Predicting Mortality in Older Adults Using Comprehensive Geriatric Assessment: A Comparative Study of Traditional Statistics and Machine Learning Approaches
Abstract
1. Introduction
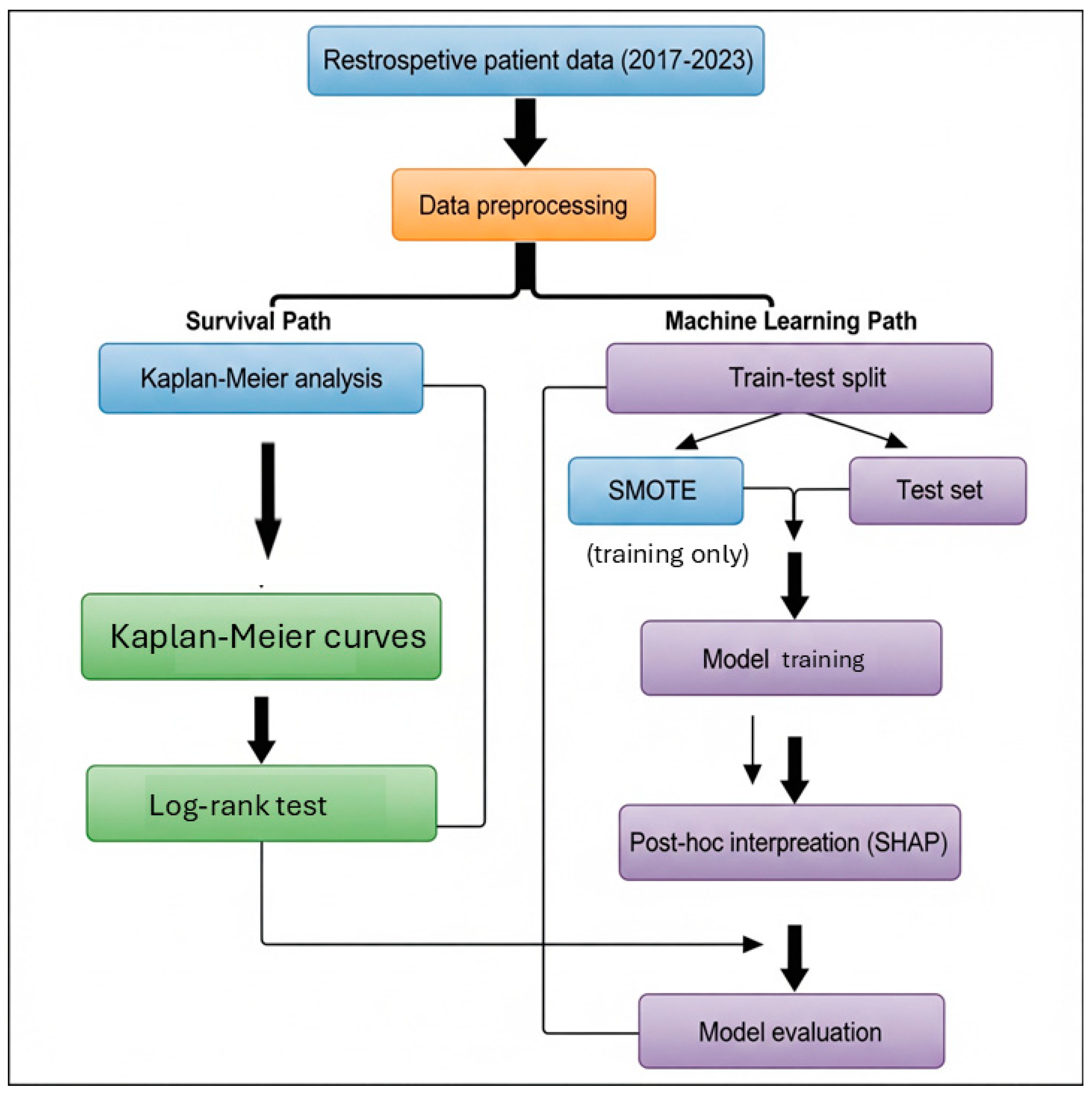
2. Materials and Methods
2.1. CGA Variables
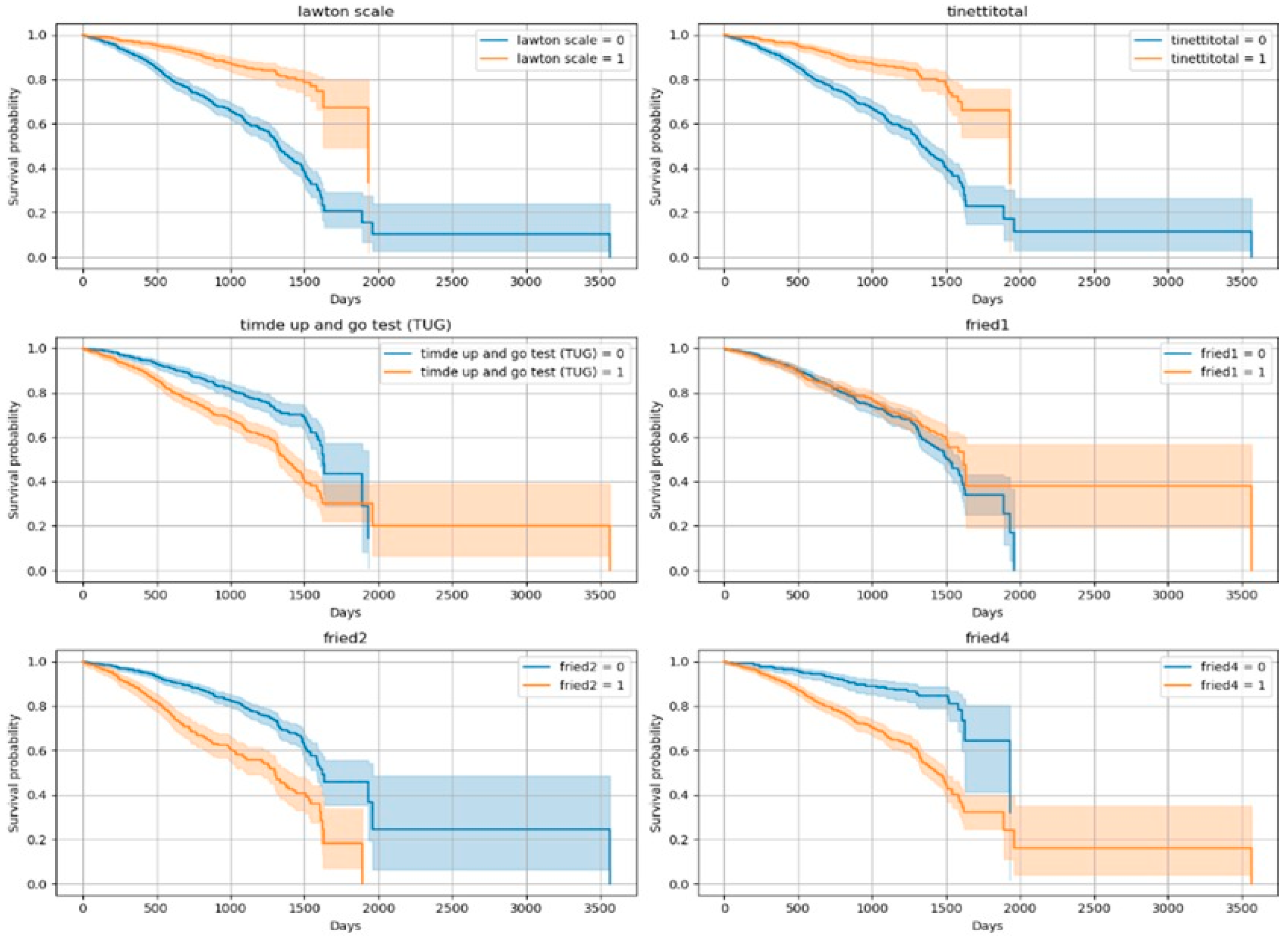
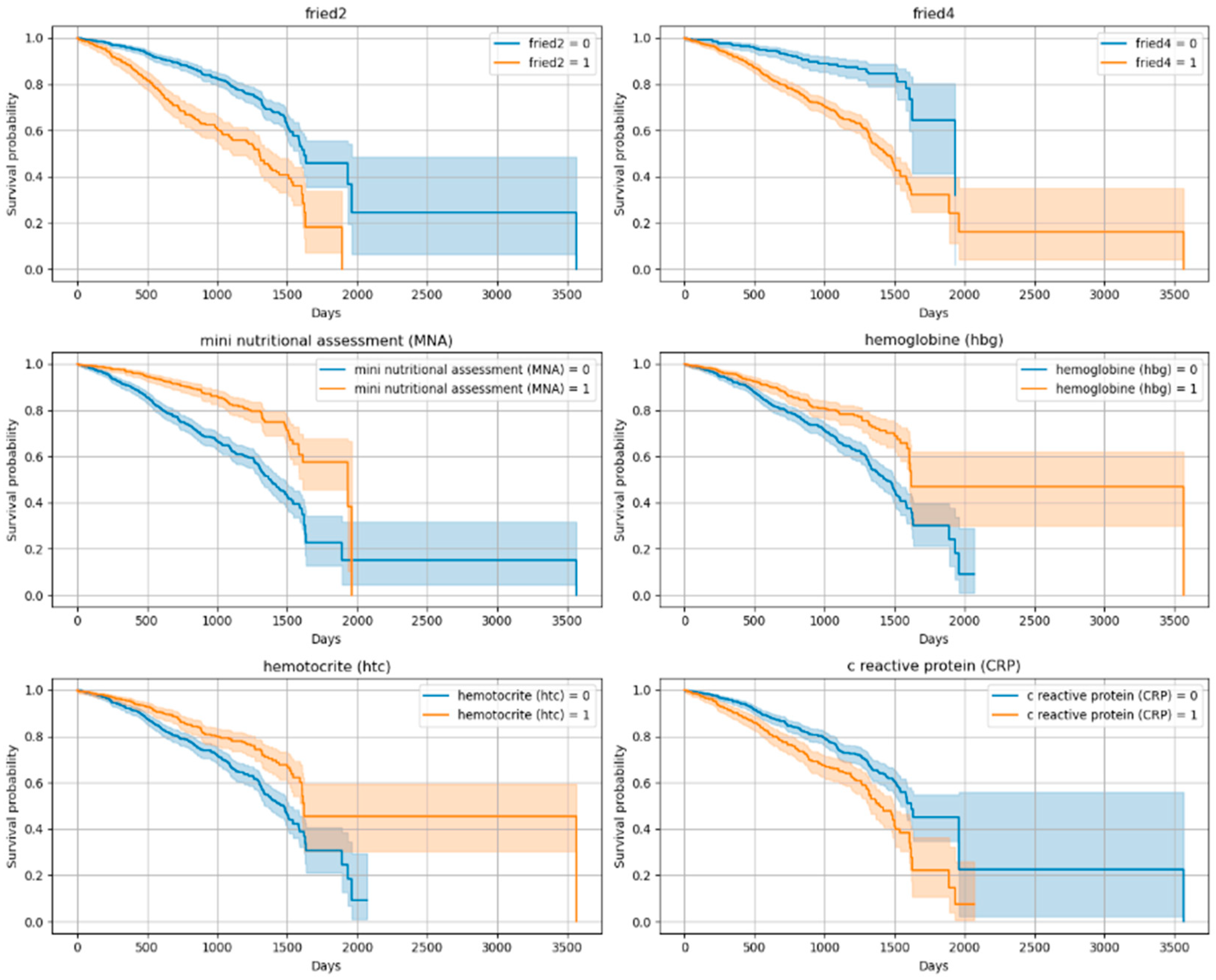
2.2. Survival Analysis
2.3. Machine Learning Models
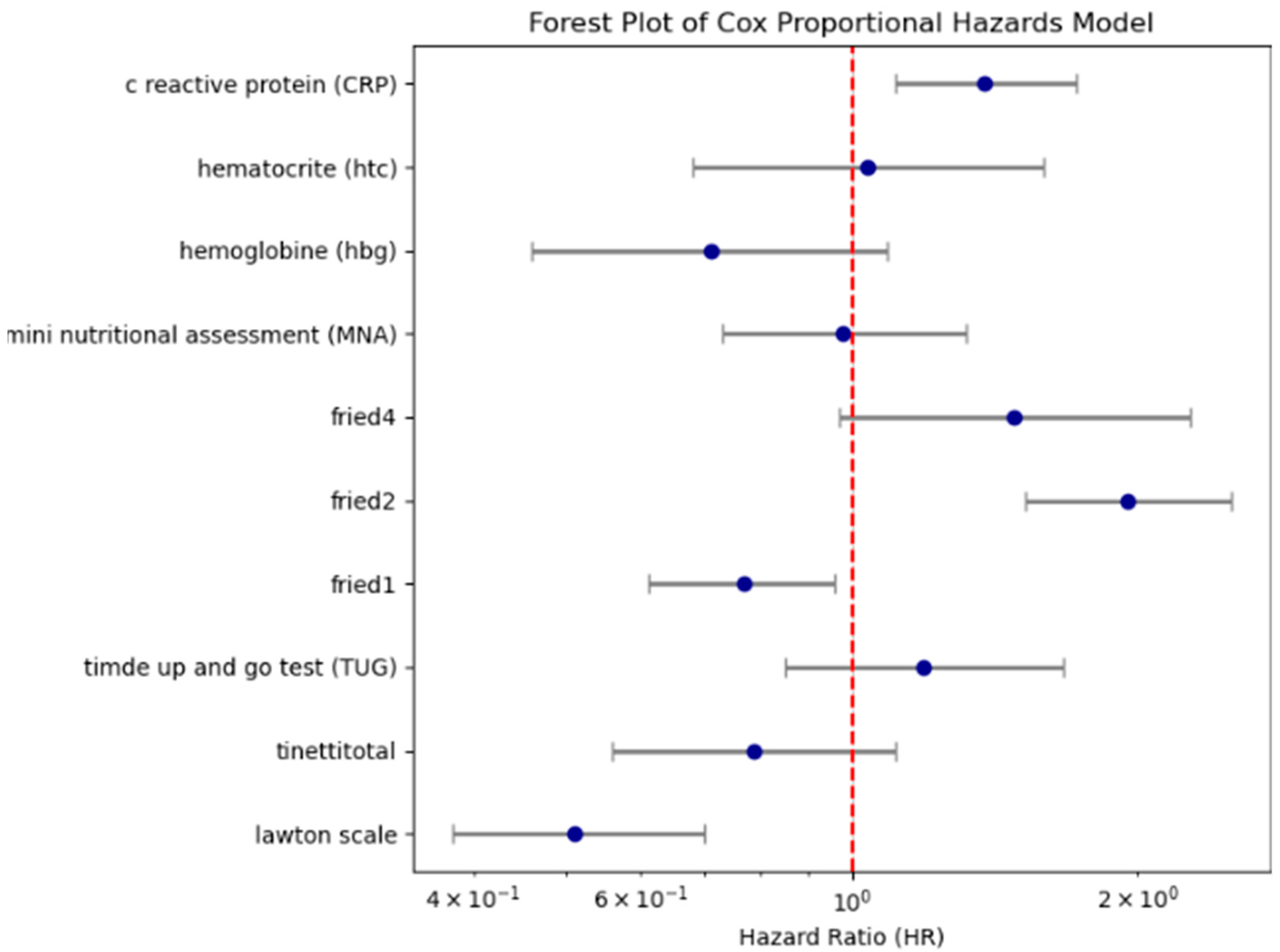
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Veronese, N.; Custodero, C.; Demurtas, J.; Smith, L.; Barbagallo, M.; Maggi, S.; Cella, A.; Vanacore, N.; Aprile, P.L.; Ferrucci, L.; et al. Comprehensive geriatric assessment in older people: An umbrella review of health outcomes. Age Ageing 2022, 51, afac104. [Google Scholar] [CrossRef]
- Veronese, N.; Fazzari, A.; Santangelo, E.; Iommi, C.; Soysal, P.; Custodero, C.; Pickert, L.; Polidori, M.C.; Stolniceanu, N.; Michalkova, H.; et al. The role of comprehensive geriatric assessment in older patients affected by knee osteoarthritis: An exploratory randomized controlled trial. Aging Clin. Exp. Res. 2025, 37, 155. [Google Scholar] [CrossRef]
- Katipoglu, B.; Kocyigit, S.E. Impact of geriatric syndrome burden on healthcare services utilization and mortality among community-dwelling older adults: Is it still too late to do something? Eur. Geriatr. Med. 2025, 16, 1055–1061. [Google Scholar] [CrossRef]
- Veizi, B.G.Y.; Naharcı, M.I. Geriatric syndromes associated with long-term mortality in adults aged 90 years and older. Geriatr. Nurs. 2025, 64, 103377. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Heybeli, C.; Koc Okudur, S.; Caliskan Bozyel, E.; Smith, L.; Kazancioglu, R. Prevalence and co-incidence of geriatric syndromes according to glomerular filtration rate in older patients. Int. Urol. Nephrol. 2023, 55, 469–476. [Google Scholar] [CrossRef]
