Diagnostic Efficacy of Cervical Elastography in Predicting Spontaneous Preterm Birth in Pregnancies with Threatened Preterm Labor †
Abstract
1. Introduction
2. Materials and Methods
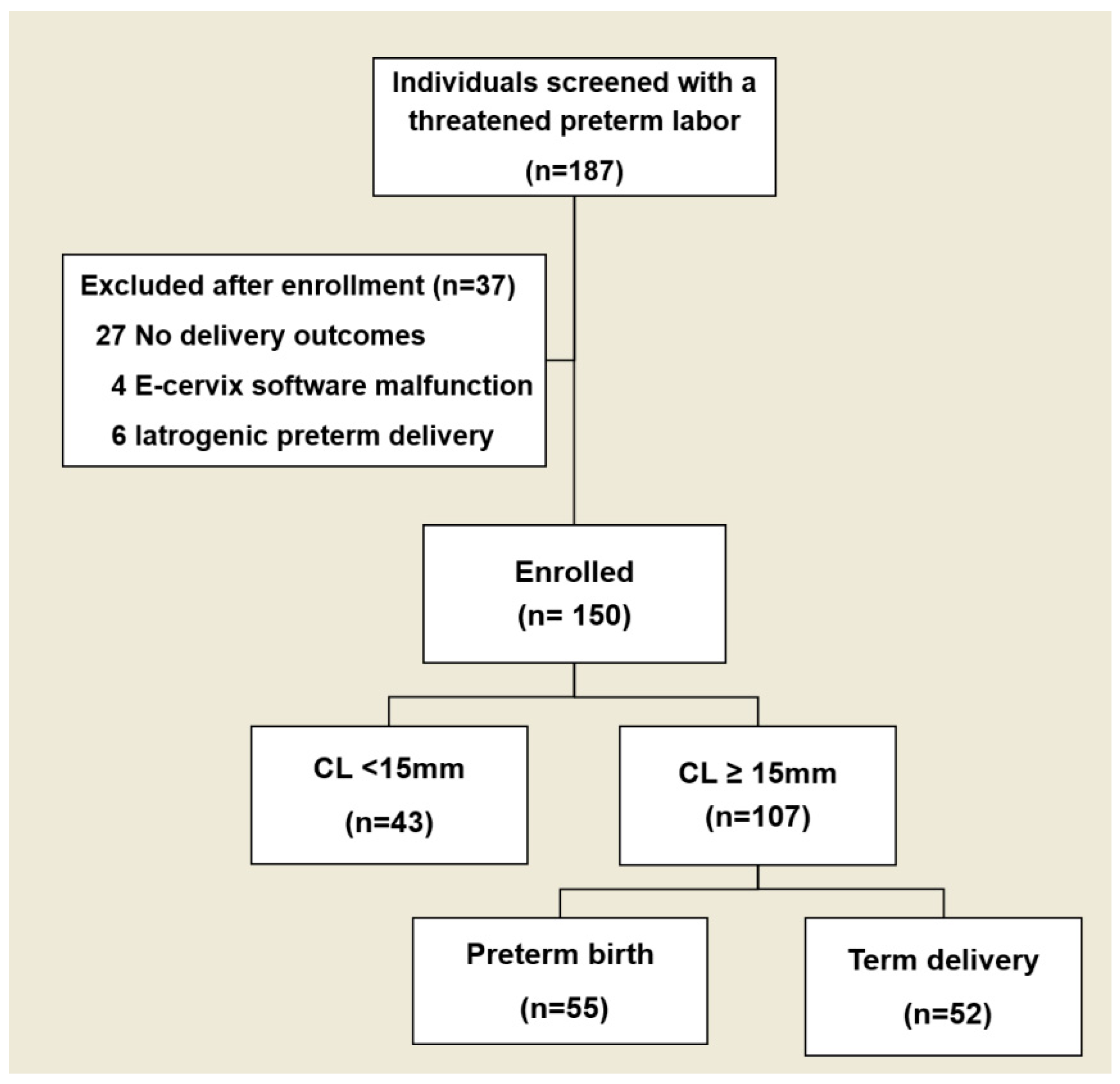
2.1. Study Population
2.2. Maternal Clinical Variables
2.3. Cervical Length and Elastographic Measurements
2.4. Statistical Analysis
3. Result
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Slattery, M.M.; Morrison, J.J. Preterm delivery. Lancet 2002, 360, 1489–1497. [Google Scholar] [CrossRef] [PubMed]
- Abadi, M.; Agarwal, A.; Barham, P.; Brevdo, E.; Chen, Z.; Citro, C.; Corrado, G.S.; Davis, A.; Dean, J.; Devin, M.; et al. TensorFlow: Large-Scale Machine Learning on Heterogeneous Distributed Systems. arXiv 2016, arXiv:1603.04467. [Google Scholar]
- Eroglu, D.; Yanık, F.; Oktem, M.; Zeyneloglu, H.B.; Kuscu, E. Prediction of preterm delivery among women with threatened preterm labor. Gynecol Obs. Investig. 2007, 64, 109–116. [Google Scholar] [CrossRef]
- Blencowe, H.; Cousens, S.; Oestergaard, M.Z.; Chou, D.; Moller, A.-B.; Narwal, R.; Adler, A.; Vera Garcia, C.; Rohde, S.; Say, L.; et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet 2012, 379, 2162–2172. [Google Scholar] [CrossRef]
- Ohuma, E.O.; Moller, A.-B.; Bradley, E.; Chakwera, S.; Hussain-Alkhateeb, L.; Lewin, A.; Okwaraji, Y.B.; Mahanani, W.R.; Johansson, E.W.; Lavin, T.; et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet 2023, 402, 1261–1271. [Google Scholar] [CrossRef]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Dagklis, T.; Akolekar, R.; Villalain, C.; Tsakiridis, I.; Kesrouani, A.; Tekay, A.; Plasencia, W.; Wellmann, S.; Kusuda, S.; Jekova, N.; et al. Management of preterm labor: Clinical practice guideline and recommendation by the WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine Foundation. Eur. J. Obstet. Gynecol. Reprod. Biol. 2023, 291, 196–205. [Google Scholar] [CrossRef]
- Lewis, M.; Passant, L.; Cooke, H.; Challis, D. Women’s experiences of antenatal transfer for threatened premature labour in NSW: A qualitative study. Women Birth 2020, 33, e535–e542. [Google Scholar] [CrossRef]
- Chawanpaiboon, S.; Pimol, K.; Sirisomboon, R. Comparison of success rate of nifedipine, progesterone, and bed rest for inhibiting uterine contraction in threatened preterm labor. J. Obstet. Gynaecol. Res. 2011, 37, 787–791. [Google Scholar] [CrossRef]
