Assessment of Preprocedural Factors Associated with 5-Year Complete Response After Transarterial Radioembolization in Patients with Hepatocellular Carcinoma
Abstract
1. Introduction
2. Subjects and Methods
2.1. Study Patients
2.2. Pre-Procedure MR Image Acquisition and Analysis
2.3. Transarterial Radioembolization Procedure
2.4. Clinical Data Collection
2.5. Statistical Analysis
3. Results
3.1. Study Patients’ Characteristics
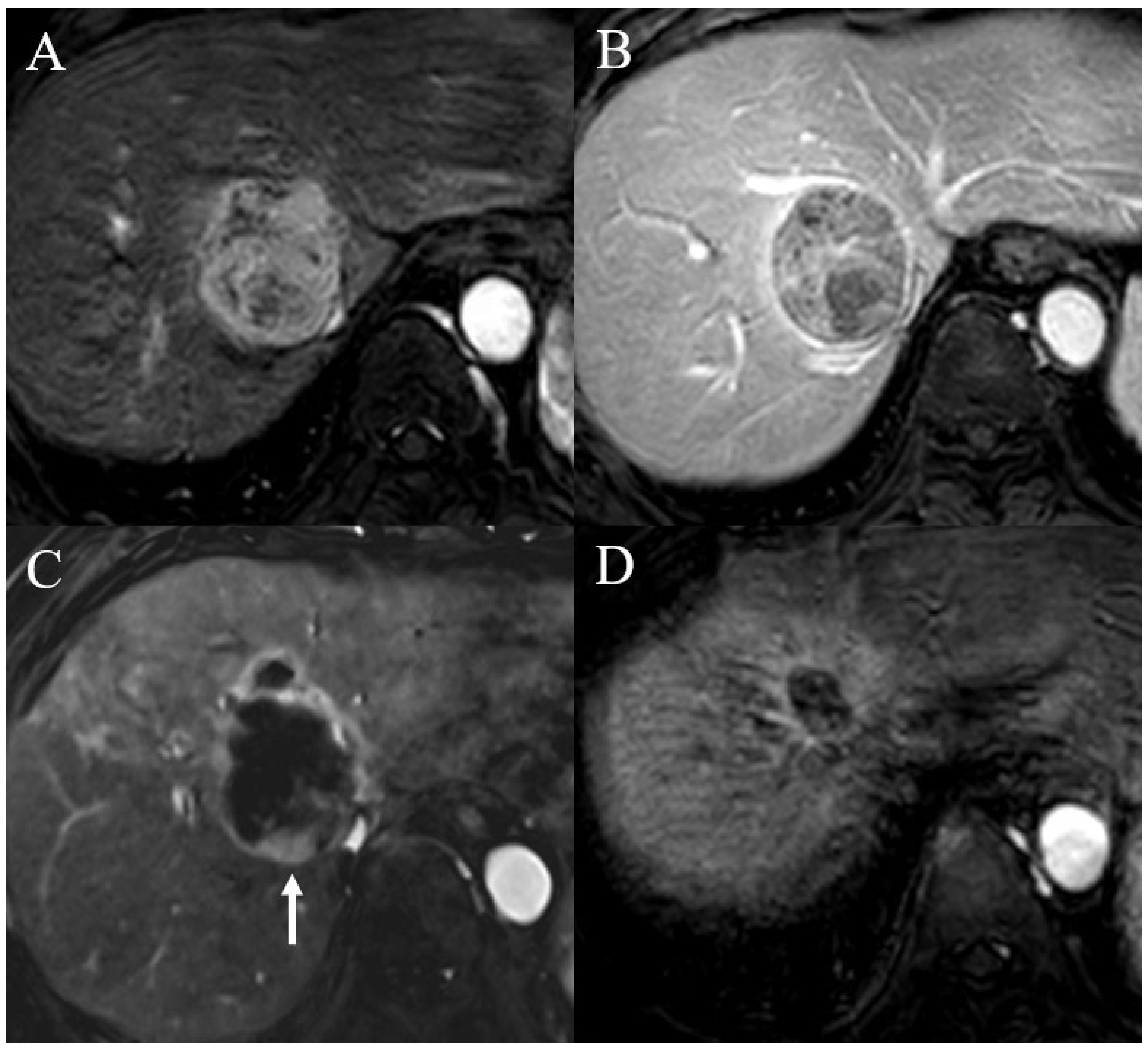
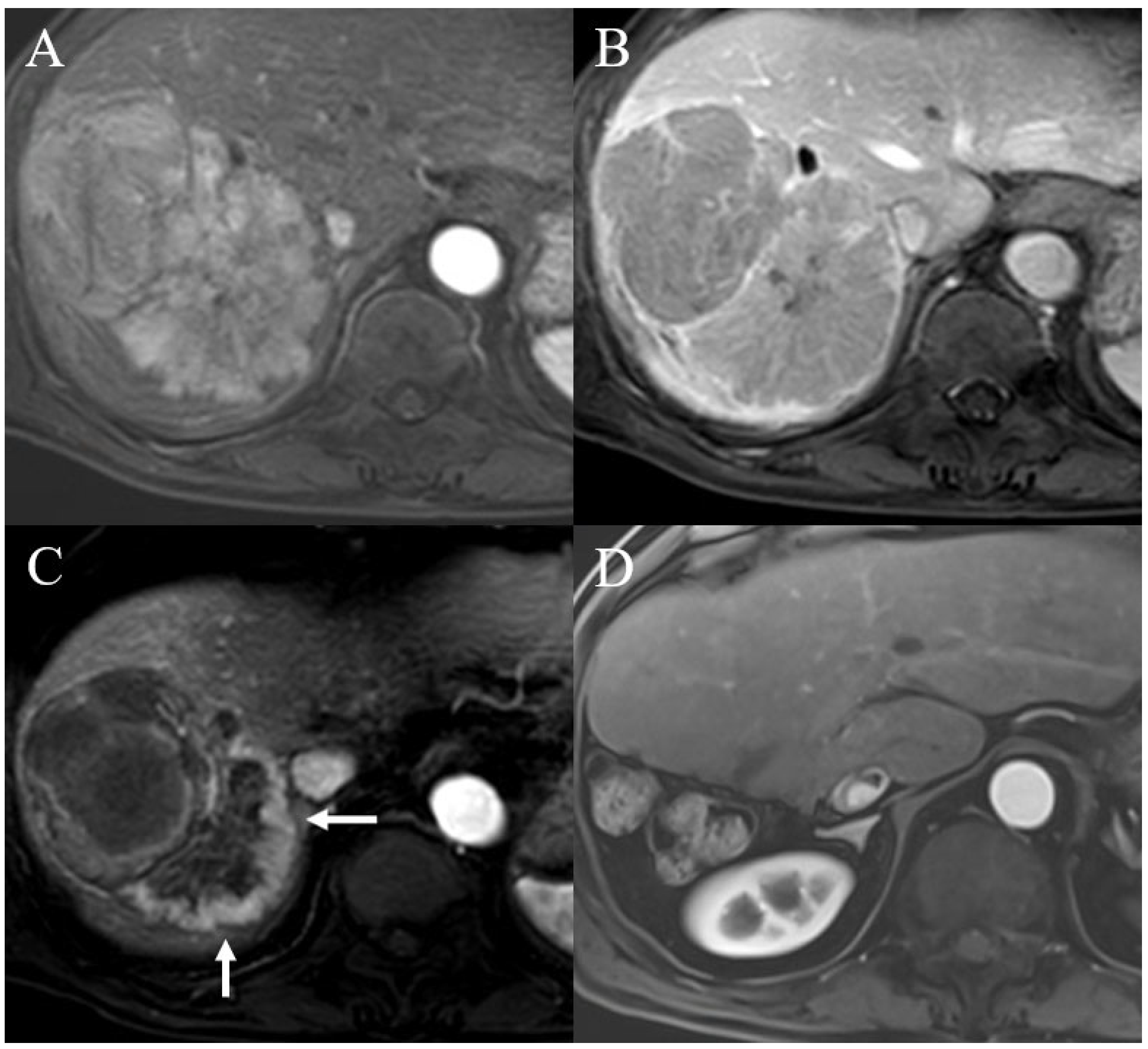
3.2. Assessment of Predictors for Tumor Recurrence After TARE
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Keshavarz, P.; Nezami, N.; Yazdanpanah, F.; Khojaste-Sarakhsi, M.; Mohammadigoldar, Z.; Azimi, M.; Hajati, A.; Sadabad, F.E.; Chiang, J.; McWilliams, J.P.; et al. Prediction of treatment response and outcome of transarterial chemoembolization in patients with hepatocellular carcinoma using artificial intelligence: A systematic review of efficacy. Eur. J. Radiol. 2025, 184, 111948. [Google Scholar] [CrossRef]
- Sacco, R.; Conte, C.; Tumino, E.; Parisi, G.; Marceglia, S.; Metrangolo, S.; Eggenhoffner, R.; Bresci, G.; Cabibbo, G.; Giacomelli, L. Transarterial radioembolization for hepatocellular carcinoma: A review. J. Hepatocell. Carcinoma 2016, 25, 25–29. [Google Scholar] [CrossRef]
- Galle, P.R.; Forner, A.; Llovet, J.M.; Mazzaferro, V.; Piscaglia, F.; Raoul, J.-L.; Schirmacher, P.; Vilgrain, V. EASL clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef]
- Kim, E.; Sher, A.; Abboud, G.; Schwartz, M.; Facciuto, M.; Tabrizian, P.; Knešaurek, K.; Fischman, A.; Patel, R.; Nowakowski, S.; et al. Radiation segmentectomy for curative intent of unresectable very early to early stage hepatocellular carcinoma (RASER): A single-centre, single-arm study. Lancet Gastroenterol. Hepatol. 2022, 7, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, R.J.; Gabr, A.; Abouchaleh, N.; Ali, R.; Al Asadi, A.; Mora, R.A.; Kulik, L.; Ganger, D.; Desai, K.; Thornburg, B.; et al. Radiation segmentectomy: Potential curative therapy for early hepatocellular carcinoma. Radiology 2018, 287, 1050–1058. [Google Scholar] [CrossRef]
