Recurrence, Readmission, and Key Mortality Predictors in Patients with Carbapenem-Resistant Enterobacterales Infections
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Settings, and Participants
2.2. Definitions
2.3. Study Outcomes
2.4. Patient Data Collection
2.5. Microbiological Data
2.6. Statistical Analysis
2.7. Ethical Considerations
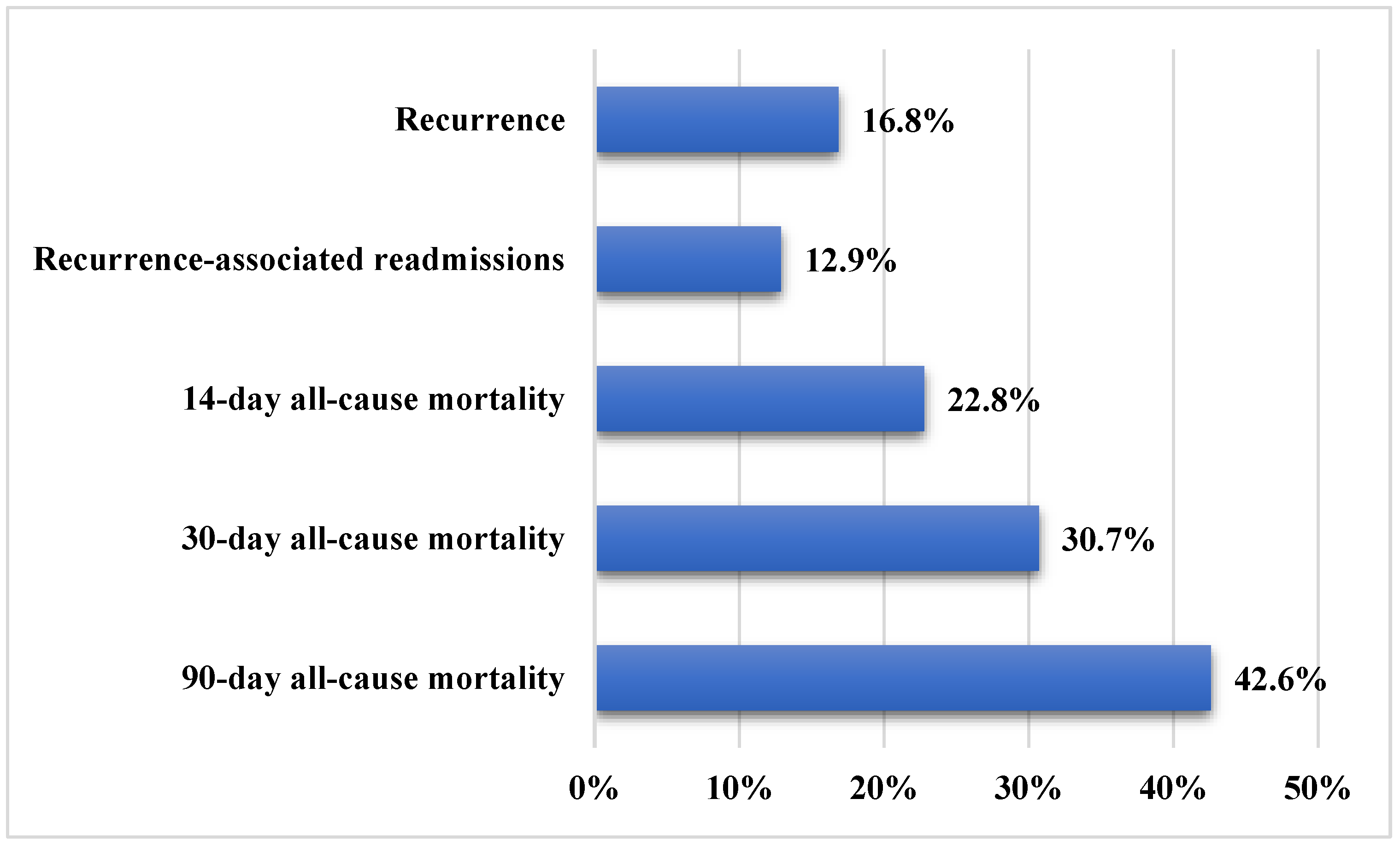
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Publishes List of Bacteria for Which New Antibiotics are Urgently Needed; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Logan, L.K.; Weinstein, R.A. The Epidemiology of Carbapenem-Resistant Enterobacteriaceae: The Impact and Evolution of a Global Menace. J. Infect. Dis. 2017, 215, S28–S36. [Google Scholar] [CrossRef]
- Villegas, M.V.; Pallares, C.J.; Escandón-Vargas, K.; Hernández-Gómez, C.; Correa, A.; Álvarez, C.; Rosso, F.; Matta, L.; Luna, C.; Zurita, J.; et al. Characterization and Clinical Impact of Bloodstream Infection Caused by Carbapenemase-Producing Enterobacteriaceae in Seven Latin American Countries. PLoS ONE 2016, 11, e0154092. [Google Scholar] [CrossRef]
- Garbati, M.A.; Sakkijha, H.; Abushaheen, A. Infections due to Carbapenem Resistant Enterobacteriaceae among Saudi Arabian Hospitalized Patients: A Matched Case-Control Study. BioMed Res. Int. 2016, 2016, 3961684. [Google Scholar] [CrossRef] [PubMed]
- Son, H.J.; Cho, E.B.; Bae, M.; Lee, S.C.; Sung, H.; Kim, M.N.; Jung, J.; Kim, M.J.; Kim, S.H.; Lee, S.O.; et al. Clinical and Microbiological Analysis of Risk Factors for Mortality in Patients With Carbapenem-Resistant Acinetobacter baumannii Bacteremia. Open Forum. Infect. Dis. 2020, 7, ofaa378. [Google Scholar] [CrossRef] [PubMed]
- Tischendorf, J.; de Avila, R.A.; Safdar, N. Risk of infection following colonization with carbapenem-resistant Enterobactericeae: A systematic review. Am. J. Infect. Control 2016, 44, 539–543. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Jean, S.S.; Lee, Y.L.; Lu, M.C.; Ko, W.C.; Liu, P.Y.; Hsueh, P.R. Carbapenem-Resistant Enterobacterales in Long-Term Care Facilities: A Global and Narrative Review. Front. Cell. Infect. Microbiol. 2021, 11, 601968. [Google Scholar] [CrossRef]