- Chiossi, G.; Facchinetti, F.; Vergani, P.; Di Tommaso, M.; Marozio, L.; Acaia, B.; Pignatti, L.; Locatelli, A.; Spitaleri, M.; Benedetto, C.; et al. Serial cervical-length measurements after first episode of threatened preterm labor improve prediction of spontaneous delivery prior to 37 weeks’ gestation. Ultrasound Obstet. Gynecol. 2021, 57, 298–304. [Google Scholar] [CrossRef]
- Rennert, K.N.; Breuking, S.H.; Schuit, E.; Bekker, M.N.; Woiski, M.; de Boer, M.A.; Sueters, M.; Scheepers, H.C.J.; Franssen, M.T.M.; Pajkrt, E.; et al. Change in cervical length after arrested preterm labor and risk of preterm birth. Ultrasound Obstet. Gynecol. 2021, 58, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Newman, R.B.; Goldenberg, R.L.; Iams, J.D.; Meis, P.J.; Mercer, B.M.; Moawad, A.H.; Thom, E.; Miodovnik, M.; Caritis, S.N.; Dombrowski, M. Preterm prediction study: Comparison of the cervical score and Bishop score for prediction of spontaneous preterm delivery. Obstet. Gynecol. 2008, 112, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Berghella, V.; Saccone, G. Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database Syst. Rev. 2019, 2019, CD006843. [Google Scholar] [CrossRef] [PubMed]
- Gyokova, E.H.; Ivanova-Yoncheva, Y.G.; Popov, Y.D.; Anzaar, A.A.; Pradip, G.; Bhamidipati, S.; Owusu, H.; Yogeswaran, K. Determination of preterm labour with pIGFBP-1 and cervical biometrics. Folia Medica 2022, 64, 302–308. [Google Scholar] [CrossRef]
- Lucovnik, M.; Kuon, R.J.; Chambliss, L.R.; Maner, W.L.; Shi, S.Q.; Shi, L.; Balducci, J.; Garfield, R.E. Use of uterine electromyography to diagnose term and preterm labor. Acta Obstet. Gynecol. Scand. 2011, 90, 150–157. [Google Scholar] [CrossRef]
- Mas-Cabo, J.; Prats-Boluda, G.; Perales, A.; Garcia-Casado, J.; Alberola-Rubio, J.; Ye-Lin, Y. Uterine electromyography for discrimination of labor imminence in women with threatened preterm labor under tocolytic treatment. Med. Biol. Eng. Comput. 2019, 57, 401–411. [Google Scholar] [CrossRef]
- Olgan, S.; Celiloglu, M. Contraction-based uterine artery Doppler velocimetry: Novel approach for prediction of preterm birth in women with threatened preterm labor. Ultrasound Obstet. Gynecol. 2016, 48, 757–764. [Google Scholar] [CrossRef]
