Identifying Pathogenic Variants in Vietnamese Children with Functional Single Ventricle Based on Whole-Exome Sequencing
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Patients’ Information
2.3. Genetic Analysis
3. Results
3.1. Phenotype of the Patients in the Study
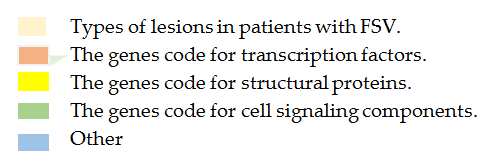
3.2. Genotype of the Patients in the Study
4. Discussion


5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Rao, P.S. Diagnosis and management of cyanotic congenital heart disease: Part II. Indian J. Pediatr. 2009, 76, 297–308. [Google Scholar] [CrossRef]
- Menon, S.C.; Erickson, L.K.; McFadden, M.; Miller, D.V. Effect of ventriculotomy on right-ventricular remodeling in hypoplastic left heart syndrome: A histopathological and echocardiography correlation study. Pediatr. Cardiol. 2013, 34, 354–363. [Google Scholar] [CrossRef]
- Coats, L.; O’Connor, S.; Wren, C.; O’Sullivan, J. The single-ventricle patient population: A current and future concern a population-based study in the North of England. Heart 2014, 100, 1348–1353. [Google Scholar] [CrossRef]
- Kempny, A.; Dimopoulos, K.; Gatzoulis, M.A. Single-ventricle physiology in the UK: An ongoing challenge of growing numbers and of growing complexity of congenital heart disease. Heart 2014, 100, 1315e6. [Google Scholar]
- Ebadi, A.; Spicer, D.E.; Backer, C.L.; Fricker, F.J.; Anderson, R.H. Double-outlet right ventricle revisited. J. Thorac. Cardiovasc. Surg. 2017, 154, 598–604. [Google Scholar]
- Zaidi, S.; Brueckner, M. Genetics and genomics of congenital heart disease. Circ. Res. 2017, 120, 923–940. [Google Scholar] [CrossRef] [PubMed]
- Saliba, A.; Figueiredo, A.C.V.; Baroneza, J.E.; Afiune, J.Y.; Pic-Taylor, A.; de Oliveira, S.F.; Mazzeu, J.F. Genetic and genomics in congenital heart disease: A clinical review. J. Pediatr. 2020, 96, 279–288. [Google Scholar] [CrossRef]
- MacRae, C.A. Mendelian forms of structural cardiovascular disease. Curr. Cardiol. Rep. 2013, 15, 399. [Google Scholar] [CrossRef]
- Pierpont, M.E.; Brueckner, M.; Chung, W.K.; Garg, V.; Lacro, R.V.; McGuire, A.L.; Mital, S.; Priest, J.R.; Pu, W.T.; Roberts, A.; et al. American Heart Association Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Genomic and Precision Medicine. Genetic basis for congenital heart disease: Revisited: A scientific statement from the American Heart Association. Circulation 2018, 138, e653–e711. [Google Scholar]
- Zhu, Y.; Gramolini, A.O.; Walsh, M.A.; Zhou, Y.Q.; Slorach, C.; Friedberg, M.K.; Takeuchi, J.K.; Sun, H.; Henkelman, R.M.; Backx, P.H.; et al. Tbx5-dependent pathway regulating diastolic function in congenital heart disease. Proc. Natl. Acad. Sci. USA 2008, 105, 5519–5524. [Google Scholar] [CrossRef]
- Nakanishi, T.; Markwald, R.R.; Baldwin, H.S.; Keller, B.B.; Srivastava, D.; Yamagishi, H. (Eds.) Etiology and Morphogenesis of Congenital Heart Disease: From Gene Function and Cellular Interaction to Morphology; Springer: Tokyo, Japan, 2016. [Google Scholar] [CrossRef]
- Durbin, M.D.; Cadar, A.G.; Williams, C.H.; Guo, Y.; Bichell, D.P.; Su, Y.R.; Hong, C.C. Hypoplastic left heart syndrome sequencing reveals a novel NOTCH1 mutation in a family with single ventricle defects. Pediatr. Cardiol. 2017, 38, 1232–1240. [Google Scholar] [CrossRef] [PubMed]
- Hinton, R.B.; Martin, L.J.; Rame-Gowda, S.; Tabangin, M.E.; Cripe, L.H.; Benson, D.W. Hypoplastic left heart syndrome links to chromosomes 10q and 6q and is genetically related to bicuspid aortic valve. J. Am. Coll. Cardiol. 2009, 53, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Hitz, M.P.; Lemieux-Perreault, L.P.; Marshall, C.; Feroz-Zada, Y.; Davies, R.; Yang, S.W.; Lionel, A.C.; D’Amours, G.; Lemyre, E.; Cullum, R.; et al. Rare copy number variants contribute to congenital left-sided heart disease. PLoS Genet. 2012, 9, e1002903. [Google Scholar] [CrossRef] [PubMed]