- Lencioni, R.; Llovet, J.M. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin. Liver Dis. 2010, 30, 52–60. [Google Scholar] [CrossRef] [PubMed]
- American College of Radiology. Liver Imaging Reporting and Data System Version 2018. Published 2018. Available online: https://www.acr.org/Clinical-Resources/Clinical-Tools-and-Reference/Reporting-and-Data-Systems/LI-RADS (accessed on 1 March 2024).
- Deng, J.; Miller, F.H.; Rhee, T.K.; Sato, K.T.; Mulcahy, M.F.; Kulik, L.M.; Salem, R.; Omary, R.A.; Larson, A.C. Diffusion-weighted MR imaging for determination of hepatocellular carcinoma response to yttrium-90 radioembolization. J. Vasc. Interv. Radiol. 2006, 17, 1195–1200. [Google Scholar] [CrossRef]
- Vietti Violi, N.; Gnerre, J.; Law, A.; Hectors, S.; Bane, O.; Doucette, J.; Abboud, G.; Kim, E.; Schwartz, M.; Fiel, M.I.; et al. Assessment of HCC response to yttrium-90 radioembolization with gadoxetate disodium MRI: Correlation with histopathology. Eur. Radiol. 2022, 32, 6493–6503. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, H.C. Radioembolization for hepatocellular carcinoma: What clinicians need to know. J. Liver Cancer 2022, 22, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, B.; Chen, M.; Stocker, D.; Charles, D.; Radell, J.; Lee, J.Y.; Fauveau, V.; Bello-Martinez, R.; Kim, E.; Taouli, B. Early prediction of response of hepatocellular carcinoma to yttrium-90 radiation segmentectomy using a machine learning MR imaging radiomic approach. J. Vasc. Interv. Radiol. 2023, 34, 1794–1801.e2. [Google Scholar] [CrossRef] [PubMed]
- Stocker, D.; King, M.J.; Homsi, M.E.; Gnerre, J.; Marinelli, B.; Wurnig, M.; Fauveau, V.; Bello-Martinez, R.; Kim, E.; Taouli, B. Early post-treatment MRI predicts long-term hepatocellular carcinoma response to radiation segmentectomy. Eur. Radiol. 2024, 34, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, J.Y.; Lee, J.-H.; Sinn, D.H.; Hur, M.H.; Hong, J.H.; Park, M.K.; Cho, H.J.; Choi, N.R.; Bin Lee, Y.; et al. Long-term outcomes of transarterial radioembolization for large single hepatocellular carcinoma: A comparison to resection. J. Nucl. Med. 2022, 63, 1215–1222. [Google Scholar] [CrossRef]