- Kim, H.; Hwang, H.S. Elastographic measurement of the cervix during pregnancy: Current status and future challenges. Obstet. Gynecol. Sci. 2017, 60, 1–7. [Google Scholar] [CrossRef]
- Park, H.S.; Kwon, H.; Kwak, D.W.; Kim, M.Y.; Seol, H.-J.; Hong, J.-S.; Shim, J.-Y.; Choi, S.-K.; Hwang, H.-S.; Oh, M.J.; et al. Addition of Cervical Elastography May Increase Preterm Delivery Prediction Performance in Pregnant Women with Short Cervix: A Prospective Study. J. Korean Med. Sci. 2019, 34, e68. [Google Scholar] [CrossRef]
- Patberg, E.T.; Wells, M.; Vahanian, S.A.; Zavala, J.; Bhattacharya, S.; Richmond, D.; Akerman, M.; Demishev, M.; Kinzler, W.L.; Chavez, M.R.; et al. Use of cervical elastography at 18 to 22 weeks’ gestation in the prediction of spontaneous preterm birth. Am. J. Obstet. Gynecol. 2021, 225, 525.e521–525.e529. [Google Scholar] [CrossRef]
- Nazzaro, G.; Saccone, G.; Miranda, M.; Ammendola, A.; Buonomo, G.; Neola, D.; Bartolini, G.; Locci, M. Cervical elastography using E-Cervix™ for prediction of preterm birth in twin pregnancies with threatened preterm labor. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 298, 104–107. [Google Scholar] [CrossRef]
- Jung, Y.J.; Kwon, H.; Shin, J.; Park, Y.; Heo, S.J.; Park, H.S.; Oh, S.Y.; Sung, J.H.; Seol, H.J.; Kim, H.M.; et al. The Feasibility of Cervical Elastography in Predicting Preterm Delivery in Singleton Pregnancy with Short Cervix Following Progesterone Treatment. Int. J. Environ. Res. Public Health 2021, 18, 2026. [Google Scholar] [CrossRef] [PubMed]
- Nazzaro, G.; Saccone, G.; Miranda, M.; Crocetto, F.; Zullo, F.; Locci, M. Cervical elastography using E-cervix for prediction of preterm birth in singleton pregnancies with threatened preterm labor. J. Matern. Fetal Neonatal Med. 2022, 35, 330–335. [Google Scholar] [CrossRef]
- Seol, H.-J.; Sung, J.-H.; Seong, W.J.; Kim, H.M.; Park, H.S.; Kwon, H.; Hwang, H.-S.; Jung, Y.J.; Kwon, J.-Y.; Oh, S.-Y. Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters. Obstet. Gynecol. Sci. 2019, 63, 42–54. [Google Scholar] [CrossRef]
- Waks, A.B.; Martinez-King, L.C.; Santiago, G.; Laurent, L.C.; Jacobs, M.B. Developing a risk profile for spontaneous preterm birth and short interval to delivery among patients with threatened preterm labor. Am. J. Obstet. Gynecol. MFM 2022, 4, 100727. [Google Scholar] [CrossRef]

| Term Delivery (n = 66) | Preterm Birth (n = 84) | p-Value | |
