Normative Data for the Montreal Cognitive Assessment (MoCA) in Mexican Adults: A Regression-Based Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
- •
- For cognition, cognitive performance was assessed using the Trail Making Test (TMT) Parts A and B and verbal fluency tasks [38,39]. The TMT evaluates processing speed, visual attention, and cognitive flexibility, with performance expressed as total response time in seconds for each form (A and B); shorter times indicate better cognitive performance, with typical completion times ranging approximately from 20–80 s for Part A and 40–180 s for Part B, depending on age and education. Verbal fluency was measured through both semantic fluency (naming animals) and phonemic fluency (words beginning with the letter “P”) tasks, which assess lexical access and executive control. Scores correspond to the total number of correct words generated in 60 s, with higher scores reflecting better verbal fluency.
- •
- For functional status, the Lawton–Brody Instrumental Activities of Daily Living (IADL) Scale and the Barthel Activities of Daily Living (ADL) Scale [40,41] were included. The Lawton–Brody IADL Scale evaluates independent functioning in complex daily tasks such as managing finances or medications, with scores ranging from 0 to 8, where higher values indicate greater independence. The Barthel ADL Scale assesses performance in basic self-care activities, such as feeding and mobility, with scores ranging from 0 to 100, where higher scores denote higher functional autonomy.
- •
- For mood status, the Center for Epidemiologic Studies Depression Scale of seven items (CES-D 7) and the Yesavage Geriatric Depression Scale (GDS) [42,43] were used. CES-D 7 measures depressive symptoms in the general population, with scores ranging from 0 to 21, where higher scores reflect greater depressive symptomatology. The Yesavage GDS, applied to participants aged 60 years and older, ranges from 0 to 15, with higher scores indicating more severe depressive symptoms.
- •
- For health status, a total of nine questions about the participants ever being diagnosed with any conditions that directly affect brain health were used. Conditions were: moderate or severe traumatic brain injury, brain tumor, epilepsy, stroke, schizophrenia or other primary psychotic disorders, clinically significant depression or other affective disorders, delirium, uncontrolled diabetes, or uncontrolled hypertension. Participants answered “yes” (=1) or “no” (=0). A dichotomous variable for each question or relevant medical condition was created, followed by a total score ranging from 0 to 9.
- •
- For sociodemographic characteristics, age was used in years as a continuous variable, Gender was coded as a binary variable (female, male) and education was used also in years, as a continuous variable.
2.2. Procedure
2.3. MoCA Administration
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Total MoCA Scores, Age Education and Sex Correlations
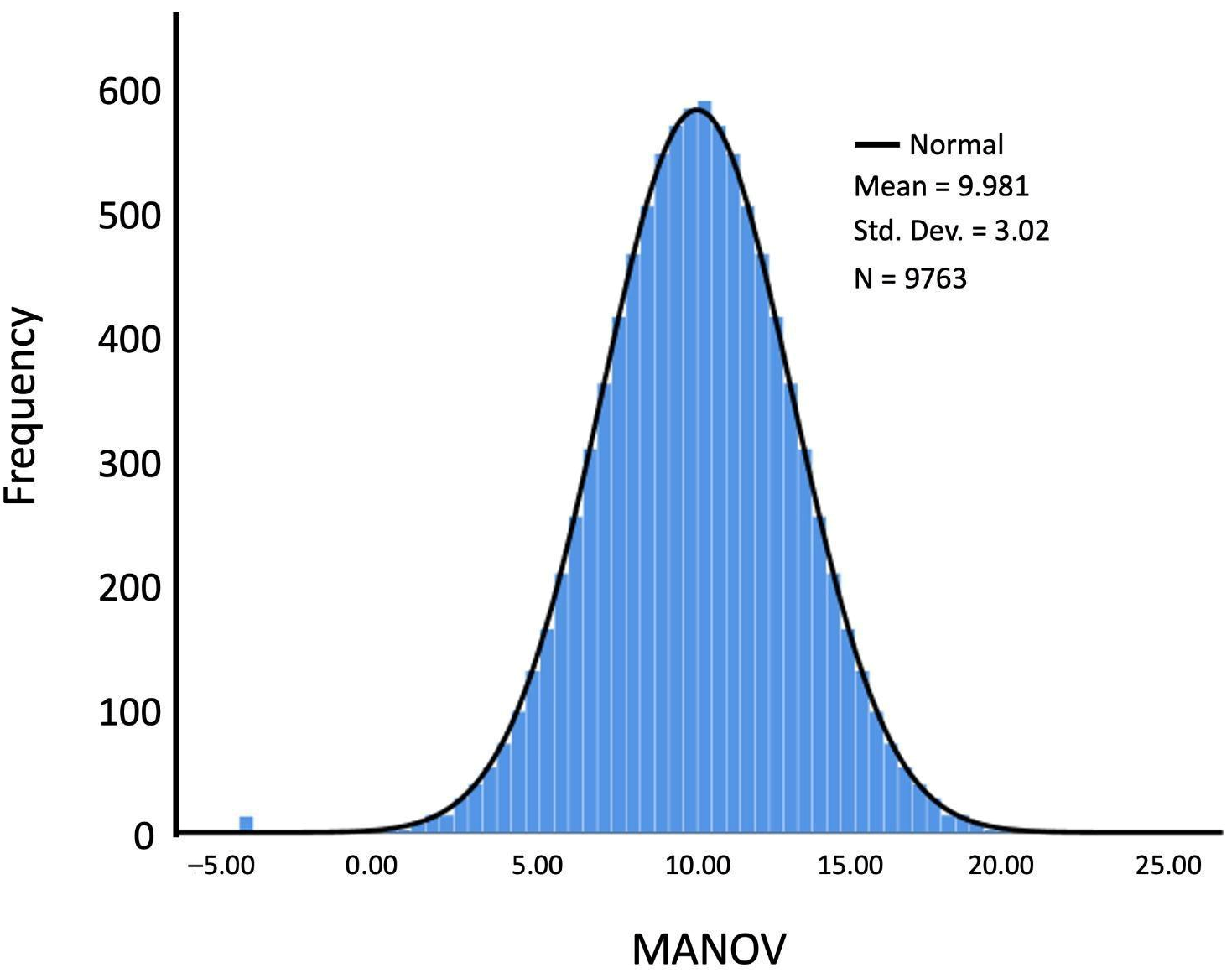
3.3. Age-Adjusted Normative Values
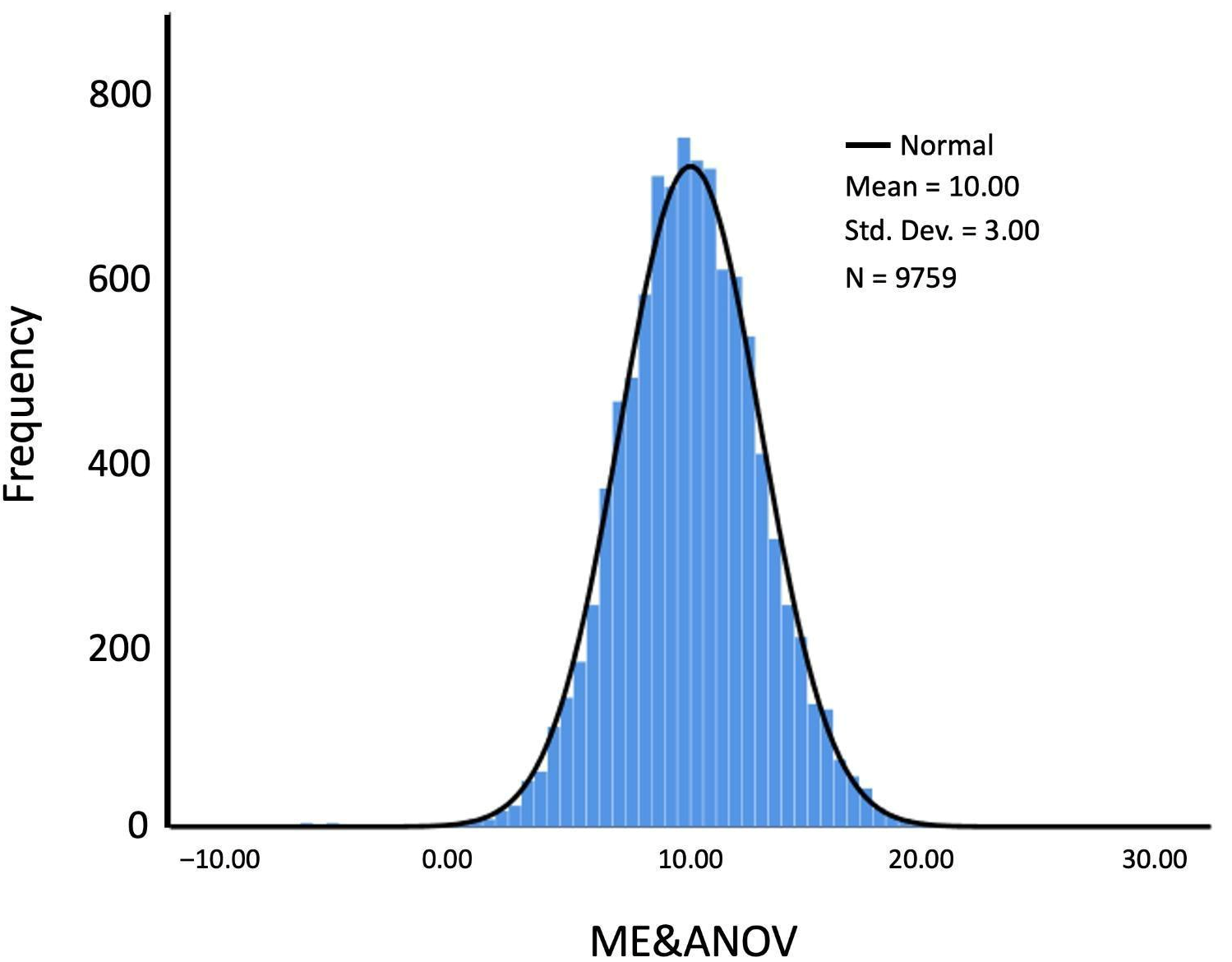
3.4. Education- and Age-Adjusted Normative Values
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Rosca, E.C.; Simu, M. Montreal Cognitive Assessment for Evaluating Cognitive Impairment in Multiple Sclerosis: A Systematic Review. Acta Neurol. Belg. 2020, 120, 1307–1321. [Google Scholar] [CrossRef]
- Scheffels, J.F.; Fröhlich, L.; Kalbe, E.; Kessler, J. Concordance of Mini-Mental State Examination, Montreal Cognitive Assessment and Parkinson Neuropsychometric Dementia Assessment in the Classification of Cognitive Performance in Parkinson’s Disease. J. Neurol. Sci. 2020, 412, 116735. [Google Scholar] [CrossRef]
