Clinical and Imaging Characteristics to Discriminate Between Complicated and Uncomplicated Acute Cholecystitis: A Regression Model and Decision Tree Analysis
Abstract
1. Introduction
2. Methods
2.1. Definition of Acute Complicated Cholecystitis (ACC)
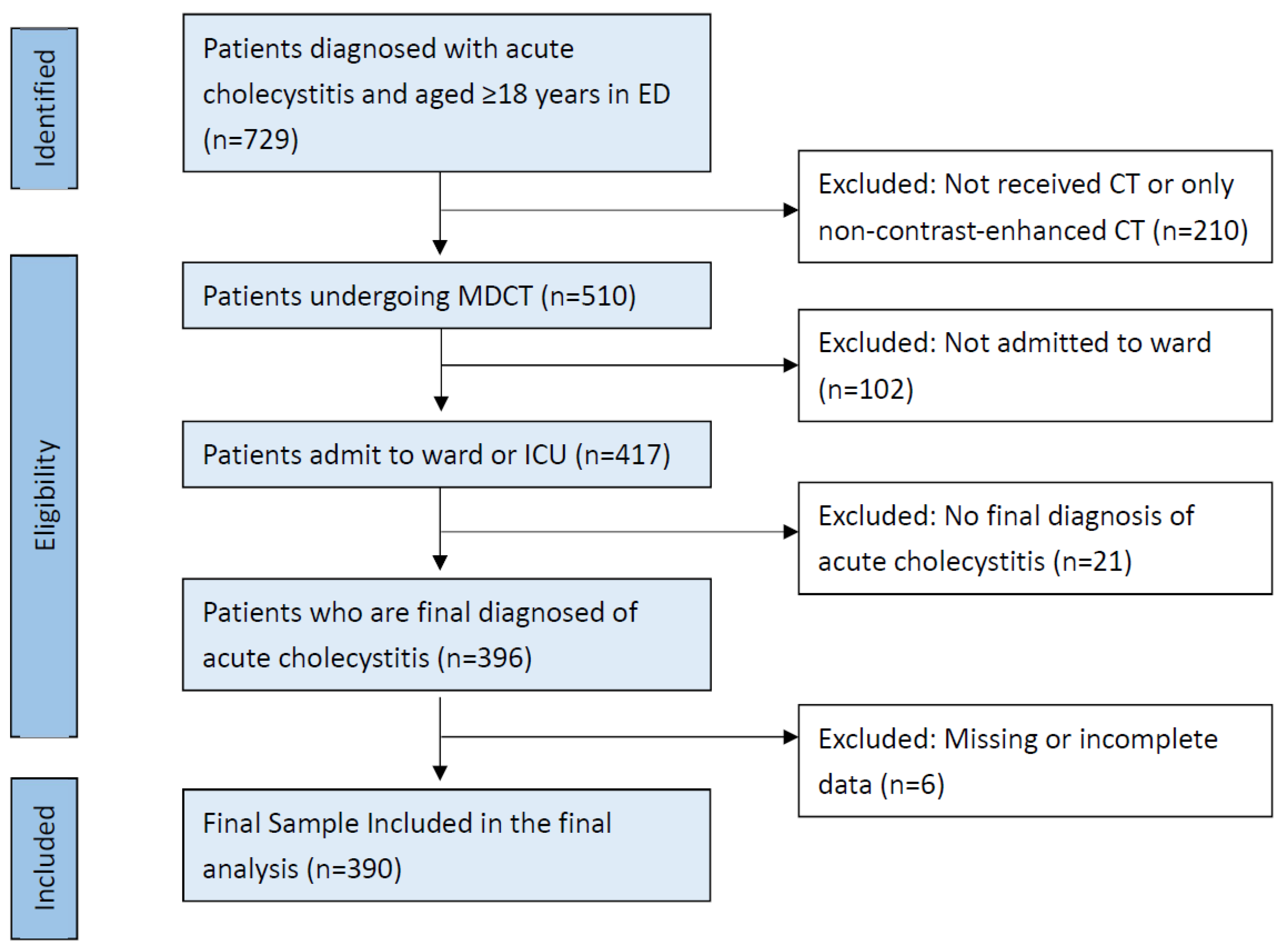
2.2. Study Design and Data Collection
2.3. Variables and Biomarkers
2.4. CT Imaging Protocol
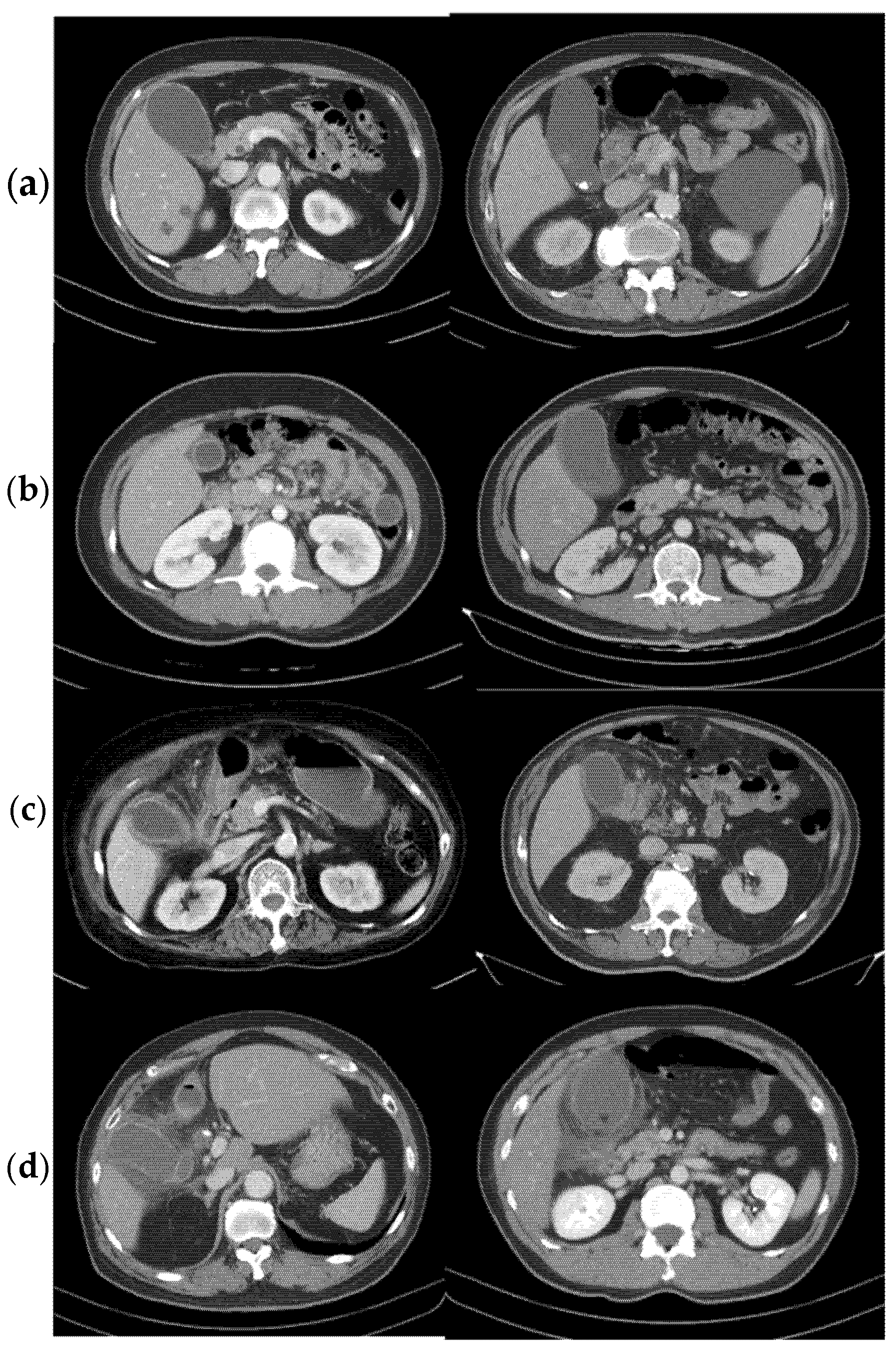
2.5. CT Features Related to Acute Cholecystitis
2.6. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Clinical Outcomes
3.3. Laboratory Markers and Radiographic Features
3.4. Predictors of Complicated Group from Univariate Analysis
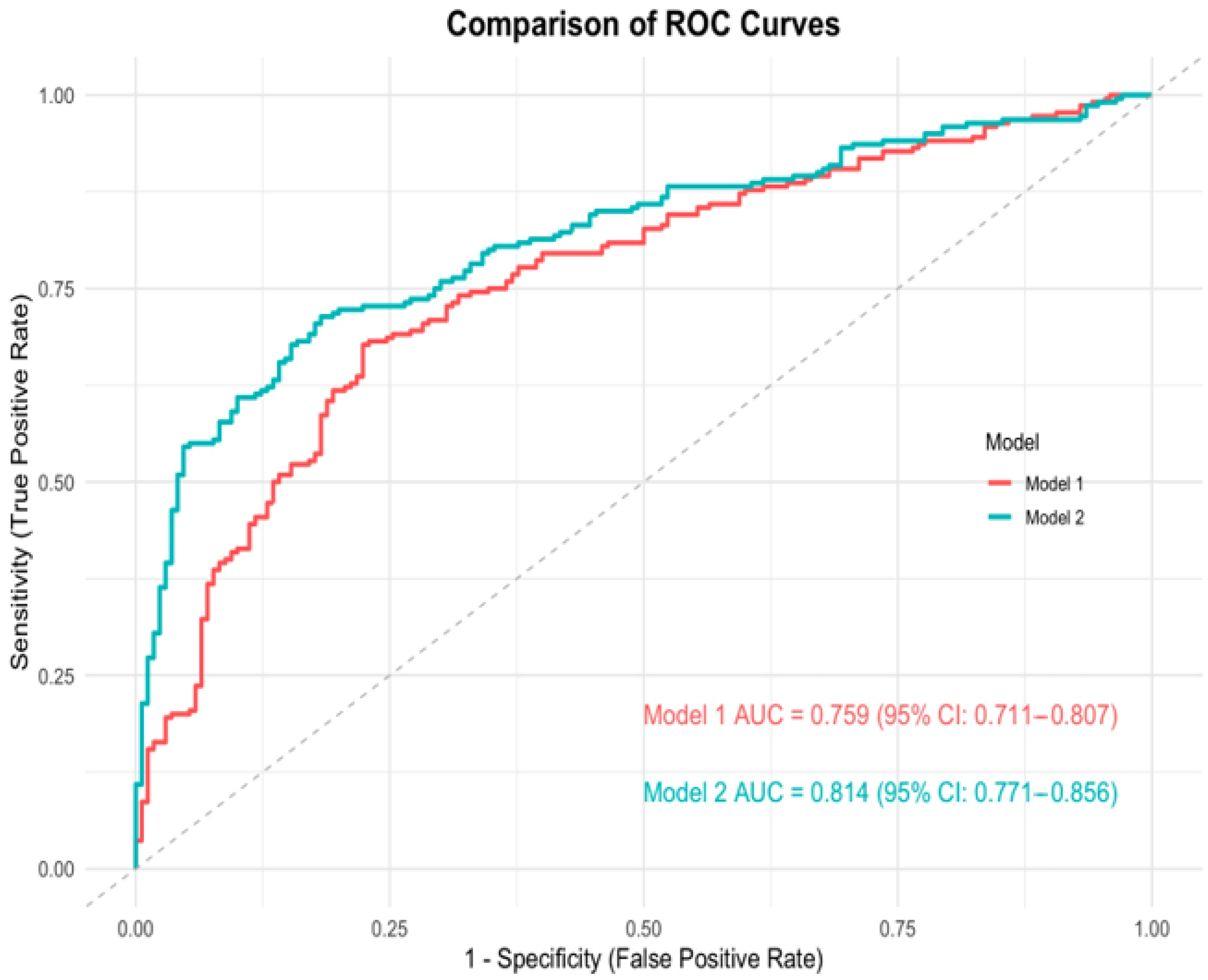
3.5. Multivariable Models for Identifying the Complicated Group
3.6. The Novel Scoring System for Predicting ACC
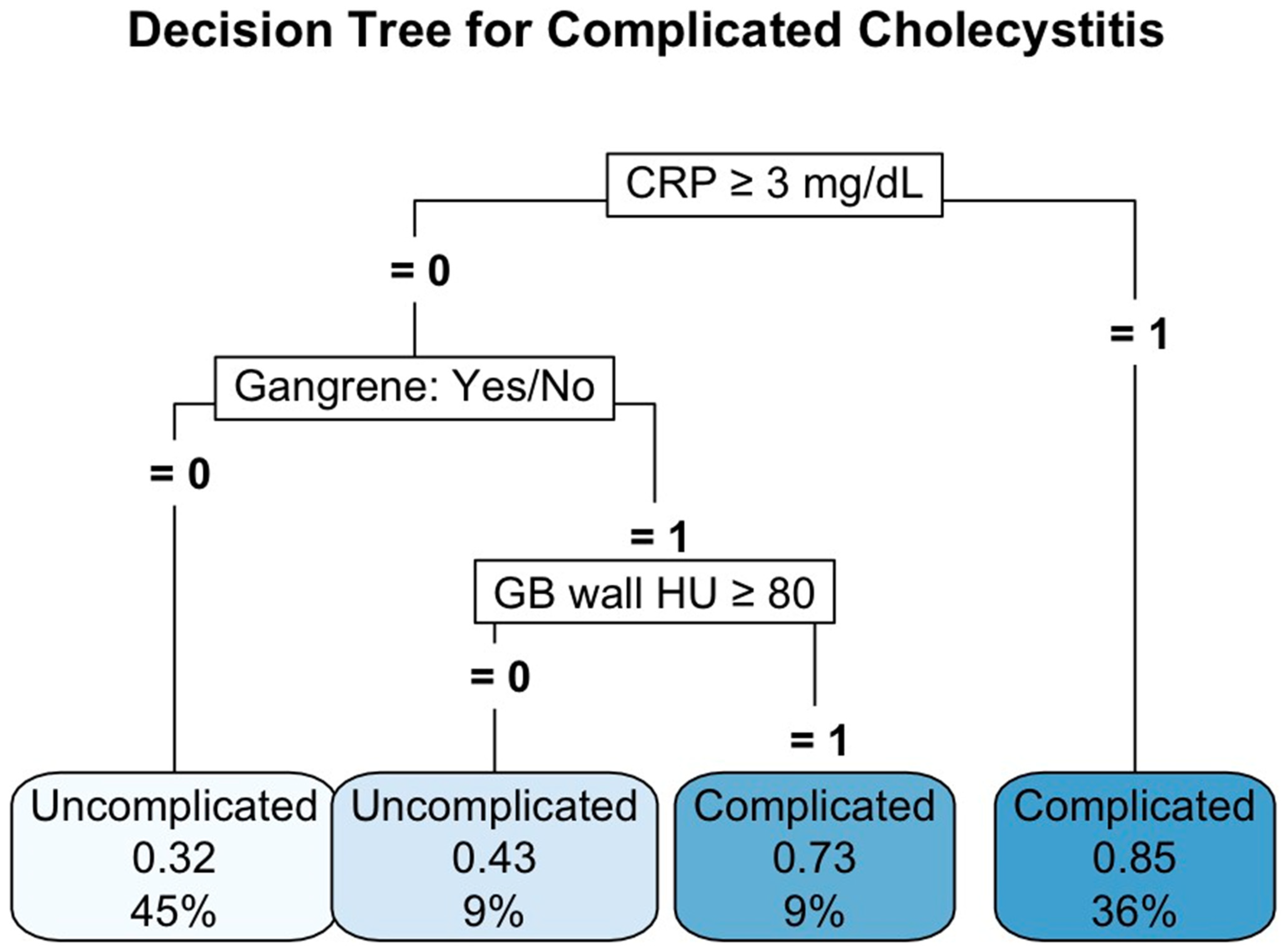
3.7. Decision Tree Analysis for Predicting ACC
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| GB | Gallbladder |
| ED | Emergency department |
| ACC | Acute complicated cholecystitis |
| LOS | Length of stay |
| CT | Computed tomography |
| MDCT | Multidetector computed tomography |
| PTGBD | Percutaneous transhepatic gallbladder drainage |
| TG18 | Tokyo Guideline 2018 |
| ICD–10–CM | International Statistical Classification of Diseases, Tenth Revision, Clinical Modification |
| GCS | Glasgow coma scale score |
| CCI | Charlson comorbidity index |
| HU | Hounsfield units |
| ANOVA | Analysis of Variance |
| ORs | Odds ratios |
| CI | Confidence intervals |
| AUC | Area under the curve |
| ROC | Receiver operating characteristic |
| CART | Classification and regression tree |
| DM | Diabetes mellitus |
| CKD | Chronic kidney disease |
| FiO2 | Mean fraction of inspired oxygen |
| WBC | White blood cell |
| CRP | C-reactive protein |
| NLR | Neutrophil-to-lymphocyte ratio |
| LMR | Lymphocyte-to-monocyte ratio |
References
- Fuks, D.; Mouly, C.; Robert, B.; Hajji, H.; Yzet, T.; Regimbeau, J.M. Acute cholecystitis: Preoperative CT can help the surgeon consider conversion from laparoscopic to open cholecystectomy. Radiology 2012, 263, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Charalel, R.A.; Jeffrey, R.B.; Shin, L.K. Complicated cholecystitis: The complementary roles of sonography and computed tomography. Ultrasound Q. 2011, 27, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.W.; Tsai, C.H.; Lin, H.A.; Chen, Y.; Hou, S.K.; Lin, S.F. Pericholecystic Fat Stranding as a Predictive Factor of Length of Stays of Patients with Acute Cholecystitis: A Novel Scoring Model. J. Clin. Med. 2024, 13, 5734. