Diagnostic Pitfalls of Prosthetic Valve Endocarditis: From Sacroiliitis to Coronary Septic Embolization
Abstract
1. Introduction
2. Methods
3. Case Report
3.1. Medical History
3.2. Clinical Case



4. Discussion
4.1. Atypical Presentation and Diagnostic Delay
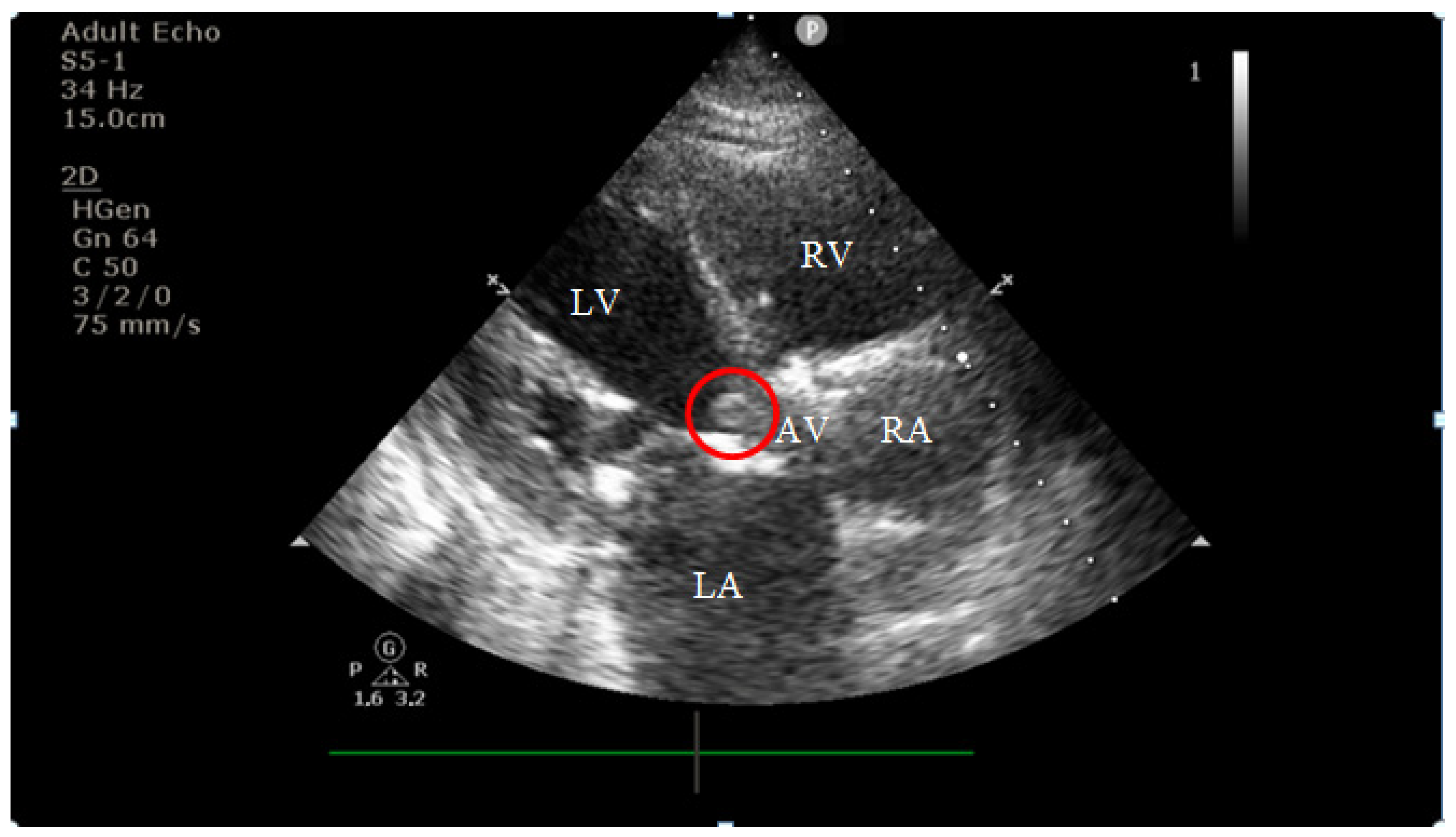
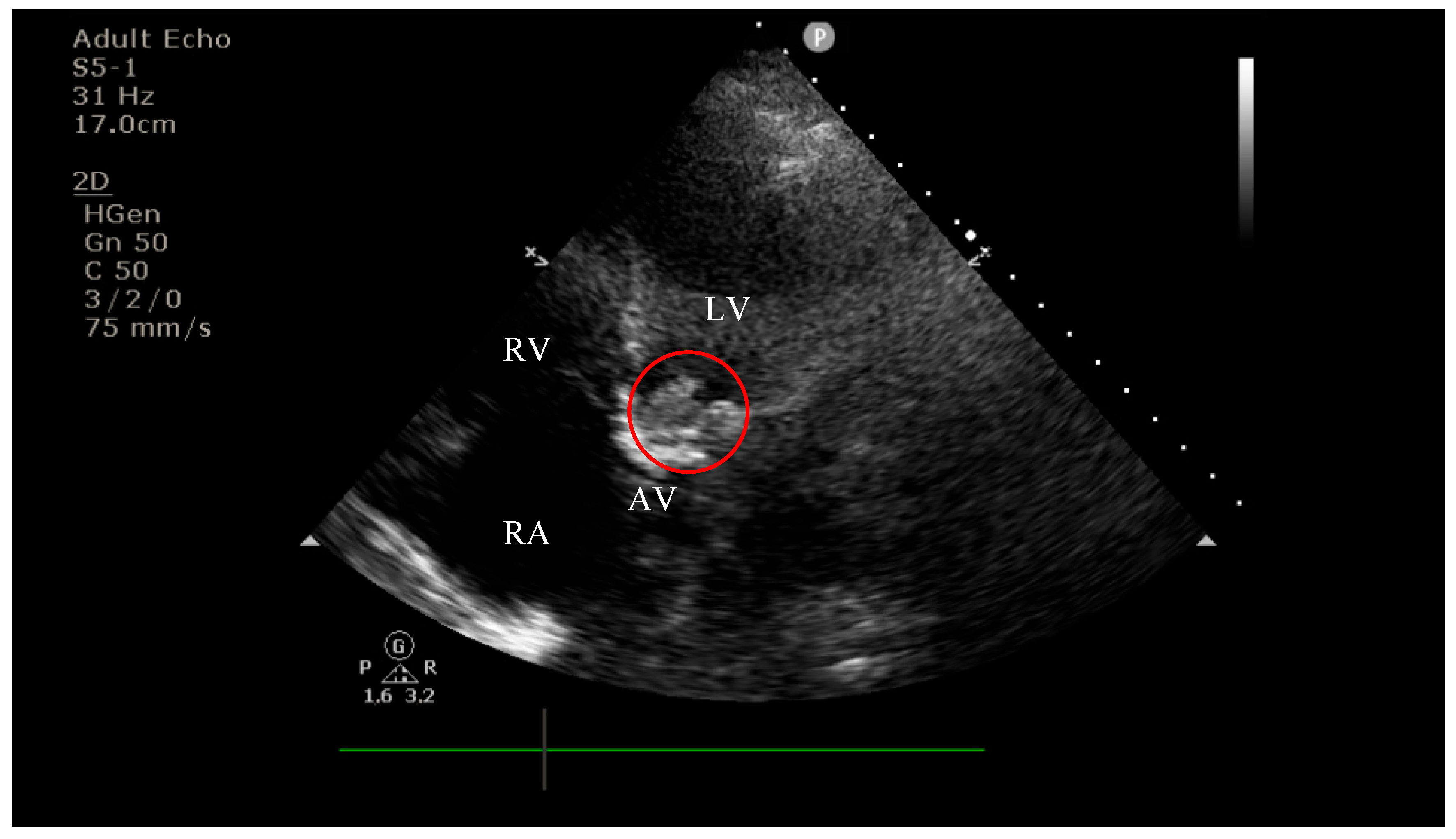
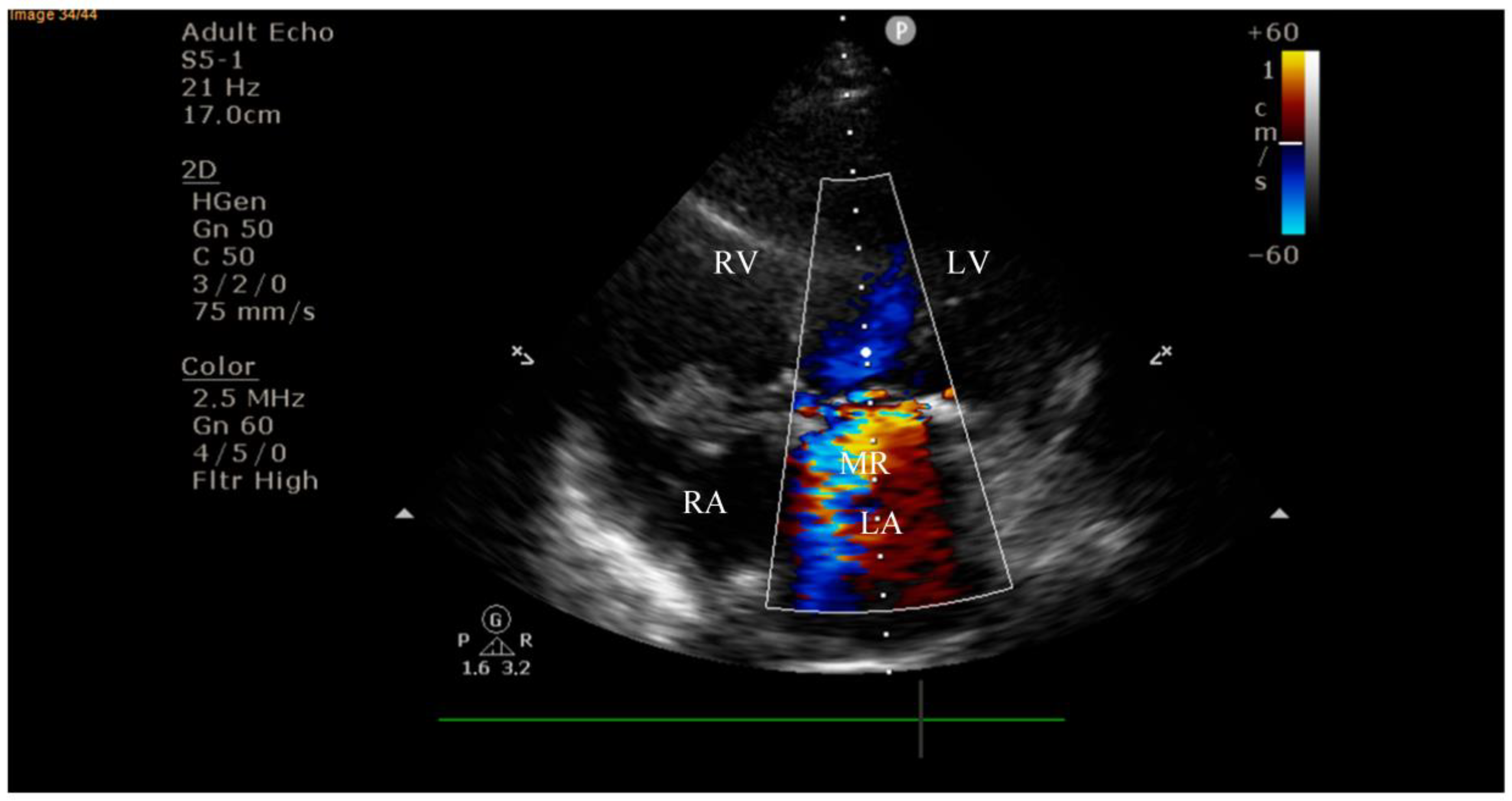