- Topcu, A.; Yasin, A.I.; Besiroglu, M.; Sucuoglu Isleyen, Z.; Alaca Topcu, Z.; Simsek, M.; Turk, H.M.; Seker, M.; Soysal, P. Prevalence and co-incidence of geriatric syndromes according to the ECOG performance status in older cancer patients. Front. Med. 2024, 11, 1331246. [Google Scholar] [CrossRef]
- Soysal, P.; Smith, L. The prevalence and co-existence of geriatric syndromes in older patients with dementia compared to those without dementia. Aging Clin. Exp. Res. 2024, 36, 66. [Google Scholar] [CrossRef] [PubMed]
- Litjens, E.J.R.; Dani, M.; Verberne, W.R.; Van Den Noortgate, N.J.; Joosten, H.M.H.; Brys, A.D.H. Geriatric Assessment in Older Patients with Advanced Kidney Disease: A Key to Personalized Care and Shared Decision-Making—A Narrative Review. J. Clin. Med. 2025, 14, 1749. [Google Scholar] [CrossRef] [PubMed]
- Overcash, J.; Ford, N.; Kress, E.; Ubbing, C.; Williams, N. Comprehensive Geriatric Assessment as a Versatile Tool to Enhance the Care of the Older Person Diagnosed with Cancer. Geriatrics 2019, 4, 39. [Google Scholar] [CrossRef]
- Bzdok, D.; Altman, N.; Krzywinski, M. Statistics versus machine learning. Nat. Methods 2018, 15, 233–234. [Google Scholar] [CrossRef]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef]
- Audureau, E.; Soubeyran, P.; Martinez-Tapia, C.; Bellera, C.; Bastuji-Garin, S.; Boudou-Rouquette, P.; Chahwakilian, A.; Grellety, T.; Hanon, O.; Mathoulin-Pélissier, S.; et al. Machine Learning to Predict Mortality in Older Patients With Cancer: Development and External Validation of the Geriatric Cancer Scoring System Using Two Large French Cohorts. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2025, 43, 1429–1440. [Google Scholar] [CrossRef] [PubMed]
- Göl, M.; Aktürk, C.; Talan, T.; Vural, M.S.; Türkbeyler, İ.H. Predicting malnutrition-based anemia in geriatric patients using machine learning methods. J. Eval. Clin. Pract. 2025, 31, e14142. [Google Scholar] [CrossRef]
- Obermeyer, Z.; Emanuel, E.J. Predicting the Future—Big Data, Machine Learning, and Clinical Medicine. N. Engl. J. Med. 2016, 375, 1216–1219. [Google Scholar] [CrossRef] [PubMed]
