Prevalence of the Peroneus Quartus Muscle and Its Association with Peroneal Tendon Pathologies: An MRI Study of 1160 Ankles
Abstract
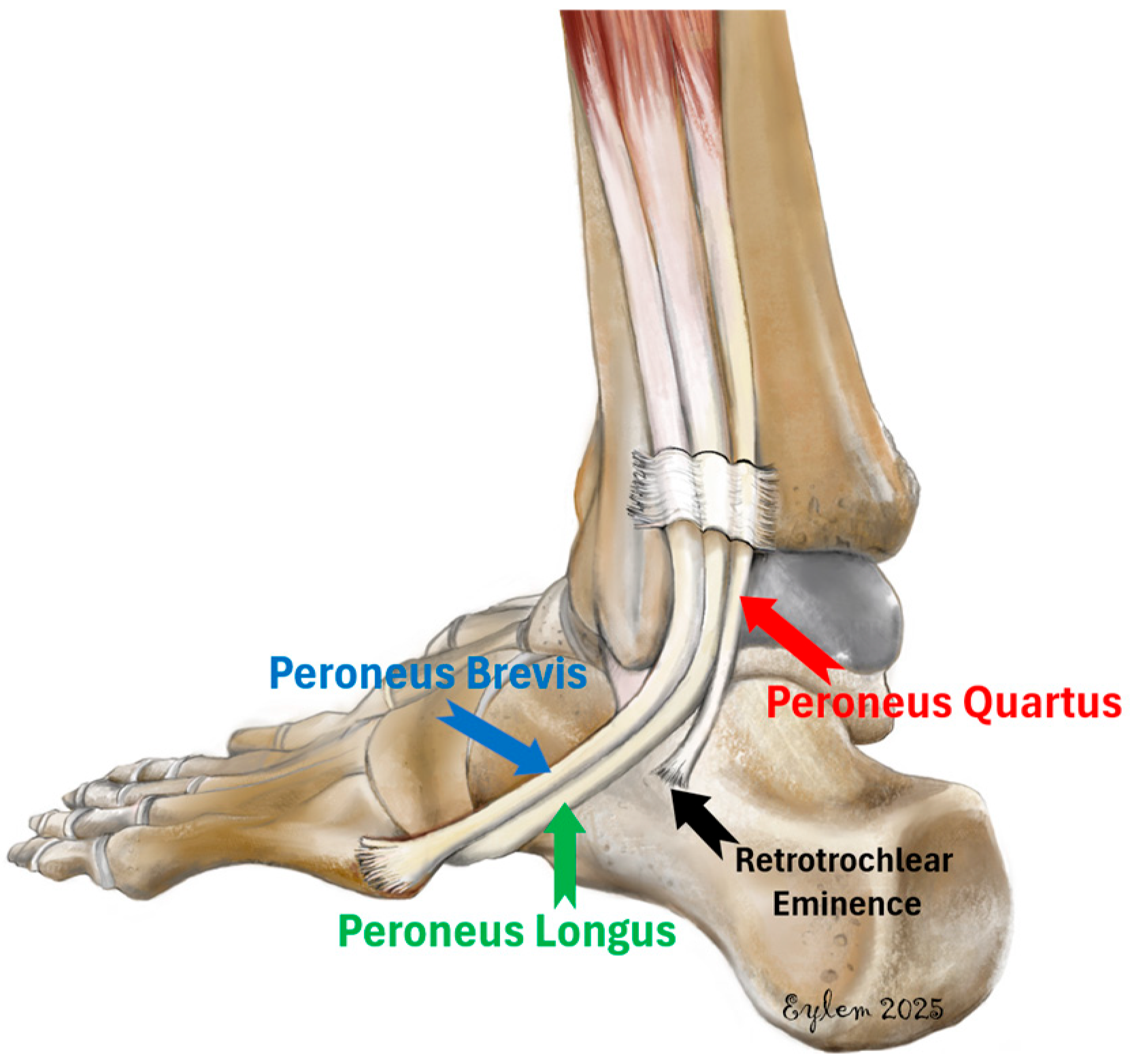
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Magnetic Resonance Imaging Protocol
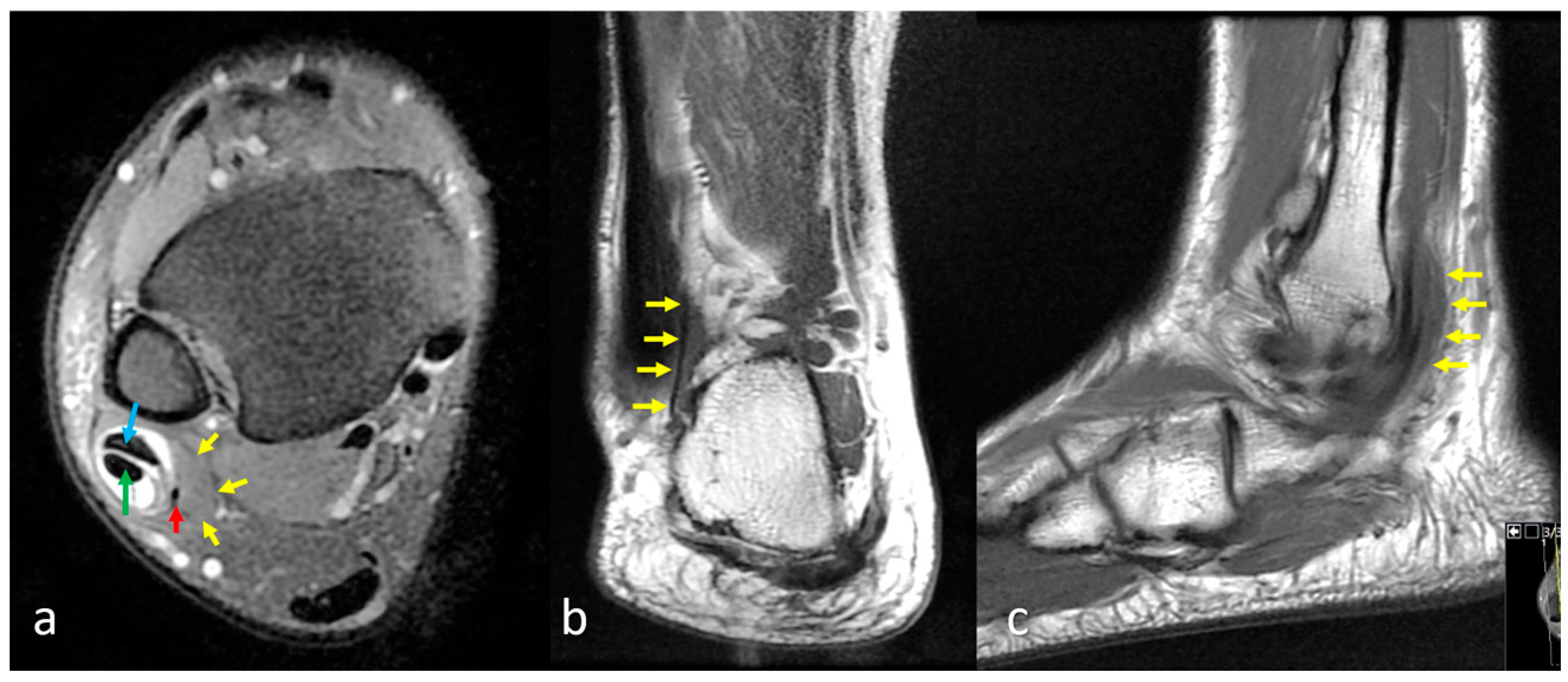
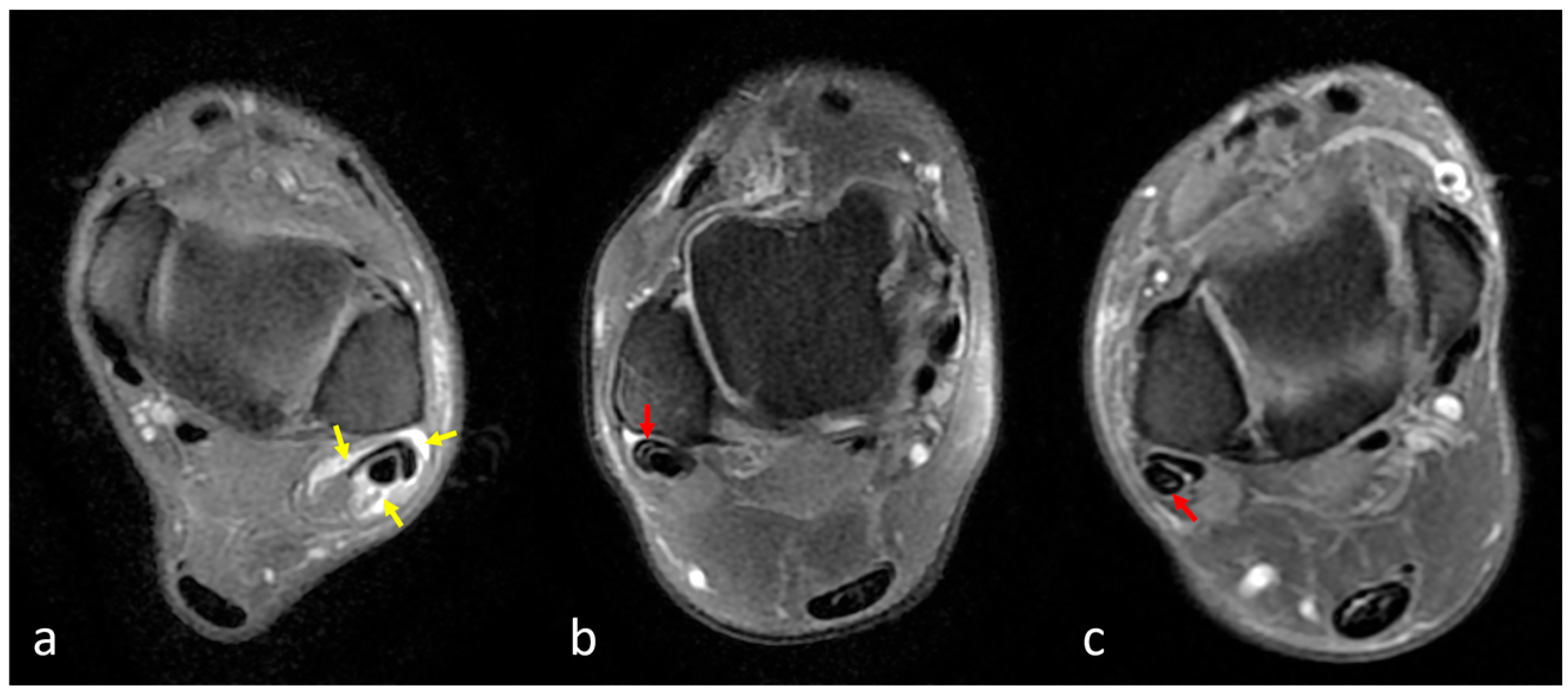
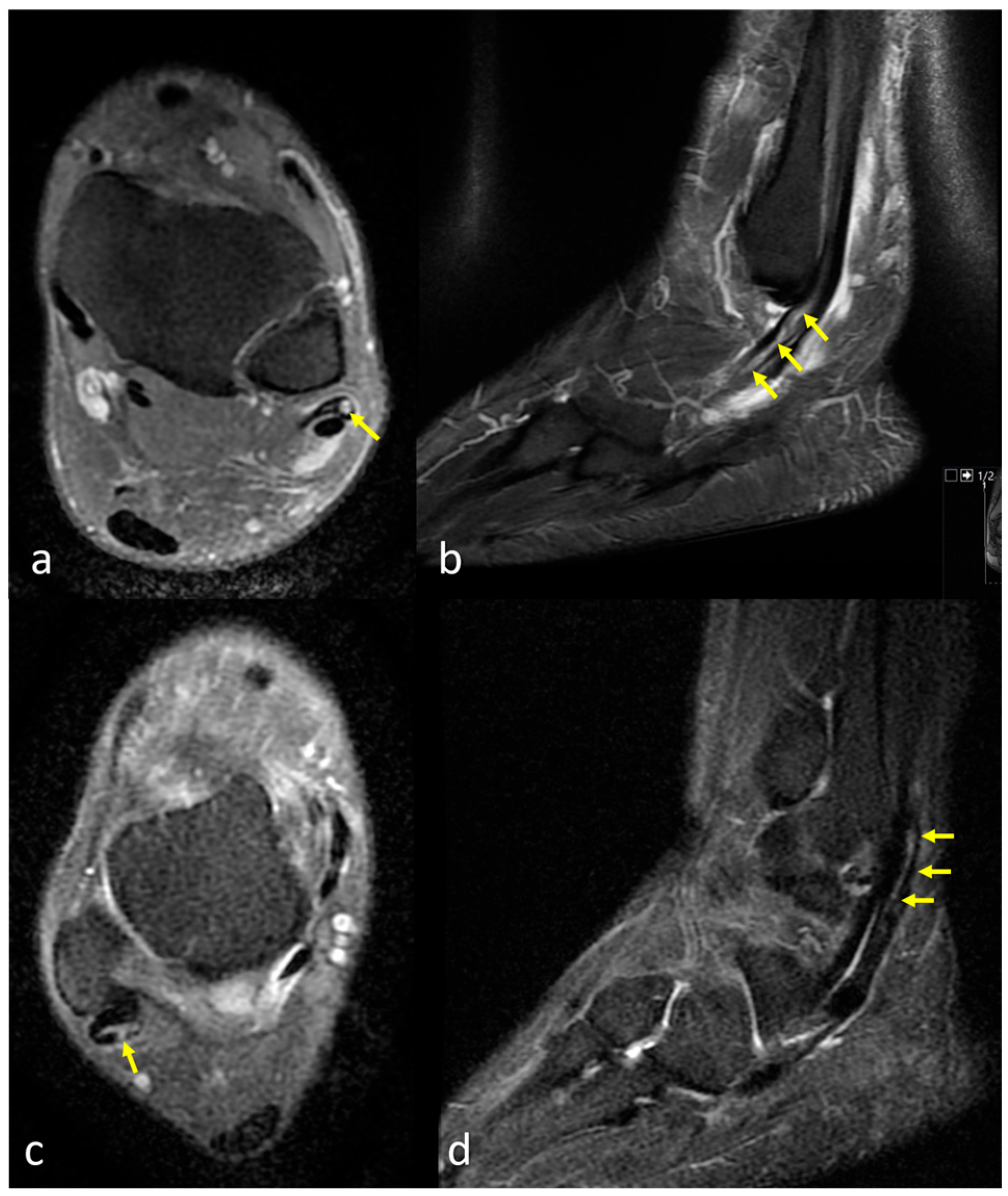
2.3. Assessment of the Peroneus Quartus Muscle and Peroneal Pathologies
2.4. Definitions of Peroneal Tendon Pathologies
2.5. Statistical Analysis
3. Results
4. Discussion
5. Strengths, Limitations, and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CI | Confidence Interval |
| FSE | Fast Spin Echo |
| MRI | Magnetic Resonance Imaging |
| OR | Odds Ratio |
| PD | Proton Density |
| PBT | Peroneus Brevis Tendon |
| PLT | Peroneus Longus Tendon |
| PQ | Peroneus Quartus |
| STIR | Short Tau Inversion Recovery |
| TSE | Turbo Spin Echo |
| TR | Repetition Time |
| TE | Echo Time |
| FOV | Field of View |
References
- Hallinan, J.T.P.D.; Wang, W.; Pathria, M.N.; Smitaman, E.; Huang, B.K. The peroneus longus muscle and tendon: A review of its anatomy and pathology. Skelet. Radiol. 2019, 48, 1329–1344. [Google Scholar] [CrossRef]
- Cheung, Y. Normal Variants: Accessory Muscles About the Ankle. Magn. Reson. Imaging Clin. N. Am. 2017, 25, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Hecker, P. Study on the peroneus on the tarsus. Anat. Rec. 1923, 26, 79–82. [Google Scholar] [CrossRef]
- Sobel, M.; Levy, M.E.; Bohne, W.H. Congenital variations of the peroneus quartus muscle: An anatomic study. Foot Ankle 1990, 11, 81–88. [Google Scholar] [CrossRef]
- Ayanoglu, T.; Arikan, E.; Kurtbogan, M.; Yilmaz, O.F.; Kaya, Y.E.; Ozturan, K.E. Anatomical Factors Which Influence the Formation of Peroneal Tendon Tears: A Retrospective Comparative Study. J. Foot Ankle Surg. 2022, 61, 1299–1302. [Google Scholar] [CrossRef]
- Pota, K.; Baysal, C.Ç.; Civan, O.; Ürgüden, M. Evaluation of the relations between foot & ankle pathologies and anatomic variations with magnetic resonance imaging of 849 study population. Jt. Dis. Relat. Surg. 2025, 36, 394–407. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, Z.S.; Beltran, J.; Cheung, Y.Y.; Colon, E.; Herraiz, F. MR features of longitudinal tears of the peroneus brevis tendon. Am. J. Roentgenol. 1997, 168, 141–147. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lamm, B.M.; Myers, D.T.; Dombek, M.; Mendicino, R.W.; Catanzariti, A.R.; Saltrick, K. Magnetic resonance imaging and surgical correlation of peroneus brevis tears. J. Foot Ankle Surg. 2004, 43, 30–36. [Google Scholar] [CrossRef]
