Placental Pathological Findings and Clinical Outcomes in Triplet Pregnancies Conceived via Oocyte Donation and Non-Oocyte Donation: A Case–Control Study
Abstract
1. Introduction
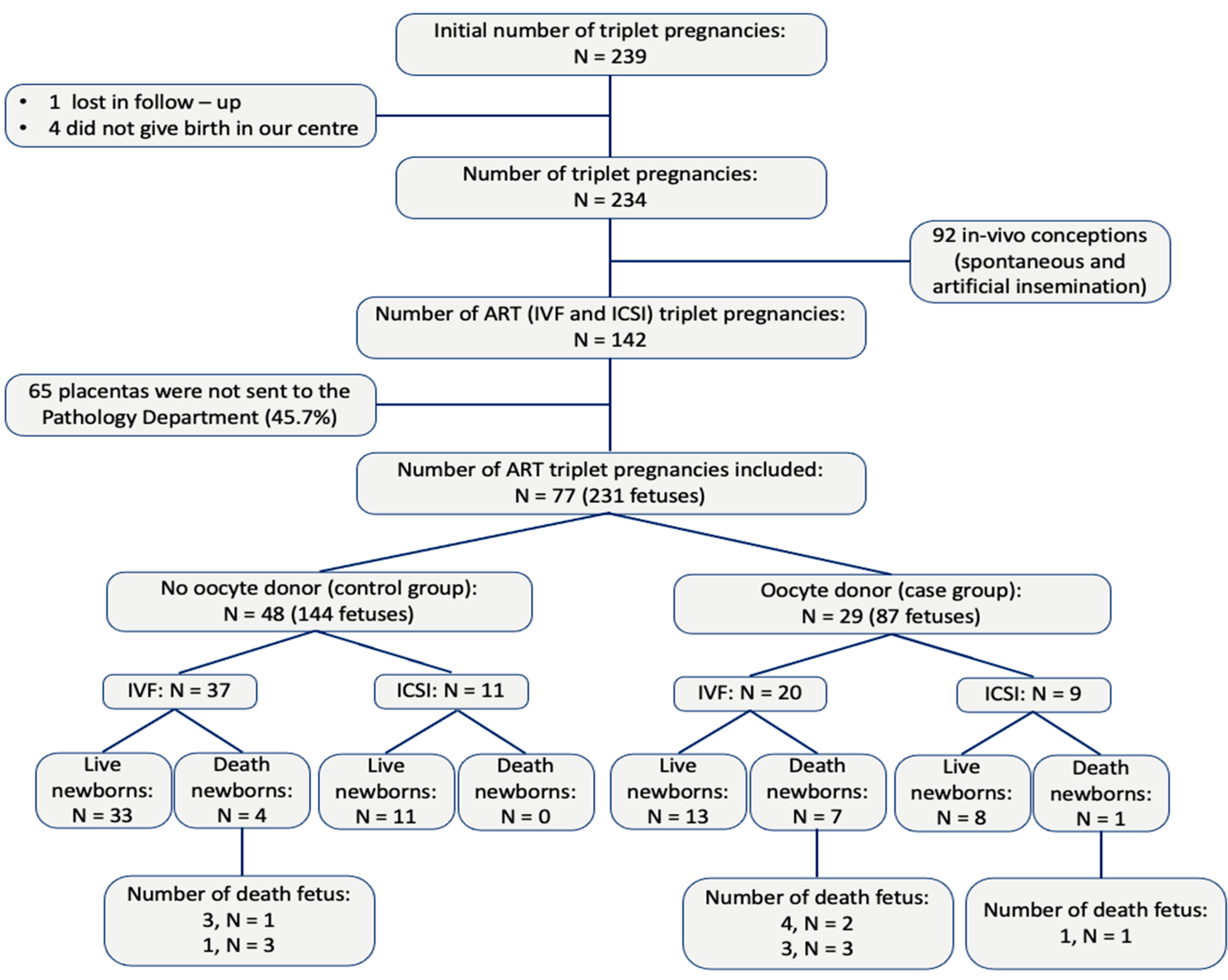
2. Materials and Methods
2.1. Study Design and Eligibility Criteria
2.2. ART Procedures and Oocyte Donor Selection
2.3. Basal Study Variables
2.4. Maternal, Obstetric and Neonatal Outcomes
2.5. Gross Placental Evaluation and Gross Variables
2.6. Pathological Examination and Pathological Variables
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Maternal and Fetal Complications
3.3. Gross Placental Findings
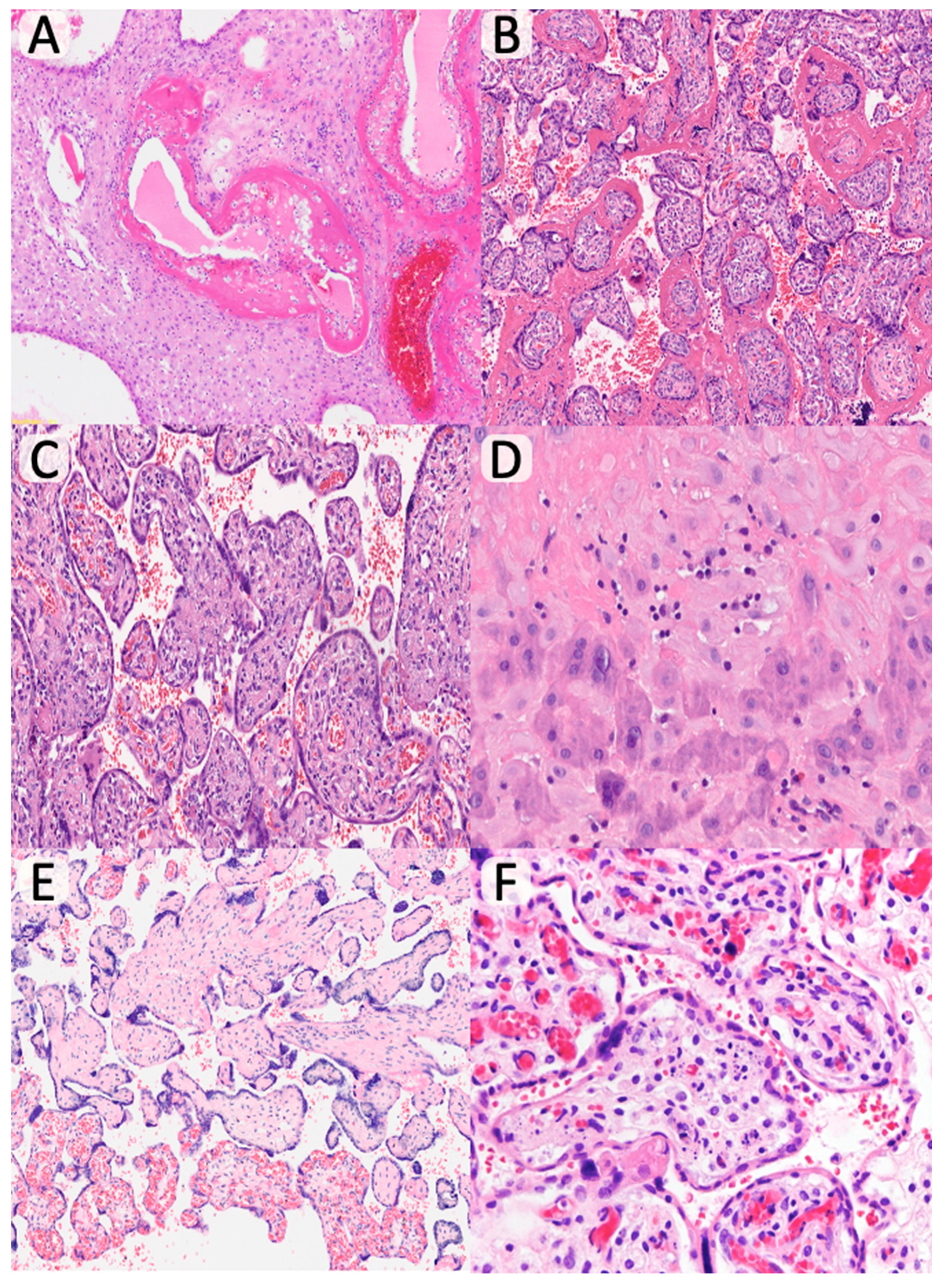
3.4. Histopathological Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murray, S.R.; Norman, J.E. Multiple pregnancies following assisted reproductive technologies—A happy consequence or double trouble? Semin. Fetal Neonatal Med. 2014, 19, 222–227. [Google Scholar] [CrossRef]
- Pena-Burgos, E.M.; Duyos-Mateo, I.; Pozo-Kreilinger, J.J.; Regojo-Zapata, R.M.; Quirós-González, V.; De La Calle, M. Comparison of maternal, fetal, obstetric and neonatal outcomes for 234 triplet pregnancies conceived in vivo versus IVF and ICSI conceptions. Reprod. Biomed. Online 2024, 48, 103419. [Google Scholar] [CrossRef]
- Geipel, A.; Berg, C.; Katalinic, A.; Plath, H.; Hansmann, M.; Germer, U.; Gembruch, U. Prenatal diagnosis and obstetric outcomes in triplet pregnancies in relation to chorionicity. BJOG Int. J. Obstet. Gynaecol. 2005, 112, 554–558. [Google Scholar] [CrossRef]
- Ballabh, P.; Kumari, J.; AlKouatly, H.B.; Yih, M.; Arevalo, R.; Rosenwaks, Z.; Krauss, A.N. Neonatal outcome of triplet versus twin and singleton pregnancies: A matched case control study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2003, 107, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Wen, S.W.; Demissie, K.; Yang, Q.; Walker, M.C. Maternal morbidity and obstetric complications in triplet pregnancies and quadruplet and higher-order multiple pregnancies. Am. J. Obstet. Gynecol. 2004, 191, 254–258. [Google Scholar] [CrossRef]
- Kupka, M.S.; Ferraretti, A.P.; de Mouzon, J.; Castilla, J.A.; Goossens, V.; Strohmer, H.; Obruca; Kreuz-Kinderwunschzentrum, S.P.G.; Bogaerts, K.; Biostat, I.; et al. Assisted reproductive technology in Europe, 2010: Results generated from European registers by ESHRE†. Hum. Reprod. 2014, 29, 2099–2113. [Google Scholar] [CrossRef]
- Martin, J.A.; Hamilton, B.E.; Osterman, M.J.K. Three decades of twin births in the United States, 1980–2009. NCHS Data Brief. 2012, 1–8. [Google Scholar]
- Savasi, V.M.; Mandia, L.; Laoreti, A.; Cetin, I. Maternal and fetal outcomes in oocyte donation pregnancies. Hum. Reprod. Update 2016, 22, 620–633. [Google Scholar] [CrossRef] [PubMed]
- Korb, D.; Schmitz, T.; Seco, A.; Le Ray, C.; Santulli, P.; Goffinet, F.; Deneux-Tharaux, C. Increased risk of severe maternal morbidity in women with twin pregnancies resulting from oocyte donation. Hum. Reprod. 2020, 35, 1922–1932. [Google Scholar] [CrossRef]