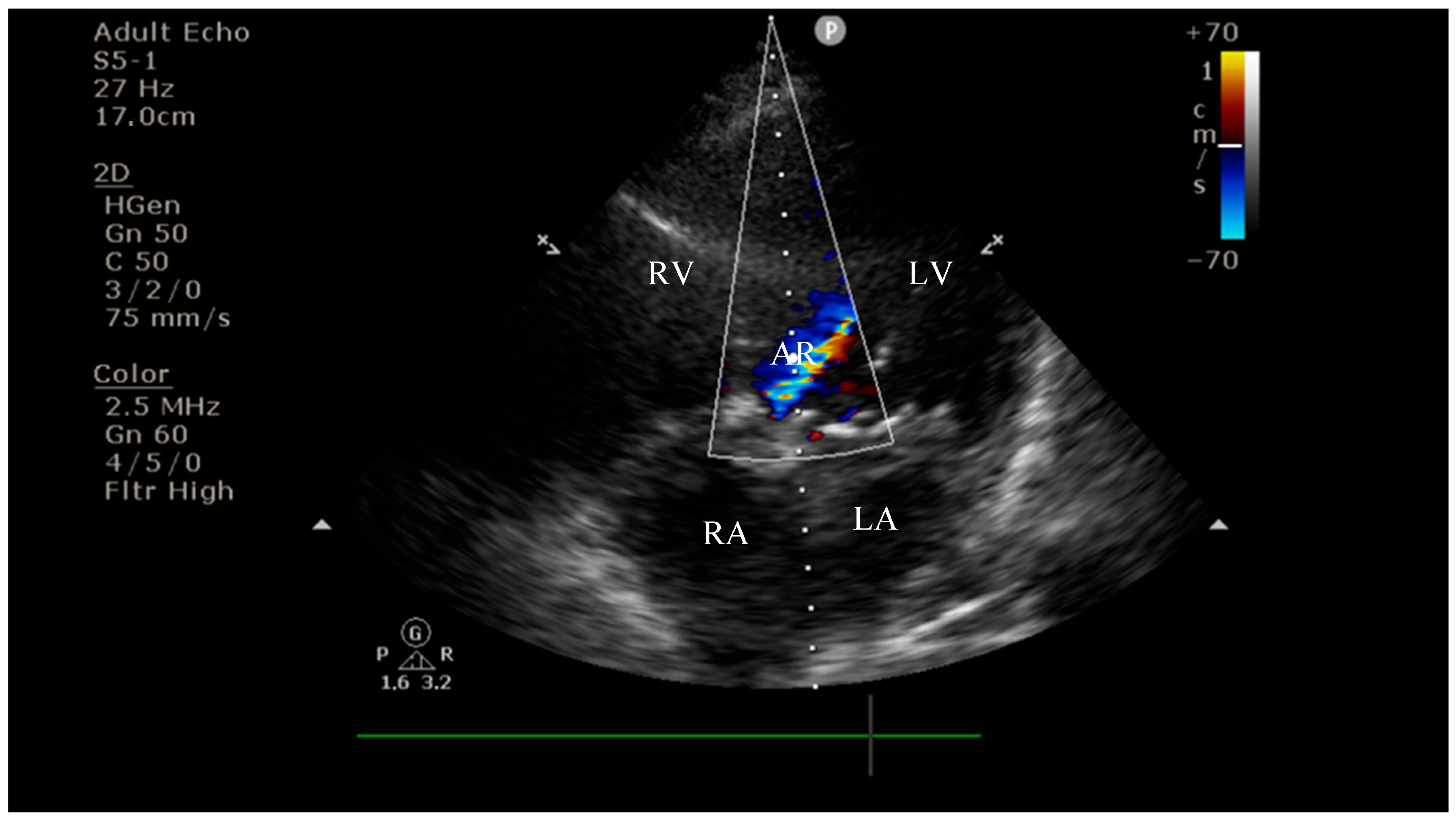
4.2. Diagnostic Findings: Mitral Valve Dysfunction and Embolic Phenomena
4.3. Coronary Complications and Diagnostic Dilemma
4.4. Therapeutic Limitations
5. Conclusions and Future Directions
- •
- PVE after TAVI is rare but associated with high morbidity and mortality, requiring a high index of suspicion.
