A Predictive Score Incorporating Clinical, Radiologic, and Hormonal Parameters to Discriminate Lymphocytic Hypophysitis from Non-Functioning Pituitary Macroadenomas
Abstract
1. Introduction
2. Methods
2.1. Study Population and Group Definition
- -
- Group 1 (G1): NFPMA group. All patients in this group underwent surgical resection of their NFPMA, with histological and immunohistochemical confirmation of its non-secreting nature.
- -
- Group 2 (G2): Hypophysitis group. The diagnosis of hypophysitis was established either histopathologically on surgical specimens from sellar surgery or based on clinical, biological, and radiological criteria suggestive of INH, panhypophysitis, or AH. A presumptive non-surgical diagnosis of hypophysitis was made based on suggestive clinical findings, partial or complete anterior pituitary deficiency, evocative imaging findings, and favorable response to corticosteroid therapy. The simultaneous involvement of both adenohypophysis and neurohypophysis was highly suggestive of an inflammatory etiology.
2.2. Sample Size and Patient Inclusion
- n = sample size;
- z = confidence level (1.96 for 95% confidence);
- p = prevalence of NFPMA in the general population;
- i = margin of error (5%).
2.3. Selection of Study Criteria
2.3.1. Clinical Criteria:
- -
- Demographics: Age (<30 years vs. ≥30 years), sex, pregnancy status (ongoing pregnancy or recent delivery ≤2 weeks postpartum).
- -
- Medical history: Autoimmune diseases, vasculitis, systemic inflammatory diseases, neoplastic or granulomatous conditions.
- -
- Tumor syndrome: Headaches, visual symptoms (decreased visual acuity, bitemporal hemianopsia, homonymous lateral hemianopsia (HLH), ophthalmoplegia, or blindness).
- -
- Signs of anterior pituitary insufficiency, hyperprolactinemia, or central diabetes insipidus (CDI).
2.3.2. Biological Criteria:
- -
- Elevated C-reactive protein (CRP > 10 mg/dL), increased erythrocyte sedimentation rate (ESR > 15 mm/h in men and >20 mm/h in women < 50 years; >20 mm/h in men and >30 mm/h in women ≥ 50 years), leukocytosis (>10,000/mm3).
- -
- Anterior pituitary insufficiency: Assessment of corticotropic (Adrenocorticotropic Hormone (ACTH) and 8 AM cortisol; Synacthen test if needed), somatotropic (Insulin-like Growth Factor 1 (IGF-1) and Growth Hormone (GH) stimulation test), gonadotropic (Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), estradiol/testosterone), thyrotropic (Thyroid-Stimulating Hormone (TSH), Free Thyroxine T4 (FT4)), lactotropic (Prolactin (PRL)), and neurohypophyseal function (water deprivation test in suspected CDI).
- -
- Hyperprolactinemia: PRL > 20 ng/mL in men and >40 ng/mL in women; PRL < 200 ng/mL suggests a disconnection hyperprolactinemia.
2.3.3. Imaging Criteria: Magnetic Resonance Imaging:
- -
- -
- Signal intensity on T1- and T2-weighted images.
- -
- Enhancement pattern (intense, homogeneous).
- -
- Symmetry of the pituitary mass.
- -
- Absence of the posterior pituitary bright spot.
- -
- Ectopic Antidiuretic Hormone (ADH) storage.
- -
- Pituitary stalk thickening (>4 mm at the optic chiasm/median eminence or >3 mm at the pituitary insertion [15]).
- -
- -
- Compression of the optic pathways.