- van der Hoorn, M.L.P.; Lashley, E.E.L.O.; Bianchi, D.W.; Claas, F.H.J.; Schonkeren, C.M.C.; Scherjon, S.A. Clinical and immunologic aspects of egg donation pregnancies: A systematic review. Hum. Reprod. Update 2010, 16, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Le Ray, C.; Scherier, S.; Anselem, O.; Marszalek, A.; Tsatsaris, V.; Cabrol, D.; Goffinet, F. Association between oocyte donation and maternal and perinatal outcomes in women aged 43 years or older. Hum. Reprod. 2012, 27, 896–901. [Google Scholar] [CrossRef]
- Masoudian, P.; Nasr, A.; De Nanassy, J.; Fung-Kee-Fung, K.; Bainbridge, S.A.; El Demellawy, D. Oocyte donation pregnancies and the risk of preeclampsia or gestational hypertension: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2016, 214, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Storgaard, M.; Loft, A.; Bergh, C.; Wennerholm, U.; Söderström-Anttila, V.; Romundstad, L.; Aittomaki, K.; Oldereid, N.; Forman, J.; Pinborg, A. Obstetric and neonatal complications in pregnancies conceived after oocyte donation: A systematic review and meta-analysis. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 561–572. [Google Scholar] [CrossRef]
- Modest, A.M.; Smith, L.H.; Toth, T.L.; Collier, A.R.Y.; Hacker, M.R. Multifoetal gestations mediate the effect of in vitro fertilisation (IVF) on ischaemic placental disease in autologous oocyte IVF more than donor oocyte IVF. Paediatr. Perinat. Epidemiol. 2022, 36, 181–189. [Google Scholar] [CrossRef]
- Sekhon, L.H.; Gerber, R.S.; Rebarber, A.; Saltzman, D.H.; Klauser, C.K.; Gupta, S.; Fox, N.S. Effect of oocyte donation on pregnancy outcomes in in vitro fertilization twin gestations. Fertil. Steril. 2014, 101, 1326–1330. [Google Scholar] [CrossRef]
- Mascarenhas, M.; Sunkara, S.K.; Antonisamy, B.; Kamath, M.S. Higher risk of preterm birth and low birth weight following oocyte donation: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 218, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Boria, F.; De La Calle, M.; Cuerva, M.; Sainz, A.; Bartha, J.L. Impact of oocyte donation on obstetric and perinatal complications in twin pregnancies. J. Matern. Fetal Neonatal Med. 2020, 33, 1960–1963. [Google Scholar] [CrossRef]
- Styer, A.K.; Parker, H.J.; Roberts, D.J.; Palmer-Toy, D.; Toth, T.L.; Ecker, J.L. Placental villitis of unclear etiology during ovum donor in vitro fertilization pregnancy. Am. J. Obstet. Gynecol. 2003, 189, 1184–1186. [Google Scholar] [CrossRef]
- Perni, S.C.; Predanik, M.; Cho, J.E.; Baergen, R.N. Placental pathology and pregnancy outcomes in donor and non-donor oocyte in vitro fertilization pregnancies. J. Perinat. Med. 2005, 33, 27–32. [Google Scholar] [CrossRef]
- Kogan, E.A.; Rudenko, E.E.; Demura, T.A.; Zharkov, N.V.; Trifonova, N.S.; Zhukova, E.V.; Aleksandrov, L.S.; Bayanova, S.N. Structural, immunohistochemical and molecular features of placentas and placental sites after in vitro fertilization with donor eggs (surrogate motherhood). Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 238, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Esteves, A.; Rozon, C.; Clancy, J.; Liao, Y.; Wen, S.W.; Fung, K.F.-K.; El Demellawy, D. Abnormal placental pathological findings and adverse clinical outcomes of oocyte donation. Placenta 2020, 101, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Schonkeren, D.; Swings, G.; Roberts, D.; Claas, F.; De Heer, E.; Scherjon, S. Pregnancy Close to the Edge: An Immunosuppressive Infiltrate in the Chorionic Plate of Placentas from Uncomplicated Egg Cell Donation. PLoS ONE 2012, 7, e32347. [Google Scholar] [CrossRef]