- Iascone, M.; Ciccone, R.; Galletti, L.; Marchetti, D.; Seddio, F.; Lincesso, A.R.; Pezzoli, L.; Vetro, A.; Barachetti, D.; Boni, L.; et al. Identification of de novo mutations and rare variants in hypoplastic left heart syndrome. Clin. Genet. 2012, 81, 542–554. [Google Scholar] [CrossRef]
- Warburton, D.; Ronemus, M.; Kline, J.; Jobanputra, V.; Williams, I.; Anyane-Yeboa, K.; Chung, W.; Yu, L.; Wong, N.; Awad, D.; et al. The contribution of de novo and rare inherited copy number changes to congenital heart disease in an unselected sample of children with conotruncal defects or hypoplastic left heart disease. Hum. Genet. 2014, 133, 11–27. [Google Scholar] [CrossRef]
- Glidewell, S.C.; Miyamoto, S.D.; Grossfeld, P.D.; Clouthier, D.E.; Coldren, C.D.; Stearman, R.S.; Geraci, M.W. Transcriptional impact of rare and private copy number variants in hypoplastic left heart syndrome. Clin. Transl. Sci. 2015, 8, 682–689. [Google Scholar] [CrossRef]
- Sucharov, C.C.; Dockstader, K.; Nunley, K.; McKinsey, T.A.; Bristow, M. Adrenergic receptor stimulation and activation of protein kinase. A protect against 1-adrenergic-mediated phosphorylation of protein kinase D and histone deacetylase 5. J. Card. Fail. 2011, 17, 592–600. [Google Scholar] [CrossRef]
- Qu, X.K.; Qiu, X.B.; Yuan, F.; Wang, J.; Zhao, C.M.; Liu, X.Y.; Zhang, X.L.; Li, R.G.; Xu, Y.J.; Hou, X.M.; et al. A novel NKX2.5 loss-of-function mutation associated with congenital bicuspid aortic valve. Am. J. Cardiol. 2014, 114, 1891–1895. [Google Scholar] [CrossRef]
- Xiang, R.; Fan, L.L.; Huang, H.; Cao, B.B.; Li, X.P.; Peng, D.Q.; Xia, K. A novel mutation of GATA4 (K319E) is responsible for familial atrial septal defect and pulmonary valve stenosis. Gene 2014, 534, 320–323. [Google Scholar] [CrossRef]
- Pan, Y.; Geng, R.; Zhou, N.; Zheng, G.F.; Zhao, H.; Wang, J.; Zhao, C.M.; Qiu, X.B.; Yang, Y.Q.; Liu, X.Y. TBX20 loss-of-function mutation contributes to double outlet right ventricle. Int. J. Mol. Med. 2015, 35, 1058–1066. [Google Scholar] [CrossRef]
- Zheng, J.; Li, F.; Liu, J.; Xu, Z.; Zhang, H.; Fu, Q.; Wang, J.; Sun, K. Investigation of somatic NKX2-5 mutations in Chinese children with congenital heart disease. Int. J. Med. Sci. 2015, 12, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Werner, P.; Latney, B.; Deardorff, M.A.; Goldmuntz, E. MESP1 mutations in patients with congenital heart defects. Hum. Mutat. 2016, 37, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Limongelli, G.; Pacileo, G.; Marino, B.; Digilio, M.C.; Sarkozy, A.; Elliott, P.; Versacci, P.; Calabro, P.; De Zorzi, A.; Di Salvo, G.; et al. Prevalence and clinical significance of cardiovascular abnormalities in patients with the LEOPARD syndrome. Am. J. Cardiol. 2007, 100, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Russell, M.W.; Chung, W.K.; Kaltman, J.R.; Miller, T.A. Advances in the understanding of the genetic determinants of congenital heart disease and their impact on clinical outcomes. J. Am. Heart. Assoc. 2018, 7, e006906. [Google Scholar] [CrossRef]
- Mital, S.; Chung, W.K.; Colan, S.D.; Sleeper, L.A.; Manlhiot, C.; Arrington, C.B.; Cnota, J.F.; Graham, E.M.; Mitchell, M.E.; Goldmuntz, E.; et al. Renin-angiotensin-aldosterone genotype influences ventricular remodeling in infants with single ventricle. Circulation 2011, 123, 2353–2362. [Google Scholar] [CrossRef]
- Burchill, L.J.; Redington, A.N.; Silversides, C.K.; Ross, H.J.; Jimenez-Juan, L.; Mital, S.; Oechslin, E.N.; Dragulescu, A.; Slorach, C.; Mertens, L.; et al. Reninangiotensin-aldosterone system genotype and serum BNP in a contemporary cohort of adults late after Fontan palliation. Int. J. Cardiol. 2015, 197, 209–215. [Google Scholar] [CrossRef]
- Ramroop, R.; Manase, G.; Lu, D.; Manase, D.; Chen, S.; Kim, R.; Lee, T.; Mahle, W.T.; McHugh, K.; Mitchell, M.; et al. Adrenergic receptor genotypes influence postoperative outcomes in infants in the single-ventricle reconstruction trial. J. Thorac. Cardiovasc. Surg. 2017, 154, 1703–1710. [Google Scholar] [CrossRef]