- •
- Atypical manifestations of endocarditis, such as musculoskeletal symptoms (sacroiliitis), can delay recognition and appropriate treatment.
- •
- Negative blood cultures, often due to prior antibiotic exposure, represent a diagnostic challenge in suspected PVE.
- •
- STEMI complicating PVE raises a critical therapeutic dilemma, as distinguishing thrombotic occlusion from septic embolization is essential but often difficult; management requires individualized, multidisciplinary decision-making.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Joseph, J.; Naqvi, S.Y.; Giri, J.; Goldberg, S. Aortic Stenosis: Pathophysiology, Diagnosis, and Therapy. Am. J. Med. 2017, 130, 253–263. [Google Scholar] [CrossRef]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of Valvular Heart Diseases: A Population-Based Study. Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Rodriguez Muñoz, D.; et al. 2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef] [PubMed]
- Osnabrugge, R.L.J.; Mylotte, D.; Head, S.J.; Van Mieghem, N.M.; Nkomo, V.T.; LeReun, C.M.; Bogers, A.J.J.C.; Piazza, N.; Kappetein, A.P. Aortic Stenosis in the Elderly. J. Am. Coll. Cardiol. 2013, 62, 1002–1012. [Google Scholar] [CrossRef]
- Yu Chen, H.; Dina, C.; Small, A.M.; Shaffer, C.M.; Levinson, R.T.; Helgadóttir, A.; Capoulade, R.; Munter, H.M.; Martinsson, A.; Cairns, B.J.; et al. Dyslipidemia, Inflammation, Calcification, and Adiposity in Aortic Stenosis: A Genome-Wide Study. Eur. Heart J. 2023, 44, 1927–1939. [Google Scholar] [CrossRef] [PubMed]
- Goody, P.R.; Hosen, M.R.; Christmann, D.; Niepmann, S.T.; Zietzer, A.; Adam, M.; Bönner, F.; Zimmer, S.; Nickenig, G.; Jansen, F. Aortic Valve Stenosis: From Basic Mechanisms to Novel Therapeutic Targets. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 885–900. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.M.; O’Brien, S.M.; Wu, C.; Sikora, J.A.H.; Griffith, B.P.; Gammie, J.S. Isolated Aortic Valve Replacement in North America Comprising 108,687 Patients in 10 Years: Changes in Risks, Valve Types, and Outcomes in the Society of Thoracic Surgeons National Database. J. Thorac. Cardiovasc. Surg. 2009, 137, 82–90. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Pibarot, P.; Hahn, R.T.; Genereux, P.; Kodali, S.K.; Kapadia, S.R.; Cohen, D.J.; Pocock, S.J.; et al. Transcatheter Aortic-Valve Replacement in Low-Risk Patients at Five Years. N. Engl. J. Med. 2023, 389, 1949–1960. [Google Scholar] [CrossRef]
- Delgado, V.; Ajmone Marsan, N.; De Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the Management of Endocarditis. Eur. Heart J. 2023, 44, 3948–4042. [Google Scholar] [CrossRef] [PubMed]
- Del Val, D.; Panagides, V.; Mestres, C.A.; Miró, J.M.; Rodés-Cabau, J. Infective Endocarditis After Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2023, 81, 394–412. [Google Scholar] [CrossRef]
