Circadian Rhythm and Psychiatric Features in Wolfram Syndrome: Toward Chrono Diagnosis and Chronotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. First Stage: Scoping Review
2.2. Second Stage—Evaluation of Executive Functions Using DEX
2.3. Rationale for Methodology
2.4. Search Strategy
2.5. Quality Assessment
2.6. Instrument Characteristics: Dysexecutive Questionnaire (DEX)
2.7. Ethics Considerations
3. Results
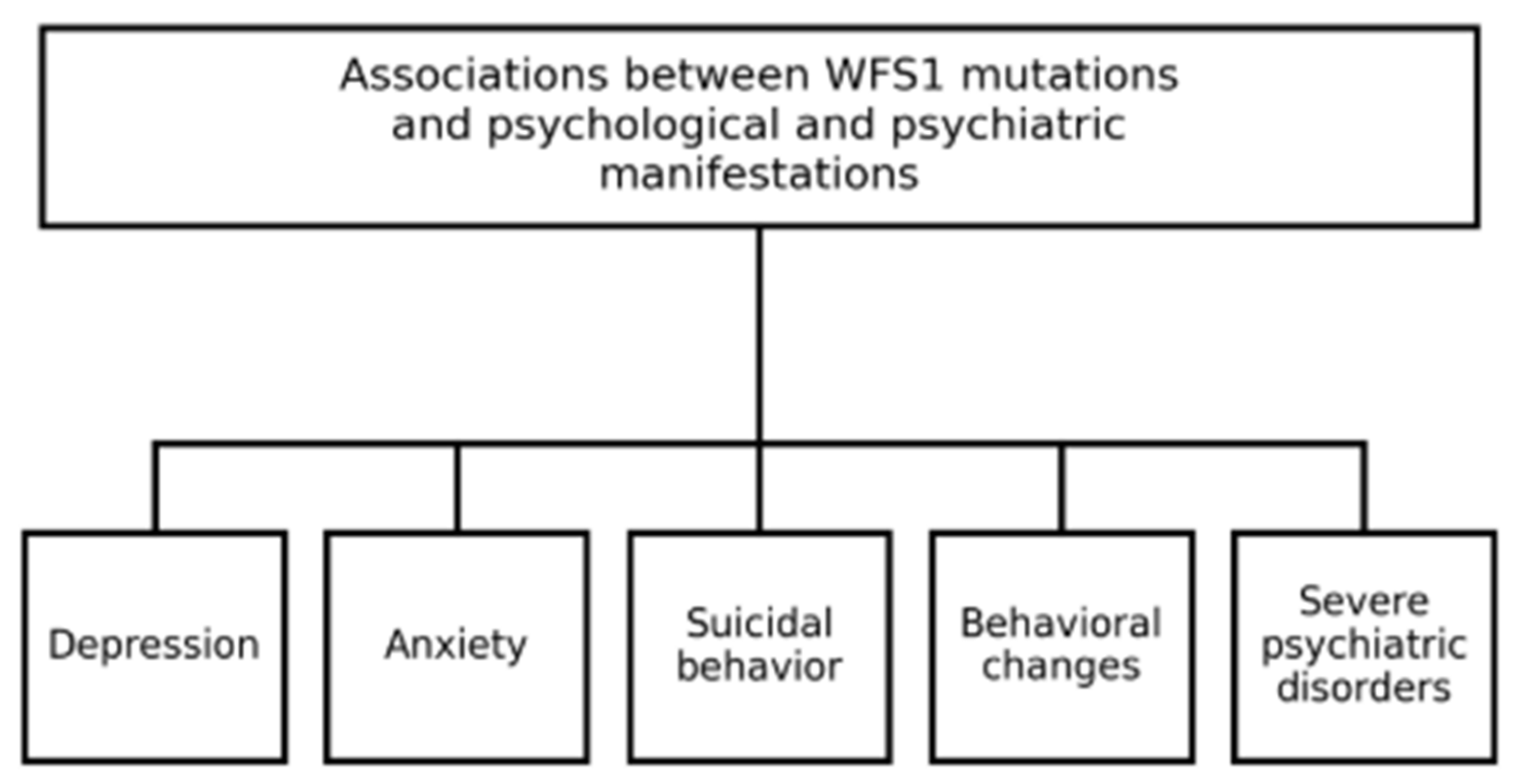
3.1. Functional Category 1—Anxiety and Depression Disorders
3.2. Functional Category 2—Suicidal and Aggressive Behaviors
3.3. Functional Category 3—Severe Psychological and Psychiatric Disorders
3.4. Functional Category 4—Chronic Fatigue Syndrome
3.5. Results of Data DEX
3.5.1. IQ Bands
3.5.2. DEX Reporting Strategy
3.5.3. Highest-Scoring Items
3.5.4. Lowest-Scoring Items
3.5.5. Analysis by DEX Categories
- ▪
- Inhibition (memory/understanding) (Table 7)
| DEX Item | 1 | 3 | 8 | 13 | 14 | 19 |
|---|---|---|---|---|---|---|
| mean | 1.94 | 1.49 | 2.03 | 1.84 | 1.99 | 1.99 |
| std | 1.25 | 0.88 | 1.30 | 1.31 | 1.22 | 1.10 |
