Use of Ultrasound for Body Composition in Assessment in Pediatric Patients: Are There Still Challenges?
Abstract
1. Introduction
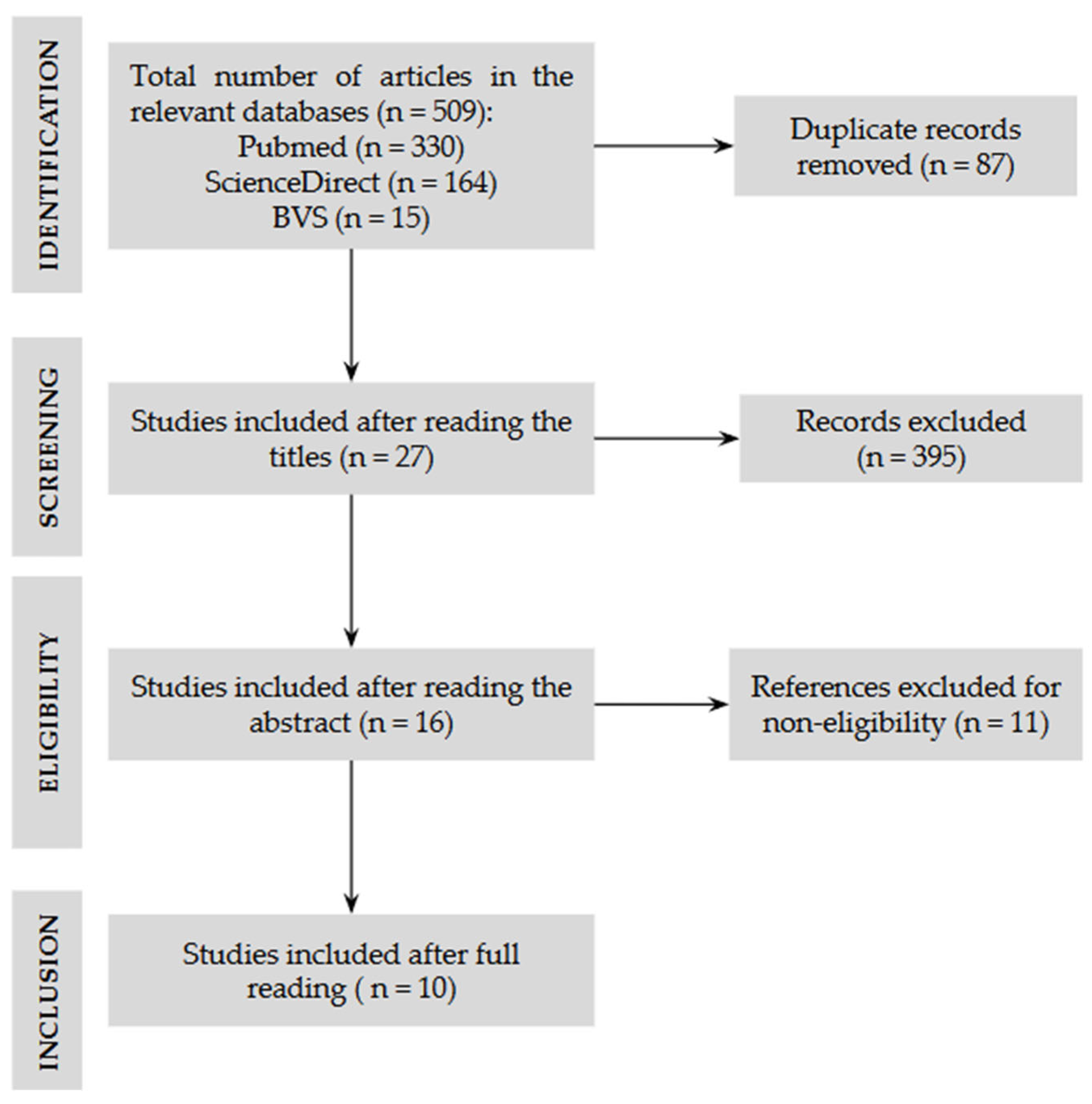
2. Materials and Methods
3. Results
3.1. Nutritional Assessment Methods: Ultrasound
3.1.1. General Characteristics of Ultrasonography and Methods Used for Body Composition Assessment
3.1.2. Challenges of Using Ultrasound in the Assessment of Pediatric Patients
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mehta, N.M.; Corkins, M.R.; Lyman, B.; Malone, A.; Goday, P.S.; Carney, L.N.; Monczka, J.L.; Plogsted, S.W.; Schwenk, W.F. Defining pediatric malnutrition: A paradigm shift toward etiology-related definitions. J. Parenter. Enter. Nutr. 2013, 37, 460–481. [Google Scholar] [CrossRef] [PubMed]
- Bouma, S. Diagnosing Pediatric Malnutrition: Paradigm Shifts of Etiology-Related Definitions and Appraisal of the Indicators. Nutr. Clin. Pract. 2017, 32, 52–67. [Google Scholar] [CrossRef] [PubMed]
- Mannar, V.; Micha, R.; Allemandi, L.; Afshin, A.; Baker, P.; Battersby, J.; Bhutta, Z.; Corvalan, C.; Di Cesare, M.; Chen, K.; et al. 2020 Global Nutrition Report: Action on Equity to End Malnutrition; Development Initiatives Poverty Research: Bristol, UK, 2020; Available online: https://globalnutritionreport.org/reports/2020-global-nutrition-report/ (accessed on 30 June 2025).