- -
- Presence of a pseudocapsule
- -
- -
- Sphenoidal sinus mucosal thickening.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACTH | Adrenocorticotropic Hormone |
| ADH | Antidiuretic Hormone, |
| AH | Adenohypophysitis |
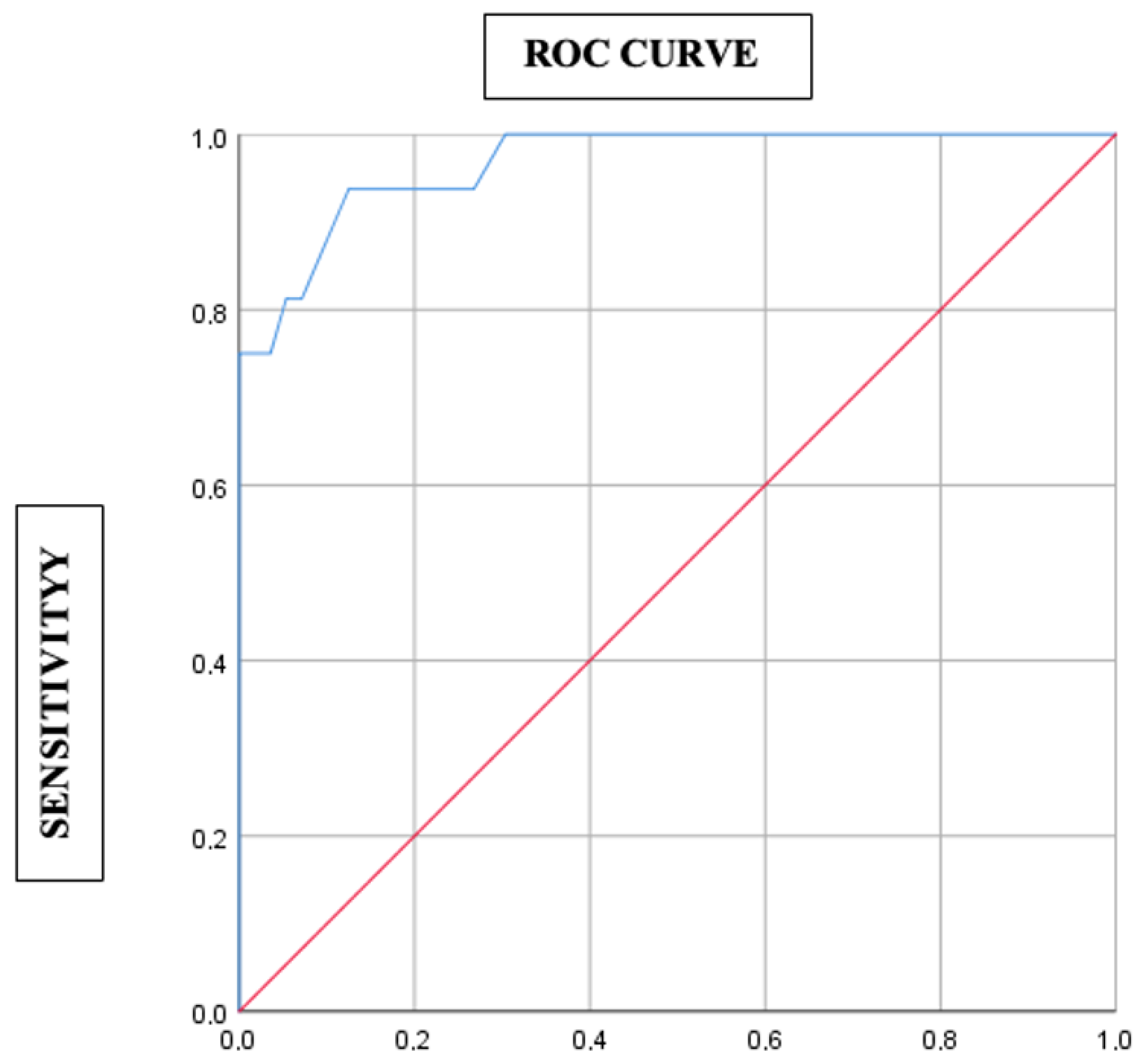
| AUC | Area Under the Curve |
| CDI | Central Diabetes Insipidus |
| CI | Confidence Interval |
| CRP | C-reactive Protein |
| ESR | Erythrocyte Sedimentation Rate |
| FSH | Follicle-Stimulating Hormone |
| FT4 | Free Thyroxine T4 |
| G1 | Group 1 |
| G2 | Group 2 |
| GH | Growth Hormone |
| HLH | Homonymous Lateral Hemianopsia |
| IGF1 | Insulin-like Growth Factor 1 |
| INH | Infundibulo-neurohypophysitis |
| IRMA | ImmunoRadioMetric Assay |
| LH | Luteinizing Hormone |
| MRI | Magnetic Resonance Imaging |
| NFPMA | Non-Functioning Pituitary Macroadenomas |
| OR | Odds Ratio |
| PA | Pituitary Adenomas |
| PRL | Prolactin |
| RIA | RadioImmunoAssay |
| ROC | Receiver Operating Characteristic |
| TSH | Thyroid-Stimulating Hormon |
References
- Burns, J.; Hsu, K.; Shifteh, K.; Erdfarb, A.J. Neuroendocrine Imaging. Adv. Clin. Radiol. 2019, 1, 151–170. [Google Scholar] [CrossRef]
- Perosevic, M.; Jones, P.S.; Tritos, N.A. Magnetic resonance imaging of the hypothalamo-pituitary region. In Handbook of Clinical Neurology; The Human Hypothalamus: Anterior Region; Elsevier: Amsterdam, The Netherlands, 2021; pp. 95–112. [Google Scholar] [CrossRef]
- Jipa, A.; Jain, V. Imaging of the sellar and parasellar regions. Clin. Imaging 2021, 77, 254–275. [Google Scholar] [CrossRef]
- Ntali, G.; Wass, J.A. Epidemiology, clinical presentation and diagnosis of non-functioning pituitary adenomas. Pituitary 2018, 21, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Langlois, F.; Varlamov, E.V.; Fleseriu, M. Hypophysitis, the growing spectrum of a rare pituitary disease. J. Clin. Endocrinol. Metab. 2022, 107, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Fontana, E.; Gaillard, R. Epidemiology of pituitary adenoma: Results of the first Swiss study. Rev. Med. Suisse 2009, 5, 2172–2174. [Google Scholar] [PubMed]
- Fernandez, A.; Karavitaki, N.; Wass, J.A.H. Prevalence of pituitary adenomas: A community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin. Endocrinol. 2010, 72, 377–382. [Google Scholar] [CrossRef]
- Caturegli, P.; Newschaffer, C.; Olivi, A.; Pomper, M.G.; Burger, P.C.; Rose, N.R. Autoimmune hypophysitis. Endocr. Rev. 2005, 26, 599–614. [Google Scholar] [CrossRef]
- Ach, T.; Ben Yahia, W.; Halloul, I.; Sghaier, F.; Atig, A. Neurosarcoidosis-Induced Hypophysitis Mimicking Pituitary Macroadenoma. Cureus 2023, 15, e39865. [Google Scholar] [CrossRef]
- Kluczyński, Ł.; Gilis-Januszewska, A.; Rogoziński, D.; Pantofliński, J.; Hubalewska-Dydejczyk, A. Hypophysitis—New insights into diagnosis and treatment. Endokrynol. Pol. 2019, 70, 260–269. [Google Scholar] [CrossRef]