- ▪
- Intention (Table 8)
| DEX Item | 6 | 9 | 11 | 12 | 15 | 16 |
|---|---|---|---|---|---|---|
| mean | 1.72 | 1.30 | 1.99 | 1.99 | 2.80 | 1.89 |
| std | 1.02 | 0.63 | 1.15 | 1.14 | 1.34 | 1.20 |
- ▪
- Executive memory (Table 9)
| DEX Item | 2 | 4 | 5 | 7 | 10 | 17 |
|---|---|---|---|---|---|---|
| mean | 2.05 | 1.70 | 1.94 | 1.72 | 1.77 | 1.87 |
| std | 1.28 | 1.11 | 1.16 | 1.11 | 1.04 | 1.18 |
- ▪
- Positive affect (Table 10)
| DEX Item | 18 | 20 |
|---|---|---|
| mean | 2.27 | 1.80 |
| std | 1.37 | 1.08 |
- Most affected domains: Attention (Item 18, M = 2.27), hyperactivity/impulsivity (Items 15, M = 2.29; 2, M = 2.05), and decision-making/behavioral regulation (Items 14 & 19, ~M = 1.99).
- Moderately affected domains: Emotional regulation (difficulty expressing or controlling emotions, Items 11–12) and motivation/initiative (lethargy, losing interest, Items 8 & 10).
- Least affected domains: Social awareness and planning (Items 3, 4, 7, 9, 13, 20), generally showing low means, though with occasional higher scores in some individuals.