- Gundogan, F.; Bianchi, D.W.; Scherjon, S.A.; Roberts, D.J. Placental pathology in egg donor pregnancies. Fertil. Steril. 2010, 93, 397–404. [Google Scholar] [CrossRef]
- Pinar, H.; Stephens, M.; Singer, D.B.; Boyd, T.K.; Pflueger, S.M.; Gang, D.L.; Roberts, D.J.; Sung, C.J. Triplet Placentas: Reference Values for Weights. Pediatr. Dev. Pathol. 2002, 5, 495–498. [Google Scholar] [CrossRef]
- Khong, T.Y.; Mooney, E.E.; Ariel, I.; Balmus, N.C.M.; Boyd, T.K.; Brundler, M.-A.; Derricott, H.; Evans, M.J.; Faye-Petersen, O.M.; Gillan, J.E.; et al. Sampling and Definitions of Placental Lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab. Med. 2016, 140, 698–713. [Google Scholar] [CrossRef]
- Redline, R.W.; Ravishankar, S.; Bagby, C.M.; Saab, S.T.; Zarei, S. Four major patterns of placental injury: A stepwise guide for understanding and implementing the 2016 Amsterdam consensus. Mod. Pathol. 2021, 34, 1074–1092. [Google Scholar] [CrossRef]
- Morency, A.M.; Shah, P.S.; Seaward, P.G.R.; Whittle, W.; Murphy, K.E. Obstetrical and neonatal outcomes of triplet births—Spontaneous versus assisted reproductive technology conception. J. Matern. Fetal Neonatal Med. 2016, 29, 938–943. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.S.; Roman, T.; Viteri, O.A.; Haidar, Z.A.; Ontiveros, A.; Sibai, B.M. The Relationship of Assisted Reproductive Technology on Perinatal Outcomes in Triplet Gestations. Am. J. Perinatol. 2018, 35, 1388–1393. [Google Scholar] [CrossRef]
- Redline, R.W.; Roberts, D.J.; Parast, M.M.; Ernst, L.M.; Morgan, T.K.; Greene, M.F.; Gyamfi-Bannerman, C.; Louis, J.M.; Maltepe, E.; Mestan, K.K.; et al. Placental pathology is necessary to understand common pregnancy complications and achieve an improved taxonomy of obstetrical disease. Am. J. Obstet. Gynecol. 2023, 228, 187–202. [Google Scholar] [CrossRef]
- Downing, M.; Sulo, S.; Parilla, B.V. Perinatal and Neonatal Outcomes of Triplet Gestations Based on Chorionicity. AJP Rep. 2017, 7, e59–e63. [Google Scholar] [CrossRef] [PubMed]
- Glinianaia, S.V.; Rankin, J.; Khalil, A.; Binder, J.; Waring, G.; Curado, J.; Pateisky, P.; Thilaganathan, B.; Sturgiss, S.N.; Hannon, T.; et al. Effect of monochorionicity on perinatal outcome and growth discordance in triplet pregnancy: Collaborative multicenter study in England, 2000–2013. Ultrasound Obstet. Gynecol. 2021, 57, 440–448. [Google Scholar] [CrossRef]
- Claverol, M.B.; Moreno, I.A.; Minaya, M.R.; Muñoz, M.F.; Angullo, Z.R.R.; Navarro, P.G.; García-Honduvilla, N.; Ortega, M.A.; Tizón, S.G.; Pintado-Recarte, M.P.; et al. Maternal, Perinatal and Neonatal Outcomes of Triplet Pregnancies According to Chorionicity: Our 15-Year Experience in a Tertiary-Level Center. J. Clin. Med. 2024, 13, 1793. [Google Scholar] [CrossRef]
- De Paepe, M.; Shapiro, S.; Greco, D.; Luks, V.; Abellar, R.; Luks, C.; Luks, F. Placental markers of twin-to-twin transfusion syndrome in diamniotic–monochorionic twins: A morphometric analysis of deep artery-to-vein anastomoses. Placenta 2010, 31, 269–276. [Google Scholar] [CrossRef]