- Abou-assy, R.S.; Aly, M.M.; Amashah, R.H.; Jastaniah, S.D.; Al Deen, H.M. Epidemiology of carbapenem resistance Enterobacterales in Saudi Arabia: A systematic review. J. Contemp. Med. Sci. 2022, 8, 18–26. [Google Scholar] [CrossRef]
- Alshehri, A.A.; Aldali, J.A.; Abdelhamid, M.A.; Alanazi, A.A.; Alhuraiz, R.B.; Alanazi, L.Z.; Alshmrani, M.A.; Alqahtani, A.M.; Alrshoud, M.I.; Alharbi, R.F. Implementation of Antimicrobial Stewardship Programs in Saudi Arabia: A Systematic Review. Microorganisms 2025, 13, 440. [Google Scholar] [CrossRef]
- Chen, J.; Ma, H.; Huang, X.; Cui, Y.; Peng, W.; Zhu, F.; Ma, S.; Rao, M.; Zhang, P.; Yang, H.; et al. Risk factors and mortality of carbapenem-resistant Klebsiella pneumoniae bloodstream infection in a tertiary-care hospital in China: An eight-year retrospective study. Antimicrob. Resist. Infect. Control 2022, 11, 161. [Google Scholar] [CrossRef]
- Seo, H.; Lee, S.C.; Chung, H.; Ra, S.H.; Sung, H.; Kim, M.N.; Jung, J.; Kim, M.J.; Kim, S.H.; Lee, S.O.; et al. Clinical and Microbiological Analysis of Risk Factors for Mortality in Patients with Carbapenem-Resistant Enterobacteriaceae Bacteremia. Int. J. Antimicrob. Agents 2020, 56, 106126. [Google Scholar] [CrossRef]
- Li, C.; Li, Y.; Zhao, Z.; Liu, Q.; Li, B. Treatment options and clinical outcomes for carbapenem-resistant Enterobacteriaceae bloodstream infection in a Chinese university hospital. J. Infect. Public Health 2019, 12, 26–31. [Google Scholar] [CrossRef]
- Van Duin, D.; Arias, C.A.; Komarow, L.; Chen, L.; Hanson, B.M.; Weston, G.; Cober, E.; Garner, O.B.; Jacob, J.T.; Satlin, M.J.; et al. Molecular and clinical epidemiology of carbapenem-resistant Enterobacterales in the USA (CRACKLE-2): A prospective cohort study. Lancet Infect. Dis. 2020, 20, 731–741. [Google Scholar] [CrossRef]
- Zheng, G.; Cai, J.; Deng, H.; Yang, H.; Xiong, W.; Chen, E.; Bai, H.; He, J. Development of a risk prediction model for subsequent infection after colonization with carbapenem-resistant Enterobacterales: A retrospective cohort study. Antimicrob. Resist. Infect. Control 2024, 13, 46. [Google Scholar] [CrossRef]
- Howard-Anderson, J.R.; Earley, M.; Komarow, L.; Abbo, L.; Anderson, D.J.; Gallagher, J.C.; Grant, M.; Kim, A.; Bonomo, R.A.; van Duin, D.; et al. Poor outcomes in both infection and colonization with carbapenem-resistant Enterobacterales. Infect. Control Hosp. Epidemiol. 2022, 43, 1840–1846. [Google Scholar] [CrossRef]
