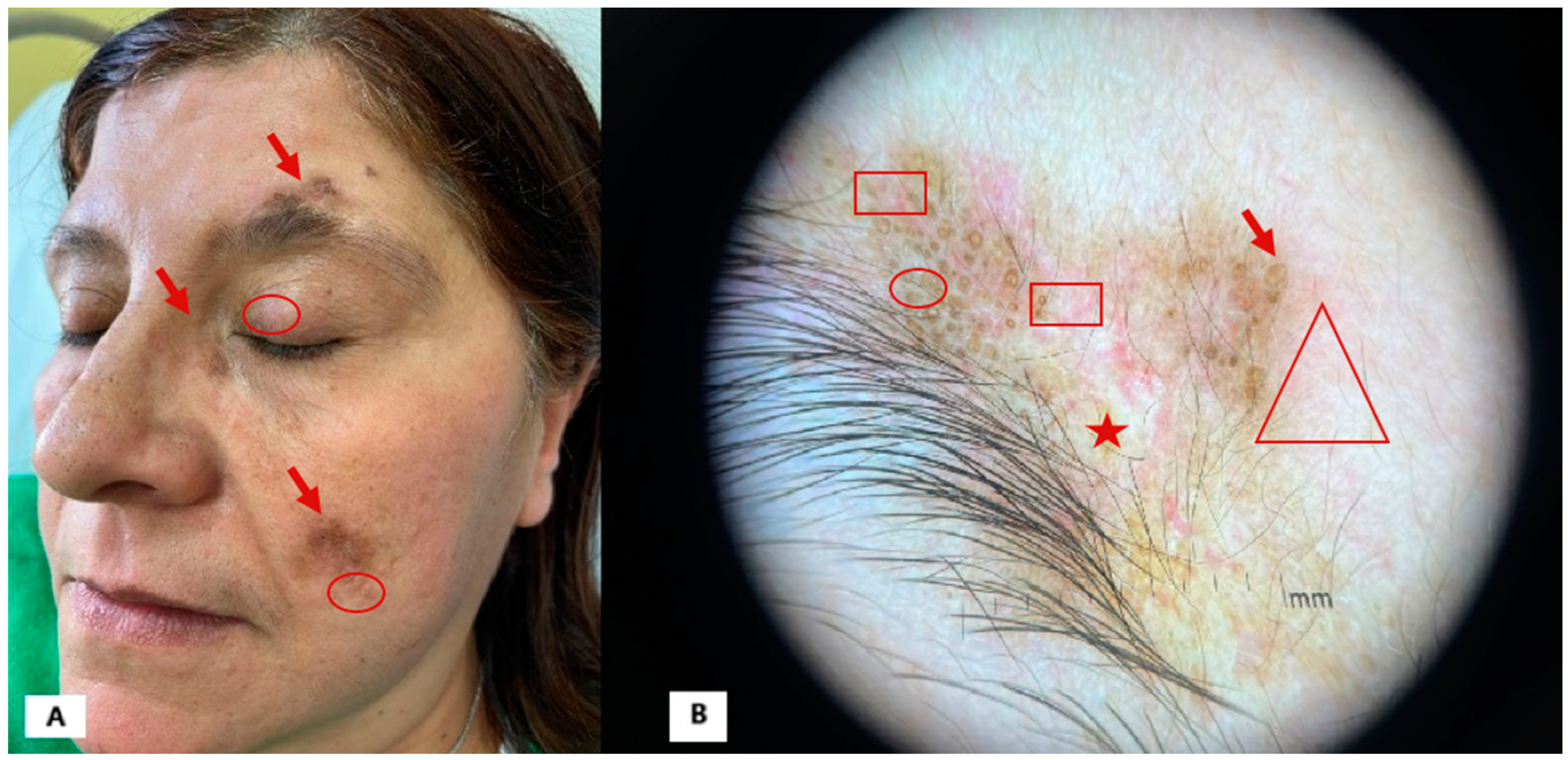
Can Dermoscopy Be a Useful Follow-Up Tool in Patients with Discoid Lupus Treated with Anifrolumab?