- Dipasquale, V.; Cucinotta, U.; Romano, C. Acute malnutrition in children: Pathophysiology, clinical effects and treatment. Nutrients 2020, 12, 2413. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhutta, Z.A.; Berkley, J.A.; Bandsma, R.H.J.; Kerac, M.; Trehan, I.; Briend, A. Severe childhood malnutrition. Nat. Rev. Dis. Primers 2017, 3, 17067. [Google Scholar] [CrossRef]
- Göktaş, Ö.A.; Tutar, E.; Büyükeren, M.; Akin, Y. Malnutrition prevalence in hospitalized pediatric patients: A comparison of national and World Health Organization Growth Standards. Nutr. Clin. Pract. 2024, 39, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, A.; Delvin, E.; Marcil, V.; Belanger, V.; Marchand, V.; Boctor, D.; Rashid, M.; Noble, A.; Davidson, B.; Groleau, V.; et al. Prevalence of Malnutrition in Pediatric Hospitals in Developed and In-Transition Countries: The Impact of Hospital Practices. Nutrients 2019, 11, 236. [Google Scholar] [CrossRef] [PubMed]
- Seremet Kurklu, N.; Geyin, F.; Ceylan, L.; Korkut Genc, D.; Kamarli Altun, H.; Karacil Ermumcu, M.S. Comparison of three different nutrition screening tools for pediatric inpatients. Nutr. Clin. Pract. 2022, 37, 698–704. [Google Scholar] [CrossRef]
- Gambra-Arzoz, M.; Alonso-Cadenas, J.A.; Jiménez-Legido, M.; López-Giménez, M.R.; Martín-Rivada, Á.; de Los Ángeles Martínez-Ibeas, M.; Cañedo-Villarroya, E.; Pedrón-Giner, C. Nutrition Risk in Hospitalized Pediatric Patients: Higher Complication Rate and Higher Costs Related to Malnutrition. Nutr. Clin. Pract. 2020, 35, 157–163. [Google Scholar] [CrossRef]
- Pereira, P.S.; da Silva, V.M.; Luz, G.D.; Silva, F.M.; Dalle Molle, R. Nutrition risk prevalence and nutrition screening tools’ validity in hospitalized pediatric patients: A systematic review. J. Parenter. Enter. Nutr. 2023, 47, 184–206. [Google Scholar] [CrossRef]
- Wang, L.Y.; Hu, L.; Huang, X.Y.; Tang, M.L. Implementation of STRONGkids for identifying nutritional risk in pediatric intensive care unit: A survey of Chinese practice. Chin. Med. J. 2020, 134, 867–869. [Google Scholar] [CrossRef]
- Hoffmann, R.M.; Ariagno, K.A.; Pham, I.V.; Barnewolt, C.E.; Jarret, D.Y.; Mehta, N.M.; Kantor, D.B. Ultrasound Assessment of Quadriceps Femoris Muscle Thickness in Critically Ill Children. Pediatr. Crit. Care Med. 2021, 22, 889–897. [Google Scholar] [CrossRef]
- Ong, C.; Lee, J.H.; Puthucheary, Z.A. Muscle Weakness and Wasting in Pediatric Critical Illness. Pediatr. Med. 2021, 4, 13. [Google Scholar] [CrossRef]
- Vieira, R.R.; de Campos, M.M.S.; Zamberlan, P.; Viani, K. Can calf circumference be a viable option for nutritional assessment in the PICU? Clin. Nutr. ESPEN 2021, 45, 356–362. [Google Scholar] [CrossRef]
- Orsso, C.E.; Tibaes, J.R.B.; Oliveira, C.L.P.; Rubin, D.A.; Field, C.J.; Heymsfield, S.B.; Prado, C.M.; Haqq, A.M. Low muscle mass and strength in pediatrics patients: Why should we care? Clin. Nutr. 2019, 38, 2002–2015. [Google Scholar] [CrossRef]
- Danziato Neto, M.A.; de Alencar, E.S.; Carioca, A.A.F.; Daltro, A.F.C.S.; Lima Junior, P.C.B. Use of ultrasound in the rectus femoris muscle to evaluate muscle mass in hospitalized patients: A systematic review. Braspen J. 2022, 37, 82–100. [Google Scholar] [CrossRef]