- Zilberberg, M.D.; Nathanson, B.H.; Sulham, K.; Fan, W.; Shorr, A.F. Carbapenem resistance, inappropriate empiric treatment and outcomes among patients hospitalized with Enterobacteriaceae urinary tract infection, pneumonia and sepsis. BMC Infect. Dis. 2017, 17, 279. [Google Scholar] [CrossRef]
- Huang, V.; Ruhe, J.J.; Lerner, P.; Fedorenko, M. Risk factors for readmission in patients discharged with outpatient parenteral antimicrobial therapy: A retrospective cohort study. BMC Pharmacol. Toxicol. 2018, 19, 50. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Wu, M.; Yu, H.; Jia, X.; Zou, H.; Ma, D.; Niu, S.; Huang, S. Clinical and Microbiological Characterization of Carbapenem-Resistant Enterobacteriales: A Prospective Cohort Study. Front. Pharmacol. 2021, 12, 2021. [Google Scholar] [CrossRef] [PubMed]
- Ciobotaro, P.; Flaks-Manov, N.; Oved, M.; Schattner, A.; Hoshen, M.; Ben-Yosef, E.; Balicer, R.D.; Zimhony, O. Predictors of Persistent Carbapenem-Resistant Enterobacteriaceae Carriage upon Readmission and Score Development. Infect. Control Hosp. Epidemiol. 2016, 37, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, F.S.; Assous, M.V.; Bdolah-Abram, T.; Lachish, T.; Yinnon, A.M.; Wiener-Well, Y. Duration of carriage of carbapenem-resistant Enterobacteriaceae following hospital discharge. Am. J. Infect. Control 2013, 41, 190–194. [Google Scholar] [CrossRef]
- Alraddadi, B.M.; Heaphy, E.L.G.; Aljishi, Y.; Ahmed, W.; Eljaaly, K.; Al-Turkistani, H.H.; Alshukairi, A.N.; Qutub, M.O.; Alodini, K.; Alosaimi, R.; et al. Molecular epidemiology and outcome of carbapenem-resistant Enterobacterales in Saudi Arabia. BMC Infect. Dis. 2022, 22, 542. [Google Scholar] [CrossRef]
- Barbara, W.; Trautner, N.W.C.-P.; Kalpana, G.; Elizabeth, B.H.; Molly, H.; Gregory, J.M.; Richard, C.; John, C.O.; Muhammad, S.A.; Shannon, C.; et al. Complicated Urinary Tract Infections (cUTI): Clinical Guidelines for Treatment and Management. IDSA 2025. Available online: https://www.idsociety.org/practice-guideline/complicated-urinary-tract-infections/ (accessed on 25 September 2025).