- Paepe, M.E.D. Examination of the twin placenta. Semin. Perinatol. 2015, 39, 27–35. [Google Scholar] [CrossRef]
- Eliner, O.; Koren, R.R.; Ram, H.S.; Levi, M.; Herzberger, E.H.; Wiser, A.; Miller, N. Perinatal Outcomes of Singleton, Twin and Triplet Gestations after Oocyte Donation: A Retrospective, Population-Based Cohort Analysis. Children 2024, 11, 962. [Google Scholar] [CrossRef] [PubMed]
- Miremerg, H.; Frig, O.; Rona, S.; Herman, H.G.; Mizrachi, Y.; Schreiber, L.; Bar, J.; Kovo, M.; Weiner, E. Is advanced maternal age associated with placental vascular malperfusion? A prospective study from a single tertiary center. Arch. Gynecol. Obstet. 2020, 301, 1441–1447. [Google Scholar] [CrossRef] [PubMed]
- Torous, V.F.; Roberts, D.J. Placentas From Women of Advanced Maternal Age. Arch. Pathol. Lab. Med. 2020, 144, 1254–1261. [Google Scholar] [CrossRef]
- Satpathy, H.K.; Fleming, A.; Frey, D.; Barsoom, M.; Satpathy, C.; Khandalavala, J. Maternal obesity and pregnancy. Postgrad. Med. 2008, 120, E01–E09. [Google Scholar] [CrossRef] [PubMed]
- Herman, H.G.; Volodarsky-Perel, A.; Nu, T.N.T.; Machado-Gedeon, A.; Cui, Y.; Shaul, J.; Dahan, M.H. Diminished ovarian reserve is a risk factor for preeclampsia and placental malperfusion lesions. Fertil. Steril. 2023, 119, 794–801. [Google Scholar] [CrossRef]
- Chisholm, K.M.; Norton, M.E.; Penn, A.A.; Heerema-McKenney, A. Classification of Preterm Birth With Placental Correlates. Pediatr. Dev. Pathol. 2018, 21, 548–560. [Google Scholar] [CrossRef]
- Luo, G.; Redline, R.W. Peripheral Insertion of Umbilical Cord. Pediatr. Dev. Pathol. 2013, 16, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.J.; Liu, P.C.; Hua, J.; Zhao, Y.; Cao, J. Placental weight and size in relation to fetal growth restriction: A case-control study. J. Matern. Fetal Neonatal Med. 2021, 34, 1356–1360. [Google Scholar] [CrossRef] [PubMed]
- Cochrane, E.; Pando, C.; Kirschen, G.W.; Soucier, D.; Fuchs, A.; Garry, D.J. Assisted reproductive technologies (ART) and placental abnormalities. J. Perinat. Med. 2020, 48, 825–828. [Google Scholar] [CrossRef] [PubMed]
- Feldman, D.M.; Borgida, A.F.; Trymbulak, W.P.; Barsoom, M.J.; Sanders, M.M.; Rodis, J.F. Clinical implications of velamentous cord insertion in triplet gestations. Am. J. Obstet. Gynecol. 2002, 186, 809–811. [Google Scholar] [CrossRef]
- Wang, H.; Jacobson, A.; Harmon, D.C.; Choy, E.; Hornicek, F.J.; Raskin, K.A.; Chebib, I.A.; DeLaney, T.F.; Chen, Y.E. Prognostic factors in alveolar soft part sarcoma: A SEER analysis: Alveolar Soft Part Sarcoma. J. Surg. Oncol. 2016, 113, 581–586. [Google Scholar] [CrossRef]
- Redline, R.W.; Ravishankar, S. Fetal vascular malperfusion, an update. APMIS 2018, 126, 561–569. [Google Scholar] [CrossRef]
- Stanek, J. Chorangiosis of Chorionic Villi: What Does It Really Mean? Arch. Pathol. Lab. Med. 2016, 140, 588–593. [Google Scholar] [CrossRef]
- Guschmann, M.; Henrich, W.; Entezami, M.; Dudenhausen, J.W. Chorioangioma—New insights into a well-known problem I. Results of a clinical and morphological study of 136 cases. J. Perinat. Med. 2003, 31, 163–169. [Google Scholar] [CrossRef]
- Grandone, E.; Villani, M.; Tiscia, G.L. Aspirin and heparin in pregnancy. Expert. Opin. Pharmacother. 2015, 16, 1793–1803. [Google Scholar] [CrossRef]