- Sidey-Gibbons, J.A.M.; Sidey-Gibbons, C.J. Machine learning in medicine: A practical introduction. BMC Med. Res. Methodol. 2019, 19, 64. [Google Scholar] [CrossRef]
- Durmaz, B.; Soysal, P.; Ellidokuz, H.; Isik, A.T. Validity and reliability of geriatric depression scale-15 (short form) in Turkish older adults. N. Clin. Istanb. 2018, 5, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Molloy, D.W.; Alemayehu, E.; Roberts, R. Reliability of a Standardized Mini-Mental State Examination compared with the traditional Mini-Mental State Examination. Am. J. Psychiatry 1991, 148, 102–105. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [CrossRef]
- Strini, V.; Piazzetta, N.; Gallo, A.; Schiavolin, R. Barthel Index: Creation and validation of two cut-offs using the BRASS Index. Acta Biomed. 2020, 91, 19–26. [Google Scholar] [CrossRef]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.L. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.-Y. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. In Advances in Neural Information Processing Systems; Curran Associates, Inc.: Red Hook, NY, USA, 2017; Volume 30, pp. 3146–3154. Available online: https://proceedings.neurips.cc/paper/2017/hash/6449f44a102fde848669bdd9eb6b76fa-Abstract.html (accessed on 1 September 2025).
- Goodfellow, I.; Bengio, Y.; Courville, A.; Bengio, Y. Deep Learning; MIT Press: Cambridge, MA, USA, 2016; Volume 1, Available online: https://www.deeplearningbook.org/ (accessed on 1 September 2025).
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Nohara, Y.; Matsumoto, K.; Soejima, H.; Nakashima, N. Explanation of machine learning models using shapley additive explanation and application for real data in hospital. Comput. Methods Programs Biomed. 2022, 214, 106584. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016; Available online: https://www.R-project.org/ (accessed on 1 September 2025).