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratalà, J.; et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Stevens, D.L.; Bisno, A.L.; Chambers, H.F.; Dellinger, E.P.; Goldstein, E.J.; Gorbach, S.L.; Hirschmann, J.V.; Kaplan, S.L.; Montoya, J.G.; Wade, J.C. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2014, 59, e10–e52. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Q.; Yin, Y.; Chen, H.; Jin, L.; Gu, B.; Xie, L.; Yang, C.; Ma, X.; Li, H.; et al. Epidemiology of Carbapenem-Resistant Enterobacteriaceae Infections: Report from the China CRE Network. Antimicrob. Agents Chemother. 2018, 62, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Rebold, N.; Lagnf, A.M.; Alosaimy, S.; Holger, D.J.; Witucki, P.; Mannino, A.; Dierker, M.; Lucas, K.; Kunz Coyne, A.J.; El Ghali, A.; et al. Risk Factors for Carbapenem-Resistant Enterobacterales Clinical Treatment Failure. Microbiol. Spectr. 2023, 11, e0264722. [Google Scholar] [CrossRef] [PubMed]
- Livorsi, D.J.; Chorazy, M.L.; Schweizer, M.L.; Balkenende, E.C.; Blevins, A.E.; Nair, R.; Samore, M.H.; Nelson, R.E.; Khader, K.; Perencevich, E.N. A systematic review of the epidemiology of carbapenem-resistant Enterobacteriaceae in the United States. Antimicrob. Resist. Infect. Control 2018, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Barros, A.; Monroy, H.; Bergo, P.; Beck, E.; David, L.; Rigatto, M.H. Antimicrobial stewardship programme associated with earlier prescription of in vitro susceptible therapy and lower 14-day mortality in patients with carbapenem-resistant Enterobacterales bacteraemia: A cohort study. J. Glob. Antimicrob. Resist. 2022, 28, 130–135. [Google Scholar] [CrossRef]
- Dickstein, Y.; Yahav, D.; Tiseo, G.; Mussini, C.; Franceschini, E.; Santoro, A.; Rahav, G.; Elinav, H.; Potruch, A.; Nutman, A.; et al. Carbapenemase type and mortality in blood-stream infections caused by carbapenemase-producing enterobacterales: A multicenter retrospective cohort study. Infection 2025, 1–11. [Google Scholar] [CrossRef]
- Rodríguez, O.L.; Sousa, A.; Pérez-Rodríguez, M.T.; Martínez-Lamas, L.; Suárez, R.L.; Martínez, C.T.; Pino, C.P.; Vidal, F.V.; Pérez-Landeiro, A.; Casal, M.C. Mortality-related factors in patients with OXA-48 carbapenemase-producing Klebsiella pneumoniae bacteremia. Medicine 2021, 100, e24880. [Google Scholar] [CrossRef]
- Alotaibi, F. Carbapenem-Resistant Enterobacteriaceae: An update narrative review from Saudi Arabia. J. Infect. Public Health 2019, 12, 465–471. [Google Scholar] [CrossRef]
- Gutiérrez-Gutiérrez, B.; Salamanca, E.; de Cueto, M.; Hsueh, P.R.; Viale, P.; Paño-Pardo, J.R.; Venditti, M.; Tumbarello, M.; Daikos, G.; Pintado, V.; et al. A Predictive Model of Mortality in Patients With Bloodstream Infections due to Carbapenemase-Producing Enterobacteriaceae. Mayo Clin. Proc. 2016, 91, 1362–1371. [Google Scholar] [CrossRef]