- Toledo, D.O.; Silva, D.C.L.; dos Santos, D.M.; de Freitas, B.J.; Dib, R.; Cordioli, R.L.; Figueiredo, E.J.A.; Piovacari, S.M.F.; Silva Junior, J.M. Bedside ultrasound is a practical measurement tool for assessing muscle mass. Rev. Bras. Ter. Intensive 2017, 29, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Valla, F.V.; Young, D.K.; Rabilloud, M.; Periasami, U.; John, M.; Baudin, F.; Vuillerot, C.; Portefaix, A.; White, D.; Ridout, J.A.; et al. Thigh Ultrasound Monitoring Identifies Decreases in Quadriceps Femoris Thickness as a Frequent Observation in Critically Ill Children. Pediatr. Crit. Care Med. 2017, 18, e339–e347. [Google Scholar] [CrossRef] [PubMed]
- Mundi, M.S.; Patel, J.J.; Martindale, R. Body Composition Technology: Implications for the ICU. Nutr. Clin. Pract. 2018, 34, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Velasco, I.T.; de Alencar, J.C.G.; Petrini, C.A. Procedimentos Com Ultrassom No Pronto Socorro, 1st ed.; Manole: Barueri, Brasil, 2021; pp. 3–11. [Google Scholar]
- Wagner, D.R. Ultrasound as a tool to assess body fat. J. Obes. 2013, 2013, 280713. [Google Scholar] [CrossRef]
- Prado, C.M.; Heymsfield, S.B. Lean tissue imaging: A new era for nutritional assessment and intervention. J. Parenter. Enter. Nutr. 2014, 38, 940–953. [Google Scholar] [CrossRef]
- Perkisas, S.; Baudry, S.; Bauer, J.; Beckeww, D.; De Cock, A.M.; Hobbelen, H.; Jager-Wittenaar, H.; Kasiukiewicz, A.; Landi, F.; Marco, E.; et al. Application of ultrasound for muscle assessment in sarcopenia: Towards standardized measurements. Eur. Geriatr. Med. 2018, 9, 739–757. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.W.; Ng, K.W.P.; Dietz, A.R.; Hartman, M.E.; Baty, J.D.; Hasan, N.; Zaidman, C.M.; Shoykhet, M. Muscle atrophy in mechanically-ventilated critically ill children. PLoS ONE 2018, 13, e0207720. [Google Scholar] [CrossRef]
- Ng, K.W.P.; Dietz, A.R.; Johnson, R.; Shoykhet, M.; Zaidman, C.M. Reliability of Bedside Ultrasound of Limb and Diaphragm Muscle Thickness in Critically Ill Children. Muscle Nerve 2019, 59, 88–94. [Google Scholar] [CrossRef]
- Montoro, D.V.; Camacho, V.R.; González, L.A.; Alonso, J.M.C. Thigh ultrasound monitoring identifies muscle atrophy in mechanically ventilated pediatric patients. Eur. J. Pediatr. 2023, 182, 65543–65551. [Google Scholar] [CrossRef]
- de Oliveira, J.K.; Schaan, C.W.; Silva, C.K.; Piva, T.C.; Sousa, I.T.; Bruno, F.; Lukrafka, J.L. Reliability of ultrasound in the assessment of muscle thickness in critically ill children. An. Pediatr. (Engl. Ed.) 2023, 98, 411–417. [Google Scholar] [CrossRef]
- de Figueiredo, R.S.; Nogueira, R.J.N.; Springer, A.M.M.; Melro, E.C.; Campos, N.B.; Batalha, R.E.; Brandão, M.B.; de Souza, T.H. Sarcopenia in critically ill children: A bedside assessment using point-of-care ultrasound and anthropometry. Clin. Nutr. 2021, 40, 4871–4877. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, S.A.; Elsawy, H.M.; Bazaraa, H.M.; Ghobashy, M.H.; Abd El Megied, A.A. Point of care ultrasonography of quadriceps femoris muscle thickness for assessing nutritional status in critically ill children. Sci. Rep. 2025, 15, 16946. [Google Scholar] [CrossRef] [PubMed]
- Gehad, M.H.; Yousif, Y.M.; Metwally, M.I.; AbdAllah, A.M.; Elhawy, L.L.; El-Shal, A.S.; Abdellatif, G.M. Utility of muscle ultrasound in nutritional assessment of children with nephrotic syndrome. Pediatr. Nephrol. 2023, 38, 1821–1829. [Google Scholar] [CrossRef] [PubMed]
- de Souza, R.P.; Donadio, M.V.F.; Heinzmann-Filho, J.P.; Baptista, R.R.; Pinto, L.A.; Epifanio, M.; Marostica, P.J.C. Uso da ultrassonografia para avaliar a espessura muscular e a gordura subcutânea em crianças e adolescentes com fibrose cística. Rev. Paul. Pediatr. 2018, 36, 457–465. [Google Scholar] [CrossRef]
