A 6-Year Retrospective Study in Surgery Patients with Thyroid Diseases in Mureș County, Romania, Before and During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Database and Study Design
2.2. Pathological Data and Study Groups
2.3. Statistical Analysis
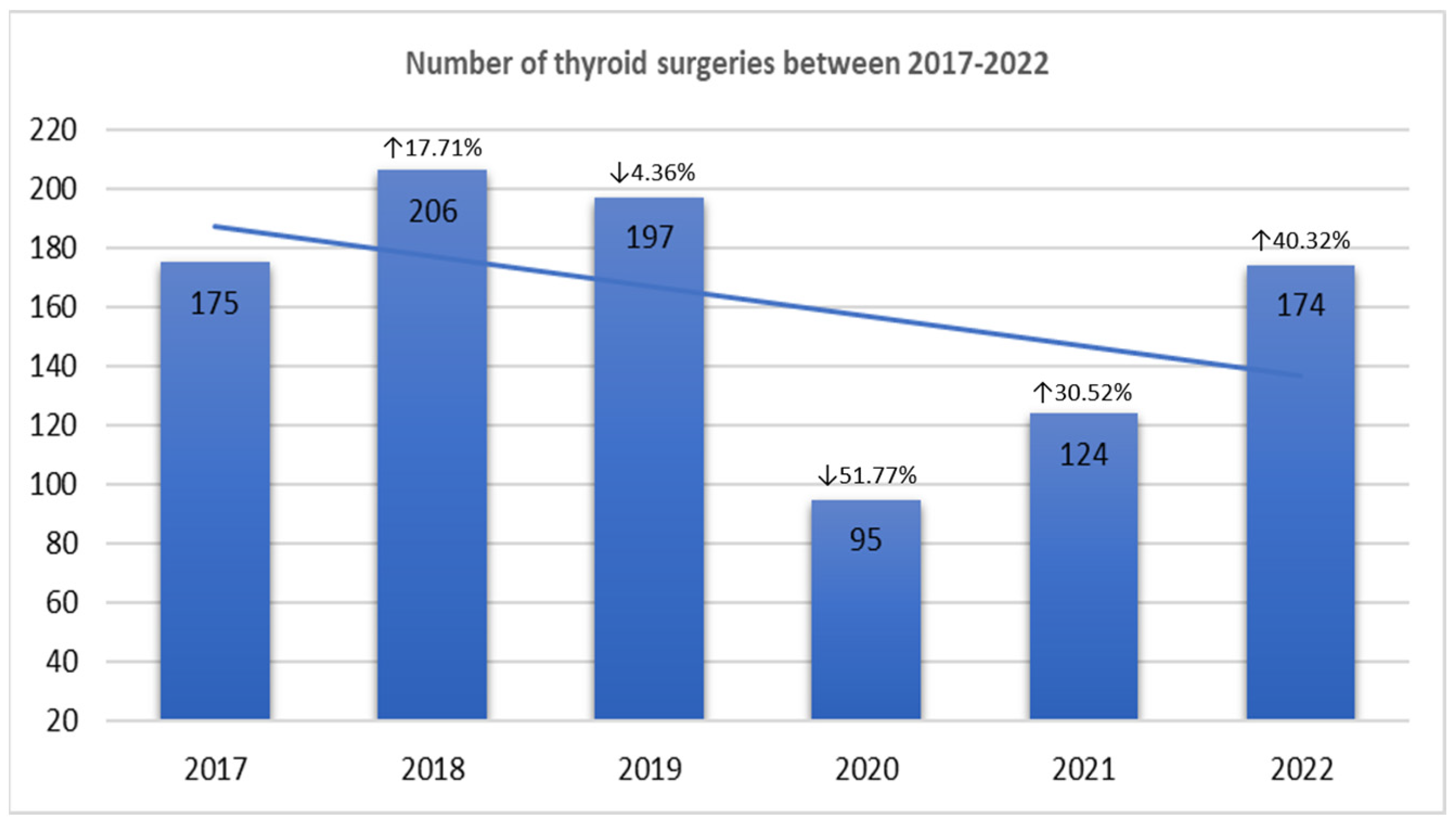
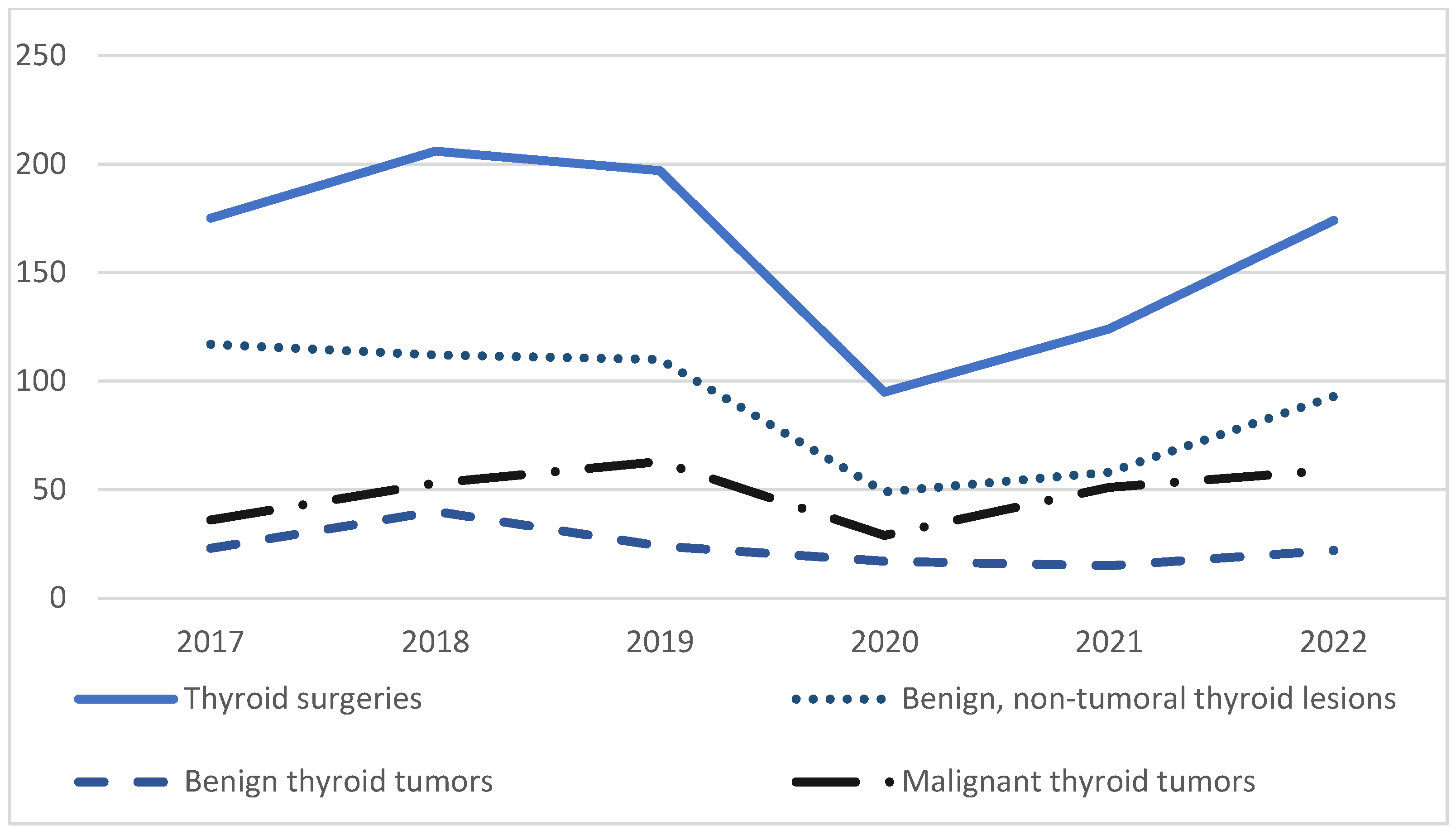
3. Results
3.1. Patient Characteristics
3.1.1. Benign Non-Tumoral Pathology Group
3.1.2. Benign Thyroid Tumors Group
3.1.3. Malignant Thyroid Tumors Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Huang, X.; Wei, F.; Hu, L.; Wen, L.; Chen, K. Epidemiology and Clinical Characteristics of COVID-19. Arch. Iran. Med. 2020, 23, 268–271. [Google Scholar] [CrossRef] [PubMed]
- Dhama, K.; Khan, S.; Tiwari, R.; Sircar, S.; Bhat, S.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Coronavirus Disease 2019-COVID-19. Clin. Microbiol. Rev. 2020, 33, e00028-20. [Google Scholar] [CrossRef] [PubMed]
- WHO. Coronavirus Disease (COVID-19) Pandemic; World Health Organization (WHO): Geneva, Switzerland, 2024; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 15 March 2024).