- Prete, A.; Salvatori, R. Hypophysitis. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519842/ (accessed on 15 October 2021).
- Di Chiro, G.; Nelson, K.B. The volume of the sella turcica. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1962, 87, 989–1008. [Google Scholar]
- Hussein, I.H.; Mansour, A.A.; Jameel, N.A. Comparing MRI volume measurement techniques for pituitary macroadenoma: Investigating volume reduction and its relationship with biochemical control. J. Med. Life 2023, 16, 998–1006. [Google Scholar] [CrossRef]
- Gutenberg, A.; Larsen, J.; Lupi, I.; Rohde, V.; Caturegli, P. A Radiologic Score to Distinguish Autoimmune Hypophysitis from Nonsecreting Pituitary Adenoma Preoperatively. Am. J. Neuroradiol. 2009, 30, 1766–1772. [Google Scholar] [CrossRef]
- Rupp, D.; Molitch, M. Pituitary stalk lesions. Curr. Opin. Endocrinol. Diabetes Obes. 2008, 15, 339–345. [Google Scholar] [CrossRef]
- Sol, Y.L.; Lee, S.; Choi, H.S.; Lee, Y.H.; Kim, J.; Kim, S. Evaluation of MRI Criteria for Cavernous Sinus Invasion in Pituitary Macroadenoma. J. Neuroimaging 2014, 24, 498–503. [Google Scholar] [CrossRef]
- Knosp, E.; Steiner, E.; Kitz, K.; Matula, C. Pituitary adenomas with invasion of the cavernous sinus space: A magnetic resonance imaging classification compared with surgical findings. Neurosurgery 1993, 33, 610–617; discussion 617–618. [Google Scholar] [CrossRef] [PubMed]
- Celli, P.; Cervoni, L.; Cantore, G. Dural tail in pituitary adenoma. J. Neuroradiol. 1997, 24, 68–69. [Google Scholar]
- Pickett, C.A. Diagnosis and management of pituitary tumors: Recent advances. Prim. Care 2003, 30, 765–789. [Google Scholar] [CrossRef]
- Joshi, M.N.; Whitelaw, B.C.; Carroll, P.V. Mechanisms in Endocrinology: Hypophysitis: Diagnosis and treatment. Eur. J. Endocrinol. 2018, 179, R151–R163. [Google Scholar] [CrossRef]
- Wright, K.; Kim, H.; Hill, T.; Lee, M.; Orillac, C.; Mogar, N.; Pacione, D.; Agrawal, N. Preoperative differentiation of hypophysitis and pituitary adenomas using a novel clinicoradiologic scoring system. Pituitary 2022, 25, 602–614. [Google Scholar] [CrossRef] [PubMed]
- De Vries, F.; Van Furth, W.R.; Biermasz, N.R.; Pereira, A.M. Hypophysitis: A comprehensive overview. Presse Méd. 2021, 50, 104076. [Google Scholar] [CrossRef] [PubMed]
- Taieb, A.; Mounira, E.E. Pilot Findings on SARS-CoV-2 Vaccine-Induced Pituitary Diseases: A Mini Review from Diagnosis to Pathophysiology. Vaccines 2022, 10, 2004. [Google Scholar] [CrossRef]
- Lee, M.S.; Pless, M. Apoplectic lymphocytic hypophysitis: Case report. J. Neurosurg. 2003, 98, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Paja, M.; Estrada, J.; Ojeda, A.; Ramón y Cajal, S.; García-Uría, J.; Lucas, T. Lymphocytic hypophysitis causing hypopituitarism and diabetes insipidus, and associated with autoimmune thyroiditis, in a non-pregnant woman. Postgrad. Med. J. 1994, 70, 220–224. [Google Scholar] [CrossRef]