3.6. Prefrontal Symptoms Assessment
4. Discussion
4.1. Hypotheses and Future Directions
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Esteban Bueno, G.; Fernández Martínez, J.L. Gonadal Dysfunction in Wolfram Syndrome: A Prospective Study. Diagnostics 2025, 15, 1594. [Google Scholar] [CrossRef]
- Hardy, C.; Khanim, F.; Torres, R.; Scott-Brown, M.; Seller, A.; Poulton, J.; Collier, D.; Kirk, J.; Polymeropoulos, M.; Latif, F.; et al. Clinical and molecular genetic analysis of 19 Wolfram syndrome kindreds demonstrating a wide spectrum of mutations in WFS1. Am. J. Hum. Genet. 1999, 65, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Bueno, G.E.; Ruiz-Castañeda, D.; Martínez, J.R.; Muñoz, M.R.; Alascio, P.C. Natural history and clinical characteristics of 50 patients with Wolfram syndrome. Endocrine 2018, 61, 440–446. [Google Scholar] [CrossRef]
- Esteban-Bueno, G.; Berenguel Hernández, A.M.; Fernández Fernández, N.; Navarro Cabrero, M.; Coca, J.R. Neurosensory Affectation in Patients Affected by Wolfram Syndrome: Descriptive and Longitudinal Analysis. Healthcare 2023, 11, 1888. [Google Scholar] [CrossRef]
- Bischoff, A.N.; Reiersen, A.M.; Buttlaire, A.; Al-Lozi, A.; Doty, T.; Marshall, B.A.; Hershey, T. Washington University Wolfram Syndrome Research Group. Selective cognitive and psychiatric manifestations in Wolfram Syndrome. Orphanet J. Rare Dis. 2015, 10, 66. [Google Scholar] [CrossRef] [PubMed]
- Swift, R.G.; Sadler, D.B.; Swift, M. Psychiatric findings in Wolfram syndrome homozygotes. Lancet 1990, 336, 667–669. [Google Scholar] [CrossRef]
- Reiersen, A.M.; Narayanan, A.; Sinkre, R.A.; Hershey, T. Psychiatric diagnoses and treatment in Wolfram Syndrome. J. Am. Acad. Child. Adolesc. Psychiatry 2019, 58, S188–S189. [Google Scholar] [CrossRef]
- Swift, M.; Gorman Swift, R. Psychiatric disorders and mutations at the Wolfram syndrome locus. Biol. Psychiatry 2000, 47, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Wilson, B.A.; Alderman, N.; Burgess, P.W.; Emslie, H.; Evans, J.J. Behavioural Assessment of the Dysexecutive Syndrome; Thames Valley Test Company: Suffolk, UK, 1996. [Google Scholar]
- Gerstorf, D.; Siedlecki, K.L.; Tucker-Drob, E.M.; Salthouse, T.A. Executive dysfunctions across adulthood: Measurement properties and correlates of the DEX self-report questionnaire. Aging Neuropsychol. Cogn. 2008, 15, 424–445. [Google Scholar] [CrossRef]
- Fonseca, S.G.; Fukuma, M.; Lipson, K.L.; Nguyen, L.X.; Allen, J.R.; Oka, Y.; Urano, F. WFS1 is a novel component of the unfolded protein response and maintains homeostasis of the endoplasmic reticulum in pancreatic β-cells. J. Biol. Chem. 2005, 280, 39609–39615. [Google Scholar] [CrossRef]
- Hao, H.; Song, L.; Zhang, L. Wolfram syndrome 1 regulates sleep in dopamine receptor neurons by modulating calcium homeostasis. PLoS Genet. 2023, 19, e1010827. [Google Scholar] [CrossRef]
- Ferreras, C.; Gorito, V.; Pedro, J.; Ferreira, S.; Costa, C.; Santos Silva, R.; Correia, C.C. Wolfram syndrome: Portuguese research. Endokrynol. Pol. 2021, 72, 353–356. [Google Scholar] [CrossRef] [PubMed]