- She, W.H.; Cheung, T.T.; Yau, T.C.; Chan, A.C.; Chok, K.S.; Chu, F.S.; Liu, R.K.Y.; Poon, R.T.P.; Chan, S.C.; Fan, S.T.; et al. Survival analysis of transarterial radioembolization with yttrium-90 for hepatocellular carcinoma patients with HBV infection. Hepatobiliary Surg. Nutr. 2014, 3, 185–193. [Google Scholar] [PubMed][Green Version]
- Muglia, R.; De Giorgio, M.; Marra, P.; Carbone, F.S.; Dulcetta, L.; Prussia, C.; Loglio, A.; Ghirardi, A.; Grikke, L.A.; Bianchi, C.; et al. Long-term outcomes of Yttrium-90 transarterial radioembolization for patients with hepatocellular carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2025, 8, 3114–3124. [Google Scholar] [CrossRef]
- Lee, S.H.; Son, H.S.; Cho, S.; Kim, S.J.; Yoo, D.S.; Kang, S.H.; Park, S.Y.; Park, J.; Chang, S.-G.; Jeon, S.H. Which patients should we follow up beyond 5 years after definitive therapy for localized renal cell carcinoma? Cancer Res. Treat. 2015, 47, 489–494. [Google Scholar] [CrossRef][Green Version]
- Hubbard, M.O.; Fu, P.; Margevicius, S.; Dowlati, A.; Linden, P.A. Five-year survival does not equal cure in non–small cell lung cancer: A Surveillance, Epidemiology, and End Results–based analysis of variables affecting 10-to 18-year survival. J. Thorac. Cardiovasc. Surg. 2012, 143, 1307–1313. [Google Scholar] [CrossRef] [PubMed]
- Bresnahan, E.; Ramadori, P.; Heikenwalder, M.; Zender, L.; Lujambio, A. Novel patient-derived preclinical models of liver cancer. J. Hepatol. 2020, 72, 239–249. [Google Scholar] [CrossRef]
- Sun, H.; Yang, H.; Mao, Y. Personalized treatment for hepatocellular carcinoma in the era of targeted medicine and bioengineering. Front. Pharmacol. 2023, 14, 1150151. [Google Scholar] [CrossRef] [PubMed]
- Chernyak, V.; Fowler, K.J.; Kamaya, A.; Kielar, A.Z.; Elsayes, K.M.; Bashir, M.R.; Kono, Y.; Do, R.K.; Mitchell, D.G.; Singal, A.G.; et al. Liver Imaging Reporting and Data System (LI-RADS) version 2018: Imaging of hepatocellular carcinoma in at-risk patients. Radiology 2018, 289, 816–830. [Google Scholar] [CrossRef]
- Roayaie, S.; Blume, I.N.; Thung, S.N.; Guido, M.; Fiel, M.I.; Hiotis, S.; Labow, D.M.; Llovet, J.M.; Schwartz, M.E. A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology 2009, 137, 850–855. [Google Scholar] [CrossRef]