- Davis, D.H.; Creavin, S.T.; Yip, J.L.; Noel-Storr, A.H.; Brayne, C.; Cullum, S. Montreal Cognitive Assessment for the Detection of Dementia. Cochrane Database Syst. Rev. 2021, 2021, CD010775. [Google Scholar] [CrossRef] [PubMed]
- Potocnik, J.; Ovcar Stante, K.; Rakusa, M. The Validity of the Montreal Cognitive Assessment (MoCA) for the Screening of Vascular Cognitive Impairment after Ischemic Stroke. Acta Neurol. Belg. 2020, 120, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Crivelli, L.; Palmer, K.; Calandri, I.; Guekht, A.; Beghi, E.; Carroll, W.; Frontera, J.; García-Azorín, D.; Westenberg, E.; Winkler, A.S.; et al. Changes in Cognitive Functioning after COVID-19: A Systematic Review and Meta-Analysis. Alzheimers Dement. 2022, 18, 1047–1066. [Google Scholar] [CrossRef]
- Julayanont, P.; Phillips, N.; Chertkow, H.; Nasreddine, Z.S. Montreal Cognitive Assessment (MoCA): Concept and Clinical Review. In Cognitive Screening Instruments: A Practical Approach; Springer Nature: New York, NY, USA, 2013; pp. 111–151. ISBN 978-1-4471-2451-1. [Google Scholar]
- Khan, G.; Mirza, N.; Waheed, W. Developing Guidelines for the Translation and Cultural Adaptation of the Montreal Cognitive Assessment: Scoping Review and Qualitative Synthesis. BJPsych Open 2022, 8, e21. [Google Scholar] [CrossRef]
- Thomann, A.E.; Berres, M.; Goettel, N.; Steiner, L.A.; Monsch, A.U. Enhanced Diagnostic Accuracy for Neurocognitive Disorders: A Revised Cut-off Approach for the Montreal Cognitive Assessment. Alzheimers Res. Ther. 2020, 12, 39. [Google Scholar] [CrossRef] [PubMed]
- Carson, N.; Leach, L.; Murphy, K.J. A Re-Examination of Montreal Cognitive Assessment (MoCA) Cutoff Scores. Int. J. Geriatr. Psychiatry 2018, 33, 379–388. [Google Scholar] [CrossRef]
- Wong, A.; Law, L.S.N.; Liu, W.; Wang, Z.; Lo, E.S.K.; Lau, A.; Wong, L.K.S.; Mok, V.C.T. Montreal Cognitive Assessment: One Cutoff Never Fits All. Stroke 2015, 46, 3547–3550. [Google Scholar] [CrossRef]
- Quang, H.; Nguyen, A.L.; Do, C.; McDonald, S.; Nguyen, C. Examining the Vietnamese Montreal Cognitive Assessment in Healthy and Moderate-to-Severe Traumatic Brain Injury Populations. Clin. Neuropsychol. 2023, 37, 1062–1077. [Google Scholar] [CrossRef]
- Angermann, S.; Baumann, M.; Steubl, D.; Lorenz, G.; Hauser, C.; Suttmann, Y.; Reichelt, A.-L.; Satanovskij, R.; Sonntag, F.; Heemann, U.; et al. Cognitive Impairment in Hemodialysis Patients: Implementation of Cut-off Values for the Montreal Cognitive Assessment (MoCA)-Test for Feasible Screening. PLoS ONE 2017, 12, e0184589. [Google Scholar] [CrossRef]
- Rosca, E.C.; Albarqouni, L.; Simu, M. Montreal Cognitive Assessment (MoCA) for HIV-Associated Neurocognitive Disorders. Neuropsychol. Rev. 2019, 29, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Borda, M.G.; Reyes-Ortiz, C.; Pérez-Zepeda, M.U.; Patino-Hernandez, D.; Gómez-Arteaga, C.; Cano-Gutiérrez, C.A. Educational level and its Association with the domains of the Montreal Cognitive Assessment Test. Aging Ment. Health 2019, 23, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- White, R.S.; Barber, J.M.; Harp, J.P.; Jicha, G.A. Examining the effects of formal education level on the Montreal Cognitive Assessment. J. Am. Board Fam. Med. 2022, 35, 1043–1057. [Google Scholar] [CrossRef] [PubMed]
- Siciliano, M.; Chiorri, C.; Passaniti, C.; Sant’Elia, V.; Trojano, L.; Santangelo, G. Comparison of Alternate and Original Forms of the Montreal Cognitive Assessment (MoCA): An Italian Normative Study. Neurol. Sci. 2019, 40, 691–702. [Google Scholar] [CrossRef]
- Narazaki, K.; Nofuji, Y.; Honda, T.; Matsuo, E.; Yonemoto, K.; Kumagai, S. Normative Data for the Montreal Cognitive Assessment in a Japanese Community-Dwelling Older Population. Neuroepidemiology 2013, 40, 23–29. [Google Scholar] [CrossRef]