- Zhang, L.; Ji, T.; Sun, F.; Li, Y.; Tang, Z.; Ma, L. A Simplified Frailty Index Predicts Mortality in Older Adults in Beijing. Risk Manag. Healthc. Policy 2021, 14, 4867–4873. [Google Scholar] [CrossRef]
- Calder, P.C.; Bosco, N.; Bourdet-Sicard, R.; Capuron, L.; Delzenne, N.; Doré, J.; Franceschi, C.; Lehtinen, M.J.; Recker, T.; Salvioli, S.; et al. Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition. Ageing Res. Rev. 2017, 40, 95–119. [Google Scholar] [CrossRef]
- Ferrucci, L.; Fabbri, E. Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef]
- Soysal, P.; Stubbs, B.; Lucato, P.; Luchini, C.; Solmi, M.; Peluso, R.; Sergi, G.; Isik, A.T.; Manzato, E.; Maggi, S.; et al. Inflammation and frailty in the elderly: A systematic review and meta-analysis. Ageing Res. Rev. 2016, 31, 1–8. [Google Scholar] [CrossRef]
- Soysal, P.; Isik, A.T.; Carvalho, A.F.; Fernandes, B.S.; Solmi, M.; Schofield, P.; Veronese, N.; Stubbs, B. Oxidative stress and frailty: A systematic review and synthesis of the best evidence. Maturitas 2017, 99, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Ahadi, S.; Zhou, W.; Schüssler-Fiorenza Rose, S.M.; Sailani, M.R.; Contrepois, K.; Avina, M.; Ashland, M.; Brunet, A.; Snyder, M. Personal aging markers and ageotypes revealed by deep longitudinal profiling. Nat. Med. 2020, 26, 83–90. [Google Scholar] [CrossRef]
- Justice, J.N.; Ferrucci, L.; Newman, A.B.; Aroda, V.R.; Bahnson, J.L.; Divers, J.; Espeland, M.A.; Marcovina, S.; Pollak, M.N.; Kritchevsky, S.B.; et al. A framework for selection of blood-based biomarkers for geroscience-guided clinical trials: Report from the TAME Biomarkers Workgroup. Geroscience 2018, 40, 419–436. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, B.K.; Berger, S.L.; Brunet, A.; Campisi, J.; Cuervo, A.M.; Epel, E.S.; Franceschi, C.; Lithgow, G.J.; Morimoto, R.I.; Pessin, J.E.; et al. Geroscience: Linking aging to chronic disease. Cell 2014, 159, 709–713. [Google Scholar] [CrossRef]