- Sacha, C.R.; Mortimer, R.M.; James, K.; Harris, A.L.; Yeh, J.; Toth, T.L.; Souter, I.; Roberts, D.J. Placental pathology of term singleton live births conceived with fresh embryo transfer compared with those conceived without assisted reproductive technology. Fertil. Steril. 2022, 117, 758–768. [Google Scholar] [CrossRef]
- Wang, H.; Zhu, J.; Li, T. Comparison of perinatal outcomes and pregnancy complications between fresh embryo transfer and frozen embryo transfer in singleton pregnant women. J. Zhejiang Univ. (Med. Sci.) 2023, 52, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Mizrachi, Y.; Weissman, A.; Fater, G.B.; Torem, M.; Horowitz, E.; Schreiber, L.; Raziel, A.; Bar, J.; Kovo, M. Placental histopathology in IVF pregnancies resulting from the transfer of frozen-thawed embryos compared with fresh embryos. J. Assist. Reprod. Genet. 2020, 37, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Weissman, A.; Ulanovsky, I.; Burke, Y.; Makhoul, I.R.; Blazer, S.; Drugan, A. Triplet pregnancies—A three-decade perspective: Do we fare better? Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Pena-Burgos, E.M.; Duyos-Mateo, I.; Pozo-Kreilinger, J.J.; Regojo-Zapata, R.M.; Quirós-González, V.; De la Calle, M. How Have the Baseline Characteristics and Outcomes of Triplet Pregnancies Changed over the Last Two Decades? J. Obstet. Gynaecol. Can. 2024, 47, 102735. [Google Scholar] [CrossRef]
| Variable | Total, n = 77 | Oocyte Donation, n = 29 | Non-Oocyte Donation, n = 48 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
|---|---|---|---|---|---|---|---|---|---|
| Chorionicity | |||||||||
| 3 (3.9) | 1 (3.4) | 2 (4.2) | 1.00 c | 0.82 | 0.07–9.48 | |||
| 37 (48.1) | 15 (51.7) | 22 (45.8) | 0.61 b | 1.26 | 0.50–3.18 | |||
| 37 (48.1) | 13 (44.8) | 24 (50.0) | 0.66 b | 0.81 | 0.32–2.04 | |||
| 40 (51.9) | 16 (55.2) | 24 (51.9) | 0.66 b | 1.23 | 0.48–3.10 | |||
| Maternal age (years) | 35.5 ± 4.1 | 34.7 ± 4.6 | 35.8 ± 3.6 | 0.53 a | - | - | |||
| Pre-pregnancy BMI (kg/m2) | 24.2 ± 2.2 | 24.4 ± 2.0 | 24.1 ± 2.3 | 0.27 a | - | - | |||
| 1 (1.3) | 0 (0) | 1 (3.4) | 0.20 c | - | - | |||
| Year of conception | |||||||||
| 23 (29.9) | 7 (24.1) | 16 (33.3) | 0.39 b | 1.57 | 0.55–4.45 | |||
| 54 (70.1) | 22 (75.9) | 32 (66.7) | ||||||
| Parity | 0.06 c | 0.32 | 0.09–1.07 | ||||||
| 57 (74.0) | 25 (86.2) | 32 (66.7) | ||||||
| 20 (26.0) | 4 (13.8) | 16 (33.3) | ||||||
| Previous failed pregnancy attempts by ART | 28 (47.5) | 16 (64.0) | 12 (42.9) | 0.02 b | 3.25 | 1.10–9-57 | 0.03 | 2.34 | 1.06–8.76 |
| Variable | Total, n = 77 | Oocyte Donation, n = 29 | Non-Oocyte Donation, n = 48 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
|---|---|---|---|---|---|---|---|---|---|
| Maternal complications | |||||||||
| Preeclampsia | 12 (15.6) | 8 (27.6) | 4 (8.3) | 0.02 b | 4.19 | 1.13–15.49 | 0.03 | 5.02 | 2.24–13.42 |
| Pregnancy-induced hypertension | 8 (10.4) | 6 (20.7) | 2 (4.2) | 0.02 c | 6.00 | 1.12–32.08 | 0.03 | 6.32 | 1.76–26.54 |
| Gestational diabetes | 8 (10.4) | 3 (10.3) | 5 (10.4) | 0.99 c | 0.99 | 0.21–4.50 | |||
| Intrahepatic cholestasis | 6 (7.8) | 5 (17.2) | 1 (2.1) | 0.01 c | 9.79 | 1.08–88.60 | 0.12 | 10.41 | 2.13–67.65 |