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ausania, F.; Guzman Suarez, S.; Alvarez Garcia, H.; Senra del Rio, P.; Casal Nuñez, E. Gallbladder perforation: Morbidity, mortality and preoperative risk prediction. Surg. Endosc. 2015, 29, 955–960. [Google Scholar] [CrossRef] [PubMed]
- Wertz, J.R.; Lopez, J.M.; Olson, D.; Thompson, W.M. Comparing the Diagnostic Accuracy of Ultrasound and CT in Evaluating Acute Cholecystitis. Am. J. Roentgenol. 2018, 211, W92–W97. [Google Scholar] [CrossRef]
- Ralls, P.W.; Colletti, P.M.; Lapin, S.A.; Chandrasoma, P.; Boswell, W.D., Jr.; Ngo, C.; Radin, D.R.; Halls, J.M. Real-time sonography in suspected acute cholecystitis. Prospective evaluation of primary and secondary signs. Radiology. 1985, 155, 767–771. [Google Scholar] [CrossRef]
- Pinto, A.; Reginelli, A.; Cagini, L.; Coppolino, F.; Stabile Ianora, A.A.; Bracale, R.; Giganti, M.; Romano, L. Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: Review of the literature. Crit. Ultrasound J. 2013, 5, S11. [Google Scholar] [CrossRef]
- Shapira-Rootman, M.; Mahamid, A.; Reindorp, N.; Nachtigal, A.; Zeina, A.R. Sonographic Diagnosis of Complicated Cholecystitis. J Ultrasound Med. 2015, 34, 2231–2236. [Google Scholar] [CrossRef] [PubMed]
- Yokoe, M.; Hata, J.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Wakabayashi, G.; Kozaka, K.; Endo, I.; Deziel, D.D.; Miura, F.; et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholecystitis (with videos). J. Hepato-Biliary-Pancreat. Sci. 2018, 25, 41–54. [Google Scholar] [CrossRef]
- Khan, S.M.; Emile, S.H.; Barsom, S.H.; Naqvi, S.A.A.; Khan, M.S. Accuracy of pre-operative parameters in predicting severe cholecystitis-A systematic review. Surgeon 2021, 19, 219–225. [Google Scholar] [CrossRef]