- Strange, J.E.; Østergaard, L.; Køber, L.; Bundgaard, H.; Iversen, K.; Voldstedlund, M.; Gislason, G.H.; Olesen, J.B.; Fosbøl, E.L. Patient Characteristics, Microbiology, and Mortality of Infective Endocarditis After Transcatheter Aortic Valve Implantation. Clin. Infect. Dis. 2023, 77, 1617–1625. [Google Scholar] [CrossRef]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.-P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the Management of Infective Endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC), Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, B.K.; Tariq, M.; Jadoon, A.; Alam, M.; Murtaza, G.; Abid, B.; Sethi, M.J.; Atiq, M.; Abrar, S.; Smego, R.A. Impact of Prior Antibiotic Use in Culture-Negative Endocarditis: Review of 86 Cases from Southern Pakistan. Int. J. Infect. Dis. 2009, 13, 606–612. [Google Scholar] [CrossRef] [PubMed]
- McHugh, J.; Saleh, O.A. Updates in Culture-Negative Endocarditis. Pathogens 2023, 12, 1027. [Google Scholar] [CrossRef]
- Thuny, F.; Disalvo, G.; Belliard, O.; Avierinos, J.-F.; Pergola, V.; Rosenberg, V.; Casalta, J.-P.; Gouvernet, J.; Derumeaux, G.; Iarussi, D.; et al. Risk of Embolism and Death in Infective Endocarditis: Prognostic Value of Echocardiography: A Prospective Multicenter Study. Circulation 2005, 112, 69–75. [Google Scholar] [CrossRef]
- García-Cabrera, E.; Fernández-Hidalgo, N.; Almirante, B.; Ivanova-Georgieva, R.; Noureddine, M.; Plata, A.; Lomas, J.M.; Gálvez-Acebal, J.; Hidalgo-Tenorio, C.; Ruíz-Morales, J.; et al. Neurological Complications of Infective Endocarditis: Risk Factors, Outcome, and Impact of Cardiac Surgery: A Multicenter Observational Study. Circulation 2013, 127, 2272–2284. [Google Scholar] [CrossRef]
- Calderón-Parra, J.; De Villarreal-Soto, J.E.; Oteo-Domínguez, J.F.; Mateos-Seirul, M.; Ríos-Rosado, E.; Dorado, L.; Vera-Puente, B.; Arellano-Serrano, C.; Ramos-Martínez, A.; Forteza-Gil, A. Risk of Infective Endocarditis Associated with Transcatheter Aortic Valve Implantation versus Surgical Aortic Valve Replacement: A Propensity Score-Based Analysis. J. Clin. Med. 2023, 12, 586. [Google Scholar] [CrossRef]
- Calero-Núñez, S.; Ferrer Bleda, V.; Corbí-Pascual, M.; Córdoba-Soriano, J.G.; Fuentes-Manso, R.; Tercero-Martínez, A.; Jiménez-Mazuecos, J.; Barrionuevo Sánchez, M.I. Myocardial Infarction Associated with Infective Endocarditis: A Case Series. Eur. Heart J. Case Rep. 2018, 2, yty032. [Google Scholar] [CrossRef]
- Cohen, S.; Ford, L.; Situ-LaCasse, E.; Tolby, N. Infective Endocarditis Causing Acute Myocardial Infarction. Cureus 2020, 12, e11245. [Google Scholar] [CrossRef]
- Ramakumar, V.; Thakur, A.; Abdulkader, R.S.; Claessen, B.; Anandaram, A.; Palraj, R.; Aravamudan, V.M.; Thoddi Ramamurthy, M.; Dangas, G.; Senguttuvan, N.B. Coronary Stent Infections—A Systematic Review and Meta-Analysis. Cardiovasc. Revasc. Med. 2023, 54, 16–24. [Google Scholar] [CrossRef]