| Pregnancy-induced hypothyroidism | 6 (7.8) | 2 (6.9) | 4 (8.3) | 0.82 c | 0.81 | 0.14–4.75 | |||
| Iron deficiency anaemia | 15 (19.5) | 6 (20.7) | 9 (18.8) | 0.83 b | 1.13 | 0.35–3.58 | |||
| Fetal complications | |||||||||
| Twin-to-twin transfusion syndrome | 3 (4.1) | 2 (7.1) | 1 (2.2) | 0.29 c | 3.46 | 0.29–40.05 | |||
| Twin anemia-polycythemia sequence | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | - | - | - | ||
| Amniotic fluid discordance | 7 (9.5) | 2 (7.1) | 5 (10.9) | 0.59 c | 0.63 | 0.11–3.49 | |||
| Biometry discordance | 7 (9.5) | 4 (14.3) | 3 (6.5) | 0.26 c | 2.38 | 0.49–11.57 | |||
| Variable | Total, n = 231 | Oocyte donation, n = 77 | Non-oocyte donation, n = 136 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
| Fetal growth restriction | 26 (11.3) | 15 (17.2) | 11 (7.6) | 0.02 b | 2.51 | 1.09–5.77 | 0.04 | 3.32 | 1.21–6.54 |
| Fetal malformations | 3 (1.4) | 2 (2.4) | 1 (0.7) | 0.30 c | 3.34 | 0.29–37.42 | |||
| Fetal death | 24 (10.4) | 18 (20.7) | 6 (4.2) | <0.01 b | 6.00 | 2.27–15.79 | 0.01 | 7.21 | 2.21–16.54 |
| Variable | Total, n = 77 | Oocyte donation, n = 29 | Non-oocyte donation, n = 48 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
| Obstetric complications | |||||||||
| Threatened preterm labor | 17 (23.0) | 5 (17.9) | 12 (26.1) | 0.41 b | 0.61 | 0.19–1.98 | |||
| Premature rupture of membranes | 13 (17.6) | 4 (14.3) | 9 (19.6) | 0.56 c | 0.68 | 0.19–2.47 | |||
| Variable | Total, n = 73 | Oocyte donation, n = 26 | Non-oocyte donation, n = 47 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
| Preterm birth | 33.0 (P25 = 31.0, P75 = 34.0) | 32.5 (P25 = 30.0, P75 = 34.7) | 33.0 (P25 = 31.0, P75 = 34.0) | 0.91 a | - | - | |||
| 45 (61.6) | 17 (60.7) | 28 (62.2) | 0.89 b | 0.93 | 0.35–2.47 | |||
| 31 (42.5) | 13 (46.4) | 18 (40.0) | 0.58 b | 1.30 | 0.50–3.37 | |||
| - Between 32.0–35.6 weeks | 41 (56.2) | 15 (53.6) | 26 (57.8) | 0.72 b | 0.84 | 0.32–2.17 | |||
| 2 (2.7) | 1 (1.4) | 1 (2.2) | 0.73 c | 1.63 | 0.09–27.14 | |||
| Variable | Total, n = 213 | Oocyte donation, n = 77 | Non-oocyte donation, n = 136 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
| Neonatal complications | |||||||||
| Birth weight (g) | 1755 (P25 = 1545, P75 = 1965) | 1670 (P25 = 1526, P75 = 2070) | 1763 (P25 = 1550, P75 = 1943) | 0.52 a | - | - | |||
| 40 (21.1) | 16 (22.5) | 24 (20.2) | 0.69 a | 1.15 | 0.56–2.35 | |||
| 144 (75.8) | 52 (73.2) | 92 (77.3) | 0.52 a | 0.80 | 0.40–1.58 | |||
| 6 (3.2) | 3 (4.2) | 3 (2.5) | 0.34 a | 1.06 | 0.48–2.03 | |||
| Umbilical cord pH | 7.33 (P25 = 7.30, P75 = 7.35) | 7.34 (P25 = 7.31, P75 = 7.36) | 7.32 (P25 = 7.29, P75 = 7.35) | 0.06 a | - | - | |||
| 11 (5.8) | 2 (2.7) | 9 (7.9) | 0.13 c | 0.32 | 0.06–1.52 | |||
| Apgar score 5 min ≤5 | 13 (7.1) | 6 (9.4) | 7 (5.9) | 0.38 b | 1.64 | 0.52–5.10 |
| Variable | Total, n = 77 | Oocyte Donation, n = 29 | Non-Oocyte Donation, n = 48 | Signification (p) | Odds Ratio (OR) | 95% IC | Adjusted p | Adjusted OR | 95% IC |
|---|---|---|---|---|---|---|---|---|---|
| Placental weight (g) | 859.74 ± 252.67 | 828.30 ± 339.45 | 878.28 ± 186.62 | 0.45 b | - | - | |||
| Placental weight | |||||||||
| 13 (17.8) | 7 (25.9) | 6 (13.0) | 0.16 c | 2.33 | 0.69–7.86 | |||