- Zainal, I.A.; Kew, T.Y.; Othman, H.A. Retrospective analysis of the sonographic and computed tomographic features of gallbladder empyema. Emerg. Radiol. 2022, 29, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.C.; Sun, Y.; Wu, E.H.; Kim, S.Y.; Wang, Z.J.; Huang, G.S.; Yeh, B.M. CT Findings for Detecting the Presence of Gangrenous Ischemia in Cholecystitis. Am. J. Roentgenol. 2016, 207, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kim, S.J.; Lee, S.C.; Lee, S.K. Risk assessment scales and predictors for simple versus severe cholecystitis in performing laparoscopic cholecystectomy. Asian J. Surg. 2017, 40, 367–374. [Google Scholar] [CrossRef]
- Sureka, B.; Jha, S.; Rodha, M.S.; Chaudhary, R.; Elhence, P.; Khera, P.S.; Grag, P.K.; Yadav, T.; Goel, A. Combined hyperdense gallbladder wall-lumen sign: New computed tomography sign in acute gangrenous cholecystitis. Pol. J. Radiol. 2020, 85, e183–e187. [Google Scholar] [CrossRef]
- Huang, S.Z.; Chen, H.Q.; Liao, W.X.; Zhou, W.Y.; Chen, J.H.; Li, W.C.; Zhou, H.; Liu, B.; Hu, K.P. Comparison of emergency cholecystectomy and delayed cholecystectomy after percutaneous transhepatic gallbladder drainage in patients with acute cholecystitis: A systematic review and meta-analysis. Updates Surg. 2021, 73, 481–494. [Google Scholar] [CrossRef]
- Ke, C.W.; Wu, S.D. Comparison of Emergency Cholecystectomy with Delayed Cholecystectomy After Percutaneous Transhepatic Gallbladder Drainage in Patients with Moderate Acute Cholecystitis. J. Laparoendosc. Adv. Surg. Tech. 2018, 6, 705–712. [Google Scholar] [CrossRef]
- Lin, D.; Wu, S.; Fan, Y.; Ke, C. Comparison of laparoscopic cholecystectomy and delayed laparoscopic cholecystectomy in aged acute calculous cholecystitis: A cohort study. Surg. Endosc. 2020, 34, 2994–3001. [Google Scholar] [CrossRef]
- Tan, H.Y.; Jiang, D.D.; Li, J.; He, K.; Yang, K. Percutaneous Transhepatic Gallbladder Drainage Combined with Laparoscopic Cholecystectomy: A Meta-Analysis of Randomized Controlled Trials. J. Laparoendosc. Adv. Surg. Tech. 2018, 28, 248–255. [Google Scholar] [CrossRef]
- Dodds, W.J.; Groh, W.J.; Darweesh, R.M.; Lawson, T.L.; Kishk, S.M.; Kern, M.K. Sonographic measurement of gallbladder volume. Am. J. Roentgenol. 1985, 145, 1009–1011. [Google Scholar] [CrossRef]
- Stolk, M.F.; van Erpecum, K.J.; van Berge Henegouwen, G.P.; Kesselring, O.F.; Hopman, W.P. Gallbladder volume and contraction measured by sum-of-cylinders method compared with ellipsoid and area-length methods. Acta Radiol. 1990, 31, 591–596. [Google Scholar] [CrossRef]