- Pedrero-Pérez, E.J.; Ruiz-Sánchez de León, J.M.; Rojo-Mota, G.; Llanero-Luque, M.; Olivar-Arroyo, A.; Bouso-Saiz, J.C.; Puerta-García, C. Versión española del Cuestionario Disejecutivo (DEX-Sp): Propiedades psicométricas en adictos y población no clínica. Adicciones 2009, 21, 155–166. [Google Scholar] [CrossRef]
- Uhlenbusch, N.; Löwe, B.; Depping, M.K. Correlates of depression and anxiety in patients with different rare diseases. J. Psychosom. Res. 2018, 109, 142. [Google Scholar] [CrossRef]
- Uhlenbusch, N.; Löwe, B.; Härter, M.; Schramm, C.; Weiler-Normann, C.; Depping, M.K. Depression and anxiety in patients with different rare chronic diseases: A cross-sectional study. PLoS ONE 2019, 14, e0211343. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.; Cedres, L.; Vomero, A.; Tapie, A.; Rodríguez, S.; Raggio, V.; Feder, S.; García, L. Síndrome de Wolfram. Rev. Esp. Endocrinol. Pediatr. 2019, 10, 74–80. [Google Scholar] [CrossRef]
- Welschen, D.; Peralta Alejandro, M.C.; Arroyo Yllanes, M.E.; Fonte-Vázquez, A. Síndrome de Wolfram: Reporte de casos. Oftalmol. Clin. Exp. 2015, 8, 29–38. [Google Scholar]
- Ferreira, V.F.S.; Campos, C.R.; Furtado, A.M.; Caixeta, L.F.; Caixeta, M.; Aversi-Ferreira, T.A. Wolfram syndrome: A case report. Res. Soc. Dev. 2021, 10, e52410616116. [Google Scholar] [CrossRef]
- Nanko, S.; Yokoyama, H.; Hoshino, Y.; Kumashiro, H.; Mikuni, M. Organic mood syndrome in two siblings with Wolfram syndrome. Br. J. Psychiatry 1992, 161, 282. [Google Scholar] [CrossRef]
- Swift, R.G.; Perkins, D.O.; Chase, C.L.; Rush, A.J.; Amador, X. Psychiatric disorders in 36 families with Wolfram syndrome. Am. J. Psychiatry 1991, 148, 775–779. [Google Scholar] [CrossRef]
- Xavier, J.; Bourvis, N.; Tanet, A.; Perisse, D. Bipolar Disorder Type 1 in a 17-Year-Old Girl with Wolfram Syndrome. J. Child. Adolesc. Psychopharmacol. 2016, 26, 750–755. [Google Scholar] [CrossRef]
- Chatterjee, S.S.; Mitra, S.; Pal, S.K. Mania in Wolfram’s disease: From bedside to bench. Clin. Psychopharmacol. Neurosci. 2017, 15, 70–72. [Google Scholar] [CrossRef][Green Version]
- Sequeira, A.; Kim, C.; Seguin, M.; Lesage, A.; Chawky, N.; Desautels, A.; Tousignant, M.; Vanier, C.; Lipp, O.; Benkelfat, C. Wolfram syndrome and suicide: Evidence for a role of WFS1 in suicidal and impulsive behavior. Am. J. Med. Genet. B Neuropsychiatr. Genet 2003, 119, 108–113. [Google Scholar] [CrossRef]
- Nickl-Jockschat, T.; Kunert, H.J.; Herpertz-Dahlmann, B.; Grözinger, M. Psychiatric symptoms in a patient with Wolfram syndrome caused by a combination of thalamic deficit and endocrinological pathologies. Neurocase 2008, 15, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Swift, M.; Gorman Swift, R. Wolframin mutations and hospitalization for psychiatric illness. Mol. Psychiatry 2005, 10, 799–803. [Google Scholar] [CrossRef]
- Owen, M.J. Psychiatric disorders in Wolfram syndrome heterozygotes. Mol. Psychiatry 1998, 3, 12–13. [Google Scholar] [CrossRef][Green Version]
- Rigoli, L.; Caruso, V.; Aloi, C.; Salina, A.; Maghnie, M.; d’Annunzio, G.; Lamacchia, O.; Salzano, G.; Lombardo, F.; Picca, G. An Atypical Case of Late-Onset Wolfram Syndrome 1 without Diabetes Insipidus. Int. J. Environ. Res. Public Health 2022, 19, 2473. [Google Scholar] [CrossRef]