- Kumar, S.S.; Suresh, S.; Iliyas, M.; Vijay, J.; Pillai, V. A Case Report of Left Circumflex Stent Infection and Mycotic Aneurysm: A Rare but Life-Threatening Complication of Percutaneous Coronary Intervention. Egypt. Heart J. 2024, 76, 8. [Google Scholar] [CrossRef]

| Test | Result | Reference Range |
|---|---|---|
| White Blood Cell Count | 10.3 × 103/uI | 4.00–10.0 × 103/uI |
| Lymphocytes | 0.94 × 103/uI | 1.0–4.0 × 103/uI |
| Hematocrit | 35% | 35.0–47.0% |
| Mean Corpuscular Hemoglobin | 26.6 pg | 27.9–34.0 pg |
| Neutrophils | 8.85 × 103/uI | 2.40–6.50 × 103/uI |
| Hemoglobin | 11 g/dL | 12.6–17.4 g/dL |
| Mean Corpuscular Volume | 86.4 fL | 80–100 fL |
| Platelet Count | 229 g/dL | 150–450 g/dL |
| Red Blood Cell Count | 4.13 × 106/uI | 3.80–5.20 × 106/uI |
| Blood glucose | 142 mg/dL | 82–115 mg/dL |
| Aspartate Transaminase | 191 U/L | 5–34 U/L |
| Alanine Transaminase | 241 U/L | 0–55 U/L |
| Gamma-Glutamyl Transferase | 300 U/L | 12–64 U/L |
| Total Bilirubin | 1.1 mg/dL | 0.2–1.2 mg/dL |
| Direct Bilirubin | 0.59 mg/dL | 0.0–0.5 mg/dL |
| Serum Urea | 40 mg/dL | 8.4–25.7 mg/dL |
| Serum Creatinine | 1.53 mg/dL | 0.72–1.25 mg/dL |
| C-Reactive Protein | 28 mg/L | 0–5.0 mg/L |
| Test | Result | Reference Range |
|---|---|---|
| White Blood Cell Count | 8.75 × 103/uI | 4.00–10.0 × 103/uI |
| Lymphocytes | 1.08 × 103/uI | 1.0–4.0 × 103/uI |
| Hematocrit | 33.9% | 35.0–47.0% |
| Mean Corpuscular Hemoglobin | 26.9 pg | 27.9–34.0 pg |
| Neutrophils | 6.99 × 103/uI | 2.40–6.50 × 103/uI |
| Hemoglobin | 10.9 g/dL | 12.6–17.4 g/dL |
| Mean Corpuscular Volume | 83.9 fL | 80–100 fL |
| Platelet Count | 205 g/dL | 150–450 g/dL |
| Red Blood Cell Count | 4.07 × 106/uI | 3.80–5.20 × 106/uI |
| Blood glucose | 150 mg/dL | 82–115 mg/dL |
| Aspartate Transaminase | 105 U/L | 5–34 U/L |
| Alanine Transaminase | 67 U/L | 0–55 U/L |
| Gamma-Glutamyl Transferase | 122 U/L | 12–64 U/L |
| Total Bilirubin | 1 mg/dL | 0.2–1.2 mg/dL |
| Direct Bilirubin | 0.5 mg/dL | 0.0–0.5 mg/dL |
| Serum Urea | 16 mg/dL | 8.4–25.7 mg/dL |
| Serum Creatinine | 1.3 mg/dL | 0.72–1.25 mg/dL |
| C-Reactive Protein | 45 mg/L | 0–5.0 mg/L |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rus, C.B.; Cinezan, C. Diagnostic Pitfalls of Prosthetic Valve Endocarditis: From Sacroiliitis to Coronary Septic Embolization. Diagnostics 2025, 15, 2620. https://doi.org/10.3390/diagnostics15202620
Rus CB, Cinezan C. Diagnostic Pitfalls of Prosthetic Valve Endocarditis: From Sacroiliitis to Coronary Septic Embolization. Diagnostics. 2025; 15(20):2620. https://doi.org/10.3390/diagnostics15202620
Chicago/Turabian StyleRus, Camelia Bianca, and Corina Cinezan. 2025. "Diagnostic Pitfalls of Prosthetic Valve Endocarditis: From Sacroiliitis to Coronary Septic Embolization" Diagnostics 15, no. 20: 2620. https://doi.org/10.3390/diagnostics15202620
APA StyleRus, C. B., & Cinezan, C. (2025). Diagnostic Pitfalls of Prosthetic Valve Endocarditis: From Sacroiliitis to Coronary Septic Embolization. Diagnostics, 15(20), 2620. https://doi.org/10.3390/diagnostics15202620