- Shakespear, J.S.; Shaaban, A.M.; Rezvani, M. CT findings of acute cholecystitis and its complications. Am. J. Roentgenol. 2010, 194, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Stogryn, S.; Metcalfe, J.; Vergis, A.; Hardy, K. Does ultrasonography predict intraoperative findings at cholecystectomy? An institutional review. Ultrasound Q. 2016, 32, 33–39. [Google Scholar]
- Maehira, H.; Itoh, A.; Kawasaki, M.; Ogawa, M.; Imagawa, A.; Mizumura, N.; Okumura, S.; Kameyama, M. Use of dynamic CT attenuation value for diagnosis of acute gangrenous cholecystitis. Am. J. Emerg. Med. 2017, 35, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Uludağ, S.S.; Akıncı, O.; Güreş, N.; Tosun, Y.; Şanlı, A.N.; Zengin, A.K.; Özçelik, M.F. An investigation into the predictive role of serum inflammatory parameters in the diagnosis of complicated acute cholecystitis. Ulus. Travma. Acil. Cerrahi. Derg. 2022, 28, 818–823. [Google Scholar] [CrossRef]
- Karakaş, D.O.; Yeşiltaş, M. Validity of the Glasgow prognostic score and modified systemic inflamma-tion score in predicting complicated cholecystitis. Hippokratia 2020, 24, 15–20. [Google Scholar]
- Ambe, P.C.; Papadakis, M.; Zirngibl, H. A proposal for a preoperative clinical scoring system for acute cholecystitis. J. Surg. Res. 2016, 200, 473–479. [Google Scholar] [CrossRef]
- Mahmood, F.; Akingboye, A.; Malam, Y.; Thakkar, M.; Jambulingam, P. Complicated Acute Cholecystitis: The Role of C-Reactive Protein and Neutrophil-Lymphocyte Ratio as Predictive Markers of Severity. Cureus 2021, 13, e13592. [Google Scholar] [CrossRef]
- Bouassida, M.; Zribi, S.; Krimi, B.; Laamiri, G.; Mroua, B.; Slama, H.; Mighri, M.M.; Azzouz, M.M.; Hamzaoui, L.; Touinsi, H. C-reactive Protein Is the Best Biomarker to Predict Advanced Acute Cholecystitis and Conversion to Open Surgery. A Prospective Cohort Study of 556 Cases. J. Gastrointest Surg. 2020, 24, 2766–2772. [Google Scholar]
- Mok, K.W.; Reddy, R.; Wood, F.; Turner, P.; Ward, J.B.; Pursnani, K.G.; Date, R.S. Is C-reactive protein a useful adjunct in selecting patients for emergency cholecystectomy by predicting severe/gangrenous cholecystitis? Int. J. Surg. 2014, 12, 649–653. [Google Scholar] [CrossRef]