- Rao, P.S. Single ventricle—A comprehensive review. Children 2021, 8, 441. [Google Scholar] [CrossRef]
- Rao, P.S. Moller, J.H., Hoffman, J.I.E., Eds.; Tricuspid atresia. In Pediatric Cardiovascular Medicine, 2nd ed.; Wiley-Blackwell/A John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2012; pp. 487–508. [Google Scholar]
- Rao, P.S. Vijayalakshmi, I.B., Rao, P.S., Chugh, R., Eds.; Tricuspid atresia. In A Comprehensive Approach to Management of Congenital Heart Diseases; Jaypee Publications: New Delhi, India, 2013; pp. 397–413. [Google Scholar]
- d’Udekem, Y.; Xu, M.Y.; Galati, J.C.; Lu, S.; Iyengar, A.J.; Konstantinov, I.E.; Wheaton, G.R.; Ramsay, J.M.; Grigg, L.E.; Millar, J.; et al. Predictors of survival after single-ventricle palliation: The impact of right ventricular dominance. J. Am. Coll. Cardiol. 2012, 59, 1178–1185. [Google Scholar] [CrossRef]
- Alsoufi, B.; Gillespie, S.; Kim, D.; Shashidharan, S.; Kanter, K.; Maher, K.; Kogon, B. Impact of dominant ventricle morphology on palliation outcomes of single ventricle anomalies. Ann. Thorac. Surg. 2016, 102, 593–601. [Google Scholar] [CrossRef]
- Ma, J.; Chen, J.; Tan, T.; Liu, X.; Liufu, R.; Qiu, H.; Zhang, S.; Wen, S.; Zhuang, J.; Yuan, H. Complications and management of functional single ventricle patients with Fontan circulation: From surgeon’s point of view. Front. Cardiovasc. Med. 2022, 9, 917059. [Google Scholar] [CrossRef]
- Balaguru, D.; Rao, P.S. Vijayalakshmi, I.B., Rao, P.S., Chugh, R., Eds.; Mitral atresia (With normal aortic root). In A Comprehensive Approach to Management of Congenital Heart Diseases; Jaypee Publications: New Delhi, India, 2013; pp. 458–467. [Google Scholar]
- Rao, P.S. Rao, P.S., Vidyasagar, D., Eds.; Other cyanotic heart defects in the neonate. In Perinatal Cardiology: A Multidisciplinary Approach; Cardiotext Publishing: Minneapolis, MN, USA, 2015. [Google Scholar]
- Atz, A.M.; Zak, V.; Mahony, L.; Uzark, K.; D’agincourt, N.; Goldberg, D.J.; Williams, R.V.; Breitbart, R.E.; Colan, S.D.; Burns, K.M.; et al. Longitudinal outcomes of patients with single ventricle after the Fontan procedure. J. Am. Coll. Cardiol. 2017, 69, 2735–2744. [Google Scholar] [CrossRef]
- Hinton, R.B., Jr.; Martin, L.J.; Tabangin, M.E.; Mazwi, M.L.; Cripe, L.H.; Benson, D.W. Hypoplastic left heart syndrome is heritable. J. Am. Coll. Cardiol. 2007, 50, 1590–1595. [Google Scholar] [CrossRef]
- Newburger, J.W.; Sleeper, L.A.; Frommelt, P.C.; Pearson, G.D.; Mahle, W.T.; Chen, S.; Dunbar-Masterson, C.; Mital, S.; Williams, I.A.; Ghanayem, N.S.; et al. Pediatric heart network I. Transplantation-free survival and interventions at 3 years in the single ventricle reconstruction trial. Circulation 2014, 129, 2013–2020. [Google Scholar] [CrossRef]
- Alsoufi, B.; Manlhiot, C.; Awan, A.; Alfadley, F.; Al-Ahmadi, M.; Al-Wadei, A.; McCrindle, B.W.; Al-Halees, J. Current outcomes of the Glenn bidirectional cavopulmonary connection for single ventricle palliation. Eur. J. Cardiothorac. Surg. 2012, 42, 42–49. [Google Scholar] [CrossRef]
- Backer, C.L. The functionally univentricular heart: Which is better-right or left ventricle? J. Am. Coll. Cardiol. 2012, 59, 1186–1187. [Google Scholar] [CrossRef]
- Heaton, J.; Heller, D. Single ventricle. [Updated 2021]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557789/ (accessed on 1 September 2025).
- Loffredo, C.A.; Chokkalingam, A.; Sill, A.M.; Boughman, J.A.; Clark, E.B.; Scheel, J.; Brenner, J.I. Prevalence of congenital cardiovascular malformations among relatives of infants with hypoplastic left heart, coarctation of the aorta, and d-transposition of the great arteries. Am. J. Med. Genet. A 2004, 124A, 225–230. [Google Scholar] [CrossRef]
- Homsy, J.; Zaidi, S.; Shen, Y.; Ware, J.S.; Samocha, K.E.; Karczewski, K.J.; DePalma, S.R.; McKean, D.; Wakimoto, H.; Gorham, J.; et al. De novo mutations in congenital heart disease with neurodevelopmental and other congenital anomalies. Science 2015, 350, 1262–1266. [Google Scholar] [CrossRef]