- Kitamura, R.A.; Maxwell, K.G.; Ye, W.; Kries, K.; Brown, C.M.; Augsornworawat, P.; Hirsch, Y.; Johansson, M.M.; Weiden, T.; Ekstein, J. Multidimensional analysis and therapeutic development using patient iPSC-derived disease models of Wolfram syndrome. JCI Insight 2022, 7, e156549. [Google Scholar] [CrossRef]
- Rosanio, F.M.; Di Candia, F.; Occhiati, L.; Fedi, L.; Malvone, F.P.; Foschini, D.F.; Franzese, A.; Mozzillo, E. Wolfram Syndrome Type 2: A Systematic Review of a Not Easily Identifiable Clinical Spectrum. Int. J. Environ. Res. Public Health 2022, 19, 835. [Google Scholar] [CrossRef] [PubMed]
- Cairns, G.; Burté, F.; Price, R.; O’Connor, E.; Toms, M.; Mishra, R.; Moosajee, M.; Pyle, A.; Sayer, J.A.; Yu-Wai-Man, P. A mutant wfs1 zebrafish model of Wolfram syndrome manifesting visual dysfunction and developmental delay. Sci. Rep. 2021, 11, 20491. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, X.; Shi, L. Wolfram syndrome 1b mutation suppresses Mauthner cell axon regeneration via ER stress signal pathway. Acta Neuropathol. Commun. 2022, 10, 184. [Google Scholar] [CrossRef] [PubMed]
- Panfili, E.; Mondanelli, G.; Orabona, C.; Belladonna, M.L.; Gargaro, M.; Fallarino, F.; Orecchini, E.; Prontera, P.; Proietti, E.; Frontino, G.; et al. Novel mutations in the WFS1 gene are associated with Wolfram syndrome and systemic inflammation. Hum. Mol. Genet. 2021, 30, 265–276. [Google Scholar] [CrossRef]
- de Muijnck, C.; ten Brink, J.B.; Bergen, A.A.; Boon, C.J.F.; van Genderen, M.M. Delineating Wolfram-like syndrome: A systematic review and discussion of the WFS1-associated disease spectrum. Surv. Ophthalmol. 2023, 68, 641–654. [Google Scholar] [CrossRef]
- Salzano, G.; Rigoli, L.; Valenzise, M.; Chimenz, R.; Passanisi, S.; Lombardo, F. Clinical Peculiarities in a Cohort of Patients with Wolfram Syndrome 1. Int. J. Environ. Res. Public Health 2022, 19, 520. [Google Scholar] [CrossRef] [PubMed]
- Reiersen, A.M.; Noel, J.S.; Doty, T.; Sinkre, R.A.; Narayanan, A.; Hershey, T. Psychiatric Diagnoses and Medications in Wolfram Syndrome. Scand. J. Child. Adolesc. Psychiatr. Psychol. 2022, 10, 163–174. [Google Scholar] [CrossRef]
- Llanero-Luque, M.; Ruiz-Sánchez de León, J.M.; Pedrero-Pérez, E.J.; Olivar-Arroyo, A.; Bouso-Saiz, J.C.; Rojo-Mota, G.; Puerta-García, C. Sintomatología disejecutiva en adictos a sustancias en tratamiento mediante la versión española del cuestionario disejecutivo (DEX-Sp). Rev. Neurol. 2008, 47, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Hershey, T.; Lugar, H.M.; Shimony, J.S.; Rutlin, J.; Koller, J.M.; Perantie, D.C.; Paciorkowski, A.R.; Eisenstein, S.A.; Permutt, M.A.; Washington University Wolfram Study Group. Early brain vulnerability in Wolfram syndrome. PLoS ONE 2012, 7, e40604. [Google Scholar] [CrossRef]
- Shi, G.; Cui, L.; Chen, R.; Liang, S.; Wang, C.; Wu, P. TT01001 attenuates oxidative stress and neuronal apoptosis by preventing mitoNEET-mediated mitochondrial dysfunction after subarachnoid hemorrhage in rats. Neuroreport 2020, 31, 845–850. [Google Scholar] [CrossRef]
- Morikawa, S.; Blacher, L.; Onwumere, C.; Urano, F. Loss of Function of WFS1 Causes ER Stress Mediated Inflammation in Pancreatic Beta Cells. Front. Endocrinol. 2022, 13, 849204. [Google Scholar] [CrossRef]