- Sabino, S.; Soares, S.; Ramos, F.; Moretti, M.; Zavascki, A.P.; Rigatto, M.H. A Cohort Study of the Impact of Carbapenem-Resistant Enterobacteriaceae Infections on Mortality of Patients Presenting with Sepsis. mSphere 2019, 4, 10–1128. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Dyrbye, L.N.; West, C.P.; Sinsky, C.A. Potential Impact of Burnout on the US Physician Workforce. Mayo Clin. Proc. 2016, 91, 1667–1668. [Google Scholar] [CrossRef] [PubMed]
- Teo, J.Q.; Chang, C.W.; Leck, H.; Tang, C.Y.; Lee, S.J.; Cai, Y.; Ong, R.T.; Koh, T.H.; Tan, T.T.; Kwa, A.L. Risk factors and outcomes associated with the isolation of polymyxin B and carbapenem-resistant Enterobacteriaceae spp.: A case-control study. Int. J. Antimicrob. Agents 2019, 53, 657–662. [Google Scholar] [CrossRef]
- Jorgensen, S.C.J.; Trinh, T.D.; Zasowski, E.J.; Lagnf, A.M.; Bhatia, S.; Melvin, S.M.; Simon, S.P.; Rosenberg, J.R.; Steed, M.E.; Estrada, S.J.; et al. Evaluation of the INCREMENT-CPE, Pitt Bacteremia and qPitt Scores in Patients with Carbapenem-Resistant Enterobacteriaceae Infections Treated with Ceftazidime-Avibactam. Infect. Dis. Ther. 2020, 9, 291–304. [Google Scholar] [CrossRef]
- Papadimitriou-Olivgeris, M.; Bartzavali, C.; Georgakopoulou, A.; Kolonitsiou, F.; Mplani, V.; Spiliopoulou, I.; Christofidou, M.; Fligou, F.; Marangos, M. External validation of INCREMENT-CPE score in a retrospective cohort of carbapenemase-producing Klebsiella pneumoniae bloodstream infections in critically ill patients. Clin. Microbiol. Infect. 2021, 27, e911–e915. [Google Scholar] [CrossRef]
- Al Khamis, M.; AlMusa, Z.; Hashhoush, M.; Alsaif, N.; Salam, A.; Atta, M. Carbapenem-Resistant Enterobacteriaceae: A Retrospective Review of Presentation, Treatment, and Clinical Outcomes in a Tertiary Care Referral Hospital. Cureus 2022, 14, e27094. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Values |
|---|---|
| Age (Mean ± SD, years) | 65.1 ± 17.1 |
| Gender | |
| Male | 43 (42.6%) |
| Female | 58 (57.4%) |
| Body weight in kilograms (mean ± SD) | 71.8 ± 18.2 |
| Isolated CRE pathogen | |
| Klebsiella pneumoniae | 95 (94.1%) |
| Escherichia coli | 5 (5.0%) |
| Serratia marcescens | 1 (1.0%) |
| Type of CRE gene | |
| OXA 48 | 71 (70.3%) |
| NDM | 11 (10.9%) |
| OXA 48 and NDM | 19 (18.8%) |
| Type of CRE infection | |
| Urinary tract infection | 36 (35.6%) |
| Bacteremia | 27 (26.7%) |
| Pneumonia | 24 (23.8%) |
| Skin/soft tissue infection | 9 (8.9%) |
| Wound infection | 5 (5.0%) |
| Osteomyelitis | 2 (2.0%) |
| Others | 2 (2.0%) |
| Source of infection | |
