. (2025). Diagnostic Value of Increased [18F]FDG Uptake in Locoregional Lymph Nodes on PET/CT in Patients with Suspected Fracture-Related Infection. Diagnostics, 15(5), 616. https://doi.org/10.3390/diagnostics15050616