- Miura, K.; Ishibashi, Y.; Tsuda, E.; Kusumi, T.; Toh, S. Split lesions of the peroneus brevis tendon in the Japanese population: An anatomic and histologic study of 112 cadaveric ankles. J. Orthop. Sci. 2004, 9, 291–295. [Google Scholar] [CrossRef]
- Major, N.M.; Helms, C.A.; Fritz, R.C.; Speer, K.P. The MR imaging appearance of longitudinal split tears of the peroneus brevis tendon. Foot Ankle Int. 2000, 21, 514–519. [Google Scholar] [CrossRef]
- Park, H.J.; Cha, S.D.; Kim, H.S.; Chung, S.T.; Park, N.H.; Yoo, J.H.; Park, J.H.; Kim, J.H.; Lee, T.W.; Lee, C.H. Reliability of MRI findings of peroneal tendinopathy in patients with lateral chronic ankle instability. Clin. Orthop. Surg. 2010, 2, 237–243. [Google Scholar] [CrossRef]
- Cabral, P.; Paulino, C.; Takahashi, R.; Clopton, P.; Resnick, D. Correlation of morphologic and pathologic features of the various tendon groups around the ankle: MR imaging investigation. Skelet. Radiol. 2013, 42, 1393–1402. [Google Scholar] [CrossRef]
- Wood, J. Variations in human myology observed during the winter session of 1867–1868 at King’s College, London. Proc. R. Soc. Lond. 1868, 16, 483–525. [Google Scholar] [CrossRef]
- Pozzi, S. Sur une varieté fréquente du muscle court péronier latéral chez l’homme (anomalie réversive). Bull. Soc. Anthropol. Paris 1872, 2, 155–161. [Google Scholar] [CrossRef]
- Macalister, A. Additional observations on muscular anomalies in human anatomy (third series), with a catalogue of the principal muscular variations hitherto published. Trans. R. Ir. Acad. 1875, 25, 1–134. [Google Scholar]
- Gruber, W. Ein neuer Musculus peroneo-calcaneus externus anterior. Arch. Pathol. Anat. Physiol. Klin. Med. 1879, 95, 177–179. [Google Scholar] [CrossRef]
- Testut, L. Les Anomalies Musculaires Chez l’Homme Expliquées par l’Anatomie Comparée, Leur Importance en Anthropologie; G. Masson: Éditeur, Libraire de l’Académie de Médecine, Paris, France, 1884; pp. 744–758. [Google Scholar] [CrossRef]