|---|---|---|---|
| Age (year) | 33 (26–42) | 34 (21–40) | 0.64 |
| nulliparity | 44 (66.7) | 50 (59.5) | 0.40 |
| Pre-pregnancy BMI | 24.42 (18.31–31.30) | 24.30 (17.62–35.71) | 0.86 |
| Smoking | 0 (0) | 1 (1.2) | 1.00 |
| Twin pregnancy | 8 (12.1) | 29 (34.5) | <0.01 |
| Prior preterm birth | 4 (6.1) | 11 (13.1) | 0.18 |
| History of LEEP | 0 (0) | 5 (6.0) | 0.07 |
| DM | 1 (1.5) | 1 (1.2) | 1.00 |
| HTN | 0 (0.0) | 2 (2.4) | 0.50 |
| GDM | 9 (15.0) | 11 (13.3) | 0.81 |
| Preeclampsia | 1 (1.7) | 3 (3.6) | 0.64 |
| GA at exam (weeks) | 29.0 ± 3.3 | 28.9 ± 3.6 | 0.86 |
| CL at exam (mm) | 25.4 (9.0–45.0) | 18.7 (2.7–41.8) | <0.01 |
| <15 mm | 14 (21.2) | 29 (34.5) | |
| 15 mm–25 mm | 22 (33.3) | 37 (44.1) | |
| >25 mm | 30 (45.5) | 18 (21.4) | |
| Funneling | 9 (13.6) | 26 (31.0) | 0.02 |
| Cerclage after enrollment | 0 (0) | 2 (2.4) | 0.50 |
| Tocolytics after enrollment | 58 (87.9) | 78 (94.0) | 0.25 |
| Progesterone after enrollment | 27 (40.9) | 39 (47.0) | 0.51 |
| GA at delivery (days) | 38.7 ± 1.0 | 33.8 ± 2.7 | <0.01 |
| Cesarean delivery | 31 (47.0) | 26 (31.3) | 0.06 |
| Term Delivery (n = 52) | Preterm Birth (n = 55) | p-Value | |
|---|---|---|---|
| Age (year) | 32 (27–42) | 34 (21–40) | 0.46 |
| Nulliparity | 34 (65.4) | 36 (65.5) | 1.00 |
| Pre-pregnancy BMI | 24.35 (18.31–31.31) | 24.03 (18.65–32.30) | 0.82 |
| Smoking | 0 (0) | 1 (1.8) | 1.00 |
| Twin pregnancy | 6 (11.5) | 18 (32.7) | 0.01 |
| Prior preterm birth | 4 (7.7) | 6 (10.9) | 0.74 |
| History of LEEP | 0 (0) | 3 (5.5) | 0.24 |
| DM | 1 (1.9) | 1 (1.8) | 1.00 |
| HTN | 0 (0.0) | 2 (3.6) | 0.50 |
| GA at exam (weeks) | 28.6 ± 3.51 | 28.4 ± 3.81 | 0.95 |
| CL at exam (mm) | 27.5 (15.0–45.0) | 21.9 (15.0–41.8) | <0.01 |
| ≤25 mm | 22 (42.3) | 37 (67.3) | |
| >25 mm. | 30 (57.7) | 18 (32.7) | |
| Funneling | 4 (7.7) | 10 (18.2) | 0.15 |
| Tocolytics after enrollment | 46 (88.5) | 50 (92.6) | 0.52 |
| Progesterone after enrollment | 19 (36.5) | 20 (37.0) | 1.00 |
| GA at delivery (days) | 38.7 ± 1.05 | 33.9 ± 2.53 | <0.01 |
| Parameters | Term Delivery (n = 52) | Preterm Birth (n = 55) | p-Value |
|---|---|---|---|
| IOS | 0.26 (0.17–0.45) | 0.30 (0.18–0.50) | 0.04 |
| EOS | 0.32 (0.19–0.56) | 0.32 (0.12-0.51) | 0.37 |
| IOS/EOS ratio | 0.84 (0.36–1.55) | 0.99 (0.63–1.95) | 0.02 |
| ECI | 3.33 (1.99–5.72) | 3.62 (2.46–6.67) | 0.04 |