- Moon, S.; Kim, G.M.; Won, J.Y.; Kwon, J.H.; Park, J.; Han, K.; Kim, M.-D.; Kim, H.C.; Kim, D.K.; Choi, J.Y. Clinical course of patients with hepatocellular carcinoma who experienced radiologic complete response after radioembolization. Front. Oncol. 2024, 14, 1349632. [Google Scholar] [CrossRef]
- Yu, Q.; Neale, M.; Ungchusri, E.; Rothenberger, N.J.; Liao, C.; Patel, M.; Pillai, A.; Navuluri, R.; Ahmed, O.; Van Ha, T. Tumor size and watershed area correlate with incomplete treatment and tumor progression after selective radioembolization for hepatocellular carcinoma. J. Vasc. Interv. Radiol. 2024, 35, 712–721.e3. [Google Scholar] [CrossRef]
- Jeong, S.O.; Kim, E.B.; Jeong, S.W.; Jang, J.Y.; Lee, S.H.; Kim, S.G.; Cha, S.W.; Kim, Y.S.; Cho, Y.D.; Kim, H.S.; et al. Predictive factors for complete response and recurrence after transarterial chemoembolization in hepatocellular carcinoma. Gut Liver 2017, 11, 409–416. [Google Scholar] [CrossRef]
- Cerban, R.; Ester, C.; Iacob, S.; Grasu, M.; Pâslaru, L.; Dumitru, R.; Lupescu, I.; Constantin, G.; Croitoru, A.; Gheorghe, L. Predictive Factors of Tumor Recurrence and Survival in Patients with Hepatocellular Carcinoma treated with Transarterial Chemoembolization. J. Gastrointestin Liver Dis. 2018, 27, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, J.S.; Lee, H.W.; Kim, B.K.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Kim, S.U. Predictors of complete response in patients with hepatocellular carcinoma treated with trans-arterial radioembolization. Curr. Oncol. 2021, 28, 965–977. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.-W.; Cheng, B.-Q.; Zhou, T.; Gao, Y,-J. Management of hepatocellular carcinoma patients with portal vein tumor thrombosis: A narrative review. Hepatobiliary Pancreat. Dis. Int. 2022, 21, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Leng, J.J.; Xu, Y.Z.; Dong, J.H. Efficacy of transarterial chemoembolization for hepatocellular carcinoma with portal vein thrombosis: A meta-analysis. ANZ J. Surg. 2016, 86, 816–820. [Google Scholar] [CrossRef]
- Silva, J.P.; Berger, N.G.; Tsai, S.; Christians, K.K.; Clarke, C.N.; Mogal, H.; White, S.; Rilling, W.; Gamblin, T.C. Transarterial chemoembolization in hepatocellular carcinoma with portal vein tumor thrombosis: A systematic review and meta-analysis. HPB 2017, 19, 659–666. [Google Scholar] [CrossRef]