- Low, R.N.; Low, R.J.; Akrami, A. A review of cytokine-based pathophysiology of Long COVID symptoms. Front. Med. 2023, 10, 1011936. [Google Scholar] [CrossRef]
- Paulsen, J.S. Cognitive impairment in Huntington disease: Diagnosis and treatment. Curr. Neurol. Neurosci. Rep. 2011, 11, 474–483. [Google Scholar] [CrossRef] [PubMed]
- Orellana, G.; Slachevsky, A. Executive functioning in schizophrenia. Front. Psychiatry 2013, 4, 35. [Google Scholar] [CrossRef] [PubMed]
- Szablewski, L. Associations Between Diabetes Mellitus and Neurodegenerative Diseases. Int. J. Mol. Sci. 2025, 26, 542. [Google Scholar] [CrossRef]
- Caruso, V.; Rigoli, L. Beyond Wolfram Syndrome 1: The WFS1 Gene’s Role in Alzheimer’s Disease and Sleep Disorders. Biomolecules 2024, 14, 1389. [Google Scholar] [CrossRef] [PubMed]
- Quittner, A.L.; Goldbeck, L.; Abbott, J.; Duff, A.; Lambrecht, P.; Solé, A. Prevalence of depression and anxiety in patients with cystic fibrosis and parent caregivers. Thorax 2014, 69, 1090–1097. [Google Scholar] [CrossRef]
- Cassidy, S.B.; Schwartz, S.; Miller, J.L.; Driscoll, D.J. Prader-Willi syndrome. Genet. Med. 2012, 14, 10–26. [Google Scholar] [CrossRef]
- Visnapuu, T.; Raud, S.; Loomets, M.; Reimets, R.; Sütt, S.; Luuk, H.; Plaas, M.; Kõks, S.; Volke, V.; Alttoa, A.; et al. Wfs1-deficient mice display altered function of serotonergic system and increased behavioral response to antidepressants. Front. Neurosci. 2013, 7, 132. [Google Scholar] [CrossRef]
- Licis, A.; Davis, G.; Eisenstein, S.A.; Lugar, H.M.; Hershey, T. Sleep disturbances in Wolfram syndrome. Orphanet J. Rare Dis. 2019, 14, 188. [Google Scholar] [CrossRef]
- Serino, M.; Amorim, P.; Pimentel, A.; Viana, P.; Pereira, J.M.; van Zeller, M. Images in sleep medicine: Sleep-disordered breathing in Wolfram’s syndrome—A near-fatal event. Sleep. Med. 2024, 124, 106–109. [Google Scholar] [CrossRef]
- Michalsky, T. Metacognitive scaffolding for preservice teachers’ self-regulated design of higher order thinking tasks. Heliyon 2024, 10, e24280. [Google Scholar] [CrossRef]
- Mirhosseini, S.; Imani-Parsa, F.; Moghadam Roshtkhar, H.; Basirinezhad, M.H.; Ameri, M.; Ebrahimi, H. Support based on psychoeducation intervention to address quality of life and care burden among caregivers of patients with cancer. Front. Psychol. 2025, 16, 1430371. [Google Scholar] [CrossRef]
- Pozuelos, J.P.; Combita, L.M.; Abundis, A.; Paz-Alonso, P.M.; Conejero, Á.; Guerra, S.; Rueda, M.R. Metacognitive scaffolding boosts cognitive and neural benefits following executive attention training in children. Dev. Sci. 2019, 22, e12756. [Google Scholar] [CrossRef] [PubMed]
- Atkins, J.C.; Padgett, C.R. Living with a Rare Disease: Psychosocial Impacts for Parents and Family Members—A Systematic Review. J. Child. Fam. Stud. 2024, 33, 617–636. [Google Scholar] [CrossRef]
- Majander, A.; Jurkute, N.; Burté, F.; Brock, K.; João, C.; Huang, H.; Neveu, M.M.; Chan, C.M.; Duncan, H.J.; Kelly, S.; et al. WFS1-Associated Optic Neuropathy: Genotype-Phenotype Correlations and Disease Progression. Am. J. Ophthalmol. 2022, 241, 9–27. [Google Scholar] [CrossRef] [PubMed]

| No. | Study Design | Sample Size | Control Group | Methodology | Reliability and Rigor Assessment |
|---|---|---|---|---|---|