- Chudzinski, T. Observations sur les variations musculaires dans les races humaines. Mém. Soc. Anthrop. Paris 1898, 2, 1–223. [Google Scholar]
- Pales, L.; Chippeaux, C. Myologie comparative du pied. Bull. Mem. Soc. Anthrop. Paris 1952, 3, 284–336. [Google Scholar] [CrossRef]
- Mori, M. Statistics on the musculature of the Japanese. Okajimas Folia Anat. Jpn. 1964, 40, 195–300. [Google Scholar] [CrossRef]
- Chaney, D.M.; Lee, M.S.; Khan, M.A.; Krueger, W.A.; Mandracchia, V.J.; Yoho, R.M. Study of ten anatomical variants of the foot and ankle. J. Am. Podiatr. Med. Assoc. 1996, 86, 532–537. [Google Scholar] [CrossRef]
- Bonnin, M.; Tavernier, T.; Bouysset, M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am. J. Sports Med. 1997, 25, 699–703. [Google Scholar] [CrossRef] [PubMed]
- Kudoh, H.; Sakai, T.; Horiguchi, M. The consistent presence of the human accessory deep peroneal nerve. J. Anat. 1999, 194, 101–108. [Google Scholar] [CrossRef]
- DiGiovanni, B.F.; Fraga, C.J.; Cohen, B.E.; Shereff, M.J. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000, 21, 809–815. [Google Scholar] [CrossRef]
- Chepuri, N.B.; Jacobson, J.A.; Fessell, D.P.; Hayes, C.W. Sonographic appearance of the peroneus quartus muscle: Correlation with MR imaging. Appearance in seven patients. Radiology 2001, 218, 415–419. [Google Scholar] [CrossRef]
- Borne, J.; Fantino, O.; Besse, J.L.; Clouet, P.L.; Tran Minh, V.A. Aspect IRM des variants anatomiques des muscles, tendons et ligaments de la Cheville. J. Radiol. 2002, 83, 27–38. [Google Scholar] [CrossRef]
- Zammit, J.; Singh, D. The peroneus quartus muscle. Anatomy and clinical relevance. J. Bone Jt. Surg. 2003, 85, 1134–1137. [Google Scholar] [CrossRef]
- Saupe, N.; Mengiardi, B.; Pfirrmann, C.W.; Vienne, P.; Seifert, B.; Zanetti, M. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology 2007, 242, 509–517. [Google Scholar] [CrossRef]
- Tubbs, R.S.; May, W.R.; Shoja, M.M.; Loukas, M.; Salter, E.G.; Oakes, W.J. Peroneotalocalcaneus muscle. Anat. Sci. Int. 2008, 83, 280–282. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.L.; Lopez-Ben, R.; Maddox, J. A preliminary report on intra-sheath peroneal tendon subluxation: A prospective review of 7 patients with ultrasound verification. J. Foot Ankle Surg. 2009, 48, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Uğurlu, M.; Bozkurt, M.; Demirkale, I.; Cömert, A.; Acar, H.I.; Tekdemir, I. Anatomy of the lateral complex of the ankle joint in relation to peroneal tendons, distal fibula and talus: A cadaveric study. Eklem Hast. Cerrahisi 2010, 21, 153–158. [Google Scholar]