- Rossetti, H.C.; Lacritz, L.H.; Cullum, C.M.; Weiner, M.F. Normative Data for the Montreal Cognitive Assessment (MoCA) in a Population-Based Sample. Neurology 2011, 77, 1272–1275. [Google Scholar] [CrossRef]
- Santangelo, G.; Siciliano, M.; Pedone, R.; Vitale, C.; Falco, F.; Bisogno, R.; Siano, P.; Barone, P.; Grossi, D.; Santangelo, F.; et al. Normative Data for the Montreal Cognitive Assessment in an Italian Population Sample. Neurol. Sci. 2015, 36, 585–591. [Google Scholar] [CrossRef]
- OECD. The Future of Mexican Higher Education: Promoting Quality and Equity, Reviews of National Policies for Education; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- Zhou, Y.; Ortiz, F.; Nuñez, C.; Elashoff, D.; Woo, E.; Apostolova, L.G.; Wolf, S.; Casado, M.; Caceres, N.; Panchal, H.; et al. Use of the MoCA in Detecting Early Alzheimer’s Disease in a Spanish-Speaking Population with Varied Levels of Education. Dement. Geriatr. Cogn. Dis. Extra 2015, 5, 85–95. [Google Scholar] [CrossRef]
- Lu, J.; Li, D.; Li, F.; Zhou, A.; Wang, F.; Zuo, X.; Jia, X.-F.; Song, H.; Jia, J. Montreal Cognitive Assessment in Detecting Cognitive Impairment in Chinese Elderly Individuals: A Population-Based Study. J. Geriatr. Psychiatry Neurol. 2011, 24, 184–190. [Google Scholar] [CrossRef]
- Elkana, O.; Tal, N.; Oren, N.; Soffer, S.; Ash, E.L. Is the Cutoff of the MoCA Too High? Longitudinal Data From Highly Educated Older Adults. J. Geriatr. Psychiatry Neurol. 2020, 33, 155–160. [Google Scholar] [CrossRef]
- Cesar, K.G.; Yassuda, M.S.; Porto, F.H.G.; Brucki, S.M.D.; Nitrini, R. MoCA Test: Normative and Diagnostic Accuracy Data for Seniors with Heterogeneous Educational Levels in Brazil. Arq. Neuropsiquiatr. 2019, 77, 775–781. [Google Scholar] [CrossRef]
- Pinto, T.C.C.; Machado, L.; Bulgacov, T.M.; Rodrigues-Júnior, A.L.; Costa, M.L.G.; Ximenes, R.C.C.; Sougey, E.B. Is the Montreal Cognitive Assessment (MoCA) Screening Superior to the Mini-Mental State Examination (MMSE) in the Detection of Mild Cognitive Impairment (MCI) and Alzheimer’s Disease (AD) in the Elderly? Int. Psychogeriatr. 2019, 31, 491–504. [Google Scholar] [CrossRef]
- Gaete, M.; Jorquera, S.; Bello-Lepe, S.; Mendoza, Y.M.; Véliz, M.; Alonso-Sanchez, M.F.; Lira, J. Resultados Estandarizados Del Montreal Cognitive Assessment (MoCA) Para Cribado Neurocognitivo En Población Chilena. Neurología 2023, 38, 246–255. [Google Scholar] [CrossRef]
- Apolinario, D.; Dos Santos, M.F.; Sassaki, E.; Pegoraro, F.; Pedrini, A.V.A.; Cestari, B.; Amaral, A.H.; Mitt, M.; Müller, M.B.; Suemoto, C.K.; et al. Normative Data for the Montreal Cognitive Assessment (MoCA) and the Memory Index Score (MoCA-MIS) in Brazil: Adjusting the Nonlinear Effects of Education with Fractional Polynomials. Int. J. Geriatr. Psychiatry 2018, 33, 893–899. [Google Scholar] [CrossRef]
- Aguilar-Navarro, S.G.; Mimenza-Alvarado, A.J.; Palacios-García, A.A.; Samudio-Cruz, A.; Gutiérrez-Gutiérrez, L.A.; Ávila-Funes, J.A. Validez y Confiabilidad Del MoCA (Montreal Cognitive Assessment) Para El Tamizaje Del Deterioro Cognoscitivo En México. [Validity and Reliability of the Spanish Version of the Montreal Cognitive Assessment (MoCA) for the Detection of Cognitive Impairment in Mexico.]. Rev. Colomb. Psiquiatr. 2018, 47, 237–243. [Google Scholar] [CrossRef]
- O’Driscoll, C.; Shaikh, M. Cross-Cultural Applicability of the Montreal Cognitive Assessment (MoCA): A Systematic Review. J Alzheimers Dis. 2017, 58, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Ge, B.; Wu, S.; Li, H.; Lin, L. Optimal Cut-off MoCA Score for Screening for Mild Cognitive Impairment in Elderly Individuals in China: A Systematic Review and Meta-Analysis. Asian J. Psychiatr. 2023, 87, 103691. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Peng, A.; Lai, W.; Wu, J.; Ji, S.; Hu, D.; Chen, S.; Zhu, C.; Hong, Q.; Zhang, M.; et al. Impacts of Education Level on Montreal Cognitive Assessment and Saccades in Community Residents from Western China. Clin. Neurophysiol. 2024, 161, 27–39. [Google Scholar] [CrossRef]