| Hospital-acquired | 79 (78.2%) |
| Community-acquired | 22 (21.8%) |
| Baseline renal function (median and IQR) | |
| Serum creatinine (mg/dL) | 1.2 (0.7–2.2) |
| Creatinine clearance (mL/min) | 46 (29–97) |
| Antibiotic combination therapy | 26 (26.5%) |
| CAZ-AVI-based combination | 15 (15.3%) |
| Colistin-based combination | 6 (6.1%) |
| Tigecycline-based combination | 3 (3.1%) |
| Carbapenem-based combination | 2 (2.0%) |
| Antibiotic monotherapy | 72 (73.5%) |
| CAZ-AVI | 41 (41.8%) |
| Colistin | 6 (6.1%) |
| Tigecycline | 5 (5.1%) |
| Carbapenems | 15 (15.3%) |
| Fluoroquinolones | 4 (4.1%) |
| Aminoglycosides | 1 (1.0%) |
| Antibiotic therapy duration (median and IQR) | 12 (7–18) |
| CRE Recurrence | p-Value | 90-Day All-Cause Mortality | p-Value | |||
|---|---|---|---|---|---|---|
| No (n = 84) | Yes (n = 17) | No (n = 58) | Yes (n = 43) | |||
| Age (Mean ± SD, years) | 65.0 ± 17.1 | 65.5 ± 17.6 | 0.902 | 63.2 ± 17.5 | 67.5 ± 16.5 | 0.216 |
| Gender | ||||||
| Male | 37 (44.0%) | 6 (35.3%) | 0.506 | 23 (39.7%) | 20 (46.5%) | 0.491 |
| Female | 47 (56.0%) | 11 (64.7%) | 35 (60.3%) | 23 (53.5%) | ||
| Isolated CRE pathogen | ||||||
| Klebsiella pneumoniae | 78 (92.9%) | 17 (100.0%) | 0.655 | 54 (93.1%) | 41 (95.3%) | 0.261 |
| Escherichia coli | 5 (6.0%) | 0 (0.0%) | 4 (6.9%) | 1 (2.3%) | ||
| Serratia marcescens | 1 (1.2%) | 0 (0.0%) | 0 (0.0%) | 1 (2.3%) | ||
| Type of CRE gene | ||||||
| OXA 48 | 60 (71.4%) | 11 (64.7%) | 0.479 | 43 (74.1%) | 28 (65.1%) | 0.319 |
| NDM | 10 (11.9%) | 1 (5.9%) | 7 (12.1%) | 4 (9.3%) | ||
| OXA 48 and NDM | 14 (16.7%) | 5 (29.4%) | 8 (13.8%) | 11 (25.6%) | ||
| Type of CRE infection | ||||||
| Bacteremia | 28 (33.3%) | 5 (29.4%) | 0.753 | 9 (15.5%) | 24 (55.8%) | <0.001 * |
| Urinary tract infection | 29 (34.5%) | 7 (41.2%) | 0.601 | 27 (46.6%) | 9 (20.9%) | 0.008 * |
| Pneumonia | 21 (25.0%) | 3 (17.6%) | 0.756 | 8 (13.8%) | 16 (37.2%) | 0.006 * |
| Skin/soft tissue infection | 7 (8.3%) | 2 (11.8%) | 0.645 | 8 (13.8%) | 1 (2.3%) | 0.074 |
| Wound infection | 5 (6.0%) | 0 (0.0%) | 0.586 | 4 (6.9%) | 1 (2.3%) | 0.391 |
| Osteomyelitis | 1 (1.2%) | 1 (5.9%) | 0.310 | 2 (3.4%) | 0 (0.0%) | 0.506 |
| Others | 2 (2.4%) | 0 (0.0%) | >0.99 | 1 (1.7%) | 1 (2.3%) | >0.99 |
| Source of infection | ||||||
| Hospital-acquired | 68 (81.0%) | 11 (64.7%) | 0.195 | 43 (74.1%) | 36 (83.7%) | 0.249 |
| Community-acquired | 16 (19.0%) | 6 (35.3%) | 15 (25.9%) | 7 (16.3%) | ||
| Comorbidities | ||||||
| Myocardial infarction | 12 (14.3%) | 1 (5.9%) | 0.690 | 8 (13.8%) | 5 (11.6%) | 0.748 |
| CHF | 14 (16.7%) | 5 (29.4%) | 0.304 | 10 (17.2%) | 9 (20.9%) | 0.639 |
| CVA or TIA | 29 (34.5%) | 5 (29.4%) | 0.684 | 20 (34.5%) | 14 (32.6%) | 0.840 |