- Saxena, A.; Luhadiya, A.; Ewen, B.; Goumas, C. Magnetic resonance imaging and incidental findings of lateral ankle pathologic features with asymptomatic ankles. J. Foot Ankle Surg. 2011, 50, 413–415. [Google Scholar] [CrossRef]
- Prakash Narayanswamy, C.; Singh, D.K.; Rajini, T.; Venkatiah, J.; Singh, G. Anatomical variations of peroneal muscles: A cadaver study in an Indian population and a review of the literature. J. Am. Podiatr. Med. Assoc. 2011, 101, 505–508. [Google Scholar] [CrossRef]
- Athavale, S.A.; Gupta, V.; Kotgirwar, S.; Singh, V. The peroneus quartus muscle: Clinical correlation with evolutionary importance. Anat. Sci. Int. 2012, 87, 106–110. [Google Scholar] [CrossRef]
- Nascimento, S.R.R.; Costa, R.W.; Ruiz, C.R.; Wafae, N. Analysis on the incidence of the fibularis quartus muscle using magnetic resonance imaging. Anat. Res. Int. 2012, 2012, 485149. [Google Scholar] [CrossRef]
- Clarkson, M.J.; Fox, J.N.; Atsas, S.; Daney, B.T.; Dodson, S.C.; Lambert, H.W. Clinical implications of novel variants of the fibularis (peroneus) quartus muscle inserting onto the cuboid bone: Peroneocuboideus and peroneocalcaneocuboideus. J. Foot Ankle Surg. 2013, 52, 118–121. [Google Scholar] [CrossRef]
- Bilgili, M.G.; Kaynak, G.; Botanlioğlu, H.; Basaran, S.H.; Ercin, E.; Baca, E.; Uzun, I. Peroneus quartus: Prevalance and clinical importance. Arch. Orthop. Trauma Surg. 2014, 134, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Zhenbo, Z.; Jin, W.; Haifeng, G.; Huanting, L.; Feng, C.; Ming, L. Sliding fibular graft repair for the treatment of recurrent peroneal subluxation. Foot Ankle Int. 2014, 35, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Hur, M.S.; Won, H.S.; Chung, I.H. A new morphological classification for the fibularis quartus muscle. Surg. Radiol. Anat. 2015, 37, 27–32. [Google Scholar] [CrossRef]