- Yasuhara, J.; Garg, V. Genetics of congenital heart disease: A narrative review of recent advances and clinical implications. Transl. Pediatr. 2021, 10, 2366–2386. [Google Scholar] [CrossRef]
- Williams, K.; Carson, J.; Lo, C. Genetics of congenital heart disease. Biomolecules 2019, 9, 879. [Google Scholar] [CrossRef]
- Chhatwal, K.; Smith, J.J.; Bola, H.; Zahid, A.; Venkatakrishnan, A.; Brand, T. Uncovering the genetic basis of congenital heart disease: Recent advancements and implications for clinical management. CJC Pediatr. Congenit. Heart Dis. 2023, 2, 464–480. [Google Scholar] [CrossRef]
- Kobylinska, J.; Dworzanski, W.; Cendrowska-Pinkosz, M.; Dworzańska, A.; Hermanowicz-Dryka, T.; Kiszka, L.; Starosławska, E.; Burdan, F. Morphological and molecular bases of cardiac development. Postep. Hig. Med. Dosw. 2013, 67, 950–957. [Google Scholar] [CrossRef]
- Morán-Barroso, V.F.; Cervantes, A.; García-Cavazos, R.J.; Queipo, G.; Briones-Garduño, J.C.; Coronel-Cruz, F.; Durán-Ruíz, E.R.; Firó-Reyes, V.; López-Noria, O.F.; Ochoa-Pérez, V.; et al. Genetic aspects in the medical approach of congenital heart defects. Rev. Med. Hosp. Gen. Mex. 2020, 83, 75–87. [Google Scholar] [CrossRef]
- Anfinson, M.; Fitts, R.H.; Lough, J.W.; James, J.M.; Simpson, P.M.; Handler, S.S.; Mitchell, M.E.; Tomita-Mitchell, A. Significance of α-Myosin heavy chain (MYH6) variants in hypoplastic left heart syndrome and related cardiovascular diseases. J. Cardiovasc. Dev. Dis. 2022, 9, 144. [Google Scholar] [CrossRef]
- Sleiman, A.K.; Sadder, L.; Nemer, G. Human genetics of tricuspid atresia and univentricular heart. Adv. Exp. Med. Biol. 2024, 1441, 875–884. [Google Scholar]
- Chen, S.; Jin, Q.; Hou, S.; Li, M.; Zhang, Y.; Guan, L.; Pan, W.; Ge, J.; Zhou, D. Identification of recurrent variants implicated in disease in bicuspid aortic valve patients through whole-exome sequencing. Hum. Genom. 2022, 16, 36. [Google Scholar] [CrossRef]
- Xu, J.; Wu, Q.; Wang, L.; Han, J.; Pei, Y.; Zhi, W.; Liu, Y.; Yin, C.; Jiang, Y. Next-generation sequencing identified genetic variations in families with fetal non-syndromic atrioventricular septal defects. Int. J. Clin. Exp. Pathol. 2018, 11, 3732–3743. [Google Scholar] [PubMed]
- Burnicka-Turek, O.; Steimle, J.D.; Huang, W.; Felker, L.; Kamp, A.; Kweon, J.; Peterson, M.; Reeves, R.H.; Maslen, C.L.; Gruber, P.J.; et al. Cilia gene mutations cause atrioventricular septal defects by multiple mechanisms. Hum. Mol. Genet. 2016, 25, 3011–3028. [Google Scholar] [CrossRef]
- Priest, J.R.; Osoegawa, K.; Mohammed, N.; Nanda, V.; Kundu, R.; Schultz, K.; Lammer, E.J.; Girirajan, S.; Scheetz, T.; Waggott, D.; et al. De novo and rare variants at multiple loci support the oligogenic origins of atrioventricular septal heart defects. PLoS Genet. 2016, 12, e1005963. [Google Scholar] [CrossRef]
- Liu, L.; Wang, H.D.; Cui, C.Y.; Qin, Y.Y.; Fan, T.B.; Peng, B.T.; Zhang, L.Z.; Wang, C.Z. Whole exome sequencing identifies novel mutation in eight Chinese children with isolated tetralogy of Fallot. Oncotarget 2017, 8, 106976–106988. [Google Scholar] [CrossRef]
- Datta, S.; Cao, W.; Skillman, M.; Wu, M. Hypoplastic left heart syndrome: Signaling & molecular perspectives, and the road ahead. Int. J. Mol. Sci. 2023, 24, 15249. [Google Scholar] [CrossRef]
- Theis, J.L.; Hu, J.J.; Sundsbak, R.S.; Evans, J.M.; Bamlet, W.R.; Qureshi, M.Y.; O’Leary, P.W.; Olson, T.M. Genetic association between hypoplastic left heart syndrome and cardiomyopathies. Circ. Genom. Precis. Med. 2021, 14, e003126. [Google Scholar] [CrossRef]
- Helle, E.; Pihkala, J.; Turunen, R.; Ruotsalainen, H.; Tuupanen, S.; Koskenvuo, J.; Ojala, T. Rare variants in genes associated with cardiomyopathy are not common in hypoplastic left heart syndrome patients with myocardial dysfunction. Front. Pediatr. 2020, 8, 596840. [Google Scholar] [CrossRef]