| Dementia | 10 (11.9%) | 2 (11.8%) | >0.99 | 7 (12.1%) | 5 (11.6%) | 0.946 |
| COPD | 1 (1.2%) | 0 (0.0%) | >0.99 | 1 (1.7%) | 0 (0.0%) | >0.99 |
| Peptic ulcer disease | 5 (6.0%) | 0 (0.0%) | 0.586 | 2 (3.4%) | 3 (7.0%) | 0.648 |
| Liver disease | 1 (1.2%) | 1 (5.9%) | 0.310 | 0 (0.0%) | 2 (4.7%) | 0.179 |
| Diabetes mellitus | 50 (59.5%) | 15 (88.2%) | 0.024 * | 36 (62.1%) | 29 (67.4%) | 0.577 |
| Hemiplegia | 1 (1.2%) | 1 (5.9%) | 0.310 | 0 (0.0%) | 2 (4.7%) | 0.179 |
| Moderate to severe CKD | 22 (26.2%) | 5 (29.4%) | 0.770 | 14 (24.1%) | 13 (30.2%) | 0.494 |
| Solid tumor | 5 (6.0%) | 1 (5.9%) | >0.99 | 2 (3.4%) | 4 (9.3%) | 0.397 |
| AIDS | 1 (1.2%) | 0 (0.0%) | >0.99 | 1 (1.7%) | 0 (0.0%) | >0.99 |
| Charlson Comorbidity Index # | 4.7 ± 2.6 | 5.3 ± 3.2 | 0.718 | 4.5 ± 2.8 | 5.2 ± 2.4 | 0.139 |
| CRE Recurrence | p-Value | ||
| Possible Predisposing Factors | No (n = 84) | Yes (n = 17) | |
| N (%) | N (%) | ||
| Previous hospitalization within 12 months | 62 (73.8%) | 13 (76.5%) | >0.99 |
| Previous antibiotic exposures within 3 months | 72 (85.7%) | 15 (88.2%) | >0.99 |
| Prolonged LOS (>14 days) | 63 (78.8%) | 16 (94.1%) | 0.183 |
| Antibiotic combination therapy | 22 (27.2%) | 4 (23.5%) | >0.99 |
| CAZ-AVI-based combination | 12 (14.8%) | 3 (17.6%) | 0.721 |
| Colistin-based combination | 6 (7.4%) | 0 (0.0%) | 0.586 |
| Tigecycline-based combination | 2 (2.5%) | 1 (5.9%) | 0.439 |
| Carbapenem-based combination | 2 (2.5%) | 0 (0.0%) | >0.99 |
| Antibiotic Monotherapy | 59 (72.8%) | 13 (76.5%) | >0.99 |
| CAZ-AVI | 34 (42.0%) | 7 (41.2%) | 0.952 |
| Colistin | 4 (4.9%) | 2 (11.8%) | 0.278 |
| Tigecycline | 5 (6.2%) | 0 (0.0%) | 0.584 |
| Carbapenems | 12 (14.8%) | 3 (17.6%) | 0.721 |
| Fluoroquinolones | 3 (3.7%) | 1 (5.9%) | 0.539 |
| Aminoglycosides | 1 (1.2%) | 0 (0.0%) | >0.99 |
| Duration of antibiotic therapy in days # | 10 (7–18) | 13 (10–19) | 0.158 |
| 90-Day All-Cause Mortality | |||
|---|---|---|---|
| Possible Mortality Predictors | No (n = 58) | Yes (n = 43) | p-Value |
| N (%) | N (%) | ||
| Hypotension | 8 (13.8%) | 21 (48.8%) | <0.001 * |
| Cardiac arrest | 3 (5.2%) | 10 (23.3%) | 0.007 * |
| Altered mental status | 4 (6.9%) | 17 (39.5%) | <0.001 * |
| Severe sepsis/septic shock | 9 (15.5%) | 21 (48.8%) | <0.001 * |
| ICU admission | 18 (31.0%) | 37 (86.0%) | <0.001 * |
| Inotropic support | 2 (3.4%) | 16 (37.2%) | <0.001 * |
| CRRT | 2 (3.4%) | 11 (25.6%) | 0.001 * |
| Mechanical ventilation | 8 (13.8%) | 18 (41.9%) | 0.001 * |
| Previous hospitalization within 12 months | 43 (74.1%) | 32 (74.4%) | 0.975 |
| Previous antibiotic exposures within 3 months | 51 (87.9%) | 36 (83.7%) | 0.545 |
| Prolonged LOS (>14 days) | 47 (83.9%) | 32 (78.0%) | 0.462 |
| Pitt bacteremia score # | 0.7 ± 1.9 | 3.3 ± 3.6 | <0.001 * |
