Expanding Role of Contrast-Enhanced Ultrasound and Elastography in the Evaluation of Abdominal Pathologies in Children
Abstract
1. Introduction
2. Contrast-Enhanced Ultrasound (CEUS)
3. Clinical Applications of CEUS
3.1. Liver
3.2. Bowel
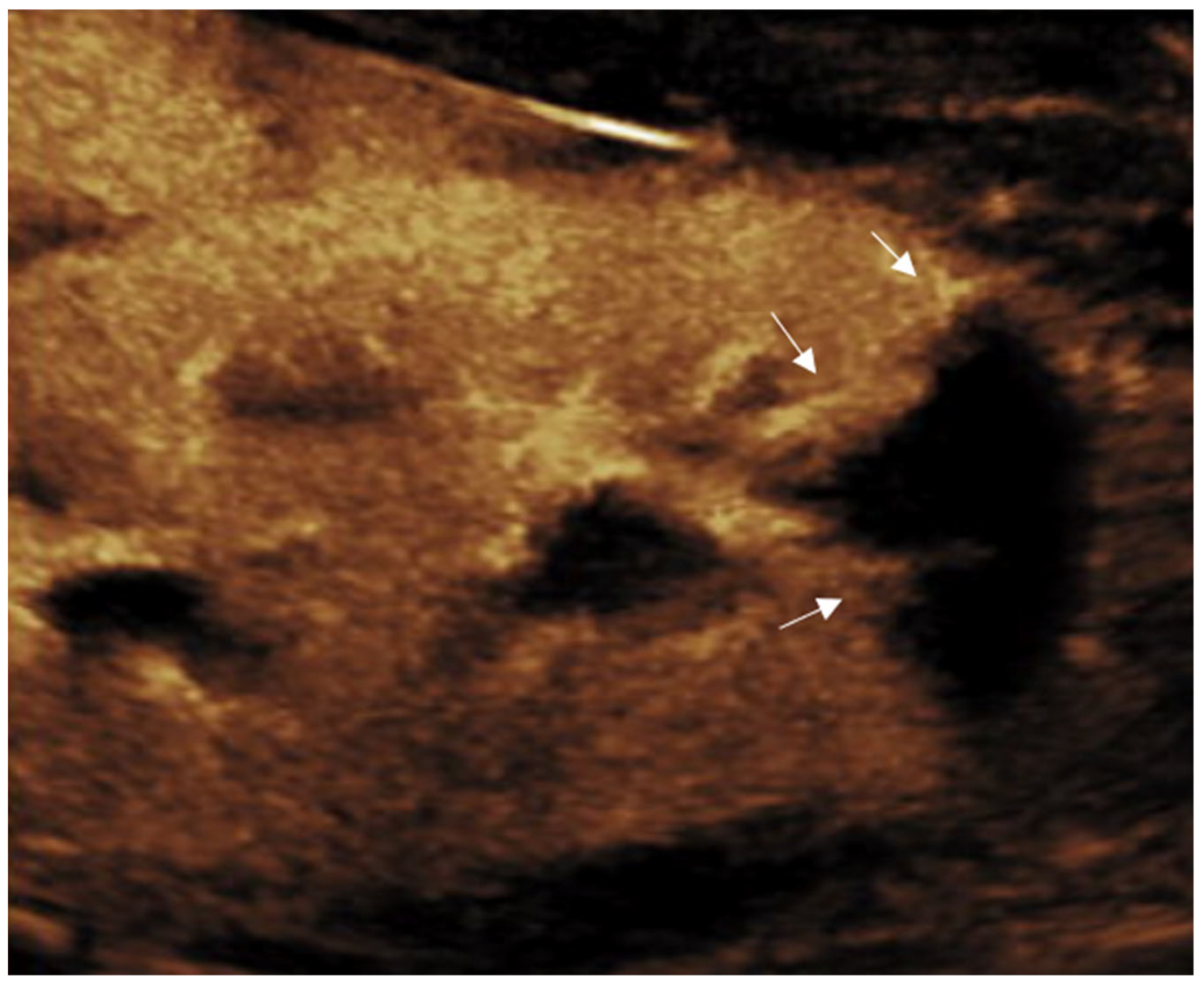
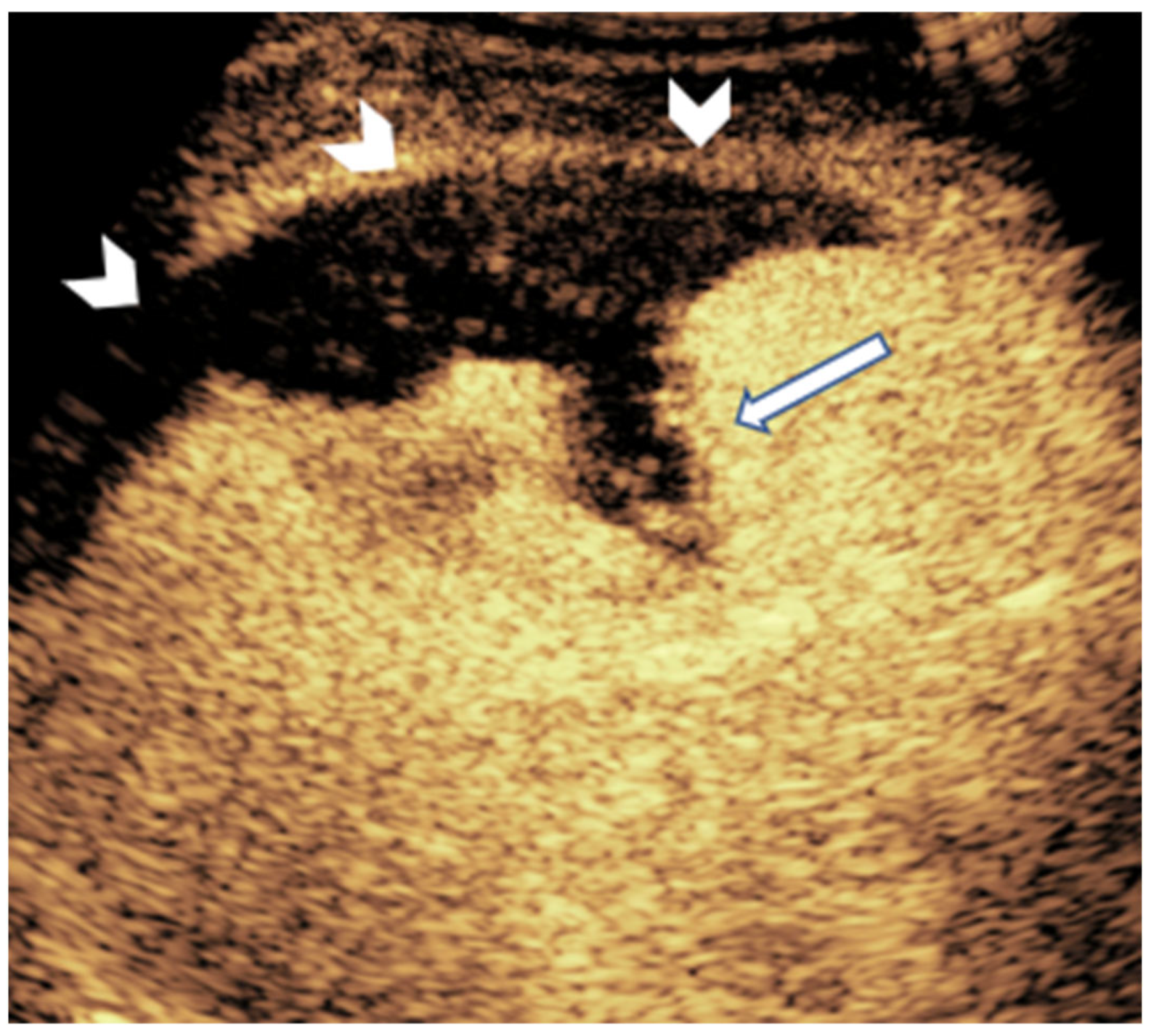
3.3. Kidney
3.4. Pancreas
3.5. Urinary Tract
3.6. Trauma
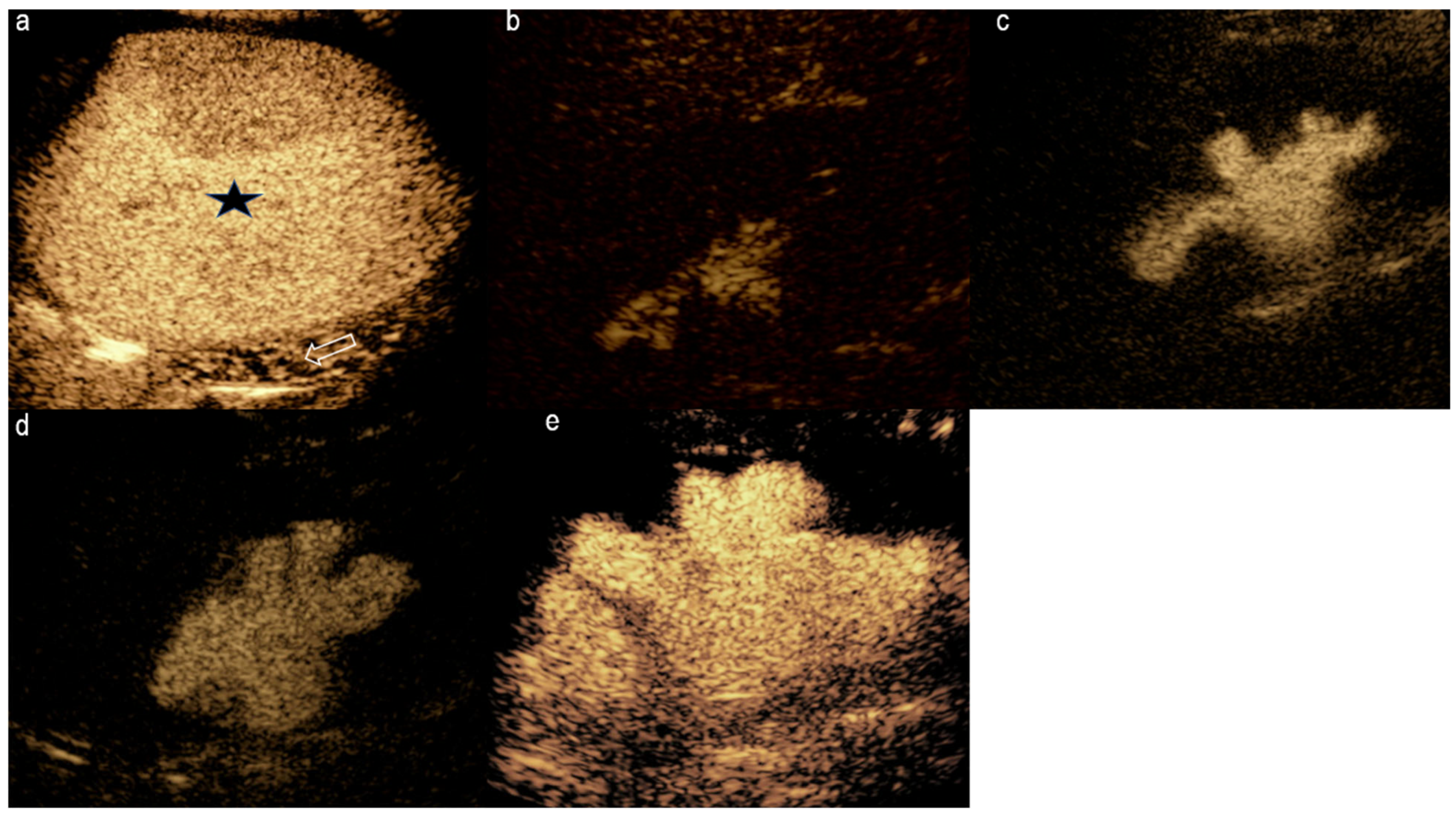
3.7. Spleen
3.8. Scrotum
4. Ultrasound Elastography (UE)
5. Clinical Applications of Elastography
5.1. Liver
5.2. Renal
5.3. Pancreas
5.4. Spleen
6. Comparative Utility and Complementary Roles
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dillman, J.R.; Gee, M.S.; Ward, C.G.; Drum, E.T.; States, L.J. Imaging sedation and anesthesia practice patterns in pediatric radiology departments—A survey of the Society of Chiefs of Radiology at Children’s Hospitals (SCORCH). Pediatr. Radiol. 2021, 51, 1497–1502. [Google Scholar] [CrossRef] [PubMed]
- Ntoulia, A.; Anupindi, S.A.; Back, S.J.; Didier, R.A.; Hwang, M.; Johnson, A.M.; Sommer, F.G.; Bellah, R.D.; Biko, D.M.; Darge, K.; et al. Contrast-enhanced ultrasound: A comprehensive review of safety in children. Pediatr. Radiol. 2021, 51, 2161–2180. [Google Scholar] [CrossRef]