- Polyakova, E.; van Gils, J.M.J.; Stöger, L.; Kiès, P.; Egorova, A.D.; Koopmann, T.T.; van Dijk, T.; DeRuiter, M.C.; Barge-Schaapveld, D.Q.C.M.; Jongbloed, M.R.M. New genetic variant in the MYH7 gene associated with hypoplastic right heart syndrome and hypertrophic cardiomyopathy in the same family. Circ. Genom. Precis. Med. 2023, 16, e004184. [Google Scholar] [CrossRef]
- Nappi, F. In-depth genomic analysis: The new challenge in congenital heart disease. Int. J. Mol. Sci. 2024, 25, 1734. [Google Scholar] [CrossRef]
- Rakhmanov, Y.; Maltese, P.E.; Zulian, A.; Beccari, T.; Dundar, M.; Bertelli, M. Genetic testing for atrial septal defect. EuroBiotech J. 2018, 2, 45–47. [Google Scholar] [CrossRef]
- Zhao, J.Y.; Yang, X.Y.; Shi, K.H.; Sun, S.N.; Hou, J.; Ye, Z.Z.; Wang, J.; Duan, W.Y.; Qiao, B.; Chen, Y.J.; et al. A functional variant in the cystathionine β-synthase gene promoter significantly reduces congenital heart disease susceptibility in a Han Chinese population. Cell Res. 2013, 23, 242–253. [Google Scholar] [CrossRef]
- Wu, Y.; Jin, X.; Zhang, Y.; Zheng, J.; Yang, R. Genetic and epigenetic mechanisms in the development of congenital heart diseases. World J. Ped. Surg. 2021, 4, e000196. [Google Scholar] [CrossRef]
- Zweier, C.; Sticht, H.; Aydin-Yaylagül, I.; Campbell, C.E.; Rauch, A. Human TBX1 missense mutations cause gain of function resulting in the same phenotype as 22q11.2 deletions. Am. J. Hum. Genet. 2007, 80, 510–517. [Google Scholar] [CrossRef]
- Ye, J.; Niu, J.Y.; Peng, Y.; Huang, J.; Wang, H.; Fu, Q.; Li, F.; Xu, R.; Chen, S.; Xu, Y.; et al. Analysis of pathogenic variants in 605 Chinese children with non-syndromic cardiac conotruncal defects based on targeted sequencing. Genomics 2023, 115, 110676. [Google Scholar] [CrossRef]
- Li, B.; Li, T.; Pu, T.; Liu, C.; Chen, S.; Sun, K.; Xu, R. Genetic and functional analyses detect one pathological NFATC1 mutation in a Chinese tricuspid atresia family. Mol. Genet. Genom. Med. 2021, 9, e1771. [Google Scholar] [CrossRef]
- D’Amato, G.; Luxan, G.; de la Pompa, J.L. Notch signalling in ventricular chamber development and cardiomyopathy. FEBS J. 2016, 283, 4223–4237. [Google Scholar] [CrossRef]
- Jin, S.C.; Homsy, J.; Zaidi, S.; Lu, Q.; Morton, S.; DePalma, S.R.; Zeng, X.; Qi, H.; Chang, J.; Sierant, M.C.; et al. Contribution of rare inherited and de novo variants in 2,871 congenital heart disease probands. Nat. Genet. 2017, 49, 1593–1601. [Google Scholar] [CrossRef]
- Tomita-Mitchell, A.; Stamm, K.D.; Mahnke, D.K.; Kim, M.S.; Hidestrand, P.M.; Liang, H.L.; Goetsch, M.A.; Hidestrand, M.; Simpson, P.; Pelech, A.N.; et al. Impact of MYH6 variants in hypoplastic left heart syndrome. Physiol. Genom. 2016, 48, 912–921. [Google Scholar] [CrossRef]
- Giusti, B.; Sticchi, E.; De Cario, R.; Magi, A.; Nistri, S.; Pepe, G. Genetic bases of bicuspid aortic valve: The contribution of traditional and high-throughput sequencing approaches on research and diagnosis. Front. Physiol. 2017, 8, 612. [Google Scholar]
- Sticchi, E.; De Cario, R.; Magi, A.; Giglio, S.; Provenzano, A.; Nistri, S.; Pepe, G.; Giusti, B. Bicuspid aortic valve: Role of multiple gene variants in influencing the clinical phenotype. BioMed Res. Int. 2018, 8386123. [Google Scholar]
- Liu, X.; Chen, W.; Li, W.; Priest, J.R.; Fu, Y.; Pang, K.; Ma, B.; Han, B.; Liu, X.; Hu, S.; et al. Exome-based case-control analysis highlights the pathogenic role of ciliary genes in transposition of the great arteries. Circ. Res. 2020, 126, 811–821. [Google Scholar]
- Li, Y.; Yagi, H.; Onuoha, E.O.; Damerla, R.R.; Francis, R.; Furutani, Y.; Tariq, M.; King, S.M.; Hendricks, G.; Cui, C.; et al. DNAH6 and its interactions with PCD genes in Heterotaxy and primary ciliary dyskinesia. PLoS Genet. 2016, 12. [Google Scholar]