- delCacho-Tena, A.; Christ, B.R.; Arango-Lasprilla, J.C.; Perrin, P.B.; Rivera, D.; Olabarrieta-Landa, L. Normative Data Estimation in Neuropsychological Tests: A Systematic Review. Arch. Clin. Neuropsychol. 2024, 39, 383–398. [Google Scholar] [CrossRef]
- Ong, R.; Yap, C.W.; Ge, L. Regression-Based Normative Scores for the Montreal Cognitive Assessment (MoCA) in an Asian Population. Sci. Rep. 2025, 15, 17895. [Google Scholar] [CrossRef]
- De Santi, S.; Pirraglia, E.; Barr, W.; Babb, J.; Williams, S.; Rogers, K.; Glodzik, L.; Brys, M.; Mosconi, L.; Reisberg, B.; et al. Robust and Conventional Neuropsychological Norms: Diagnosis and Prediction of Age-Related Cognitive Decline. Neuropsychology 2008, 22, 469–484. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, F.; Tan, F.E.S.; Candel, M.J.J.M.; van Breukelen, G.J.P. Sample Size Calculation and Optimal Design for Regression-Based Norming of Tests and Questionnaires. Psychol. Methods 2023, 28, 89–106. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-García, S.; García-Peña, C.; Salvà, A.; Sánchez-Arenas, R.; Granados-García, V.; Cuadros-Moreno, J.; Velázquez-Olmedo, L.B.; Cárdenas-Bahena, Á. Frailty in Community-Dwelling Older Adults: Association with Adverse Outcomes. Clin. Interv. Aging 2017, 12, 1003–1011. [Google Scholar] [CrossRef]
- Pekkala, S. Verbal Fluency Tasks and the Neuropsychology of Language. In The Handbook of the Neuropsychology of Language, Vol 1: Language Processing in the Brain: Basic Science, Vol 2: Language Processing in the Brain: Clinical Populations; Wiley-Blackwell handbooks of behavioral neuroscience; Wiley Blackwell: Hoboken, NJ, USA, 2012; pp. 619–634. ISBN 978-1-4443-3040-3. [Google Scholar]
- Bowie, C.R.; Harvey, P.D. Administration and Interpretation of the Trail Making Test. Nat. Protoc. 2006, 1, 2277–2281. [Google Scholar] [CrossRef] [PubMed]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A Reliability Study. Int. Disabil. Stud. 1988, 10, 61–63. [Google Scholar] [CrossRef]
- Graf, C. The Lawton Instrumental Activities of Daily Living Scale. Am. J. Nurs. 2008, 108, 52–62. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and Validation of a Geriatric Depression Screening Scale: A Preliminary Report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Arango-Lasprilla, J.C.; Rivera, D.; Aguayo, A.; Rodríguez, W.; Garza, M.T.; Saracho, C.P.; Rodríguez-Agudelo, Y.; Aliaga, A.; Weiler, G.; Luna, M.; et al. Trail Making Test: Normative Data for the Latin American Spanish Speaking Adult Population. NeuroRehabilitation 2015, 37, 639–661. [Google Scholar] [CrossRef]
- Olabarrieta-Landa, L.; Rivera, D.; Galarza-Del-Angel, J.; Garza, M.T.; Saracho, C.P.; Rodríguez, W.; Chávez-Oliveros, M.; Rábago, B.; Leibach, G.; Schebela, S.; et al. Verbal Fluency Tests: Normative Data for the Latin American Spanish Speaking Adult Population. NeuroRehabilitation 2015, 37, 515–561. [Google Scholar] [CrossRef] [PubMed]
- Vergara, I.; Bilbao, A.; Orive, M.; Garcia-Gutierrez, S.; Navarro, G.; Quintana, J.M. Validation of the Spanish Version of the Lawton IADL Scale for Its Application in Elderly People. Health Qual. Life Outcomes 2012, 10, 130. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Ayala, R.E.; Velasco-Rojano, Á.E.; Duarte-Ayala, R.E.; Velasco-Rojano, Á.E. Validación psicométrica del índice de Barthel en adultos mayores mexicanos. Horiz. Sanit. 2022, 21, 113–120. [Google Scholar] [CrossRef]
- García-Peña, C.; Wagner, F.A.; Sánchez-Garcia, S.; Juárez-Cedillo, T.; Espinel-Bermúdez, C.; García-Gonzalez, J.J.; Gallegos-Carrillo, K.; Franco-Marina, F.; Gallo, J.J. Depressive Symptoms Among Older Adults in Mexico City. J. Gen. Intern. Med. 2008, 23, 1973–1980. [Google Scholar] [CrossRef]
