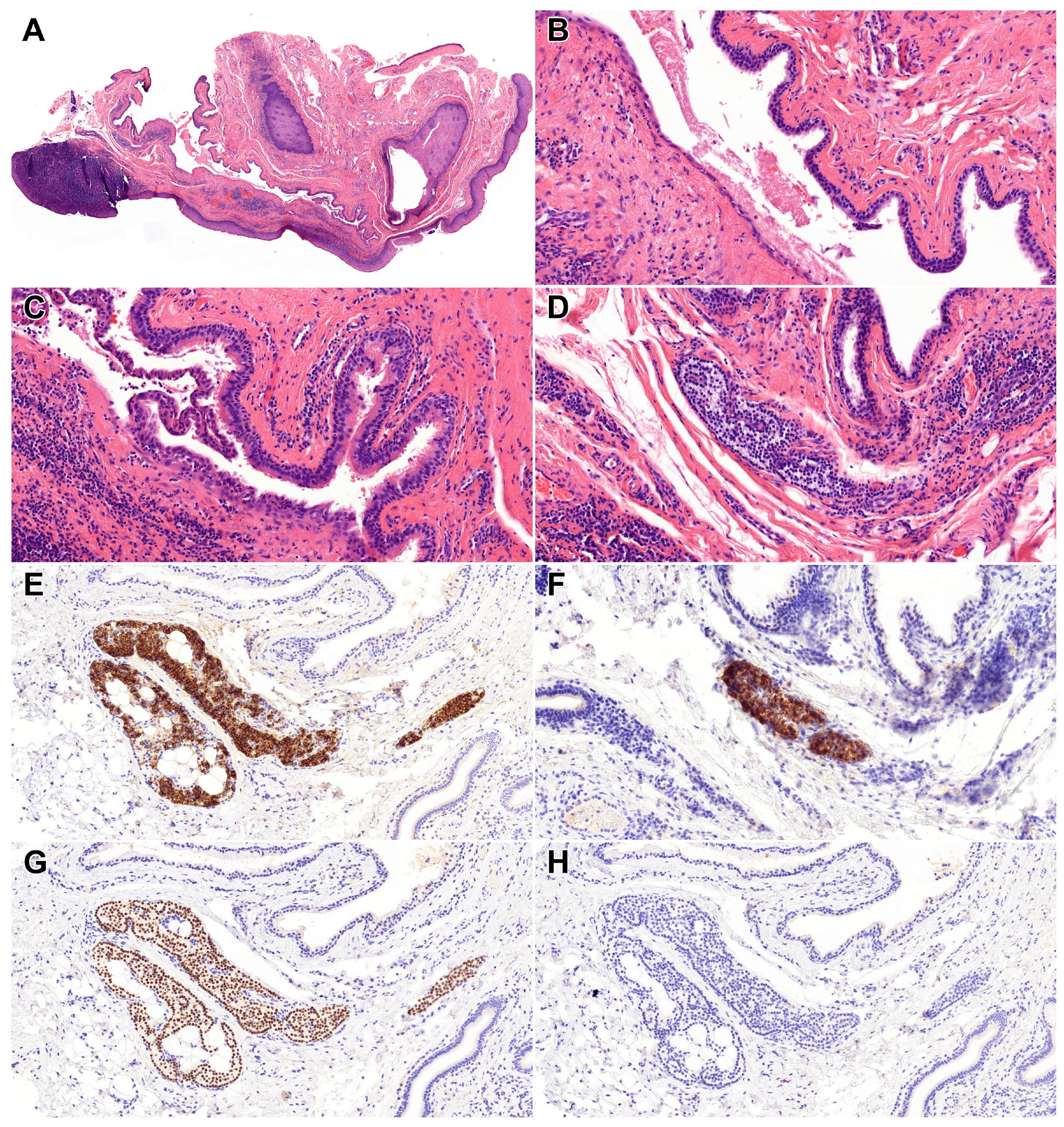
Uvular Branchial Cleft Cyst with Ectopic Parathyroid
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FNAC | Fine needle aspiration cytology |
| GATA3 | GATA binding protein 3 |
| HE | Hematoxylin and eosin |
| MALT | Mucosa-associated lymphoid tissue |
| PTH | Parathyroid hormone |
| TTF1 | Thyroid transcription factor-1 |
References
- Harmon, K.A.; Fegan, A.; La-Anyane, O.; Theis, S.M.; Tragos, C. Uvular dermoid cyst: More than just a lump in the throat-management of resultant velopharyngeal insufficiency. J. Craniofac. Surg. 2023, 34, e534–e536. [Google Scholar] [CrossRef]
- Lim, H.R.; Cho, H.H.; Yang, H.C.; Kim, H.C. An epidermoid cyst of the uvula causing dyspnea in an infant: A case report. Medicine 2020, 99, e22573. [Google Scholar] [CrossRef] [PubMed]
- Daram, S.; Ulualp, S.O.; Uddin, N. Epidermoid cyst of the uvula in a child. SAGE Open Med. Case Rep. 2016, 4, 2050313X16683629. [Google Scholar] [CrossRef] [PubMed]
- Salas, S.V.; Pedro, K.; Balram, A.; Syed, S.; Kotaka, K.; Kadivar, A.; Eke, B.O.; McFarland, M.; Sung, M.; Behera, N.; et al. Head and neck cystic lesions: A cytology review of common and uncommon entities. Acta Cytol. 2022, 66, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.; Heffelfinger, R. Low-grade B-cell lymphoma presenting as a uvular mass. Ear Nose Throat. J. 2012, 91, E22–E24. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.S.; Wang, C.H.; Shih, C.P. T-cell lymphoma manifesting as uvular mass. Rheumatology 2013, 52, 608. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hamada, Y.; Tanaka, K.; Horiki, N.; Nakagawa, H. Early uvular cancer detected by esophagogastroduodenoscopy. Intern. Med. 2022, 61, 3141–3142. [Google Scholar] [CrossRef] [PubMed]
- Overton, L.J.; Fritsch, V.A.; Lentsch, E.J. Squamous cell carcinoma of the uvula: An analysis of factors affecting survival. Laryngoscope 2013, 123, 898–903. [Google Scholar] [CrossRef] [PubMed]
- Wareing, M.J.; Irving, R.M.; Moffat, D.A. Parapharyngeal space tumour presenting as recurrent uvular oedema. J. Laryngol. Otol. 1993, 107, 640–641. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Eguchi, K.; Yoshida, N. Papillary thyroid carcinoma with a retropharyngeal cystic goitre extending into the pharyngeal mucosal space. BMJ Case Rep. 2024, 17, e258684. [Google Scholar] [CrossRef] [PubMed]