- Escobar-Morreale, H.; Serrano-Gotarredona, J.; Varela, C. Isolated adrenocorticotropic hormone deficiency due to probable lymphocytic hypophysitis in a man. J. Endocrinol. Investig. 1994, 17, 127–131. [Google Scholar] [CrossRef]
- Sauter, N.P.; Toni, R.; McLaughlin, C.D.; Dyess, E.M.; Kritzman, J.; Lechan, R.M. Isolated adrenocorticotropin deficiency associated with an autoantibody to a corticotroph antigen that is not adrenocorticotropin or other proopiomelanocortin-derived peptides. J. Clin. Endocrinol. Metab. 1990, 70, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Nagai, Y.; Ieki, Y.; Ohsawa, K.; Kobayashi, K. Simultaneously found transient hypothyroidism due to Hashimoto’s thyroiditis, autoimmune hepatitis and isolated ACTH deficiency after cessation of glucocorticoid administration. Endocr. J. 1997, 44, 453–458. [Google Scholar] [CrossRef][Green Version]
- Caranci, F.; Leone, G.; Ponsiglione, A.; Muto, M.; Tortora, F.; Muto, M.; Cirillo, S.; Brunese, L.; Cerase, A. Imaging findings in hypophysitis: A review. Radiol. Med. 2020, 125, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Tartaglione, T.; Chiloiro, S.; Laino, M.E.; Giampietro, A.; Gaudino, S.; Zoli, A.; Bianchi, A.; Pontecorvi, A.; Colosimo, C.; De Marinis, L. Neuro-radiological features can predict hypopituitarism in primary autoimmune hypophysitis. Pituitary 2018, 21, 414–424. [Google Scholar] [CrossRef]
- Greenman, Y.; Ouaknine, G.; Veshchev, I.; Reider-Groswasser, I.I.; Segev, Y.; Stern, N. Postoperative surveillance of clinically nonfunctioning pituitary macroadenomas: Markers of tumour quiescence and regrowth. Clin. Endocrinol. 2003, 58, 763–769. [Google Scholar] [CrossRef]
- Greenman, Y.; Stern, N. Non-functioning pituitary adenomas. Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 625–638. [Google Scholar] [CrossRef]
- Demetri, C.; Shoukri, K.C.; Taylor, S.L.; Silva, J.E. Postpartum granulomatous hypophysitis with sphenoid sinus involvement: A case study. Endocr. Pract. 2010, 16, 264–269. [Google Scholar] [CrossRef][Green Version]
- Nussbaum, C.E.; Okawara, S.H.; Jacobs, L.S. Lymphocytic hypophysitis with involvement of the cavernous sinus and hypothalamus. Neurosurgery 1991, 28, 440–444. [Google Scholar] [CrossRef]
- Pagoada-Torres, J.D.; Villalobos-Díaz, R.; Pineda-Centeno, L.M.; Pesci-Eguia, L.; Gomez-Villegas, T.; Rivera-Montes, H.; Portocarrero-Ortiz, L.A. Bilateral Sixth Nerve Palsy: A Rare Presentation of Primary Hypophysitis. Cureus 2024, 16, e58850. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, D.E.H.; Ibrahim, A.E.K.; Ellison, D.W.; Armitage, M.; Gawne-Cain, M.; Lees, P.D. Inflammatory Hypophysitis—The Spectrum of Disease. Acta Neurochir. 2002, 144, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Catford, S.; Wang, Y.Y.; Wong, R. Pituitary stalk lesions: Systematic review and clinical guidance. Clin. Endocrinol. 2016, 85, 507–521. [Google Scholar] [CrossRef] [PubMed]