- Salinas-Rodríguez, A.; Manrique-Espinoza, B.; Acosta-Castillo, G.I.; Franco-Núñez, A.; Rosas-Carrasco, Ó.; Gutiérrez-Robledo, L.M.; Sosa-Ortiz, A.L. Validación de un punto de corte para la versión breve de la Escala de Depresión del Centro de Estudios Epidemiológicos en adultos mayores mexicanos. Salud Pública México 2014, 56, 279–285. [Google Scholar] [CrossRef]
- Martin, P.K.; Schroeder, R.W.; Baade, L.E. A Tale of Two Norms: The Impact of Normative Sample Selection Criteria on Standardized Scores in Older Adults. Clin. Neuropsychol. 2017, 31, 1204–1218. [Google Scholar] [CrossRef]
- Lucas, J.A.; Ivnik, R.J.; Willis, F.B.; Ferman, T.J.; Smith, G.E.; Parfitt, F.C.; Petersen, R.C.; Graff-Radford, N.R. Mayo’s Older African Americans Normative Studies: Normative Data for Commonly Used Clinical Neuropsychological Measures. Clin. Neuropsychol. 2005, 19, 162–183. [Google Scholar] [CrossRef]
- Peña-Casanova, J.; Blesa, R.; Aguilar, M.; Gramunt-Fombuena, N.; Gómez-Ansón, B.; Oliva, R.; Molinuevo, J.L.; Robles, A.; Barquero, M.S.; Antúnez, C.; et al. Spanish Multicenter Normative Studies (NEURONORMA Project): Methods and Sample Characteristics. Arch. Clin. Neuropsychol. 2009, 24, 307–319. [Google Scholar] [CrossRef]
- Pauker, J.D. Constructing Overlapping Cell Tables to Maximize the Clinical Usefulness of Normative Test Data: Rationale and an Example from Neuropsychology. J. Clin. Psychol. 1988, 44, 930–933. [Google Scholar] [CrossRef]
- Malec, J.F.; Ivnik, R.J.; Smith, G.E.; Tangalos, E.G.; Petersen, R.C.; Kokmen, E.; Kurland, L.T. Mayo’s Older Americans Normative Studies: Utility of Corrections for Age and Education for the WAIS-R. Clin. Neuropsychol. 1992, 6, 31–47. [Google Scholar] [CrossRef]
- Ivnik, R.J.; Malec, J.F.; Smith, G.E.; Tangalos, E.G.; Petersen, R.C.; Kokmen, E.; Kurland, L.T. Mayo’s Older Americans Normative Studies: Updated AVLT Norms for Ages 56 to 97. Clin. Neuropsychol. 1992, 6, 83–104. [Google Scholar] [CrossRef]
- Ivnik, R.J.; Malec, J.F.; Tangalos, E.G.; Petersen, R.C.; Kokmen, E.; Kurland, L.T. The Auditory-Verbal Learning Test (AVLT): Norms for Ages 55 Years and Older. Psychol. Assess. A J. Consult. Clin. Psychol. 1990, 2, 304–312. [Google Scholar] [CrossRef]
- Mungas, D.; Marshall, S.C.; Weldon, M.; Haan, M.; Reed, B.R. Age and Education Correction of Mini-Mental State Examination for English- and Spanish-Speaking Elderly. Neurology 1996, 46, 700–706. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Psychological Testing in the Service of Disability Determination; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar] [CrossRef]
- Sachdev, P.S.; Blacker, D.; Blazer, D.G.; Ganguli, M.; Jeste, D.V.; Paulsen, J.S.; Petersen, R.C. Classifying neurocognitive disorders: The DSM-5 approach. Nat. Rev. Neurol. 2014, 10, 634–642. [Google Scholar] [CrossRef]
- Kessels, R.P.C.; de Vent, N.R.; Bruijnen, C.J.W.H.; Jansen, M.G.; de Jonghe, J.F.M.; Dijkstra, B.A.G.; Oosterman, J.M. Regression-Based Normative Data for the Montreal Cognitive Assessment (MoCA) and Its Memory Index Score (MoCA-MIS) for Individuals Aged 18–91. J. Clin. Med. 2022, 11, 4059. [Google Scholar] [CrossRef]
- Classon, E.; van den Hurk, W.; Lyth, J.; Johansson, M.M. Montreal Cognitive Assessment: Normative Data for Cognitively Healthy Swedish 80- to 94-Year-Olds. J. Alzheimers Dis. 2022, 87, 1335–1344. [Google Scholar] [CrossRef] [PubMed]
- Gillis, C.; Mirzaei, F.; Potashman, M.; Ikram, M.A.; Maserejian, N. The Incidence of Mild Cognitive Impairment: A Systematic Review and Data Synthesis. Alzheimers Dement. 2019, 11, 248–256. [Google Scholar] [CrossRef]