- Faivre, L.; Collod-Beroud, G.; Loeys, B.L.; Child, A.; Binquet, C.; Gautier, E.; Callewaert, B.; Arbustini, E.; Mayer, K.; Arslan-Kirchner, M.; et al. Effect of mutation type and location on clinical outcome in 1,013 probands with Marfan syndrome or related phenotypes and FBN1 mutations: An international study. Am. J. Hum. Genet. 2007, 81, 454–466. [Google Scholar]
- Zhang, J.; Wu, Q.; Wang, L.; Li, X.; Ma, Y.; Yao, L. Association of GDF1 rs4808863 with fetal congenital heart defects: A case–control study. BMJ Open 2015, 5, e009352. [Google Scholar]
- Odelin, G.; Faucherre, A.; Marchese, D.; Pinard, A.; Jaouadi, H.; Le Scouarnec, S.; Consortium, F.G.R.; Chiarelli, R.; Achouri, Y.; Faure, M.; et al. Variations in the poly-histidine repeat motif of HOXA1 contribute to bicuspid aortic valve in mouse and zebrafish. Nat. Commun. 2023, 14, 1543. [Google Scholar]
- Wang, J.; Luo, J.; Chen, Q.; Wang, X.; He, J.; Zhang, W.; Yin, Z.; Zheng, F.; Pan, H.; Li, T.; et al. Identification of LBX2 as a novel causal gene of atrial septal defect. Int. J. Cardiol. 2018, 265, 188–194. [Google Scholar]
- Zaidi, S.; Choi, M.; Wakimoto, H.; Ma, L.; Jiang, J.; Overton, J.D.; Romano-Adesman, A.; Bjornson, R.D.; Breitbart, R.E.; Brown, K.K.; et al. De novo mutations in histone-modifying genes in congenital heart disease. Nature 2013, 498, 220–223. [Google Scholar]
- Zhang, M.; Li, F.X.; Liu, X.Y.; Huang, R.T.; Xue, S.; Yang, X.X.; Li, Y.J.; Liu, H.; Shi, H.Y.; Pan, X.; et al. MESP1 loss-of-function mutation contributes to double outlet right ventricle. Mol. Med. Rep. 2017, 16, 2747–2754. [Google Scholar]
- Chahal, G.; Tyagi, S.; Ramialison, M. Navigating the non-coding genome in heart development and congenital heart disease. Differentiation 2019, 107, 11–23. [Google Scholar]
- Zhao, X.; Hou, C.; Xiao, T.; Xie, L.; Li, Y.; Jia, J.; Zheng, J.; Zhang, Y.; Xu, M. An interesting Mybpc3 heterozygous mutation associated with bicuspid aortic valve. Transl. Pediatr. 2020, 9, 610–618. [Google Scholar]
- Auxerre-Plantié, E.; Nielsen, T.; Grunert, M.; Olejniczak, O.; Perrot, A.; Özcelik, C.; Harries, D.; Matinmehr, F.; Remedios, C.D.; Mühlfeld, C.; et al. Identification of MYOM2 as a candidate gene in hypertrophic cardiomyopathy and Tetralogy of Fallot, and its functional evaluation in the Drosophila heart. Dis. Model. Mech. 2020, 13, dmm045377. [Google Scholar]
- D’Alessandro, L.C.A.; Al Turki, S.; Manickaraj, A.K.; Manase, D.; Mulder, B.J.M.; Bergin, L.; Rosenberg, H.C.; Mondal, T.; Gordon, E.; Lougheed, J.; et al. Exome sequencing identifies rare variants in multiple genes in atrioventricular septal defect. Genet. Med. 2016, 18, 189–198. [Google Scholar]
- Zhang, Z.; Xu, K.; Ji, L.; Zhang, H.; Yin, J.; Zhou, M.; Wang, C.; Yang, S. A novel loss-of-function mutation in NRAP is associated with left ventricular non-compaction cardiomyopathy. Front. Cardiovasc. Med. 2023, 10, 1097957. [Google Scholar]
- Puteri, M.U.; Azmi, N.U.; Kato, M.; Saputri, F.C. PCSK9 promotes cardiovascular diseases: Recent evidence about its association with platelet activation-induced myocardial infarction. Life 2022, 12. [Google Scholar]
- Tariq, M.; Belmont, J.W.; Lalani, S.; Smolarek, T.; Ware, S.M. SHROOM3 is a novel candidate for heterotaxy identified by whole exome sequencing. Genome Biol. 2011, 12, R91. [Google Scholar]
- Ma, L.; Li, J.; Liu, Y.; Pang, S.; Huang, W.; Yan, B. Novel and functional variants within the TBX18 gene promoter in ventricular septal defects. Mol. Cell. Biochem. 2013, 382, 121–126. [Google Scholar]


| Group 1. Tricuspid atresia, atrial septal defects, ventricular septal defect | ||||||||
| ID | Sex/Age (y) | Hypoplastic Right Ventricular | Pulmonary Valve Stenosis/Pulmonary Stenosis | RVOTO | DORV | Transposition of the Great Arteries | Patent Ductus Arteriosus | |
| P1 | F/1 | x | x | x | ||||
| P2 | M/6 | x | x | x | x | |||
| P3 | M/15 | x | x | x | ||||
| P4 | M/8 | x | x | x | ||||
| P5 | F/6 | x | x | |||||
| P6 | M/7 | x | x | |||||
| P7 | M/7 | x | x | |||||
| P8 | M/1 | x | x | x | ||||