- Gorchane, A.; Ach, T.; Sahli, J.; Abdelkrim, A.B.; Mallouli, M.; Bellazreg, F.; Hachfi, W.; Chaieb, M.C.; Ach, K. Uncovering the alarming rise of diabetic ketoacidosis during COVID-19 pandemic: A pioneer African study and review of literature. Front. Endocrinol. 2023, 14, 1234256. [Google Scholar] [CrossRef] [PubMed]
- Darvishi, M.; Nazer, M.R.; Shahali, H.; Nouri, M. Association of Thyroid Dysfunction and COVID-19: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2022, 13, 947594. [Google Scholar] [CrossRef]
- Lui, D.T.W.; Tsoi, K.H.; Lee, C.H.; Cheung, C.Y.Y.; Fong, C.H.Y.; Lee, A.C.H.; Tam, A.R.; Pang, P.; Ho, T.Y.; Law, C.Y.; et al. A Prospective Follow-up on Thyroid Function, Thyroid Autoimmunity and Long COVID among 250 COVID-19 Survivors. Endocrine 2023, 80, 380–391. [Google Scholar] [CrossRef]
- Khoo, B.; Tan, T.; Clarke, S.A.; Mills, E.G.; Patel, B.; Modi, M.; Phylactou, M.; Eng, P.C.; Thurston, L.; Alexander, E.C.; et al. Thyroid Function Before, During, and after COVID-19. J. Clin. Endocrinol. Metab. 2021, 106, e803–e811. [Google Scholar] [CrossRef]
- Duntas, L.H.; Jonklaas, J. COVID-19 and Thyroid Diseases: A Bidirectional Impact. J. Endocr. Soc. 2021, 5, bvab076. [Google Scholar] [CrossRef]
- Scappaticcio, L.; Pitoia, F.; Esposito, K.; Piccardo, A.; Trimboli, P. Impact of COVID-19 on the Thyroid Gland: An Update. Rev. Endocr. Metab. Disord. 2021, 22, 803–815. [Google Scholar] [CrossRef]
- Naguib, R. Potential Relationships between COVID-19 and the Thyroid Gland: An Update. J. Int. Med. Res. 2022, 50, 03000605221082898. [Google Scholar] [CrossRef]
- Murugan, A.K.; Alzahrani, A.S. SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases. J. Inflamm. Res. 2021, 14, 6191–6221. [Google Scholar] [CrossRef] [PubMed]
- Kitahara, C.M.; Schneider, A.B. Epidemiology of Thyroid Cancer. Cancer Epidemiol. Biomark. Prev. 2022, 31, 1284–1297. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhao, X.; Sun, J.; Cheng, C.; Yin, C.; Bai, R. The Epidemic of Thyroid Cancer in China: Current Trends and Future Prediction. Front. Oncol. 2022, 12, 932729. [Google Scholar] [CrossRef] [PubMed]
- Ashorobi, D.; Lopez, P.P. Cancer, Follicular Thyroid; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Berger, N.; Borda, A. Pathologie Thyroidienne, Parathyroidienne et Surrenalienne; Sauramps Medical: Montpellier, France, 2010. [Google Scholar]
- Rosai, J.; Osamura, R.Y.; Klöppel, G.; Lloyd, R.V. WHO Classification of Tumours of Endocrine Organs; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Umakanthan, S.; Sahu, P.; Ranade, A.V.; Bukelo, M.M.; Rao, J.S.; Abrahao-Machado, L.F.; Dahal, S.; Kumar, H.; Kv, D. Origin, Transmission, Diagnosis and Management of Coronavirus Disease 2019 (COVID-19). Postgrad. Med. J. 2020, 96, 753–758. [Google Scholar]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Koo, J.R.; Cook, A.R.; Park, M.; Sun, Y.; Sun, H.; Lim, J.T.; Tam, C.; Dickens, B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020, 20, 678–688. [Google Scholar] [CrossRef]