| [5] | Exp. | n = 19 | Yes (n = 50) | Multiple standardized cognitive and psychiatric tests | High reliability. Small sample |
| [7] | Exp. | n = 39 | No | Questionnaires and interviews | High reliability and rigor. Medium sample |
| [8] | Retr. | n = 68 | No | Follow-up of previous study | Moderate reliability. No new data collected |
| [11] | Exp. | N/A | No | Molecular method | High reliability. No human sample |
| [13] | Retr. | n = 11 | No | Clinical data review | Medium reliability. Small sample and no control group |
| [15] | Retr. | n = 790 | No | Cross-sectional study | High reliability. Large sample but no control group |
| [16] | Retr. | n = 300 | No | Correlational analysis | High reliability. Large sample but no control group |
| [17] | CR | n = 1 | No | Clinical case description | Moderate reliability. Single case limits generalizability |
| [18] | CR | n = 1 | No | Clinical case description | Moderate reliability. Single case limits generalizability |
| [19] | CR | n = 1 | No | Clinical case description | Moderate reliability. Single case limits generalizability |
| [20] | CR | n = 2 | No | Clinical case description | Moderate reliability. Small sample and no control group |
| [21] | Exp. | n = 36 | Yes (spouses) | Questionnaires | High reliability. Control group (spouses) provides some comparison |
| [22] | CR | n = 1 | No | WAIS-III and clinical observation | Moderate reliability. Single case limits generalizability |
| [23] | CR | n = 1 | No | Clinical observation | Moderate reliability. Single case limits generalizability |
| [24] | Exp. | n = 111 | Yes (n = 129) | Post-mortem genetic analysis | High reliability. Control group and genetic analysis |
| [25] | CR | n = 1 | No | WAIS and WMS tests | Moderate reliability. Single case limits generalizability |
| [26] | Exp. | n = 25 | No | Questionnaires and interviews | Moderate reliability. Small sample and no control group |
| [27] | Review | N/A | No | Literature review | Moderate reliability. No original data |
| [28] | CR | n = 1 | No | Clinical case description | Moderate reliability. Single case limits generalizability |
| [29] | Exp. | N/A | No | iPSC-derived models | Innovative method but no human sample |
| [30] | Review | N/A | No | Literature review | Comprehensive but no original data |
| [31] | Exp. | N/A | No | Zebrafish model | Animal model limits human applicability |
| [32] | Exp. | N/A | No | Genetic and cellular analysis | Moderate reliability. Focus on molecular mechanisms |
| [33] | Exp./Case | n = 1 | No | Genetic and clinical analysis | Moderate reliability. Single case limits generalizability |
| [34] | Review | n = 86 | No | Literature review | Moderate reliability. Comprehensive but no original data. |
| [35] | Retr. | n = 14 | No | Clinical data review | Small sample and no control group |
| [36] | Long. | n = 39 | Yes | Structured interviews and CASI-5 | High reliability. Control group and standardized measures. |
| Category | Summary | References |
|---|---|---|
| Severe psychological and psychiatric disorders | Includes the presence of psychiatric conditions such as depression, anxiety, and bipolar disorder. These papers examine potential biological, genetic, and neurological links. Also, addresses cognitive deficits, neurodegeneration, and neuropsychiatric changes in WS, and their impact on daily function and disease progression | [5,6,7,22,24,27,32,36] |