| Criterion | G1 | G2 | p |
|---|---|---|---|
| Age (mean ± standard deviation) | 50.21 ± 11.97 years | 43.5 ± 12.36 years | 0.053 |
| Male gender n (%) | 24 (42.9%) | 1 (6.2%) | 0.007 |
| Female gender n (%) | 32 (57.1%) | 15 (93.8%) | |
| Pregnancy n (%) | 1 (1.7%) | 2 (12.5%) | 0.122 |
| Autoimmune disease n (%) | 1 (1.7%) | 2 (12.5%) | 0.122 |
| Tumoral pathology n (%) | 2 (3.5%) | 0 (0%) | 0.7 |
| Granulomatosis n (%) | 0 (0%) | 1 (6.2%) | 0.222 |
| Vasculitis n (%) | 0 (0%) | 1 (6.2%) | 0.222 |
| Tumoral syndrome n (%) | 56 (100%) | 7 (43.8%) | <0.001 |
| Headaches n (%) | 53 (94.6%) | 8 (50%) | <0.001 |
| Visual disturbances n (%) | 51 (91.1%) | 6 (37.5%) | <0.001 |
| -Bitemporal hemianopia | 24 (42.9%) | 2 (12.5%) | 0.026 |
| -HLH | 3 (5.4%) | 0 (0%) | 1 |
| -Ophtalmoplegia | 8 (14.3%) | 0 (0%) | 0.186 |
| -Blindness | 3 (5.4%) | 0 (0%) | 1 |
| -Decreased visual acuity | 22 (39.3%) | 4 (25%) | 0.294 |
| CDI n (%) | 1 (1.7%) | 10 (62.5%) | <0.001 |
| Parameter | G1 | G2 | p |
|---|---|---|---|
| Corticotropic axis | |||
| Basal cortisol < 50 ng/mL n (%) | 10 (17.8%) | 10 (62.5%) | 0.003 |
| Peak cortisol < 180 ng/mL n (%) | 13 (23.1%) | 10 (62.5%) | 0.003 |
| Thyrotropic axis | |||
| FT4 < 7 pg/mL n (%) | 7 (12.5%) | 5 (31.3%) | 0.32 |
| Mean TSH (μUI/mL) [standard deviation] | 2.5 [±1] | 1.8 [±1.2] | 0.23 |
| Gonadotropic axis | |||
| Hypogonadism n (%) | 8 (14.3%) | 0 (0%) | 0.122 |
| Mean FSH (mUI/mL) [standard deviation] | 9.58 [±9.8] | 33.9 [±55.9] | 0.222 |
| Mean LH (mUI/mL) [standard deviation] | 10 [±11.56] | 19.6 [±23.8] | 0.323 |
| Somatotropic axis | |||
| Mean IGF1 (ng/mL) [minimum–maximum] | 97.91 [40–322] | 157.83 [8–323.4] | <0.001 |
| GH deficiency n (%) | 45 (80.4%) | 3 (18.8%) | <0.001 |
| Lactotropic axis | |||
| Mean PRL (ng/mL) [standard deviation] | 36.5 [±36.4] | 23.98 [±25.7] | 0.1 |
| Lactotropic insufficiency n (%) | 0 (0%) | 0 (0%) | - |
| Radiological Parameter | G1 | G2 | p |
|---|---|---|---|
| Pituitary volume > 7 cm3 (%) | 42.9 | 6.2 | 0.007 |
| Isointense signal on T1-weighted sequences (%) | 89.3 | 100 | 0.327 |
| Isointense signal on T2-weighted sequences (%) | 76.8 | 93.8 | 0.169 |
| Homogeneous signal before contrast injection (%) | 25 | 93.7 | <0.001 |
| Intense contrast enhancement (%) | 1.8 | 50 | <0.001 |
| Homogeneous contrast enhancement (%) | 41.1 | 93.8 | <0.001 |
| Symmetry (%) | 17.9 | 100 | <0.001 |
| Presence of dural-tail sign (%) | 10.7 | 0 | 0.327 |
| Pituitary stalk thickening (%) | 1.7 | 62.5 | <0.001 |
| Presence of a pituitary pseudo-capsule (%) | 16.1 | 0 | 0.192 |
| Loss of the posterior pituitary bright spot (%) | 25 | 62.5 | <0.001 |
| Ectopic ADH storage (%) | 23.2 | 0 | 0.059 |
| Invasion of the cavernous sinuses (%) | 50 | 6.3 | <0.001 |
| Compression of the optic chiasm (%) | 62.5 | 0 | <0.001 |