- Real-Noval, H.; Fernández-Fernández, J.; Soler-Dorda, G. Predicting factors for the diagnosis of gangrene acute cholecystitis. Cir. Y Cirujanos 2019, 87, 443–449. [Google Scholar]
- Lee, S.K.; Lee, S.C.; Park, J.W.; Kim, S.J. The utility of the preoperative neutrophil-to-lymphocyte ratio in predicting severe cholecystitis: A retrospective cohort study. BMC Surg. 2014, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Micić, D.; Stanković, S.; Lalić, N.; Đukić, V.; Polovina, S. Prognostic Value of Preoperative Neutrophil-to-lymphocyte Ratio for Prediction of Severe Cholecystitis. J. Med. Biochem. 2018, 37, 121–127. [Google Scholar] [PubMed]
- Sato, N.; Kinoshita, A.; Imai, N.; Akasu, T.; Yokota, T.; Iwaku, A.; Koike, K.; Saruta, M. Inflammation-based prognostic scores predict disease severity in patients with acute cholecystitis. Eur. J. Gastroenterol Hepatol. 2018, 30, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Ares, J.A.D.; Garcia, R.M.; Vidagany, N.E.; Tomas, N.P.; Roig, M.P.; Gras, M.V.; Gonzalez, T.R. Can inflammatory biomarkers help in the diagnosis and prognosis of gangrenous acute cholecystitis? A prospective study. Rev. Esp. Enferm. Dig. 2021, 113, 41–44. [Google Scholar]
- Turhan, V.B.; Gök, H.F.; Ünsal, A.; Akpınar, M.; Güler Şimşek, G.; Buluş, H. Pre-operative neutrophil/lymphocyte and platelet/lymphocyte ratios are effective in predicting complicated acute cholecystitis. Ulus. Travma. Acil. Cerrahi. Derg. 2022, 28, 471–476. [Google Scholar]
- Sakalar, S.; Ozakın, E.; Cevik, A.A.; Acar, N.; Dogan, S.; Kaya, F.B.; Kara, T. Plasma Procalcitonin Is Useful for Predicting the Severity of Acute Cholecystitis. Emerg. Med. Int. 2020, 2020, 8329310. [Google Scholar] [CrossRef]
- Yuzbasioglu, Y.; Duymaz, H.; Tanrikulu, C.S.; Halhalli, H.C.; Koc, M.O.; Tandoğan, M.; Coskun, F. Role of Procalcitonin in Evaluation of the Severity of Acute Cholecystitis. Eurasian J. Med. 2016, 48, 162–166. [Google Scholar] [CrossRef]
- Raffee, L.; Kuleib, S.; Oteir, A.; Kewan, T.; Alawneh, K.; Beovich, B.; Williams, B. Utility of leucocytes, inflammatory markers and pancreatic enzymes as indicators of gangrenous cholecystitis. Postgrad. Med. J. 2020, 96, 134–138. [Google Scholar] [CrossRef]

| Tokyo Grading | Mild | Moderate | Severe | p Value |
|---|---|---|---|---|