- Levine, M.E. Modeling the rate of senescence: Can estimated biological age predict mortality more accurately than chronological age? J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Isik, A.T.; Arik, F.; Kalan, U.; Eyvaz, A.; Veronese, N. Validity of the Mini-Nutritional Assessment Scale for Evaluating Frailty Status in Older Adults. J. Am. Med. Dir. Assoc. 2019, 20, 183–187. [Google Scholar] [CrossRef]
- Tan, H.C.; Zeng, L.J.; Yang, S.J.; Hou, L.S.; Wu, J.H.; Cai, X.H.; Heng, F.; Gu, X.Y.; Zhong, Y.; Dong, B.R.; et al. Deep learning model for the prediction of all-cause mortality among long term care people in China: A prospective cohort study. Sci. Rep. 2024, 14, 14639. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 2010, 21, 128–138. [Google Scholar] [CrossRef]
- Van Calster, B.; McLernon, D.J.; van Smeden, M.; Wynants, L.; Steyerberg, E.W.; Bossuyt, P.; Collins, G.S.; Macaskill, P.; McLernon, D.J.; Moons, K.G.M.; et al. Calibration: The Achilles heel of predictive analytics. BMC Med. 2019, 17, 230. [Google Scholar] [CrossRef]
- Susnjak, T.; Griffin, E. Towards clinical prediction with transparency: An explainable AI approach to survival modelling in residential aged care. Comput. Methods Programs Biomed. 2025, 263, 108653. [Google Scholar] [CrossRef]
| Mortality Status (Status) | |||
|---|---|---|---|
| Variables | 0 N = 1544 * | 1 N = 430 * | p-value ** |
| Gender, Female (%) | 1.139 (74%) | 260 (60%) | <0.001 |
| Age, years | 81.01 (7.71) | 86.19 (7.17) | <0.001 |
| Marital Status | <0.001 | ||
| Single | 77 (5.0%) | 44 (10%) | |
| Married | 740 (48%) | 182 (42%) | |
| Wife/Husband ex | 699 (45%) | 200 (47%) | |
| Widowed | 28 (1.8%) | 4 (0.9%) | |
| Caregiving Status | 131 (8.5%) | 12 (2.8%) | <0.001 |
| Driving | <0.001 | ||
| Never drove | 1213 (79%) | 330 (77%) | |
| Driver in the past | 222 (14%) | 88 (20%) | |
| Active driver | 109 (7.1%) | 12 (2.8%) | |
| Smoking | 0.6 | ||