| Suicidal and aggressive behaviors | WS has been linked on different papers to an increased risk of suicidal and aggressive behaviors | [5,24,27,30,36] |
| Anxiety and depression disorders | Studies examines anxiety and depressive disorders in individuals with WS and other rare diseases, focusing on the psychological burden of chronic progressive conditions | [13,14] |
| Characteristic | Value |
|---|---|
| N (total) | 28 |
| Sex: Women, n (%) | 13 (46.4) |
| Sex: Men, n (%) | 15 (53.6) |
| Age, mean (SD) | 24.4 (9.7) |
| IQ band: High, n (%) | 13 (46.4) |
| IQ band: Normal, n (%) | 9 (32.1) |
| IQ band: Low-average, n (%) | 4 (14.3) |
| IQ band: Low/borderline, n (%) | 1 (3.6) |
| IQ band: Intellectual disability, n (%) | 1 (3.6) |
| Education: Higher education, n (%) | 9 (32.1) |
| Education: Basic education, n (%) | 9 (32.1) |
| Education: Middle-level, n (%) | 3 (10.7) |
| Education: Age-appropriate level, n (%) | 4 (14.3) |
| Education: Medium-level, n (%) | 2 (7.1) |
| Measure | DEX Total Score |
|---|---|
| Mean | 30.43 |
| SD | N/A |
| Median | 22.50 (approx.) |
| IQR (Q1–Q3) | 20.00–32.25 (approx.) |
| Min | ≥20.00 (bound) |
| Max | ≤70.00 (bound) |
| Question | Executive Dimension | Mean |
|---|---|---|
| 15 | Hyperactivity and restlessness | 2.80 |
| 18 | Difficulties in maintaining attention | 2.27 |
| 2 | Impulsivity (acting without thinking) | 2.05 |
| 8 | Lack of enthusiasm/apathy | 2.03 |
| 11, 12, 14, 19 | Difficulty in showing emotions, anger, repetitive behaviors, indecisiveness | 1.99 |
| 17,16 | Inconsistency between what is said and what is done | 1.89, 1.87 |
| Question | Executive Dimension | Mean |
|---|---|---|
| 9 | Embarrassing behavior toward others | 1.30 |
| 3 | Confusion with reality (false memories) | 1.49 |
| 4 | Future planning | 1.70 |
| 6, 7 | Confusion between events | 1.72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esteban-Bueno, G.; Jiménez-Soto, A.; Fernández-Martínez, J.L.; Fernández-Vilas, E.; Coca, J.R. Circadian Rhythm and Psychiatric Features in Wolfram Syndrome: Toward Chrono Diagnosis and Chronotherapy. Diagnostics 2025, 15, 2338. https://doi.org/10.3390/diagnostics15182338
Esteban-Bueno G, Jiménez-Soto A, Fernández-Martínez JL, Fernández-Vilas E, Coca JR. Circadian Rhythm and Psychiatric Features in Wolfram Syndrome: Toward Chrono Diagnosis and Chronotherapy. Diagnostics. 2025; 15(18):2338. https://doi.org/10.3390/diagnostics15182338
Chicago/Turabian StyleEsteban-Bueno, Gema, Annabel Jiménez-Soto, Juan Luis Fernández-Martínez, Enrique Fernández-Vilas, and Juan R. Coca. 2025. "Circadian Rhythm and Psychiatric Features in Wolfram Syndrome: Toward Chrono Diagnosis and Chronotherapy" Diagnostics 15, no. 18: 2338. https://doi.org/10.3390/diagnostics15182338
APA StyleEsteban-Bueno, G., Jiménez-Soto, A., Fernández-Martínez, J. L., Fernández-Vilas, E., & Coca, J. R. (2025). Circadian Rhythm and Psychiatric Features in Wolfram Syndrome: Toward Chrono Diagnosis and Chronotherapy. Diagnostics, 15(18), 2338. https://doi.org/10.3390/diagnostics15182338