- Galli, M.M.; Protzman, N.M.; Mandelker, E.M.; Malhotra, A.D.; Schwartz, E.; Brigido, S.A. An examination of anatomic variants and incidental peroneal tendon pathologic features: A comprehensive MRI review of asymptomatic lateral ankles. J. Foot Ankle Surg. 2015, 54, 164–172. [Google Scholar] [CrossRef]
- Somesh, M.S.; Murlimanju, B.V.; Roshan, S.; Kamble, G. Peroneus quartus in south indian population: A Cadaveric study. Int. J. Anat. Res. 2016, 4, 1972–1976. [Google Scholar] [CrossRef]
- Grace, S.; Preethi Ramya, T.; Anjana, T.S.R. An adaptational Change of evolutionary significance in peroneal Tendons: An anomalous peroneus quartus and a Proximally migrated peroneus brevis tendon. Int. J. Anat. Res. 2016, 4, 2454–2458. [Google Scholar] [CrossRef]
- Mustafa, A.Y.A.E.; Mohammed, W.A.; Alasmari; Alkushi, A.G.; Sakran, A.M.E.A. Peroneus quartus muscle: Its incidence and Clinical importance. Int. J. Anat. Res. 2017, 5, 4691–4694. [Google Scholar] [CrossRef][Green Version]
- Dangintawat, P.; Apinun, J.; Huanmanop, T.; Agthong, S.; Chentanez, V. Morphometric study of inferior peroneal retinaculum and contents of inferior peroneal tunnel. Folia Morphol. 2019, 78, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Ersoz, E.; Tokgoz, N.; Kaptan, A.Y.; Ozturk, A.M.; Ucar, M. Anatomical variations related to pathological conditions of the peroneal tendon: Evaluation of ankle MRI with a 3D SPACE sequence in symptomatic patients. Skelet. Radiol. 2019, 48, 1221–1231. [Google Scholar] [CrossRef]
- Inchai, C.; Apivatthakakul, T.; Sinthubua, A.; Mahakkanukrauh, P. The prevalence of the accessory peroneal muscle; peroneus quartus and its clinical implications. Int. Med. J. 2021, 28, 240–242. [Google Scholar]
- Cheung, Y.Y.; Rosenberg, Z.S.; Ramsinghani, R.; Beltran, J.; Jahss, M.H. Peroneus quartus muscle: MR imaging features. Radiology. 1997, 202, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Yammine, K. The accessory peroneal (fibular) muscles: Peroneus quartus and peroneus digiti quinti. A systematic review and meta-analysis. Surg. Radiol. Anat. 2015, 37, 617–627. [Google Scholar] [CrossRef]
- Kassim, M.M.; Rosenfeld, P. Tendoscopic debridement of peroneus quartus muscle for chronic lateral ankle pain: A case report. Foot Ankle Int. 2012, 33, 1024–1026. [Google Scholar] [CrossRef]
- Lui, T.H.; Li, H.M. Endoscopic Resection of Peroneus Quartus. Arthrosc. Tech. 2019, 9, e35–e38. [Google Scholar] [CrossRef]