| INCREMENT-CPE score # | 4.9 ± 3.1 | 8.7 ± 4.5 | <0.001 * |
| Antibiotic combination therapy | 14 (24.6%) | 12 (29.3%) | 0.603 |
| CAZ-AVI-based combination | 6 (10.5%) | 9 (22.0%) | 0.121 |
| Colistin-based combination | 6 (10.5%) | 0 (0.0%) | 0.039 * |
| Tigecycline-based combination | 1 (1.8%) | 2 (4.9%) | 0.570 |
| Carbapenem-based combination | 1 (1.8%) | 1 (2.4%) | >0.99 |
| Antibiotic Monotherapy | 43 (75.4%) | 29 (70.7%) | 0.603 |
| CAZ-AVI | 24 (42.1%) | 17 (41.5%) | 0.949 |
| Colistin | 2 (3.5%) | 4 (9.8%) | 0.233 |
| Tigecycline | 4 (7.0%) | 1 (2.4%) | 0.396 |
| Carbapenems | 8 (14.0%) | 7 (17.1%) | 0.680 |
| Fluoroquinolones | 4 (7.0%) | 0 (0.0%) | 0.137 |
| Aminoglycosides | 1 (1.8%) | 0 (0.0%) | >0.99 |
| Duration of antibiotic therapy in days # | 12 (7–18) | 10 (5–16) | 0.257 |
| Hazard Ratios | 95% Confidence | p-Value | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Pneumonia | 2.39 | 1.23 | 4.64 | 0.010 |
| Critical care | 6.24 | 2.44 | 15.97 | <0.001 |
| Hypotension | 4.10 | 1.84 | 9.15 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshehail, B.M.; Alwezzeh, M.J.; Almalki, H.H.; Alnimr, A.; Wali, H.; Al Jamea, Z.; Al Rashed, A.S.; Alhajri, M.; Abdulaal, H.A.; Alanbari, L.A.; et al. Recurrence, Readmission, and Key Mortality Predictors in Patients with Carbapenem-Resistant Enterobacterales Infections. Diagnostics 2025, 15, 2957. https://doi.org/10.3390/diagnostics15232957
Alshehail BM, Alwezzeh MJ, Almalki HH, Alnimr A, Wali H, Al Jamea Z, Al Rashed AS, Alhajri M, Abdulaal HA, Alanbari LA, et al. Recurrence, Readmission, and Key Mortality Predictors in Patients with Carbapenem-Resistant Enterobacterales Infections. Diagnostics. 2025; 15(23):2957. https://doi.org/10.3390/diagnostics15232957
Chicago/Turabian StyleAlshehail, Bashayer Mohammed, Marwan Jabr Alwezzeh, Hussain Humaid Almalki, Amani Alnimr, Haytham Wali, Zainab Al Jamea, Abdullatif S. Al Rashed, Mashael Alhajri, Hawra Abdulwahab Abdulaal, Lujain Ali Alanbari, and et al. 2025. "Recurrence, Readmission, and Key Mortality Predictors in Patients with Carbapenem-Resistant Enterobacterales Infections" Diagnostics 15, no. 23: 2957. https://doi.org/10.3390/diagnostics15232957
APA StyleAlshehail, B. M., Alwezzeh, M. J., Almalki, H. H., Alnimr, A., Wali, H., Al Jamea, Z., Al Rashed, A. S., Alhajri, M., Abdulaal, H. A., Alanbari, L. A., Alsowaida, Y. S., Alamri, A., Almuthen, S., Azaiez, F., Alzahrani, S., Zakari, N., Asiri, J., Alanazi, W., Bakkar, M., ... AlBahrani, S. (2025). Recurrence, Readmission, and Key Mortality Predictors in Patients with Carbapenem-Resistant Enterobacterales Infections. Diagnostics, 15(23), 2957. https://doi.org/10.3390/diagnostics15232957