- Ajmal, S. Contrast-Enhanced Ultrasonography: Review and Applications. Cureus 2021, 13, e18243. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.S.; Yamanari, M.G.I.; Suzuki, L.; Pedrosa, É.F.N.C.; Lopes, R.I.; Chammas, M.C. Use of contrast-enhanced ultrasound in pediatrics. Radiol. Bras. 2021, 54, 321–328. [Google Scholar] [CrossRef]
- Squires, J.H.; McCarville, M.B. Contrast-Enhanced Ultrasound in Children: Implementation and Key Diagnostic Applications. AJR Am. J. Roentgenol. 2021, 217, 1217–1231. [Google Scholar] [CrossRef]
- Gumus, M.; Oommen, K.C.; Squires, J.H. Contrast-enhanced ultrasound of the neonatal brain. Pediatr. Radiol. 2022, 52, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Coleman, J.L.; Navid, F.; Furman, W.L.; McCarville, M.B. Safety of ultrasound contrast agents in the pediatric oncologic population: A single-institution experience. AJR Am. J. Roentgenol. 2014, 202, 966–970. [Google Scholar] [CrossRef]
- Mao, M.; Xia, B.; Chen, W.; Gao, X.; Yang, J.; Li, S.; Zhang, Y.; Liu, H.; Zhao, T.; Wang, L.; et al. The safety and effectiveness of intravenous contrast-enhanced sonography in Chinese children—A single center and prospective study in China. Front. Pharmacol. 2019, 10, 1447. [Google Scholar] [CrossRef]
- Piskunowicz, M.; Kosiak, W.; Batko, T.; Piankowski, A.; Połczyńska, K.; Adamkiewicz-Drożyńska, E. Safety of intravenous application of second-generation ultrasound contrast agent in children: Prospective analysis. Ultrasound Med. Biol. 2015, 41, 1095–1099. [Google Scholar] [CrossRef]