- Weng, Z.; Ertle, J.; Zheng, S.; Lauenstein, T.; Mueller, S.; Bockisch, A.; Gerken, G.; Yang, D.; Schlaak, J.F.; Hoshida, Y. A new model to estimate prognosis in patients with hepatocellular carcinoma after Yttrium-90 radioembolization. PLoS ONE 2013, 8, e82225. [Google Scholar] [CrossRef]
- Lopez-Lopez, V.; Miura, K.; Kuemmerli, C.; Capel, A.; Eshmuminov, D.; Ferreras, D.; Baroja-Mazo, A.; Cascales-Campos, P.; Jiménez-Mascuñán, M.I.; Pons, J.A.; et al. Selecting the appropriate downstaging and bridging therapies for hepatocellular carcinoma: What is the role of transarterial radioembolization? A pooled analysis. Cancers 2023, 15, 2122. [Google Scholar] [CrossRef]
- Kim, H.C. Radioembolization for the treatment of hepatocellular carcinoma. Clin. Mol. Hepatol. 2017, 23, 109–114. [Google Scholar] [CrossRef]
- Upadhaya, T.; Vallières, M.; Chatterjee, A.; Lucia, F.; Bonaffini, P.A.; Masson, I.; Mervoyer, A.; Reinhold, C.; Schick, U.; Seuntjens, J.; et al. Comparison of radiomics models built through machine learning in a multicentric context with independent testing: Identical data, similar algorithms, different methodologies. IEEE Trans. Radiat. Plasma Med. Sci. 2018, 3, 192–200. [Google Scholar] [CrossRef]
- Vallières, M.; Zwanenburg, A.; Badic, B.; Le Rest, C.C.; Visvikis, D.; Hatt, M. Responsible radiomics research for faster clinical translation. J. Nucl. Med. 2018, 59, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Hatt, M.; Lucia, F.; Schick, U.; Visvikis, D. Multicentric validation of radiomics findings: Challenges and opportunities. EBioMedicine 2019, 47, 20–21. [Google Scholar] [CrossRef] [PubMed]
- Welch, M.L.; McIntosh, C.; Haibe-Kains, B.; Milosevic, M.F.; Wee, L.; Dekker, A.; Huang, S.H.; Purdie, T.G.; O'SUllivan, B.; Aerts, H.J.; et al. Vulnerabilities of radiomic signature development: The need for safeguards. Radiother. Oncol. 2019, 130, 2–9. [Google Scholar] [CrossRef]
- Schmoor, C.; Sauerbrei, W.; Schumacher, M. Sample size considerations for the evaluation of prognostic factors in survival analysis. Stat. Med. 2000, 19, 441–452. [Google Scholar] [CrossRef]

| Characteristic | CR Group | Non-CR Group | p Value | Total |