| Number, n (%) | 170 | 170 | 50 | |
| Age (years) | 56.07 ± 16.06 | 61.81 ± 16.92 | 72.38 ± 16.78 | <0.001 * |
| Sex | 0.026 * | |||
| Female, n (%) | 91 (53.5%) | 87 (51.2%) | 16 (32%) | |
| Male, n (%) | 79 (46.5%) | 83 (48.8%) | 34 (68%) | |
| BMI (kg/m2) | 25.2 ± 3.79 | 25.36 ± 4.47 | 24.61 ± 4.54 | 0.553 |
| Comorbidities | ||||
| Diabetes mellitus, n (%) | 27 (15.9%) | 32 (18.8%) | 22 (44%) | <0.001 * |
| Hypertension, n (%) | 54 (31.8%) | 68 (40%) | 31 (62%) | 0.001 * |
| CKD, n (%) | 1 (0.6%) | 0 (0%) | 10 (20%) | <0.001 * |
| CCI | 7.73 ± 75.91 | 2.49 ± 2.134 | 24.48 ± 140.79 | 0.161 |
| Vital signs at triage | ||||
| Temperature (°C) | 36.72 ± 0.63 | 37.05 ± 0.79 | 37.41 ± 1.08 | <0.001 * |
| Heart rate (bpm) | 79.9 ± 16.48 | 89.56 ± 18.32 | 106.5 ± 23.71 | <0.001 * |
| Respiratory rate (bpm) | 17.99 ± 7.76 | 17.46 ± 1.77 | 18.86 ± 3.05 | 0.259 |
| MAP (mmHg) | 102.60 ± 17.37 | 99.28 ± 16.66 | 97.68 ± 20.96 | 0.104 |
| GCS | 15 ± 0 | 15 ± 0 | 14.02 ± 1.97 | <0.001 * |
| O2 supply, n (%) | 6 (3.5%) | 19 (11.2%) | 18 (10.6%) | <0.001 * |
| FiO2 (%) | 21.44 ± 2.34 | 22.2 ± 4.93 | 31.57 ± 14.58 | <0.001 * |
| Inotrope use, n (%) | 0 (0%) | 0 (0%) | 12 (24%) | <0.001 * |
| Outcomes | ||||
| Length of stay (days) | 5.59 ± 2.86 | 7.02 ± 4.22 | 12.54 ± 10.16 | <0.001 * |
| ERCP, n (%) | 27 (15.9%) | 34 (20%) | 11 (22%) | 0.52 |
| PTGBD, n (%) | 18 (10.6%) | 55 (32.4%) | 28 (16.5%) | <0.001 * |
| Surgery, n (%) | 94 (55.3%) | 72 (42.4%) | 6 (12%) | <0.001 * |
| ICU admission, n (%) | 5 (2.9%) | 20 (11.8%) | 18 (36%) | <0.001 * |
| Mortality, n (%) | 0 (0%) | 0 (0%) | 3 (6%) | 0.002 * |
| Tokyo Grading | Mild (n = 170) | Moderate (n = 170) | Severe (n = 50) | p Value |
|---|---|---|---|---|
| Lab data | ||||
| WBC (per 103/μL) | 9.79 ± 3.21 | 13.10 ± 5.27 | 12.40 ± 6.00 | <0.001 * |
| Platelet (per 103/μL) | 236.49 ± 76.65 | 229.36 ± 75.56 | 186.22 ± 92.60 | <0.001 * |
| Neutrophil (%) | 71.24 ± 14.08 | 79.19 ± 10.99 | 81.25 ± 12.00 | <0.001 * |
| CRP (mg/dL) | 1.59 ± 3.82 | 8.52 ± 10.73 | 13.95 ± 13.33 | <0.001 * |
| Creatinine (mg/dL) | 0.82 ± 0.24 | 0.89 ± 0.32 | 2.7 ± 3.39 | <0.001 * |
| Bilirubin T+ (mg/dL) | 0.94 ± 1.09 | 1.53 ± 1.69 | 1.93 ± 1.30 | <0.001 * |
| Lactate (mg/dL) | 17.07 ± 10.82 | 16.81 ± 7.93 | 27.03 ± 21.46 | 0.03 * |