- Riccabona, M. Application of a second-generation US contrast agent in infants and children—A European questionnaire-based survey. Pediatr. Radiol. 2012, 42, 1471–1480. [Google Scholar] [CrossRef]
- U.S Food and Drug Administration. LUMASON (Sulfur Hexafluoride Lipid-Type Amicrospheres) for Injectable Suspension, for Intravenous Use or Intravesical Use. 2021. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/203684s009lbl.pdf (accessed on 17 March 2018).
- Ntoulia, A.; Aguirre Pascual, E.; Back, S.J.; Bellah, R.D.; Beltrán Salazar, V.P.; Chan, P.K.J.; Damasio, M.B.; Darge, K.; Duran, C.; Fanti, S.; et al. Contrast-enhanced voiding urosonography, part 1: Vesicoureteral reflux evaluation. Pediatr. Radiol. 2021, 51, 2351–2367. [Google Scholar] [CrossRef] [PubMed]
- Anupindi, S.A.; Biko, D.M.; Ntoulia, A.; Poznick, L.; Morgan, T.A.; Darge, K.; Back, S.J.; Johnson, A.M.; Bellah, R.D.; Sommer, F.G.; et al. Contrast-enhanced US assessment of focal liver lesions in children. Radiographics 2017, 37, 1632–1647. [Google Scholar] [CrossRef]
- Claudon, M.; Dietrich, C.F.; Choi, B.I.; Cosgrove, D.O.; Kudo, M.; Nolsøe, C.P.; Piscaglia, F.; Wilson, S.R.; Barr, R.G.; Chammas, M.C.; et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver—Update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. Eur. J. Ultrasound 2013, 34, 11–29. [Google Scholar]