- Islam, N.; Hashem, R.; Gad, M.; Brown, A.; Levis, B.; Renoux, C.; Thombs, B.D.; McInnes, M.D. Accuracy of the Montreal Cognitive Assessment Tool for Detecting Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Alzheimers Dement. 2023, 19, 3235–3243. [Google Scholar] [CrossRef]
- Ciesielska, N.; Sokołowski, R.; Mazur, E.; Podhorecka, M.; Polak-Szabela, A.; Kędziora-Kornatowska, K. Is the Montreal Cognitive Assessment (MoCA) Test Better Suited than the Mini-Mental State Examination (MMSE) in Mild Cognitive Impairment (MCI) Detection among People Aged over 60? Meta-Analysis. Psychiatr. Pol. 2016, 50, 1039–1052. [Google Scholar] [CrossRef] [PubMed]

| Total Sample (n) | 2546 |
| Sex (%) | |
| Male | 43.44 |
| Female | 56.56 |
| Age (%) | |
| 18–34 years | 15.67 |
| 35–54 years | 17.05 |
| 55–64 years | 32.60 |
| 65–74 years | 21.01 |
| 75–99 years | 13.67 |
| Education (%) | |
| Basic (6 or fewer years) | 22.02 |
| Intermediate (7 until 12 years) | 32.10 |
| Superior (13 to 15 years) | 32.68 |
| Above superior (more than 15 years) | 13.20 |
| Groups | Mid-Point Age | Age Range for Mid-Points | Age Range for Norms | Sample Size MOCA |
|---|---|---|---|---|
| 1 | 29 | ≤31 | 19–39 | 452 |
| 2 | 34 | 32–36 | 24–44 | 368 |
| 3 | 39 | 37–41 | 29–49 | 380 |
| 4 | 44 | 42–46 | 34–54 | 369 |
| 5 | 49 | 47–51 | 39–59 | 370 |
| 6 | 54 | 52–56 | 44–64 | 1099 |
| 7 | 59 | 57–61 | 49–69 | 1462 |
| 8 | 64 | 62–66 | 54–74 | 1473 |
| 9 | 69 | 67–71 | 59–79 | 1595 |
| 10 | 74 | 72–76 | 64–84 | 1073 |
| 11 | 79 | 77–81 | 69–89 | 545 |
| 12 | 84 | 82–86 | 74–94 | 384 |
| 13 | 89 | ≥87 | 79–99 | 193 |
| MOCA | Age (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | ≤31 | 32–36 | 37–41 | 42–46 | 47–51 | 52–56 | 57–61 | 62–66 | 67–71 | 72–76 | 77–81 | 82–86 | ≥87 |
| 1 | 0 | 0 | 0 | ||||||||||
| 2 | 0 | 1 | 2 | ||||||||||
| 3 | |||||||||||||
| 4 | 1 | 2 | 2 | 0 | |||||||||
| 5 | 1 | 2 | 3 | 3 | 2 | ||||||||
| 6 | 0 | 0 | 2 | 2 | 3 | 3 | 3 | ||||||
| 7 | 0 | 1 | 1 | 2 | 3 | 3 | 4 | 4 | |||||
| 8 | 2 | 2 | 3 | 3 | 4 | 4 | 5 | ||||||
| 9 | 2 | 2 | 3 | 3 | 4 | 4 | 5 | 5 | |||||
| 10 | 3 | 3 | 3 | 4 | 4 | 5 | 5 | 6 | |||||
| 11 | 3 | 3 | 3 | 4 | 4 | 5 | 6 | 6 | |||||
| 12 | 3 | 3 | 4 | 4 | 5 | 6 | 6 | 6 | |||||
| 13 | 4 | 4 | 4 | 5 | 5 | 6 | 7 | 7 | |||||
| 14 | 4 | 4 | 5 | 5 | 6 | 7 | 7 | 8 | |||||
| 15 | 5 | 5 | 5 | 5 | 6 | 7 | 8 | 8 | |||||
| 16 | 5 | 5 | 5 | 6 | 7 | 8 | 8 | 8 | |||||
| 17 | 0 | 0 | 5 | 6 | 6 | 6 | 7 | 8 | 9 | 9 | |||
| 18 | 2 | 2 | 6 | 6 | 7 | 7 | 8 | 8 | 9 | 9 | |||
| 19 | 0 | 1 | 1 | 3 | 3 | 7 | 7 | 7 | 8 | 8 | 9 | 9 | 10 |
| 20 | 3 | 4 | 4 | 7 | 8 | 8 | 8 | 9 | 9 | 10 | 10 | ||
| 21 | 2 | 3 | 4 | 5 | 5 | 8 | 8 | 8 | 9 | 9 | 10 | 10 | 11 |
| 22 | 3 | 4 | 5 | 5 | 6 | 8 | 9 | 9 | 9 | 10 | 10 | 11 | 11 |
| 23 | 4 | 5 | 5 | 6 | 6 | 9 | 9 | 9 | 10 | 10 | 11 | 11 | 12 |
| 24 | 5 | 5 | 6 | 6 | 7 | 9 | 10 | 10 | 10 | 11 | 11 | 12 | 12 |
| 25 | 6 | 6 | 7 | 7 | 8 | 10 | 11 | 11 | 11 | 12 | 12 | 12 | 13 |
| 26 | 8 | 8 | 8 | 9 | 9 | 11 | 11 | 12 | 12 | 13 | 13 | 13 | 14 |
| 27 | 9 | 9 | 10 | 11 | 11 | 12 | 13 | 13 | 13 | 14 | 14 | 15 | 15 |
| 28 | 11 | 11 | 12 | 12 | 12 | 14 | 14 | 14 | 15 | 15 | 15 | 16 | 16 |
| 29 | 13 | 13 | 13 | 14 | 14 | 15 | 16 | 16 | 16 | 16 | 17 | 17 | 17 |
| 30 | 16 | 16 | 16 | 16 | 17 | 18 | 18 | 18 | 18 | 18 | 19 | 18 | 18 |
| MOCA | Age (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | ≤31 | 32–36 | 37–41 | 42–46 | 47–51 | 52–56 | 57–61 | 62–66 | 67–71 | 72–76 | 77–81 | 82–86 | ≥87 |
| 1 | 2 | 2 | 2 | ||||||||||
| 2 | 3 | 4 | 4 | ||||||||||
| 3 | |||||||||||||
| 4 | 3 | 4 | 5 | 2 | |||||||||
| 5 | 4 | 4 | 5 | 5 | 5 | ||||||||
| 6 | 2 | 2 | 4 | 5 | 5 | 6 | 6 | ||||||
| 7 | 3 | 3 | 3 | 5 | 5 | 6 | 6 | 7 | |||||
| 8 | 4 | 4 | 5 | 6 | 6 | 7 | 7 | ||||||
| 9 | 4 | 5 | 5 | 6 | 6 | 7 | 7 | 8 | |||||
| 10 | 5 | 5 | 5 | 6 | 7 | 7 | 8 | 8 | |||||
| 11 | 5 | 5 | 6 | 6 | 7 | 8 | 8 | 8 | |||||