- Noussios, G.; Anagnostis, P.; Natsis, K. Ectopic parathyroid glands and their anatomical, clinical and surgical implications. Exp. Clin. Endocrinol. Diabetes 2012, 120, 604–610. [Google Scholar] [CrossRef]
- Okuda, I.; Nakajima, Y.; Maruno, H.; Kohno, T.; Hirata, K. Diagnostic localization of ectopic parathyroid lesions: Developmental consideration. Jpn. J. Radiol. 2010, 28, 707–713. [Google Scholar] [CrossRef]
- Anemoulis, M.; Kachtsidis, V.; Geropoulos, G.; Panagiotopoulos, N. Robot-assisted thoracoscopic resection of ectopic parathyroid tissue in mediastinum: A scoping review. Innovations 2024, 19, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Kwak, S.; Fishman, E.K. Ectopic mediastinal parathyroid: A case report of recurrent secondary hyperparathyroidism. Radiol. Case. Rep. 2023, 18, 2229–2231. [Google Scholar] [CrossRef] [PubMed]
- Hartert, M.; Tripsy, J.; Huertgen, M. Technique for ectopic intrathymic parathyroid adenoma: The uniportal subxiphoid approach. J. Surg. Case Rep. 2021, 2021, rjab520. [Google Scholar] [CrossRef] [PubMed]
- Rabazzi, G.; Elia, G.; Aprile, V.; Korasidis, S.; Mastromarino, M.G.; Bacchin, D.; Lenzini, A.; Ambrogi, M.C.; Alí, G.; Cetani, F.; et al. Surgical management of mediastinal ectopic parathyroids. J. Pers. Med. 2025, 15, 276. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sejben, A.; Lantos, T.; Sejben, I. Uvular Branchial Cleft Cyst with Ectopic Parathyroid. Diagnostics 2025, 15, 2748. https://doi.org/10.3390/diagnostics15212748
Sejben A, Lantos T, Sejben I. Uvular Branchial Cleft Cyst with Ectopic Parathyroid. Diagnostics. 2025; 15(21):2748. https://doi.org/10.3390/diagnostics15212748
Chicago/Turabian StyleSejben, Anita, Tamás Lantos, and István Sejben. 2025. "Uvular Branchial Cleft Cyst with Ectopic Parathyroid" Diagnostics 15, no. 21: 2748. https://doi.org/10.3390/diagnostics15212748
APA StyleSejben, A., Lantos, T., & Sejben, I. (2025). Uvular Branchial Cleft Cyst with Ectopic Parathyroid. Diagnostics, 15(21), 2748. https://doi.org/10.3390/diagnostics15212748