| No smoking history | 1023 (66%) | 254 (59%) | |
| Smoker in the past | 400 (26.2%) | 141 (33%) | |
| Active smoker | 116 (7.5%) | 34 (7.9%) | |
| Number of Drugs Used | 6.39 (3.50) | 6.91 (3.68) | 0.006 |
| Dementia | 455 (29%) | 186 (43%) | <0.001 |
| Coronary Artery disease (CAD) | 252 (16%) | 135 (31%) | <0.001 |
| Congestive Heart failure (CHF) | 148 (9.6%) | 76 (18%) | <0.001 |
| Benign Prostate Hyperplasia (BPH) | 105 (6.8%) | 52 (12%) | <0.001 |
| Osteoarthritis (OA) | 273 (18%) | 45 (10%) | <0.001 |
| Fall-1 year | 624 (40%) | 227 (53%) | <0.001 |
| Dizziness | 690 (45%) | 177 (41%) | <0.001 |
| Number of Nocturia | 2.17 (1.96) | 2.51 (2.36) | <0.001 |
| Constipation | 667 (43%) | 202 (47%) | 0.002 |
| Hypertension | 1081 (70%) | 287 (67%) | 0.4 |
| Chronic Obstructive Lung Disease (COPD) | 96 (6.2%) | 41 (9.5%) | 0.017 |
| Cerebrovascular disease (CVD) | 166 (11%) | 65 (15%) | 0.013 |
| Parkinson Disease | 128 (8.3%) | 53 (12%) | 0.010 |
| Incontinence | 869 (56%) | 253 (59%) | 0.2 |
| Nocturia | 1239 (80%) | 32 (77%) | 0.3 |
| Pain | 949 (61%) | 214 (50%) | 0.2 |
| Variable → HR | (exp(coef)) | p-Value | Interpretation |
|---|---|---|---|
| Lawton scale | 0.51 | <0.005 | Low functional status → Approximately 2 times higher risk of mortality |
| fried2 | 1.95 | <0.005 | Frailty component → 95% increased risk |
| fried4 | 1.48 | 0.07 | Marginally significant |
| CRP | 1.38 | <0.005 | High CRP → 38% increased risk |
| fried1 | 0.77 | 0.02 | Appears to have a slight protective effect |
| Tinetti total | 0.79 | 0.17 | Not statistically significant |
| TUG | 1.19 | 0.31 | Not significant |
| MNA | 0.98 | 0.89 | Not significant |
| Hb | 0.71 | 0.38 | Not significant |
| Htc | 1.04 | 0.86 | Not significant |
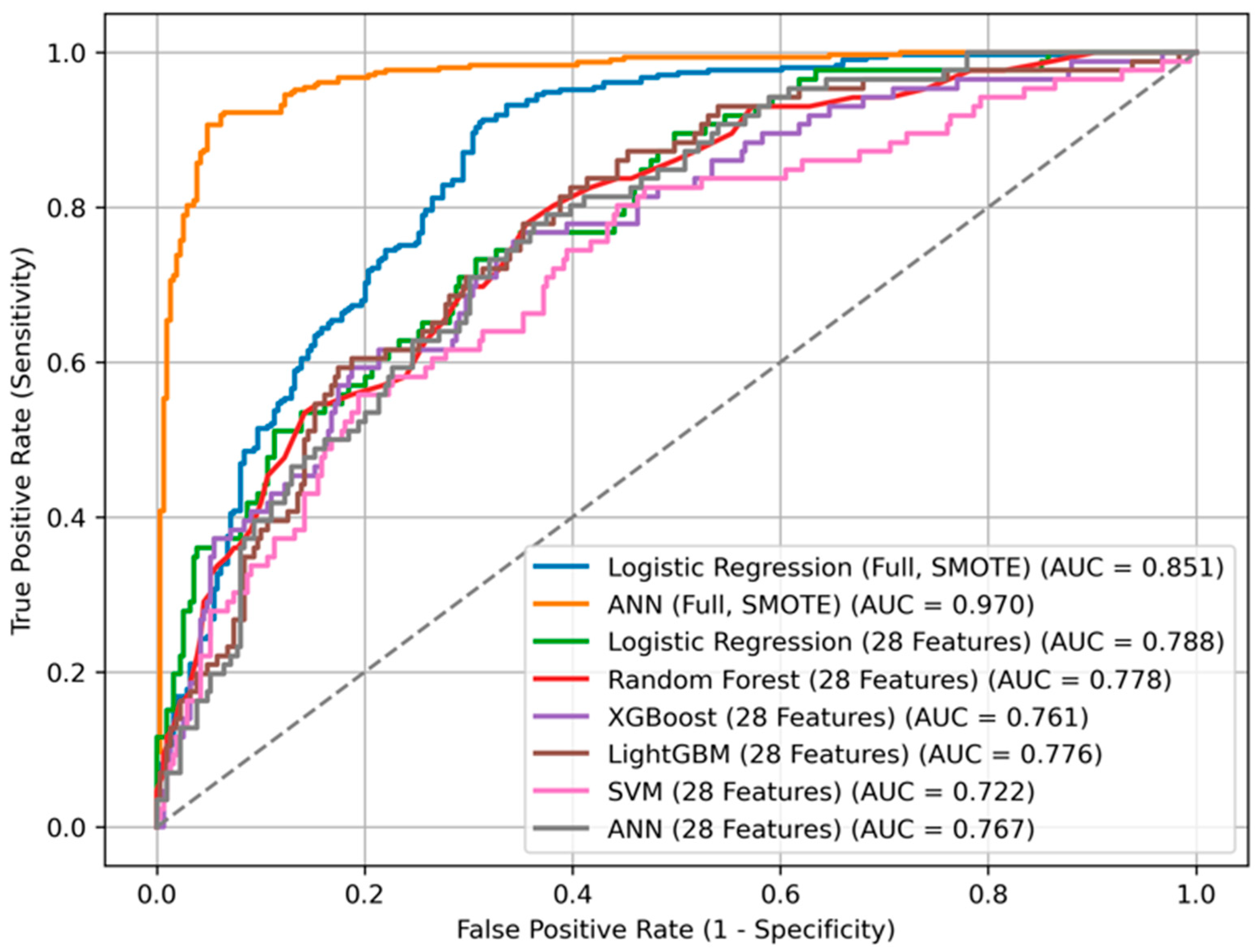