|---|---|---|---|---|
| No. of patients | 9 | 28 | 37 | |
| Age (years) | 65 (52–69) | 64 (54–74) | 0.726 | 64 (53–72) |
| Sex (men), n (%) | 7 (77.8) | 23 (82.1) | 0.556 | 30 (81.1) |
| Cirrhosis, n (%) | 5 (55.6) | 15 (53.6) | 0.612 | 20 (54.1) |
| Child–Pugh class, n (%) | 0.578 | |||
| A | 8 (88.9) | 26 (92.9) | 34 (91.9) | |
| B | 1 (11.1) | 2 (7.1) | 3 (8.1) | |
| MELD score | 7.4 (6.0–8.0) | 7.5 (6.0–8.0) | 0.889 | 7.5 (6.0–8.0) |
| Tumor characteristics | ||||
| Diameter of largest tumor (cm) | 5.9 (4.8–6.8) | 9.8 (6.8–12.0) | 0.006 | 7.6 (6.2–11.6) |
| Diameter of largest tumor, n (%) | 0.004 | |||
| ≤7 cm | 8 (88.9) | 9 (32.1) | 17 (45.9) | |
| >7 cm | 1 (11.1) | 19 (67.9) | 20 (54.1) | |
| Tumor epicenter, n (%) | 0.444 | |||
| Right | 8 (88.9) | 22 (78.6) | 30 (81.1) | |
| Left | 1 (11.1) | 6 (21.4) | 7 (18.9) | |
| Number of main tumors | 1 (1–1) | 1 (1–2) | 0.256 | 2 (1–2) |
| Presence of satellite nodule, n (%) | 1 (11.1) | 6 (21.4) | 0.444 | 7 (18.9) |
| Tumor enhancement pattern, n (%) | 0.432 | |||
| Typical enhancement | 8 (88.9) | 27 (96.4) | 35 (94.6) | |
| Atypical enhancement | 1 (11.1) | 1 (3.6) | 2 (5.4) | |
| Tumor margin, n (%) | 0.543 | |||
| Smooth | 8 (88.9) | 23 (82.1) | 31 (83.8) | |
| Irregular | 1 (11.1) | 5 (17.9) | 6 (16.2) | |
| Portal vein thrombosis, n (%) | 1 (11.1) | 13 (46.4) | 0.062 | 14 (37.8) |
| Hepatic vein invasion, n (%) | 1 (11.1) | 1 (3.6) | 0.432 | 2 (5.4) |
| Ascites | 0.471 | |||
| None | 5 (55.6) | 10 (35.7) | 15 (40.5) | |
| Small amount | 4 (44.4) | 16 (57.1) | 20 (54.1) | |
| Moderate to large amount | 0 (0.0) | 2 (7.1) | 2 (5.4) | |
| Laboratory data | ||||
| Alpha-fetoprotein (ng/mL) | 2.7 (2.3–5.2) | 3.1 (2.0–6.2) | 0.419 | 3.0 (2.2–5.5) |
| PIVKA-II (mAU/mL) | 153.0 (22.0–14,430.0) | 316.5 (103.8–3766.0) | 0.232 | 302.0 (77.0–3677.0) |
| Total bilirubin (mg/dL) | 0.9 (0.7–1.3) | 0.8 (0.5–1.0) | 0.915 | 0.8 (0.6–1.0) |
| Albumin (g/dL) | 3.7 (3.3–4.1) | 3.7 (3.3–4.0) | 0.654 | 3.7 (3.3–4.0) |
| AST (IU/L) | 49.0 (35.0–54.0) | 55.0 (32.3–81.5) | 0.319 | 52.0 (32.5–77.0) |
| ALT (IU/L) | 24.0 (19.5–42.5) | 32.5 (19.3–40.8) | 0.336 | 31.0 (19.5–40.5) |