| - 11–50 | 23 (31.5) | 6 (22.2) | 17 (37.0) | 0.19 c | 0.48 | 0.16–1.44 | |||
| - 51–89 | 18 (24.7) | 8 (29.6) | 10 (21.7) | 0.45 c | 1.51 | 0.51–4.47 | |||
| 19 (26.0) | 6 (22.2) | 13 (28.3) | 0.57 c | 0.72 | 0.23–2.20 | |||
| Placental size (cm) | 21.0 (P25 = 17.5, P75 = 28.5) | 21.0 (P25 = 18.0, P75 = 29.0) | 21.0 (P25 = 17.0, P75 = 30.0) | 0.41 a | - | - | |||
| Placental thickness (cm) | 2.1 (P25 = 2.0, P75 = 2.4) | 2.1 (P25 = 2.0, P75 = 2.5) | 2.2 (P25 = 2.0, P75 = 2.3) | 0.65 a | - | - | |||
| Variable | Total, n = 40 | Oocyte donation, n = 16 | Non-oocyte donation, n = 24 | Signification (p) | Odds Ratio (OR) | CI 95% | Adjusted p | Adjusted OR | 95% IC |
| Superficial vascular anastomoses | 9 (42.9) | 3 (50.0) | 6 (40.0) | 0.67 d | 1.50 | 0.22–10.97 | |||
| Variable | Total, n = 231 | Oocyte donation, n = 77 | Non-oocyte donation, n = 136 | Signification (p) | Odds Ratio (OR) | CI 95% | Adjusted p | Adjusted OR | 95% IC |
| Umbilicial cord insertion | |||||||||
| 17 (7.9) | 3 (3.6) | 14 (10.6) | 0.06 d | 0.31 | 0.08–1.13 | |||
| 82 (38.0) | 35 (41.7) | 47 (35.6) | 0.37 c | 1.29 | 0.73–2.26 | |||
| 68 (31.5) | 26 (31.0) | 42 (31.8) | 0.84 c | 0.96 | 0.53–1.73 | |||
| 49 (22.7) | 20 (23.8) | 29 (22.0) | 0.75 c | 1.11 | 0.58–2.12 | |||
| Umbilical cord lenght | 18.0 (P25 = 13.0, P75 = 22.0) | 18.0 (P25 = 13.0, P75 = 22.0) | 18.0 (P25 = 12.0, P75 = 23.0) | 0.97 a | - | - | |||
| Umbilical cord thickness | 1.2 (P25 = 1.0, P75 = 1.4) | 1.2 (P25 = 1.0, P75 = 1.4) | 1.2 (P25 = 1.0, P75 = 1.47) | 0.23 a | - | - | |||
| Umbilical cord coiling | |||||||||
| 9 (6.2) | 5 (9.6) | 4 (4.3) | 0.20 d | 2.36 | 0.60–9.23 | |||
| 121 (83.4) | 44 (84.6) | 77 (82.8) | 0.77 c | 1.14 | 0.45–2.88 | |||
| 15 (10.3) | 3 (5.8) | 12 (12.9) | 0.23 d | 0.41 | 0.11–1.53 | |||
| Single umbilical artery | 10 (5.8) | 4 (6.3) | 6 (5.6) | 0.86 d | 1.12 | 0.30–4.13 | |||
| True umbilical knots | 4 (2.2) | 0 (0.0) | 4 (3.4) | 0.12 d | 0.63 | 0.56–1.02 | |||
| Variable | Total, n = 188 | Oocyte donation, n = 70 | Non-oocyte donation, n = 118 | Signification (p) | Odds Ratio (OR) | CI 95% | Adjusted p | Adjusted OR | 95% IC |
| Membranous alterations | 5 (3.2) | 2 (3.5) | 3 (3.1) | 0.88 d | 1.13 | 0.18–7.03 | |||
| Variable | Total, n = 231 | Oocyte donation, n = 77 | Non-oocyte donation, n = 136 | Signification (p) | Odds Ratio (OR) | CI 95% | Adjusted p | Adjusted OR | 95% IC |
| Intraparenchymatous infarct/hematoma | 36 (16.5) | 20 (23.5) | 16 (12.0) | 0.02 c | 2.25 | 1.09-4.64 | 0.04 | 3.43 | 1.65–7.54 |
| Retroplacental hematoma | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | - | - | |||
| Subchorionic hematoma | 5 (2.5) | 2 (2.6) | 3 (2.5) | 0.94 d | 1.06 | 0.17-6.51 |
| Variable | Total, n = 231 | Oocyte Donation, n = 77 | Non-Oocyte Donation, n = 136 | Signification (p) | Odds Ratio (OR) | IC 95% | Adjusted p | Adjusted OR | IC 95% |
|---|---|---|---|---|---|---|---|---|---|
| Inflammatory pattern findings | |||||||||
| Acute chorioamnionitis | 21 (9.9) | 7 (9.3) | 14 (10.1) | 0.85 a | 0.91 | 0.35–2.36 | |||
| Acute funisitis | 9 (5.2) | 4 (7.0) | 5 (4.3) | 0.44 b | 1.69 | 0.43–6.55 | |||
| Chronic deciduitis | 4 (2.3) | 4 (6.7) | 0 (0) | 0.01 b | 2.33 | 0.27–0.41 | 0.03 | 3.24 | 1.32–8.78 |