- Pujolar, G.; Oliver-Anglès, A.; Vargas, I.; Vázquez, M.L. Changes in Access to Health Services during the COVID-19 Pandemic: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 1749. [Google Scholar] [CrossRef]
- Zhang, Y.N.; Chen, Y.; Wang, Y.; Li, F.; Pender, M.; Wang, N.; Yan, F.; Ying, X.H.; Tang, S.L.; Fu, C.W. Reduction in Healthcare Services during the COVID-19 Pandemic in China. BMJ Glob. Health 2020, 5, e003421. [Google Scholar] [CrossRef]
- Tsioufis, K.; Chrysohoou, C.; Kariori, M.; Leontsinis, I.; Dalakouras, I.; Papanikolaou, A.; Charalambus, G.; Sambatakou, H.; Siasos, G.; Panagiotakos, D.; et al. The Mystery of “Missing” Visits in an Emergency Cardiology Department, in the Era of COVID-19.; a Time-Series Analysis in a Tertiary Greek General Hospital. Clin. Res. Cardiol. 2020, 109, 1483–1489. [Google Scholar] [CrossRef]
- Diaz, A.; Sarac, B.A.; Schoenbrunner, A.R.; Janis, J.E.; Pawlik, T.M. Elective Surgery in the Time of COVID-19. Am. J. Surg. 2020, 219, 900. [Google Scholar] [CrossRef]
- Halley, M.C.; Stanley, T.; Maturi, J.; Goldenberg, A.J.; Bernstein, J.A.; Wheeler, M.T.; Tabor, H.K. “It Seems like COVID-19 Now Is the Only Disease Present on Earth”: Living with a Rare or Undiagnosed Disease during the COVID-19 Pandemic. Genet. Med. 2021, 23, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Karavadra, B.; Stockl, A.; Prosser-Snelling, E.; Simpson, P.; Morris, E. Women’s Perceptions of COVID-19 and Their Healthcare Experiences: A Qualitative Thematic Analysis of a National Survey of Pregnant Women in the United Kingdom. BMC Pregnancy Childbirth 2020, 20, 600. [Google Scholar] [CrossRef] [PubMed]
- Hailemariam, S.; Agegnehu, W.; Derese, M. Exploring COVID-19 Related Factors Influencing Antenatal Care Services Uptake: A Qualitative Study among Women in a Rural Community in Southwest Ethiopia. J. Prim. Care Community Health 2021, 12, 2150132721996892. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.W.; Billany, J.C.T.; Adam, R.; Martin, L.; Tobin, R.; Bagdai, S.; Galvin, N.; Farr, I.; Allain, A.; Davies, L.; et al. Rapid Implementation of Virtual Clinics Due to COVID-19: Report and Early Evaluation of a Quality Improvement Initiative. BMJ Open Qual. 2020, 9, e000985. [Google Scholar] [CrossRef]
- Smulever, A.; Abelleira, E.; Bueno, F.; Pitoia, F. Thyroid Cancer in the Era of COVID-19. Endocrine 2020, 70, 1–5. [Google Scholar] [CrossRef]
- Popa, O.; Barna, R.A.; Borlea, A.; Cornianu, M.; Dema, A.; Stoian, D. The Impact of the COVID-19 Pandemic on Thyroid Nodular Disease: A Retrospective Study in a Single Center in the Western Part of Romania. Front. Endocrinol. 2023, 14, 1221795. [Google Scholar] [CrossRef]
- Feier, C.V.I.; Muntean, C.; Faur, A.M.; Blidari, A.; Contes, O.E.; Streinu, D.R.; Olariu, S. The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania. Cancers 2023, 15, 3032. [Google Scholar] [CrossRef]