| Platelet (1000/μL) | 221.0 (119.5–256.0) | 195.5 (169.5–274.0) | 0.345 | 202.0 (157.0–272.0) |
| PT-INR | 1.0 (0.9–1.1) | 1.0 (1.0–1.1) | 0.664 | 1.0 (1.0–1.1) |
| Interval periods (days) | 20 (16–22) | 16 (13–21) | 0.102 | 17 (13–21) |
| Lung shunt (%) | 5.7 (4.2–9.8) | 4.9 (3.2–7.6) | 0.759 | 5.3 (3.4–7.9) |
| Variables | Univariable Analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Age | 0.874 | 0.780–0.979 | 0.556 | |||
| MELD score | 0.956 | 0.856–1.055 | 0.757 | |||
| Diameter of largest tumor | ||||||
| ≤7 cm | Reference | |||||
| >7 cm | 16.949 | 1.825–166.667 | 0.013 | 21.277 | 2.066–200.000 | 0.010 |
| Number of main tumors | 4.293 | 0.503–36.673 | 0.183 | |||
| Presence of satellite nodule | 0.458 | 0.048–4.420 | 0.500 | |||
| Portal vein thrombosis | 6.933 | 0.762–63.047 | 0.086 | 9.779 | 0.881–108.595 | 0.063 |
| Hepatic vein invasion | 3.375 | 0.189–60.238 | 0.408 | |||
| Alpha-fetoprotein (ng/mL) | 1.051 | 0.871–1.267 | 0.605 | |||
| PIVKA-II | 2.852 | 0.973–7.330 | 0.244 | |||
| Interval periods | 0.862 | 0.719–1.033 | 0.108 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.; Kim, D.K.; Lee, S.; Hwang, S.H. Assessment of Preprocedural Factors Associated with 5-Year Complete Response After Transarterial Radioembolization in Patients with Hepatocellular Carcinoma. Diagnostics 2025, 15, 2297. https://doi.org/10.3390/diagnostics15182297
Park J, Kim DK, Lee S, Hwang SH. Assessment of Preprocedural Factors Associated with 5-Year Complete Response After Transarterial Radioembolization in Patients with Hepatocellular Carcinoma. Diagnostics. 2025; 15(18):2297. https://doi.org/10.3390/diagnostics15182297
Chicago/Turabian StylePark, June, Dong Kyu Kim, Seungsoo Lee, and Shin Hye Hwang. 2025. "Assessment of Preprocedural Factors Associated with 5-Year Complete Response After Transarterial Radioembolization in Patients with Hepatocellular Carcinoma" Diagnostics 15, no. 18: 2297. https://doi.org/10.3390/diagnostics15182297
APA StylePark, J., Kim, D. K., Lee, S., & Hwang, S. H. (2025). Assessment of Preprocedural Factors Associated with 5-Year Complete Response After Transarterial Radioembolization in Patients with Hepatocellular Carcinoma. Diagnostics, 15(18), 2297. https://doi.org/10.3390/diagnostics15182297