| P9 | M/6 | x | x | x | ||||
| Group 2. Mitral valve atresia, hypoplastic left ventricular, DORV | ||||||||
| ID | Sex/Age (y) | VSD | ASD | Transposition of the Great Arteries | Atrioventricular Discordance | Patent Ductus Arteriosus | ||
| P10 | M/1 | x | x | x | x | |||
| P11 | F/6 | x | ||||||
| P12 | M/1 | x | x | x | ||||
| Group 3. Double outlet right ventricle, CAVSD, pulmonary valve stenosis | ||||||||
| ID | Sex/Age (y) | Single Atrium | Single Ventricle | Transposition of the Great Arteries | ASD/VSD | Aortic Valve Stenosis/Aortic Arch Hypoplasia | ||
| P13 | F/1 | x | x | x | ||||
| P14 | M/8 | x | ||||||
| P15 | M/3 | TAPVC | x | x | x | |||
| P16 | M/5 | x | x | |||||
| P17 | F/1 | x | x | x | ||||
| P18 | F/5 | x | x | |||||
| P19 | M/1 | x | x | x/x | ||||
| P20 | M/1 | TAPVC | x | |||||
| P21 | F/5 | x | x | VSD | ||||
| P22 | M/15 | x | x | x | ||||
| P23 | M/5 | x | ||||||
| P24 | M/4 | x | x | x | x | |||
| Group 4. Hypoplastic left heart syndrome | ||||||||
| ID | Sex/Age (y) | Aortic Valve Stenosis | Aortic Arch Hypoplasia | BAV | ASD | VSD | Patent Ductus Arteriosus | |
| P25 | M/1 | x | x | x | ||||
| P26 | M/1 | x | x | x | x | x | x | |
| P27 | M/1 | x | x | x | x | |||
| P28 | M/1 | x | x | x | x | x | ||
| P29 | F/1 | x | x | x | ||||
| Group 1. Tricuspid atresia, atrial septal defects, ventricular septal defect | |||||
| ID/Gene | HGVS.c | HGVS.p | ID/Gene | HGVS.c | HGVS.p |
| P1 | P5 | ||||
| BMP2 | c.482T>C rs34183594 | p.Leu161Ser | ZFPM2 | c.2107A>C rs121908603 | p.Met703Leu |
| EOGT | c.620+27C>T rs181373917 | MESP1 | c.156_157insCCGAGCCCCGT novel | p.Ala53fs | |
| P2 | PCSK9 | c.1026A>G rs509504 | p.Gln342Gln | ||
| TTN | c.103772G>A novel | p.Arg34591Gln | P6 | ||
| c.9749T>G rs55634230 | p.Val3250Gly | NOTCH3 | c.4762A>C novel | p.Asn1588His | |
| EVC | c.1727G>A rs1383180 | p.Arg576Gln | EP300 | c.6998C>T rs750944383 | p.Pro2333Leu |
| NOTCH1 | c.2864G>A rs557049479 | p.Arg955His | COL6A1 | c.2662C>T rs368307185 | p.Arg888Trp |
| MESP1 | c.359T>C rs565846523 | p.Leu120Pro | BMP2 | c.393A>T rs140417301 | p.Arg131Ser |
| SEMA3C | c.1009G>A rs1527482 | p.Val337Met | P7 | ||
| P3 | MYH6 | c.5410C>A rs144571463 | p.Gln1804Lys | ||
| EOGT | c.1399A>T novel | p.Thr467Ser | FBN1 | c.1676C>T rs141551765 | p.Ala559Val |
| DOCK6 | c.6014G>A novel | p.Arg2005His | COL6A2 | c.185C>T novel | p.Pro62Leu |
| COL6A2 | c.3004T>C rs527236952 | p.Tyr1002His | P8 | ||
| MYH11 | c.5110G>A rs538145374 | p.Ala1704Thr | DNAH11 | c.4306C>T rs183489539 | p.Arg1436Trp |
| EVC2 | c.2739G>C rs180747811 | p.Lys913Asn | MYH6 | c.5410C>A rs144571463 | p.Gln1804Lys |
| NFATC1 | c.524G>C rs538981258 | p.Ser175Thr | P9 | ||
| P4 | TTN | c.34216C>A rs532102837 | p.Pro11406Thr | ||
| MYH6 | c.5410C>A rs144571463 | p.Gln1804Lys | SHROOM3 | c.2905C>T rs3733245 | p.Arg969Trp |
| SEMA3C | c.1009G>A rs1527482 | p.Val337Met | c.740A>G rs760622199 | p.Asp247Gly | |
| Group 2. Mitral valve atresia, hypoplastic left ventricular, double outlet right ventricle | |||||
| ID/Gene | HGVS.c | HGVS.p | ID/Gene | HGVS.c | HGVS.p |
| P10 | P12 | ||||
| PCDHB4 | c.599A>G novel | p.Asp200Gly | TTN | c.73568C>A rs753557799 | p.Pro24523Gln |
| NOTCH1 | c.1699A>G rs369067940 | p.Ile567Val | CREBBP | c.4490A>C novel | p.Lys1497Thr |
| P11 | c.4485G>C | p.Lys1495Asn | |||
| TTN | c.77836G>A novel | p.Ala25946Thr | novel | ||
| EP300 | c.2971G>C novel | p.Asp991His | |||
| MYH7 | c.1322C>T rs121913653 | p.Thr441Met | |||
| Group 3. Double outlet right ventricle, complete atrioventricular septal defect, pulmonary valve stenosis | |||||
| ID/Gene | HGVS.c | HGVS.p | ID/Gene | HGVS.c | HGVS.p |
| LRP2 | c.233G>C rs546882372 | p.Gly78Ala | TTN | c.97733A>T novel | p.Asn32578Ile |
| NRAP | c.724C>T rs776357401 | p.Pro242Ser | DNAH11 | c.4306C>T rs183489539 | p.Arg1436Trp |
| AXIN1 | c.1265G>A rs1187305370 | p.Gly422Asp | NOTCH1 | c.7645C>T rs200893930 | p.Arg2549Cys |