- Kim, S.H.; Min, E.; Hwang, Y.M.; Choi, Y.S.; Yi, J.W. Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea. Cancers 2022, 14, 4338. [Google Scholar] [CrossRef]
- Chen, W.; Tian, Y.; Li, Z.; Zhu, J.; Wei, T.; Lei, J. Potential Interaction between SARS-CoV-2 and Thyroid: A Review. Endocrinology 2021, 162, bqab004. [Google Scholar] [CrossRef]
- Jafarzadeh, A.; Nemati, M.; Jafarzadeh, S.; Nozari, P.; Mortazavi, S.M.J. Thyroid Dysfunction Following Vaccination with COVID-19 Vaccines: A Basic Review of the Preliminary Evidence. J. Endocrinol. Investig. 2022, 45, 1835–1863. [Google Scholar] [CrossRef]
- Allam, M.M.; El-Zawawy, H.T.; Ahmed, S.M.; Aly Abdelhamid, M. Thyroid Disease and COVID-19 Infection: Case Series. Clin. Case Rep. 2021, 9, e04225. [Google Scholar] [CrossRef] [PubMed]
- LeClair, K.; Bell, K.J.L.; Furuya-Kanamori, L.; Doi, S.A.; Francis, D.O.; Davies, L. Evaluation of Gender Inequity in Thyroid Cancer Diagnosis. JAMA Intern. Med. 2021, 181, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Moleti, M.; Sturniolo, G.; Di Mauro, M.; Russo, M.; Vermiglio, F. Female Reproductive Factors and Differentiated Thyroid Cancer. Front. Endocrinol. 2017, 8, 111. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Ros, R.; Rinaldi, S.; Biessy, C.; Tjønneland, A.; Halkjær, J.; Fournier, A.; Boutron-Ruault, M.C.; Mesrine, S.; Tikk, K.; Fortner, R.T.; et al. Reproductive and Menstrual Factors and Risk of Differentiated Thyroid Carcinoma: The EPIC Study. Int. J. Cancer 2015, 136, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, R.; Zhang, L.; Kebebew, E. Thyroid Cancer Gender Disparity. Future Oncol. 2010, 6, 1771–1779. [Google Scholar] [CrossRef]
- Peterson, E.; De, P.; Nuttall, R. BMI, Diet and Female Reproductive Factors as Risks for Thyroid Cancer: A Systematic Review. PLoS ONE 2012, 7, e29177. [Google Scholar] [CrossRef]
- Haymart, M.R. Understanding the Relationship Between Age and Thyroid Cancer. Oncologist 2009, 14, 216–221. [Google Scholar] [CrossRef]
| 2017–2019 n (%) | 2020–2022 n (%) | p * | |
|---|---|---|---|
| Benign, non-tumoral thyroid lesions | 339 (56.8) | 200 (50.8) | 0.017 |
| Nodular goiter | 268 (79) | 169 (84.5) | 0.139 |
| Diffuse goiter | 13 (3.8) | 2 (1) | 0.060 |
| Basedow–Graves disease | 24 (7.1) | 11 (5.5) | 0.588 |
| Autoimmune thyroiditis | 27 (7.9) | 15 (7.5) | 0.990 |
| Cysts | 5 (1.5) | 2 (1) | 0.990 |
| Subacute thyroiditis | 1 (0.3) | 0 | - |
| Thyroid tuberculosis | 1 (0.3) | 0 | - |
| Thyroid abscess | 0 | 1 (0.5) | - |
| Benign thyroid tumors | 87 (15.1) | 54 (13.7) | 0.579 |
| Follicular adenoma | 46 (52.9) | 22 (40.7) | 0.170 |
| Hürthle cell adenoma | 13 (14.9) | 7 (12.9) | 0.808 |
| Hyalinizing trabecular tumor | 0 | 1 | - |
| Other encapsulated follicular-patterned thyroid tumors (non-invasive) | 28 (32.2) | 24 (44.4) | 0.154 |
| TT-UMP | 9 (32.2) | 10 (41.6) | 0.151 |
| NIFTP | 19 (67.8) | 14 (58.4) | 0.782 |
| Malignant thyroid tumors | 152 (26.3) | 139 (49.5) | 0.002 |