| Variables Count | Missing Value Handling | Model | Accu. | Specif. | Sensitiv. | F1 Score | PPV * | NPV * | Balanced Acc. | ROC AUC | AUC (CV, #break# Mean ± SD) | AUC (95% CI) | Brier Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALL Features | Imputation (Median) + SMOTE | ANN | 0.872 | 0.861 | 0.883 | 0.874 | 0.864 | 0.881 | 0.872 | 0.970 | 0.962 ± 0.012 | (0.958–0.981) | 0.079 |
| ALL Features | Multiple Imputation (MI) + SMOTE | ANN | 0.868 | 0.857 | 0.879 | 0.870 | 0.860 | 0.877 | 0.868 | 0.964 | 0.958 ± 0.013 | (0.952–0.976) | 0.083 |
| All Features | Imputation (Median) + SMOTE | LR | 0.841 | 0.826 | 0.847 | 0.826 | 0.834 | 0.853 | 0.838 | 0.851 | 0.846 ± 0.015 | (0.832–0.868) | 0.148 |
| ALL Features | Multiple Imputation (MI) + SMOTE | LR | 0.839 | 0.824 | 0.844 | 0.824 | 0.833 | 0.852 | 0.837 | 0.848 | 0.843 ± 0.016 | (0.829–0.866) | 0.152 |
| Selected 28 Features | Complete Case Anal. | LR | 0.813 | 0.974 | 0.233 | 0.351 | 0.714 | 0.823 | 0.603 | 0.788 | 0.787 ± 0.019 | (0.770–0.809) | 0.172 |
| Selected 28 Features | MI | LR | 0.815 | 0.971 | 0.237 | 0.355 | 0.718 | 0.826 | 0.606 | 0.790 | 0.788 ± 0.018 | (0.771–0.810) | 0.170 |
| Selected 28 Features | Complete Case Anal. | ANN | 0.808 | 0.951 | 0.291 | 0.397 | 0.625 | 0.828 | 0.621 | 0.767 | 0.765 ± 0.022 | (0.746–0.792) | 0.180 |
| Selected 28 Features | MI | ANN | 0.811 | 0.948 | 0.296 | 0.302 | 0.629 | 0.831 | 0.622 | 0.769 | 0.767 ± 0.020 | (0.748–0.791) | 0.182 |
| Selected 28 Features | Complete Case Anal. | RF | 0.800 | 0.977 | 0.163 | 0.262 | 0.667 | 0.807 | 0.570 | 0.778 | 0.775 ± 0.018 | (0.760–0.800) | 0.161 |
| Selected 28 Features | MI | RF | 0.802 | 0.975 | 0.169 | 0.268 | 0.670 | 0.810 | 0.573 | 0.780 | 0.778 ± 0.014 | (0.762–0.802) | 0.159 |
| Selected 28 Features | Complete Case Anal. | XGBoost | 0.815 | 0.945 | 0.349 | 0.451 | 0.638 | 0.839 | 0.647 | 0.761 | 0.760 ± 0.020 | 0.741–0.785) | 0.168 |
| Selected 28 Features | MI | XGBoost | 0.817 | 0.943 | 0.353 | 0.455 | 0.642 | 0.841 | 0.658 | 0.763 | 0.761 ± 0.013 | (0.744–0.786) | 0.165 |
| Selected 28 Features | Complete Case Anal. | LightGBM | 0.777 | 0.929 | 0.233 | 0.312 | 0.476 | 0.813 | 0.581 | 0.776 | 0.775 ± 0.018 | (0.756–0.797 | 0.170 |