| HR | 65.90 (27.78–77.42) | 59.37 (24.90–87.65) | 0.17 |
| p-Value | aOR | 95% CI | |
|---|---|---|---|
| CL ≤ 25 mm | 0.02 | 2.62 | 1.17–5.89 |
| Twin pregnancy | 0.09 | 2.69 | 0.86–8.41 |
| IOS | 0.18 | 1.46 | 0.84–2.51 |
| IOS/EOS ratio | 0.01 | 10.45 | 1.82–59.98 |
| ECI | 0.04 | 1.55 | 1.01–2.37 |
| ROC/AUC | 95% CI | p-Value | Cutoff | Sensitivity (%) | Specificity (%) | Youden Index | |
|---|---|---|---|---|---|---|---|
| CL ≤ 25 mm | 0.63 | 0.52–0.73 | 0.03 | 62.7 | 62.5 | 0.25 | |
| IOS/EOS ratio | 0.68 | 0.58–0.78 | <0.01 | ≥0.96 | 65.5 | 30.8 | 0.35 |
| ECI | 0.61 | 0.51–0.72 | 0.04 | ≥3.21 | 70.9 | 51.9 | 0.19 |
| Models for predicting preterm birth | |||||||
| CL ≤ 25 mm + IOS/EOS ratio | 0.71 | 0.61–0.81 | <0.01 | ≥0.87 | 73.0 | 54.5 | 0.41 |
| CL ≤ 25 mm + ECI | 0.68 | 0.58–0.78 | <0.01 | ≥2.99 | 83.8 | 59.1 | 0.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, H.; Sung, J.-H.; Park, H.S.; Kwon, J.-Y.; Jung, Y.J.; Seol, H.-J.; Kim, H.M.; Seong, W.J.; Hwang, H.S.; Oh, S.-Y.; et al. Diagnostic Efficacy of Cervical Elastography in Predicting Spontaneous Preterm Birth in Pregnancies with Threatened Preterm Labor. Diagnostics 2025, 15, 1934. https://doi.org/10.3390/diagnostics15151934
Kwon H, Sung J-H, Park HS, Kwon J-Y, Jung YJ, Seol H-J, Kim HM, Seong WJ, Hwang HS, Oh S-Y, et al. Diagnostic Efficacy of Cervical Elastography in Predicting Spontaneous Preterm Birth in Pregnancies with Threatened Preterm Labor. Diagnostics. 2025; 15(15):1934. https://doi.org/10.3390/diagnostics15151934
Chicago/Turabian StyleKwon, Hayan, Ji-Hee Sung, Hyun Soo Park, Ja-Young Kwon, Yun Ji Jung, Hyun-Joo Seol, Hyun Mi Kim, Won Joon Seong, Han Sung Hwang, Soo-Young Oh, and et al. 2025. "Diagnostic Efficacy of Cervical Elastography in Predicting Spontaneous Preterm Birth in Pregnancies with Threatened Preterm Labor" Diagnostics 15, no. 15: 1934. https://doi.org/10.3390/diagnostics15151934
APA StyleKwon, H., Sung, J.-H., Park, H. S., Kwon, J.-Y., Jung, Y. J., Seol, H.-J., Kim, H. M., Seong, W. J., Hwang, H. S., Oh, S.-Y., & on behalf of The Korean Consortium for the Study of Cervical Elastography in Prediction of Preterm Delivery. (2025). Diagnostic Efficacy of Cervical Elastography in Predicting Spontaneous Preterm Birth in Pregnancies with Threatened Preterm Labor. Diagnostics, 15(15), 1934. https://doi.org/10.3390/diagnostics15151934