| AXIN2 | c.1878T>A rs767756290 | p.Ser626Arg | P20 | ||
| P14 | MESP2 | c.306C>A rs77473319 | p.His102Gln | ||
| FOXC1 | c.1347_1348insAGC novel | p.Gly449_Gly450insSer | GATA4 | c.790G>A rs201520087 | p.Ala264Thr |
| ZFPM2 | c.2095C>T novel | p.His699Tyr | DNAH6 | c.4218T>G rs1398626964 | p.Phe1406Leu |
| P15 | COL11A1 | c.2227C>A novel | p.Pro743Thr | ||
| TTN | c.92336G>C novel | p.Arg30779Thr | P21 | ||
| c.46847C>T rs368057764 | p.Thr15616Met | SHROOM3 | c.440T>A rs3821979 | p.Leu147His | |
| NFATC1 | c.2251T>G rs754093 | p.Cys751Gly | DNAH6 | c.4615C>G rs571512486 | p.Gln1539Glu |
| NRAP | c.4696C>T rs1885434 | p.Arg1566Cys | P22 | ||
| SEMA3C | c.1009G>A rs1527482 | p.Val337Met | TBX18 | c.244_255dupACGTCTGGGCCG | p.Pro85_Ala86insThrSerGlyPro |
| P16 | HOXA1 | c.215_223delATCGCCACC rs544314279 | p.His72_His74del | ||
| EVC | c.1727G>A rs1383180 | p.Arg576Gln | TTN | c.105876G>A rs372521529 | p.Leu35292Leu |
| GDF1 | c.985C>T novel | p.Pro329Ser | COL3A1 | c.3061C>A rs139619440 | p.Leu1021Ile |
| MYBPC3 | c.2504G>T rs527305885 | p.Arg835Leu | LRP2 | c.6130G>A rs142266106 | p.Ala2044Thr |
| P17 | P23 | ||||
| TBX1 | c.928G>A rs41298838 | p.Gly310Ser | NKX2-6 | c.368G>A rs568127693 | p.Arg123His |
| MYH7 | c.1322C>T rs121913653 | p.Thr441Met | MYH11 | c.5550G>A rs146024732 | p.Ser1850Ser |
| P18 | NRAP | c.4439A>G rs368150420 | p.Tyr1480Cys | ||
| TBX20 | c.785C>T novel | p.Thr262Met | NIPBL | c.7489G>T rs759115050 | p.Val2497Phe |
| SRCAP | c.6397G>A novel | p.Val2133Ile | SHROOM3 | c.2888C>T rs367782393 | p.Ser963Leu |
| MYH6 | c.5410C>A rs144571463 | p.Gln1804Lys | P24 | ||
| LBX2 | c.548C>G rs199798817 | p.Pro183Arg | GATA5 | c.374A>T novel | p.Gln125Leu |
| MYOM2 | c.656C>T rs34823600 | p.Ala219Val | NIPBL | c.3049A>C rs146714879 | p.Ile1017Leu |
| SHROOM3 | c.2905C>T rs3733245 | p.Arg969Trp | |||
| Group 4. Hypoplastic left heart syndrome | |||||
| ID/Gene | HGVS.c | HGVS.p | ID/Gene | HGVS.c | HGVS.p |
| P25 | P28 | ||||
| TTN | c.78855T>C rs139953862 | p.Asp26285Asp | MYBPC3 | c.1286C>T rs370412052 | p.Ala429Val |
| NOTCH1 | c.4864C>T rs747447584 | p.Arg1622Cys | TTN | c.75137A>C rs759445513 | p.Lys25046Thr |
| P26 | MYH6 | c.1262T>C novel | p.Val421Ala | ||
| MYH6 | c.5410C>A rs144571463 | p.Gln1804Lys | P29 | ||
| CBS | c.598C>T novel | p.Pro200Ser | TTN | c.10840G>T rs540059730 | p.Glu3614* |
| P27 | MYH6 | c.428G>A | p.Arg143Gln | ||
| TTN | c.105642C>A rs560557634 | p.Phe35214Leu | rs200377640 | ||
| MYH7 | c.2183C>T rs121913644 | p.Ala728Val | |||
| SRCAP | c.278A>G rs555507140 | p.His93Arg | |||
| KDR | c.2524C>T rs41469552 | p.Arg842Cys | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, L.T.; Lien, N.T.K.; Tung, N.V.; Van, D.T.H.; Nga, V.Q.; Tho, N.T.; Hien, N.T.; Duc, N.M.; Hoang, N.H. Identifying Pathogenic Variants in Vietnamese Children with Functional Single Ventricle Based on Whole-Exome Sequencing. Diagnostics 2025, 15, 2627. https://doi.org/10.3390/diagnostics15202627
Tu LT, Lien NTK, Tung NV, Van DTH, Nga VQ, Tho NT, Hien NT, Duc NM, Hoang NH. Identifying Pathogenic Variants in Vietnamese Children with Functional Single Ventricle Based on Whole-Exome Sequencing. Diagnostics. 2025; 15(20):2627. https://doi.org/10.3390/diagnostics15202627
Chicago/Turabian StyleTu, Le Trong, Nguyen Thi Kim Lien, Nguyen Van Tung, Dang Thi Hai Van, Vu Quynh Nga, Nguyen Tat Tho, Nguyen Thanh Hien, Nguyen Minh Duc, and Nguyen Huy Hoang. 2025. "Identifying Pathogenic Variants in Vietnamese Children with Functional Single Ventricle Based on Whole-Exome Sequencing" Diagnostics 15, no. 20: 2627. https://doi.org/10.3390/diagnostics15202627
APA StyleTu, L. T., Lien, N. T. K., Tung, N. V., Van, D. T. H., Nga, V. Q., Tho, N. T., Hien, N. T., Duc, N. M., & Hoang, N. H. (2025). Identifying Pathogenic Variants in Vietnamese Children with Functional Single Ventricle Based on Whole-Exome Sequencing. Diagnostics, 15(20), 2627. https://doi.org/10.3390/diagnostics15202627