| Papillary thyroid carcinoma | 118 (77.6) | 124 (89.2) | 0.011 |
| Conventional variant | 61 (51.7) | 51 (41.1) | 0.121 |
| Follicular variant | 18 (15.2) | 28 (22.6) | 0.189 |
| Papillary microcarcinoma | 23 (19.5) | 26 (20.9) | 0.873 |
| Encapsulated variant | 0 | 1 (0.8) | - |
| Oncocytic variant | 0 | 2 (1.6) | - |
| Warthin-like variant | 3 (2.5) | 6 (4.8) | 0.500 |
| Tall cell variant | 7 (5.9) | 6 (4.8) | 0.780 |
| Hobnail variant | 3 (2.5) | 2 (1.6) | 0.677 |
| Solid-trabecular variant | 3 (2.5) | 0 | - |
| Diffuse sclerosing variant | 0 | 2 (1.6) | - |
| Follicular thyroid carcinoma | 1 (0.80) | 0 | - |
| Hürthle cell carcinoma | 0 | 2 (1.4) | - |
| Poorly differentiated thyroid carcinoma | 8 (5.2) | 5 (3.6) | 0.577 |
| Anaplastic thyroid carcinoma | 2 (1.3) | 0 | - |
| Medullary thyroid carcinoma | 15 (9.9) | 4 (2.9) | 0.017 |
| Metastasis | 3 (1.9) | 1 (0.7) | 0.623 |
| Other type ** | 5 (3.3) | 3 (2.2) | 0.725 |
| Pathology Group | 2017–2019 | 2020–2022 | p | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Age (Years) | W/M Ratio | Average Age for Men (Years) | Average Age for Women (Years) | Average Age (Years) | W/M Ratio | Average Age for Men (Years) | Average Age for Women (Years) | Average Age | Average Age for Men (Years) | Average Age for Women (Years) | |
| Benign non-tumoral thyroid pathology | 53.59 | 9.2/1 | 54.43 | 53.48 | 53.67 | 7.3/1 | 60.83 | 52.69 | 0.552 | 0.002 | 0.556 |
| Benign thyroid tumors | 49.73 | 7.7/1 | 50.90 | 49.58 | 51.90 | 6.8/1 | 51.68 | 53.42 | 0.363 | 0.694 | 0.419 |
| Malignant thyroid tumors | 50.96 | 4.6/1 | 54.64 | 50.10 | 49.57 | 5.3/1 | 48.47 | 48.71 | 0.356 | 0.186 | 0.542 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cătană, R.T.; Nechifor-Boila, A.; Zăhan, A.; Militaru, A.D.; Radu, G.-N.; Borda, A. A 6-Year Retrospective Study in Surgery Patients with Thyroid Diseases in Mureș County, Romania, Before and During the COVID-19 Pandemic. Diagnostics 2025, 15, 287. https://doi.org/10.3390/diagnostics15030287
Cătană RT, Nechifor-Boila A, Zăhan A, Militaru AD, Radu G-N, Borda A. A 6-Year Retrospective Study in Surgery Patients with Thyroid Diseases in Mureș County, Romania, Before and During the COVID-19 Pandemic. Diagnostics. 2025; 15(3):287. https://doi.org/10.3390/diagnostics15030287
Chicago/Turabian StyleCătană, Ramona Teodora, Adela Nechifor-Boila, Ancuța Zăhan, Andreea Deborah Militaru, Georgian-Nicolae Radu, and Angela Borda. 2025. "A 6-Year Retrospective Study in Surgery Patients with Thyroid Diseases in Mureș County, Romania, Before and During the COVID-19 Pandemic" Diagnostics 15, no. 3: 287. https://doi.org/10.3390/diagnostics15030287
APA StyleCătană, R. T., Nechifor-Boila, A., Zăhan, A., Militaru, A. D., Radu, G.-N., & Borda, A. (2025). A 6-Year Retrospective Study in Surgery Patients with Thyroid Diseases in Mureș County, Romania, Before and During the COVID-19 Pandemic. Diagnostics, 15(3), 287. https://doi.org/10.3390/diagnostics15030287