- Lui, T.H. Tendoscopic resection of low-lying muscle belly of peroneus brevis or quartus. Foot Ankle Int. 2012, 33, 912–914. [Google Scholar] [CrossRef]
| Plane | Sequence | TR (ms) | TE (ms) | Slice (mm) | FOV (mm) | Acquisition Time |
|---|---|---|---|---|---|---|
| Sagittal | STIR | 1800–5500 | 9.1–136.3 | 4.0 | 160 | 216 s |
| T1-w FSE | 300–650 | 12.6–50.6 | 4.0 | 160 | 134 s | |
| T2-w TSE (with STIR) | 2500–6000 | 10–61 | 3.5 | 200 | 122 s | |
| T1-w TSE | 350–650 | 10–30 | 3.5 | 200 | 50 s | |
| Axial | PD-w FSE, fat-suppressed | 1500–3000 | 8.5–76.9 | 5.0 | 160 | 113 s |
| PD-w TSE, fat-suppressed | 3200–4500 | 10–82 | 4.0 | 180 | 115 s | |
| Coronal | T1-w FSE | 300–1500 | 12.6–50.6 | 4.0 | 160 | 122 s |
| T1-w TSE | 537–650 | 11–32 | 4.0 | 180 | 102 s | |
| PD-w, fat-suppressed | 152–2500 | 12.6–113.8 | 4.0 | 160 | 135 s | |
| PD-w TSE, fat-suppressed | 3300–4000 | 10–83 | 4.0 | 180 | 131 s |
| Gender | PQ Present | PQ Absent | p-Value |
|---|---|---|---|
| Male (n, % within males) | 59 (12.7%) | 405 (87.3%) | 0.064 1 |
| Female (n, % within females) | 64 (9.2%) | 632 (90.8%) | |
| Total (n, % within total) | 123 (10.6%) | 1037 (89.4%) | |
| Right | Left | p-value | |
| Male (n, % within males) | 38 (64.4%) | 21 (35.6%) | 0.150 1 |
| Female (n, % within females) | 36 (56.2%) | 28 (43.8%) | |
| Total (n, % within total) | 74 (60.2%) | 49 (39.8%) |
| Peroneus Quartus | Overall | Male | Female | p-Value |
|---|---|---|---|---|
| Bilateral Absent | 70 (80.5%) | 27 (79.4%) | 43 (81.1%) | 0.579 |
| Unilateral Present | 12 (13.8%) | 4 (11.8%) | 8 (15.1%) | |
| Bilateral Present | 5 (5.7%) | 3 (8.8%) | 2 (3.8%) | |
| Total | 87 (100%) | 34 (100%) | 53 (100%) |
| Pathologies | Peroneus Quartus | p-Value | Odd’s Ratio (95% CI) | ||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Tenosynovitis | No | 1008 (89.5%) | 118 (10.5%) | 0.396 | 1.47 (0.56–3.88) |
| Yes | 29 (85.3%) | 5 (14.7%) | |||
| PBT Tendinitis | No | 982 (90.3%) | 105 (9.7%) | 0.001 | 3.06 (1.73–5.41) |
| Yes | 55 (75.3%) | 18 (24.7%) | |||
| PBT Tear | No | 1015 (89.9%) | 114 (10.1%) | 0.003 | 3.64 (1.64–8.1) |
| Yes | 22 (71.0%) | 9 (29.0%) | |||
| PLT Tendinitis | No | 906 (90.9%) | 91 (9.1%) | 0.001 | 2.43 (1.56–3.79) |
| Yes | 131 (80.4%) | 32 (19.6%) | |||