| Na (mEq/L) | 138.61 ± 2.47 | 136.8 ± 3.72 | 135.8 ± 3.35 | <0.001 * |
| K (mEq/L) | 3.79 ± 0.37 | 3.69 ± 0.37 | 3.9 ± 0.055 | <0.001 * |
| INR | 1.02 ± 0.10 | 1.08 ± 0.12 | 1.39 ± 0.51 | <0.001 * |
| NLR | 6.63 ± 6.94 | 12.63 ± 15.42 | 20.6 ± 22.05 | <0.001 * |
| PLR | 19.53 ± 20.91 | 32.24 ± 38.89 | 37.79 ± 35.56 | <0.001 * |
| LMR | 2.94 ± 1.58 | 1.87 ± 1.27 | 1.94 ± 2.71 | <0.001 * |
| Image parameter | ||||
| GB wall thickness (mm) | 4.22 ± 2.50 | 6.74 ± 4.32 | 5.85 ± 2.92 | <0.001 * |
| GB wall HU | 60.51 ± 26.53 | 74.64 ± 26.36 | 73.5 ± 26.65 | <0.001 * |
| GB volume (mm3) | 99.72 ± 51.84 | 122.68 ± 66.04 | 123.76 ± 72.73 | <0.001 * |
| Gallstone present, n (%) | 98 (57.6%) | 97 (57.1%) | 21 (42%) | 0.124 |
| Multiple Gallstones, n (%) | 59 (34.7%) | 53 (31.2%) | 15 (30%) | 0.736 |
| Sludge present, n (%) | 18 (10.6%) | 26 (15.3%) | 7 (14%) | 0.43 |
| Gallstone over GB outlet, n (%) | 58 (34.1%) | 64 (37.6%) | 12 (24%) | 0.202 |
| Pericholecystic fluid, n (%) | 106 (62.4%) | 157 (92.4%) | 40 (80%) | <0.001 * |
| Abscess formation, n (%) | 2 (1.2%) | 12 (7.1%) | 4 (8%) | 0.007 * |
| Gangrene change, n (%) | 38 (22.4%) | 99 (58.2%) | 24 (48%) | <0.001 * |
| GB perforation, n (%) | 2 (1.18%) | 13 (7.64%) | 4 (8%) | 0.0053 |
| Characteristics | Odds Ratio (95% CI) | p Value |
|---|---|---|
| Age | 1.03 (1.02–1.04) | <0.0001 * |
| Sex | 0.76 (0.51–1.14) | 0.189 |
| Diabetes mellitus | 1.68 (1.01–2.81) | 0.048 * |
| Hypertension | 1.70 (1.12–2.58) | 0.013 * |
| CKD | 7.88 (0.99–62.15) | 0.05 |
| O2 supply | 0.185 (0.08–0.45) | <0.0001 * |
| Vital signs | ||
| Temperature (°C) | 2.24 (1.61–3.12) | <0.0001 * |
| Heart rate (bpm) | 1.04 (1.03–1.06) | <0.0001 * |
| FiO2 (%) | 1.12 (1.05–1.2) | 0.001 * |
| GCS | 0 | 0.096 |
| Lab data | ||
| WBC (per 103/μL) | 1.15 (1.1–1.21) | <0.0001 * |
| Platelet (per 103/μL) | 1.00 (0.99–1.00) | 0.002 |
| Neutrophil (%) | 0.96 (0.93–1.00) | <0.0001 * |
| CRP (mg/dL) | 1.19 (1.13–1.25) | <0.0001 * |
| Creatinine (mg/dL) | 5.4 (2.48–11.78) | <0.0001 * |
| Bilirubin T (mg/dL) | 1.56 (1.27–1.98) | <0.0001 * |
| INR | 6.85 (0.48–97.74) | <0.0001 * |
| Na (mEq/L) | 0.812 (0.75–0.88) | <0.0001 * |
| K (mEq/L) | 0.75 (0.45–1.24) | 0.262 |
| Image parameter | ||
| GB wall thickness (mm) | 9.15 (4.14–20.2) | <0.0001 * |