| 12 | 6 | 6 | 6 | 7 | 7 | 8 | 9 | 9 | |||||
| 13 | 6 | 6 | 7 | 7 | 8 | 9 | 9 | 10 | |||||
| 14 | 7 | 7 | 7 | 8 | 8 | 9 | 10 | 10 | |||||
| 15 | 7 | 7 | 8 | 8 | 9 | 10 | 10 | 11 | |||||
| 16 | 8 | 8 | 8 | 9 | 9 | 10 | 11 | 11 | |||||
| 17 | 2 | 2 | 8 | 8 | 9 | 9 | 10 | 11 | 11 | 12 | |||
| 18 | 4 | 4 | 9 | 9 | 9 | 10 | 10 | 11 | 12 | 12 | |||
| 19 | 2 | 3 | 3 | 5 | 5 | 9 | 10 | 10 | 10 | 11 | 12 | 12 | 13 |
| 20 | 5 | 6 | 6 | 10 | 10 | 10 | 11 | 11 | 12 | 13 | 13 | ||
| 21 | 4 | 6 | 6 | 7 | 7 | 11 | 11 | 11 | 11 | 12 | 13 | 13 | 14 |
| 22 | 6 | 6 | 7 | 8 | 8 | 11 | 11 | 12 | 12 | 12 | 13 | 14 | 14 |
| 23 | 7 | 7 | 8 | 9 | 9 | 12 | 12 | 12 | 13 | 13 | 14 | 14 | 15 |
| 24 | 8 | 8 | 8 | 9 | 10 | 12 | 13 | 13 | 13 | 14 | 15 | 15 | 15 |
| 25 | 9 | 9 | 9 | 10 | 10 | 13 | 13 | 14 | 14 | 15 | 15 | 16 | 16 |
| 26 | 10 | 10 | 11 | 12 | 12 | 14 | 15 | 15 | 15 | 16 | 16 | 17 | 17 |
| 27 | 12 | 12 | 13 | 14 | 14 | 16 | 16 | 16 | 17 | 17 | 18 | 18 | 18 |
| 28 | 14 | 14 | 15 | 15 | 15 | 17 | 17 | 18 | 18 | 18 | 19 | 19 | 19 |
| 29 | 16 | 16 | 16 | 17 | 17 | 19 | 19 | 19 | 20 | 20 | 21 | 21 | 20 |
| 30 | 20 | 19 | 19 | 20 | 20 | 21 | 22 | 22 | 22 | 22 | 22 | 22 | 21 |
| MOCA | Age (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | ≤31 | 32–36 | 37–41 | 42–46 | 47–51 | 52–56 | 57–61 | 62–66 | 67–71 | 72–76 | 77–81 | 82–86 | ≥87 |
| 1 | 1 | 1 | 1 | ||||||||||
| 2 | 2 | 3 | 3 | ||||||||||
| 3 | |||||||||||||
| 4 | 2 | 3 | 4 | 1 | |||||||||
| 5 | 3 | 3 | 4 | 4 | 4 | ||||||||
| 6 | 1 | 1 | 3 | 4 | 5 | 5 | 5 | ||||||
| 7 | 2 | 2 | 2 | 4 | 4 | 5 | 6 | 6 | |||||
| 8 | 3 | 3 | 4 | 5 | 6 | 6 | 6 | ||||||
| 9 | 3 | 4 | 4 | 5 | 5 | 6 | 7 | 7 | |||||
| 10 | 4 | 4 | 5 | 5 | 6 | 6 | 7 | 7 | |||||
| 11 | 4 | 5 | 5 | 5 | 6 | 7 | 7 | 8 | |||||
| 12 | 5 | 5 | 5 | 6 | 7 | 7 | 8 | 8 | |||||
| 13 | 5 | 5 | 6 | 6 | 7 | 8 | 9 | 9 | |||||
| 14 | 6 | 6 | 6 | 7 | 8 | 8 | 9 | 10 | |||||
| 15 | 6 | 6 | 7 | 7 | 8 | 9 | 10 | 10 | |||||
| 16 | 7 | 7 | 7 | 8 | 9 | 9 | 10 | 10 | |||||
| 17 | 1 | 1 | 7 | 8 | 8 | 8 | 9 | 10 | 11 | 11 | |||
| 18 | 3 | 3 | 8 | 8 | 8 | 9 | 9 | 10 | 11 | 11 | |||
| 19 | 1 | 3 | 3 | 4 | 4 | 9 | 9 | 9 | 9 | 10 | 11 | 12 | 12 |
| 20 | 4 | 5 | 6 | 9 | 9 | 10 | 10 | 10 | 11 | 12 | 12 | ||
| 21 | 4 | 5 | 5 | 6 | 7 | 10 | 10 | 10 | 11 | 11 | 12 | 13 | 13 |
| 22 | 5 | 6 | 6 | 7 | 7 | 10 | 11 | 11 | 11 | 12 | 13 | 13 | 14 |
| 23 | 6 | 6 | 7 | 8 | 8 | 11 | 11 | 11 | 12 | 12 | 13 | 14 | 14 |
| 24 | 7 | 7 | 8 | 8 | 9 | 11 | 12 | 12 | 13 | 13 | 14 | 14 | 14 |
| 25 | 8 | 8 | 8 | 9 | 9 | 12 | 13 | 13 | 13 | 14 | 14 | 15 | 15 |
| 26 | 9 | 10 | 10 | 11 | 11 | 13 | 14 | 14 | 14 | 15 | 15 | 16 | 16 |
| 27 | 11 | 11 | 12 | 13 | 13 | 15 | 15 | 15 | 16 | 16 | 17 | 17 | 17 |
| 28 | 13 | 13 | 14 | 14 | 15 | 16 | 16 | 17 | 17 | 17 | 18 | 18 | 18 |
| 29 | 15 | 15 | 15 | 16 | 16 | 18 | 18 | 18 | 19 | 19 | 20 | 20 | 19 |
| 30 | 19 | 19 | 19 | 19 | 19 | 20 | 21 | 21 | 21 | 21 | 21 | 21 | 20 |
| MOCA | Age (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | ≤31 | 32–36 | 37–41 | 42–46 | 47–51 | 52–56 | 57–61 | 62–66 | 67–71 | 72–76 | 77–81 | 82–86 | ≥87 |
| 1 | 0 | 0 | 0 | ||||||||||
| 2 | 0 | 1 | 2 | ||||||||||
| 3 | |||||||||||||
| 4 | 1 | 2 | 2 | 0 | |||||||||
| 5 | 1 | 2 | 3 | 3 | 2 | ||||||||
| 6 | 0 | 0 | 2 | 2 | 3 | 4 | 3 | ||||||
| 7 | 0 | 1 | 1 | 2 | 3 | 4 | 4 | 4 | |||||
| 8 | 2 | 2 | 3 | 3 | 4 | 5 | 5 | ||||||
| 9 | 2 | 2 | 3 | 3 | 4 | 5 | 5 | 5 | |||||
| 10 | 3 | 3 | 3 | 4 | 4 | 5 | 6 | 6 | |||||
| 11 | 3 | 3 | 3 | 4 | 5 | 5 | 6 | 6 | |||||
| 12 | 3 | 3 | 4 | 4 | 5 | 6 | 7 | 7 | |||||
| 13 | 4 | 4 | 4 | 5 | 6 | 7 | 7 | 8 | |||||
| 14 | 4 | 5 | 5 | 5 | 6 | 7 | 8 | 8 | |||||
| 15 | 5 | 5 | 5 | 6 | 7 | 7 | 8 | 8 | |||||
| 16 | 5 | 6 | 6 | 6 | 7 | 8 | 9 | 9 | |||||
| 17 | 0 | 0 | 6 | 6 | 6 | 7 | 8 | 9 | 9 | 10 | |||
| 18 | 2 | 2 | 6 | 7 | 7 | 7 | 8 | 9 | 10 | 10 | |||