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Żychowska, M.; Żychowska, M. Dermoscopy of discoid lupus erythematosus—A systematic review of the literature. Int. J. Dermatol. 2021, 60, 818–828. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Tintos, B.O.; Garcia-Hidalgo, L.; Orozco-Topete, R. Dermoscopy in active discoid lupus. Arch. Dermatol. 2009, 145, 358. [Google Scholar] [CrossRef] [PubMed]
- Żychowska, M.; Reich, A. Dermoscopic Features of Acute, Subacute, Chronic and Intermittent Subtypes of Cutaneous Lupus Erythematosus in Caucasians. J. Clin. Med. 2022, 11, 4088. [Google Scholar] [CrossRef]
- Jha, A.; Sonthalia, S.; Sarkar, R. Dermoscopy of discoid lupus erythematosus. Indian Dermatol. Online J. 2016, 7, 458. [Google Scholar] [CrossRef] [PubMed]
- Lallas, A.; Apalla, Z.; Lefaki, I.; Sotiriou, E.; Lazaridou, E.; Ioannides, D.; Tiodorovic-Zivkovic, D.; Sidiropoulos, T.; Konstantinou, D.; Di Lernia, V.; et al. Dermoscopy of discoid lupus erythematosus. Br. J. Dermatol. 2013, 168, 284–288. [Google Scholar] [CrossRef]
- Martín-Torregrosa, D.; Mansilla-Polo, M.; Morgado-Carrasco, D. Use of Anifrolumab in Systemic Lupus Erythematosus, Cutaneous Lupus Erythematosus, and Other Autoimmune Dermatoses. Actas Dermosifiliogr. 2024, 116, 55–67. [Google Scholar] [CrossRef]
- Azuma, N.; Natsuaki, M.; Hashimoto, N.; Abe, T.; Ueda, S.; Ohno, Y.; Jinnin, M.; Matsui, K. Efficacy of anifrolumab in long-term intractable alopecia due to discoid lupus erythematosus. Mod. Rheumatol. Case Rep. 2024, 8, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Centner, C.S.; Robertson, N.M.; Kang, J.; Sander, I.B.; Timlin, H. Treatment of discoid lupus with lenalidomide and anifrolumab: Case report and review of the literature. Lupus 2024, 33, 1487–1491. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.S.; Rajeh, A.; Le, T.; Kahn, P.J.; Oza, V.S.; Arkin, L.M.; Vleugels, R.A. Anifrolumab for Adolescent Discoid Lupus Erythematosus. JAMA Netw. Open 2023, 6, E2338200. [Google Scholar] [CrossRef] [PubMed]
- Bao, A.; Petri, M.A.; Fava, A.; Kang, J. Case series of anifrolumab for treatment of cutaneous lupus erythematosus and lupus-related mucocutaneous manifestations in patients with SLE. Lupus Sci. Med. 2023, 10, e001007. [Google Scholar] [CrossRef] [PubMed]
- Rönnblom, L.; Alm, G.V.; Eloranta, M.L. The type I interferon system in the development of lupus. Semin. Immunol. 2011, 23, 113–121. [Google Scholar] [CrossRef]
- Braunstein, I.; Klein, R.; Okawa, J.; Werth, V.P. The interferon-regulated gene signature is elevated in subacute cutaneous lupus erythematosus and discoid lupus erythematosus and correlates with the cutaneous lupus area and severity index score. Br. J. Dermatol. 2012, 166, 971–975. [Google Scholar] [CrossRef]
- Ohyama, M. Primary cicatricial alopecia: Recent advances in understanding and management. J. Dermatol. 2012, 39, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Trentin, F.; Tani, C.; Elefante, E.; Stagnaro, C.; Zucchi, D.; Mosca, M. Treatment with Anifrolumab for Discoid Lupus Erythematosus. JAMA Dermatol. 2023, 159, 224–226. [Google Scholar] [CrossRef]
- Han, S.; Ferrer, J.; Bittar, M.; Jones, A. Alopecia secondary to severe discoid lupus responding to anifrolumab. Int. J. Women’s Dermatol. 2023, 9, E098. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ambrogio, F.; Foti, C.; Noviello, S.; Cazzato, G.; Meduri, A.R.; Marasco, C.; Vacca, A.; Tirone, B. Can Dermoscopy Be a Useful Follow-Up Tool in Patients with Discoid Lupus Treated with Anifrolumab? Diagnostics 2025, 15, 522. https://doi.org/10.3390/diagnostics15050522
Ambrogio F, Foti C, Noviello S, Cazzato G, Meduri AR, Marasco C, Vacca A, Tirone B. Can Dermoscopy Be a Useful Follow-Up Tool in Patients with Discoid Lupus Treated with Anifrolumab? Diagnostics. 2025; 15(5):522. https://doi.org/10.3390/diagnostics15050522
Chicago/Turabian StyleAmbrogio, Francesca, Caterina Foti, Silvia Noviello, Gerardo Cazzato, Alexandre Raphael Meduri, Carolina Marasco, Angelo Vacca, and Benedetta Tirone. 2025. "Can Dermoscopy Be a Useful Follow-Up Tool in Patients with Discoid Lupus Treated with Anifrolumab?" Diagnostics 15, no. 5: 522. https://doi.org/10.3390/diagnostics15050522
APA StyleAmbrogio, F., Foti, C., Noviello, S., Cazzato, G., Meduri, A. R., Marasco, C., Vacca, A., & Tirone, B. (2025). Can Dermoscopy Be a Useful Follow-Up Tool in Patients with Discoid Lupus Treated with Anifrolumab? Diagnostics, 15(5), 522. https://doi.org/10.3390/diagnostics15050522