| Compression of the optic nerve (%) | 5.4 | 0 | 0.154 |
| Mucosal thickening of the sphenoidal sinus (%) | 44.6 | 0 | <0.001 |
| Criterion | β * | OR | CI95% | p | Score |
|---|---|---|---|---|---|
| Clinical Criteria | |||||
| Female sex | 2.719 | 15.164 | 0.255–903.268 | 0.192 | 3 |
| Headaches | −2.011 | 0.134 | 0.002–8.508 | 0.342 | −2 |
| Visual disturbances | −1.881 | 0.152 | 0.005–4.294 | 0.269 | −2 |
| Biological Criterion | |||||
| Corticotropic insufficiency | 1.054 | 2.869 | 0.138–59.599 | 0.496 | 1 |
| Radiologiccal Criteria | |||||
| Pituitary volume ≤ 7 cm3 | 0.484 | 1.623 | 0.068–38.642 | 0.765 | 0.5 |
| Loss of posterior pituitary T1 hyperintensity | 0.318 | 1.375 | 0.024–78.285 | 0.877 | 0.5 |
| Cavernous sinus invasion | −0.436 | 0.647 | 0.04–10.557 | 0.76 | −0.5 |
| Pituitary stalk thickening | 4.579 | 97.386 | 1.975–4801.324 | 0.021 | 4.5 |
| Optic pathway compression | −1.717 | 0.18 | 0.003–9.429 | 0.396 | −2 |
| Criteria | Points |
|---|---|
| Female sex | +3 |
| Presence of headaches | −2 |
| Presence of visual disturbances | −2 |
| Corticotropic insufficiency | +1 |
| Pituitary volume < 7 cm3 | +0.5 |
| Loss of the posterior pituitary bright spot | +0.5 |
| Cavernous sinus invasion | −0.5 |
| Pituitary stalk thickening | +4.5 |
| Optic pathway compression | −2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taieb, A.; Bouzaouache, I.; Gasmi, A.; Ghachem, A.; Halloul, I.; Saafi, W.; Hamza, E.; Ghada, S.; Hasni, Y.; Mhabrech, H. A Predictive Score Incorporating Clinical, Radiologic, and Hormonal Parameters to Discriminate Lymphocytic Hypophysitis from Non-Functioning Pituitary Macroadenomas. Diagnostics 2025, 15, 2334. https://doi.org/10.3390/diagnostics15182334
Taieb A, Bouzaouache I, Gasmi A, Ghachem A, Halloul I, Saafi W, Hamza E, Ghada S, Hasni Y, Mhabrech H. A Predictive Score Incorporating Clinical, Radiologic, and Hormonal Parameters to Discriminate Lymphocytic Hypophysitis from Non-Functioning Pituitary Macroadenomas. Diagnostics. 2025; 15(18):2334. https://doi.org/10.3390/diagnostics15182334
Chicago/Turabian StyleTaieb, Ach, Ines Bouzaouache, Ayoub Gasmi, Aicha Ghachem, Imen Halloul, Wiem Saafi, ElFekih Hamza, Saad Ghada, Yosra Hasni, and Houda Mhabrech. 2025. "A Predictive Score Incorporating Clinical, Radiologic, and Hormonal Parameters to Discriminate Lymphocytic Hypophysitis from Non-Functioning Pituitary Macroadenomas" Diagnostics 15, no. 18: 2334. https://doi.org/10.3390/diagnostics15182334
APA StyleTaieb, A., Bouzaouache, I., Gasmi, A., Ghachem, A., Halloul, I., Saafi, W., Hamza, E., Ghada, S., Hasni, Y., & Mhabrech, H. (2025). A Predictive Score Incorporating Clinical, Radiologic, and Hormonal Parameters to Discriminate Lymphocytic Hypophysitis from Non-Functioning Pituitary Macroadenomas. Diagnostics, 15(18), 2334. https://doi.org/10.3390/diagnostics15182334