| 19 | 0 | 1 | 1 | 3 | 3 | 7 | 7 | 8 | 8 | 8 | 9 | 10 | 10 |
| 20 | 3 | 4 | 4 | 8 | 8 | 8 | 9 | 9 | 10 | 11 | 11 | ||
| 21 | 2 | 3 | 4 | 5 | 5 | 8 | 9 | 9 | 9 | 10 | 10 | 11 | 12 |
| 22 | 3 | 4 | 5 | 6 | 6 | 9 | 9 | 9 | 10 | 10 | 11 | 12 | 12 |
| 23 | 4 | 5 | 6 | 6 | 7 | 9 | 10 | 10 | 10 | 11 | 12 | 12 | 13 |
| 24 | 5 | 6 | 6 | 7 | 7 | 10 | 10 | 11 | 11 | 11 | 12 | 13 | 13 |
| 25 | 6 | 7 | 7 | 8 | 8 | 11 | 11 | 11 | 12 | 12 | 13 | 13 | 14 |
| 26 | 8 | 8 | 9 | 9 | 10 | 12 | 12 | 12 | 13 | 13 | 14 | 14 | 15 |
| 27 | 10 | 10 | 11 | 11 | 11 | 13 | 14 | 14 | 14 | 15 | 15 | 16 | 16 |
| 28 | 12 | 12 | 12 | 13 | 13 | 15 | 15 | 15 | 16 | 16 | 16 | 17 | 17 |
| 29 | 14 | 13 | 14 | 15 | 15 | 16 | 17 | 17 | 17 | 17 | 18 | 18 | 18 |
| 30 | 17 | 17 | 17 | 18 | 18 | 19 | 19 | 19 | 20 | 20 | 20 | 20 | 19 |
| MOCA | Age (Years) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | ≤31 | 32–36 | 37–41 | 42–46 | 47–51 | 52–56 | 57–61 | 62–66 | 67–71 | 72–76 | 77–81 | 82–86 | ≥87 |
| 1 | 0 | 0 | 0 | ||||||||||
| 2 | 0 | 0 | 0 | ||||||||||
| 3 | |||||||||||||
| 4 | 0 | 1 | 1 | 0 | |||||||||
| 5 | 0 | 0 | 1 | 2 | 1 | ||||||||
| 6 | 0 | 0 | 0 | 1 | 2 | 2 | 2 | ||||||
| 7 | 0 | −1 | −1 | 1 | 1 | 2 | 3 | 3 | |||||
| 8 | 0 | 1 | 1 | 2 | 3 | 3 | 3 | ||||||
| 9 | 0 | 1 | 1 | 2 | 3 | 3 | 4 | 4 | |||||
| 10 | 1 | 1 | 2 | 2 | 3 | 4 | 4 | 4 | |||||
| 11 | 1 | 2 | 2 | 3 | 3 | 4 | 4 | 5 | |||||
| 12 | 2 | 2 | 2 | 3 | 4 | 4 | 5 | 5 | |||||
| 13 | 2 | 2 | 3 | 3 | 4 | 5 | 6 | 6 | |||||
| 14 | 3 | 3 | 3 | 4 | 5 | 6 | 6 | 7 | |||||
| 15 | 3 | 4 | 4 | 4 | 5 | 6 | 7 | 7 | |||||
| 16 | 4 | 4 | 4 | 5 | 6 | 6 | 7 | 7 | |||||
| 17 | 0 | 0 | 4 | 5 | 5 | 5 | 6 | 7 | 8 | 8 | |||
| 18 | 0 | 0 | 5 | 5 | 5 | 6 | 7 | 7 | 8 | 8 | |||
| 19 | 0 | 0 | 0 | 2 | 1 | 6 | 6 | 6 | 7 | 7 | 8 | 9 | 9 |
| 20 | 2 | 3 | 3 | 6 | 7 | 7 | 7 | 8 | 8 | 9 | 10 | ||
| 21 | 1 | 2 | 2 | 3 | 4 | 7 | 7 | 7 | 8 | 8 | 9 | 10 | 10 |
| 22 | 2 | 3 | 3 | 4 | 5 | 7 | 8 | 8 | 8 | 9 | 10 | 10 | 11 |
| 23 | 3 | 4 | 4 | 5 | 5 | 8 | 8 | 8 | 9 | 9 | 10 | 11 | 11 |
| 24 | 4 | 4 | 5 | 5 | 6 | 8 | 9 | 9 | 10 | 10 | 11 | 11 | 12 |
| 25 | 5 | 5 | 5 | 6 | 7 | 9 | 10 | 10 | 10 | 11 | 11 | 12 | 12 |
| 26 | 6 | 7 | 7 | 8 | 8 | 10 | 11 | 11 | 11 | 12 | 12 | 13 | 13 |
| 27 | 8 | 8 | 9 | 10 | 10 | 12 | 12 | 12 | 13 | 13 | 14 | 14 | 14 |
| 28 | 10 | 10 | 11 | 12 | 12 | 13 | 14 | 14 | 14 | 14 | 15 | 15 | 15 |
| 29 | 12 | 12 | 12 | 13 | 13 | 15 | 15 | 15 | 16 | 16 | 17 | 17 | 16 |
| 30 | 16 | 16 | 16 | 16 | 16 | 17 | 18 | 18 | 18 | 18 | 19 | 18 | 17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parra-Rodríguez, L.; Silva-Pereyra, J.; Sánchez-García, S.; García-Peña, C.; Flores-Vázquez, J.F.; Roa-Rojas, P. Normative Data for the Montreal Cognitive Assessment (MoCA) in Mexican Adults: A Regression-Based Approach. Diagnostics 2025, 15, 2920. https://doi.org/10.3390/diagnostics15222920
Parra-Rodríguez L, Silva-Pereyra J, Sánchez-García S, García-Peña C, Flores-Vázquez JF, Roa-Rojas P. Normative Data for the Montreal Cognitive Assessment (MoCA) in Mexican Adults: A Regression-Based Approach. Diagnostics. 2025; 15(22):2920. https://doi.org/10.3390/diagnostics15222920
Chicago/Turabian StyleParra-Rodríguez, Lorena, Juan Silva-Pereyra, Sergio Sánchez-García, Carmen García-Peña, Juan Francisco Flores-Vázquez, and Paloma Roa-Rojas. 2025. "Normative Data for the Montreal Cognitive Assessment (MoCA) in Mexican Adults: A Regression-Based Approach" Diagnostics 15, no. 22: 2920. https://doi.org/10.3390/diagnostics15222920
APA StyleParra-Rodríguez, L., Silva-Pereyra, J., Sánchez-García, S., García-Peña, C., Flores-Vázquez, J. F., & Roa-Rojas, P. (2025). Normative Data for the Montreal Cognitive Assessment (MoCA) in Mexican Adults: A Regression-Based Approach. Diagnostics, 15(22), 2920. https://doi.org/10.3390/diagnostics15222920