| Chronic villitis (UEV) | 15 (8.2) | 10 (15.2) | 5 (4.3) | 0.02 b | 4.00 | 1.30–12.26 | 0.02 | 4.21 | 1.56–10.65 |
| Chronic intervillitis | 3 (1.7) | 3 (5.0) | 0 (0) | 0.03 b | 0.32 | 0.26–0.40 | 0.06 | 0.45 | 0.34–4.34 |
| Vascular pattern findings Maternal vascular malperfusion | |||||||||
| Accelerated villous maturation | 146 (83.9) | 50 (82.0) | 96 (85.0) | 0.69 a | 0.80 | 0.35–1.84 | |||
| Distal villous hypoplasia | 26 (14.9) | 9 (14.8) | 17 (15.0) | 0.95 a | 0.97 | 0.40–2.34 | |||
| Decidual arteriopathy | 6 (3.4) | 3 (4.8) | 3 (2.7) | 0.46 b | 1.83 | 0.35–9.36 | |||
| Fetal vascular malperfusion | |||||||||
| Vascular trombi | 7 (3.9) | 5 (8.1) | 2 (1.7) | 0.03 b | 5.13 | 0.96–27.26 | 0.08 | 6.54 | 2.41–15.57 |
| Avascular villi | 11 (5.9) | 9 (13.6) | 2 (1.7) | <0.01 b | 9.23 | 1.93–44.15 | 0.02 | 7.82 | 2.21–19.09 |
| Stem vessels obliteration | 7 (3.9) | 5 (8.1) | 2 (1.7) | 0.03 b | 5.13 | 0.96–27.26 | 0.06 | 4.42 | 0.21–13.23 |
| Stromal-vascular karyorrhexis | 11 (5.9) | 9 (13.6) | 2 (1.7) | <0.01 b | 9.23 | 1.93–44.15 | 0.01 | 8.65 | 3.01–18.76 |
| Intramural fibrin deposits | 3 (1.3) | 3 (3.6) | 0 (0) | 0.02 b | 0.36 | 0.30–0.42 | 0.10 | 0.42 | 0.08–1.87 |
| Other findings | |||||||||
| Villous edema | 46 (26.9) | 12 (21.1) | 34 (29.8) | 0.22 a | 0.62 | 0.29–1.33 | |||
| Chorangiosis | 115 (66.1) | 35 (61.4) | 80 (68.4) | 0.36 a | 0.73 | 0.38–1.42 | |||
| Chorangioma | 11 (6.4) | 7 (11.9) | 4 (3.5) | 0.03 b | 3.70 | 1.03–13.20 | 0.06 | 4.56 | 0.96–10.45 |
| Dystrophic calcifications | 40 (29.2) | 9 (20.5) | 3 (33.3) | 0.12 b | 0.51 | 0.22–1.20 | |||
| Intervillous fibrin deposits | 84 (38.9) | 37 (50.0) | 64 (33.1) | 0.01 b | 2.02 | 1.13–3.59 | 0.02 | 2.78 | 1.21–6.56 |
| Nucleated red blood cells | 9 (5.0) | 3 (5.0) | 6 (5.0) | 1.00 b | 1.00 | 0.24–4.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pena-Burgos, E.M.; De la Calle, M.; Pozo-Kreilinger, J.J.; García-Díaz, C.; Regojo-Zapata, R.M. Placental Pathological Findings and Clinical Outcomes in Triplet Pregnancies Conceived via Oocyte Donation and Non-Oocyte Donation: A Case–Control Study. Diagnostics 2025, 15, 2681. https://doi.org/10.3390/diagnostics15212681
Pena-Burgos EM, De la Calle M, Pozo-Kreilinger JJ, García-Díaz C, Regojo-Zapata RM. Placental Pathological Findings and Clinical Outcomes in Triplet Pregnancies Conceived via Oocyte Donation and Non-Oocyte Donation: A Case–Control Study. Diagnostics. 2025; 15(21):2681. https://doi.org/10.3390/diagnostics15212681
Chicago/Turabian StylePena-Burgos, Eva Manuela, Maria De la Calle, Jose Juan Pozo-Kreilinger, Cecilia García-Díaz, and Rita María Regojo-Zapata. 2025. "Placental Pathological Findings and Clinical Outcomes in Triplet Pregnancies Conceived via Oocyte Donation and Non-Oocyte Donation: A Case–Control Study" Diagnostics 15, no. 21: 2681. https://doi.org/10.3390/diagnostics15212681
APA StylePena-Burgos, E. M., De la Calle, M., Pozo-Kreilinger, J. J., García-Díaz, C., & Regojo-Zapata, R. M. (2025). Placental Pathological Findings and Clinical Outcomes in Triplet Pregnancies Conceived via Oocyte Donation and Non-Oocyte Donation: A Case–Control Study. Diagnostics, 15(21), 2681. https://doi.org/10.3390/diagnostics15212681