| PLT Tear | No | 1033 (89.4%) | 123 (10.6%) | 0.638 | 1.05 (0.06–19.97) |
| Yes | 4 (100%) | 0 (0%) | |||
| Author | Year | Country | Study Type | Number of Patients (Ankles) * | Overall Prevalence |
|---|---|---|---|---|---|
| Wood [13] | 1868 | UK | Cadaver | 140 ankles | 1.4% (2/140) |
| Pozzi [14] | 1872 | France | Cadaver | 52 ankles | 7.7% (4/52) |
| Macalister et al. [15] | 1875 | UK | Cadaver | 60 ankles | 13.3% (8/60) |
| Gruber [16] | 1879 | Russian | Cadaver | 982 ankles | 12% (118/982) |
| Testut [17] | 1884 | France | Cadaver | 36 ankles | 55.6% (20/36) |
| Chudzinski [18] | 1898 | France | Cadaver | 30 ankles | 23.3% (7/30) |
| Hecker [3] | 1923 | France | Cadaver | 47 ankles | 13% (6/47) |
| Pales et Chippaux [19] | 1952 | Vietnam | Cadaver | 36 ankles | 19.4% (7/36) |
| Mori [20] | 1964 | Japan | Cadaver | 73 ankles | 2.7% (2/73) |
| Sobel et al. [4] | 1990 | USA | Cadaver | 65 (124 ankles) | 21.7% (27/124) |
| Chaney et al. [21] | 1996 | USA | Cadaver | 269 ankles | 3% (8/269) |
| Rosenberg et al. [7] | 1997 | USA | MRI | 37 (41 ankles) | 4.9% (2/41) |
| Cheung et al. [47] | 1997 | USA | MRI | 76 (136 ankles) | 10.3% (14/136) |
| Bonnin et al. [22] | 1997 | France | Surgical | 18 (18 ankles) | 16.7% (3/18) |
| Kudoh et al. [23] | 1999 | Japan | Cadaver | 24 ankles | 12.5% (3/24) |
| Major et al. [10] | 2000 | USA | MRI | 42 ankles | 23.8% (10/42) |
| DiGiovanni et al. [24] | 2000 | USA | Surgical | 61 (61 ankles) | 8.2% (5/61) |
| Chepuri et al. [25] | 2001 | USA | USG/MRI | 32 ankles | 21.8% (7/32) |
| Borne et al. [26] | 2002 | France | MRI | 63 ankles | 11.1% (7/63) |
| Zammit & Singh [27] | 2003 | UK | Cadaver | 66 (102 ankles) | 5.9% (6/102) |
| Miura et al. [9] | 2004 | Japan | Cadaver | 56 (112 ankles) | 5.3% (6/112) |
| Lamm et al. [8] | 2004 | USA | Surgical | 32 ankles | 15.6% (5/32) |
| Saupe et al. [28] | 2007 | Switzerland | MRI | 65 (65 ankles) | 16.9% (11/65) |
| Tubbs et al. [29] | 2008 | USA | Cadaver | 89 ankles | 1.1% (1/89) |
| Thomas et al. [30] | 2009 | USA | MRI | 7 (7 ankles) | 14.2% (1/7) |
| Ugurlu et al. [31] | 2010 | Turkey | Cadaver | 11 (22 ankles) | 9% (2/22) |
| Park et al. [11] | 2010 | Korea | MRI | 82 ankles | 6% (5/82) |
| Saxena et al. [32] | 2011 | USA | MRI | 100 (102 ankles) | 0.98% (1/102) |
| Prakash et al. [33] | 2011 | India | Cadaver | 70 ankles | 4.3% (3/70) |