| GB wall HU | 1.02 (1.01–1.03) | <0.0001 * |
| GB volume (mm3) | 1.01 (0.99–1.01) | <0.0001 * |
| Pericholecystic fluid, n (%) | 5.17 (3.08–8.95) | <0.0001 * |
| Gangrene change, n (%) | 4.25 (0.72–6.25) | <0.0001 * |
| Abscess formation, n (%) | 6.45 (1.46–28.44) | 0.014 * |
| Characteristics | Original Model 1 OR (95% CI) | p Value | Original Model 2 OR (95% CI) | p Value |
|---|---|---|---|---|
| GB wall thickness (mm) | 1.90 (0.791–4.92) | 0.166 | 1.25 (0.48–3.42) | 0.649 |
| GB wall HU | 1.01 (1.00–1.02) | <0.018 * | 1.01 (1.00–1.02) | 0.028 * |
| Gangrene change, n (%) | 2.10 (1.21–3.71) | <0.01 * | 1.98 (1.08–3.69) | 0.028 * |
| GB volume (mm3) | 1.01 (1.00–1.01) | <0.01 * | 1.00 (0.99–1.01) | 0.355 |
| Pericholecystic fluid | 2.34 (1.28–4.36) | <0.01 * | 1.68 (0.892–3.20) | 0.112 |
| WBC (per 103/μL) | 1.08 (1.01–1.15) | 0.022 * | ||
| CRP (mg/dL) | 1.10 (1.06–1.17) | <0.01 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Kuo, N.; Lin, H.-A.; Chao, C.-C.; Lee, S.; Tsai, C.-H.; Lin, S.-F.; Hou, S.-K. Clinical and Imaging Characteristics to Discriminate Between Complicated and Uncomplicated Acute Cholecystitis: A Regression Model and Decision Tree Analysis. Diagnostics 2025, 15, 1777. https://doi.org/10.3390/diagnostics15141777
Chen Y, Kuo N, Lin H-A, Chao C-C, Lee S, Tsai C-H, Lin S-F, Hou S-K. Clinical and Imaging Characteristics to Discriminate Between Complicated and Uncomplicated Acute Cholecystitis: A Regression Model and Decision Tree Analysis. Diagnostics. 2025; 15(14):1777. https://doi.org/10.3390/diagnostics15141777
Chicago/Turabian StyleChen, Yu, Ning Kuo, Hui-An Lin, Chun-Chieh Chao, Suhwon Lee, Cheng-Han Tsai, Sheng-Feng Lin, and Sen-Kuang Hou. 2025. "Clinical and Imaging Characteristics to Discriminate Between Complicated and Uncomplicated Acute Cholecystitis: A Regression Model and Decision Tree Analysis" Diagnostics 15, no. 14: 1777. https://doi.org/10.3390/diagnostics15141777
APA StyleChen, Y., Kuo, N., Lin, H.-A., Chao, C.-C., Lee, S., Tsai, C.-H., Lin, S.-F., & Hou, S.-K. (2025). Clinical and Imaging Characteristics to Discriminate Between Complicated and Uncomplicated Acute Cholecystitis: A Regression Model and Decision Tree Analysis. Diagnostics, 15(14), 1777. https://doi.org/10.3390/diagnostics15141777