- Lintz, V.C.; Vieira, R.A.; Carioca, F.L.; Ferraz, I.S.; Silva, H.M.; Ventura, A.M.C.; de Souza, D.C.; Brandão, M.B.; Nogueira, R.J.N.; de Souza, T.H. Fluid accumulation in critically ill children: A systematic review and meta-analysis. EClinicalMedicine 2024, 74, 102714. [Google Scholar] [CrossRef]
- Orsso, C.E.; Tibaes, J.R.; Oliveira, C.L.P.; Rubin, D.A.; Field, C.J.; Heymsfield, S.B.; Prado, C.M.; Haqq, A.M. Metabolic implications of low muscle mass in the pediatric population: A critical review. Metabolism 2019, 99, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Ventura, J.C.; Oliveira, L.D.D.A.; Silveira, T.T.; Hauschild, D.B.; Mehta, N.M.; Moreno, Y.M.F.; PICU-ScREEN Study Group. Admission factors associated with nutritional status deterioration and prolonged PICU stay in critically ill children: PICU-ScREEN multicenter study. J. Parenter. Enter. Nutr. 2021, 46, 330–338. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | USG Model | Parameters Evaluated | Key Findings | Transducer | Location/Measurement Point | Muscle Mass | Thickness |
|---|---|---|---|---|---|---|---|
| Valla (2017) [18] | Vivid S6/SonoSitand EDGE | Age, sex, weight, BMI, energy and protein intake, duration of MV, cachexia | QF thickness reduction: 9.8% (day 5) and 13.3% (final); good inter-rater reliability | Linear, 9–13 MHz | Thigh: widest portion measured from this point to the upper tip of the patella, perpendicular probe, minimal compression, supine position, 4 measurements (average), unilateral | QF thickness: femoral cortex to fascia | Median: 2.25 cm |
| Hoffman (2021) [12] | GE Logiq S8/Nextgen | Water balance, weight, nutritional intake | Reduction in QF thickness associated with caloric and protein deficiency; good reliability | Linear, 10 MHz or 4.2–13 MHz | Thigh: 2/3 anterior superior iliac spine of the patella, perpendicular probe, minimal compression, supine position, 4 measurements (average), unilateral | QF thickness: femoral cortex to fascia | 2.4 ± 0.56 cm |
| Johnson (2018) [24] | SonoSitand Edge II | Electrical impedance myography, clinical and demographic variables | Reduction: diaphragm 11.1% and QF 8.62%; 83% muscle atrophy; age and TBI → greater loss | Linear, 6–13 MHz | Diaphragm, biceps, QF, tibial: defined anatomical locations; minimal compression; supine position; 3 measurements (average), unilateral | Atrophy defined as ≥10% reduction; increased fat and reduced muscle quality | QF: ↓8.62% or 1.5%/day |
| Ng (2019) [25] | SonoSitand Edge II | Clinical and demographic variables | Correlation between muscle thickness and age and weight; atrophy: >13% limbs and >38% diaphragm | Linear, 6–13 MHz | Biceps, QF, tibial: maximum diameter; diaphragm: intercostal window; minimum compression; supine; 3 measurements (average), unilateral | Thickness: perpendicular to fascia/bones; diaphragm: between pleural layers | QFMT: 2.19 ± 0.89 cm |
| Montoro (2023) [26] | SonoSitand M-Turbo | Age, sex, BMI, energy and protein intake, duration of MV, neuromuscular blockers | QF thickness reduction: average 13% (1.57%/day); predictors: age, blockers, greater inflammation | Linear, 12 MHz | Thigh: midpoint of the anterior superior iliac spine of the patella; perpendicular probe; minimal compression; supine position; 3 measurements (average), unilateral | Thickness: femoral cortex to fascia | QFMT: 1.56 cm (median) |
| Oliveira (2023) [27] | InnoSight | Anthropometric and nutritional measurements | Reliable USG for muscle changes in UTIP | Linear, 4–12 MHz | Biceps, QF: anatomical locations; minimal compression; supine; 3 measurements (average) | Thickness defined by bone landmarks; assessment of muscle mass | Bíceps: 1.14 cm; QF: 1.85 cm |