| Athavale et al. [34] | 2012 | India | Cadaver | 92 ankles | 21.7% (20/92) |
| Nascimento et al. [35] | 2012 | Brazil | MRI | 135 (211 ankles) | 7.6% (16/211) |
| Clarkson et al. [36] | 2013 | USA | Cadaver | 277 ankles | 20.9% (58/277) |
| Bilgili et al. [37] | 2014 | Turkey | Cadaver | 58 (115 ankles) | 5.2% (6/115) |
| Zhenbo et al. [38] | 2014 | China | Surgical | 26 ankles | 15.3% (4/26) |
| Hur et al. [39] | 2015 | Korea | Cadaver | 40 (80 ankles) | 16.3% (13/80) |
| Galli et al. [40] | 2015 | USA | MRI | 104 (108 ankles) | 12.9% (14/108) |
| M S Somesh et al. [41] | 2016 | India | Cadaver | 47 ankles | 4.2% (2/47) |
| Grace et al. [42] | 2016 | India | Cadaver | 32 (64 ankles) | 1.5% (1/64) |
| Mustafa et al. [43] | 2017 | Saudi Arabia | Cadaver | 20 ankles | 20% (4/20) |
| Dangintawat et al. [44] | 2019 | Thailand | Cadaver | 109 ankles | 11.93% (13/109) |
| Ersoz et al. [45] | 2019 | Turkey | MRI | 60 (69 ankles) | 13% (9/69) |
| Inchai et al. [46] | 2021 | Thailand | Cadaver | 30 (60 ankles) | 6.6% (6/60) |
| Pota et al. [6] | 2025 | Turkey | MRI | 738 (849 ankles) | 13.8% (117/849) |
| Current study | 2025 | Turkey | MRI | 1073 (1160 ankles) | 10.6% (123/1160) |
| Total | 6236 ankles | 11.3% (708/6236) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuksel, Y.; Ergun, T.; Kose, O. Prevalence of the Peroneus Quartus Muscle and Its Association with Peroneal Tendon Pathologies: An MRI Study of 1160 Ankles. Diagnostics 2025, 15, 2329. https://doi.org/10.3390/diagnostics15182329
Yuksel Y, Ergun T, Kose O. Prevalence of the Peroneus Quartus Muscle and Its Association with Peroneal Tendon Pathologies: An MRI Study of 1160 Ankles. Diagnostics. 2025; 15(18):2329. https://doi.org/10.3390/diagnostics15182329
Chicago/Turabian StyleYuksel, Yavuz, Tarkan Ergun, and Ozkan Kose. 2025. "Prevalence of the Peroneus Quartus Muscle and Its Association with Peroneal Tendon Pathologies: An MRI Study of 1160 Ankles" Diagnostics 15, no. 18: 2329. https://doi.org/10.3390/diagnostics15182329
APA StyleYuksel, Y., Ergun, T., & Kose, O. (2025). Prevalence of the Peroneus Quartus Muscle and Its Association with Peroneal Tendon Pathologies: An MRI Study of 1160 Ankles. Diagnostics, 15(18), 2329. https://doi.org/10.3390/diagnostics15182329