| Selected 28 Features | MI | LightGBM | 0.779 | 0.927 | 0.238 | 0.317 | 0.480 | 0.816 | 0.582 | 0.777 | 0.776 ± 0.018 | (0.757–0.798) | 0.168 |
| Selected 28 Features | Complete Case Anal. | SVM | 0.782 | 0.990 | 0.035 | 0.065 | 0.500 | 0.787 | 0.513 | 0.722 | 0.720 ± 0.021 | (0.700–0.747) | 0.190 |
| Selected 28 Features | MI | SVM | 0.784 | 0.987 | 0.040 | 0.070 | 0.503 | 0.790 | 0.515 | 0.724 | 0.724 ± 0.021 | (0.703–0.749) | 0.188 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avsar Kucukkurt, E.; Sonuvar, E.T.; Yapar, D.; Demir Avcı, Y.; Tanriverdi, I.; Behzad, A.; Soysal, P. Predicting Mortality in Older Adults Using Comprehensive Geriatric Assessment: A Comparative Study of Traditional Statistics and Machine Learning Approaches. Diagnostics 2025, 15, 2491. https://doi.org/10.3390/diagnostics15192491
Avsar Kucukkurt E, Sonuvar ET, Yapar D, Demir Avcı Y, Tanriverdi I, Behzad A, Soysal P. Predicting Mortality in Older Adults Using Comprehensive Geriatric Assessment: A Comparative Study of Traditional Statistics and Machine Learning Approaches. Diagnostics. 2025; 15(19):2491. https://doi.org/10.3390/diagnostics15192491
Chicago/Turabian StyleAvsar Kucukkurt, Esin, Esra Tokur Sonuvar, Dilek Yapar, Yasemin Demir Avcı, Irem Tanriverdi, Andisha Behzad, and Pinar Soysal. 2025. "Predicting Mortality in Older Adults Using Comprehensive Geriatric Assessment: A Comparative Study of Traditional Statistics and Machine Learning Approaches" Diagnostics 15, no. 19: 2491. https://doi.org/10.3390/diagnostics15192491
APA StyleAvsar Kucukkurt, E., Sonuvar, E. T., Yapar, D., Demir Avcı, Y., Tanriverdi, I., Behzad, A., & Soysal, P. (2025). Predicting Mortality in Older Adults Using Comprehensive Geriatric Assessment: A Comparative Study of Traditional Statistics and Machine Learning Approaches. Diagnostics, 15(19), 2491. https://doi.org/10.3390/diagnostics15192491