| Souza (2018) [31] | DP 6600 Laptop | Anthropometric measurements, skinfold thickness, nutritional changes | USG correlated with skinfold thickness in the assessment of body fat | Linear, 7.5 MHz | Triceps, QF, gastrocnemius: anatomical landmarks; minimal compression; supine; unilateral | Thickness: distance between bone and muscle boundaries; subcutaneous fat | Triceps: 1.4 cm; QF: 2.4 cm; Gastrocnemius: 1.7 cm |
| Figueiredo (2021) [28] | Vivid Q | Anthropometry and nutritional supply | Significant reduction in QFMT in both subgroups; correlation with protein deficiency | Linear, 5–13 MHz | Thigh: 2/3 anterior superior iliac spine of the patella; maximum compression; supine; 3 measurements (average), unilateral | Thickness: from the upper margin of the femur to the deep fascia | Subgroup 1: 0.65 ± 0.23 cm; Subgroup 2: 0.63 ± 0.22 cm |
| Gehad (2022) [30] | Philips HD7xe | Age, sex, BMI, energy and protein intake, renal function | Smaller QRF and QVI muscles in the NS group; greater subcutaneous fat. | Linear, 7.5 MHz | Thigh: Measurement at the midpoint and at the border between the upper 2/3 and lower one-third of the line between the upper pole of the patella and the anterior superior iliac spine. | Maximum thickness measured from the inner edge of the muscle to the femur (QVI) and from the subcutaneous layer to the inner edge (QRF). | QRFT): NS group: 1.088 cm Control group: 1.27 cm (QVIT): NS group: 0.999 cm Control group: 1.138 cm. |
| Mohamed (2025) [29] | GE Logiq S8 | Age, gender, BMI, medical history, diet, use of supplements, anthropometry, duration of VM, tests. | Significant reduction in QFMT on days 3 and 7 after admission, correlation between nutritional intake and QFMT thickness, muscle atrophy associated with longer hospital stays and unfavorable outcomes. | Linear 11 MHz | Thigh: 2/3 anterior superior iliac spine of the patella; perpendicular probe, maximum compression, supine position, 3 measurements (average), unilateral | Thickness: distance between the upper edge of the muscle and the cortex of the femur. | QFMT: 0.97 ± 0.40 cm (0.43–2.5 cm) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farias, P.M.; Melo, A.M.L.; da Costa, A.A.; Nascimento, V.A.d.; Pott, A.; Guimarães, R.d.C.A.; Freitas, K.d.C. Use of Ultrasound for Body Composition in Assessment in Pediatric Patients: Are There Still Challenges? Diagnostics 2025, 15, 2472. https://doi.org/10.3390/diagnostics15192472
Farias PM, Melo AML, da Costa AA, Nascimento VAd, Pott A, Guimarães RdCA, Freitas KdC. Use of Ultrasound for Body Composition in Assessment in Pediatric Patients: Are There Still Challenges? Diagnostics. 2025; 15(19):2472. https://doi.org/10.3390/diagnostics15192472
Chicago/Turabian StyleFarias, Patricia Miranda, Amanda Matos Lima Melo, Aryanne Almeida da Costa, Valter Aragão do Nascimento, Arnildo Pott, Rita de Cássia Avellaneda Guimarães, and Karine de Cássia Freitas. 2025. "Use of Ultrasound for Body Composition in Assessment in Pediatric Patients: Are There Still Challenges?" Diagnostics 15, no. 19: 2472. https://doi.org/10.3390/diagnostics15192472
APA StyleFarias, P. M., Melo, A. M. L., da Costa, A. A., Nascimento, V. A. d., Pott, A., Guimarães, R. d. C. A., & Freitas, K. d. C. (2025). Use of Ultrasound for Body Composition in Assessment in Pediatric Patients: Are There Still Challenges? Diagnostics, 15(19), 2472. https://doi.org/10.3390/diagnostics15192472