- Schooler, G.R.; Squires, J.H.; Alazraki, A.; Chavhan, G.B.; Chernyak, V.; Davis, J.T.; Darge, K.; Hoffer, F.A.; Hwang, M.; Kandel, J.J.; et al. Pediatric hepatoblastoma, hepatocellular carcinoma, and other hepatic neoplasms: Consensus imaging recommendations from American College of Radiology Pediatric Liver Reporting and Data System (LI-RADS) Working Group. Radiology 2020, 296, 493–497. [Google Scholar] [CrossRef]
- Fang, C.; Anupindi, S.A.; Back, S.J.; Franke, D.; Green, T.G.; Harkanyi, Z.; Hwang, M.; Johnson, A.M.; Ntoulia, A.; Sommer, F.G.; et al. Contrast-enhanced ultrasound of benign and malignant liver lesions in children. Pediatr. Radiol. 2021, 51, 2181–2197. [Google Scholar] [CrossRef] [PubMed]
- Thimm, M.A.; Rhee, D.; Takemoto, C.M.; Karnsakul, W.; Cuffari, C.; Guerrerio, A.L.; Arasu, V.A.; Majd, M.; Restrepo, R.; Bhargava, R.; et al. Diagnosis of congenital and acquired focal lesions in the neck, abdomen, and pelvis with contrast-enhanced ultrasound: A pictorial essay. Eur. J. Pediatr. 2018, 177, 1459–1470. [Google Scholar] [CrossRef] [PubMed]
- Moga, T.V.; Lupusoru, R.; Danila, M.; Ghiuchici, A.M.; Popescu, A.; Miutescu, B.; Iacob, R.; Niculescu, D.A.; Enache, L.S.; Comanescu, A.; et al. Challenges in diagnosing focal liver lesions using contrast-enhanced ultrasound. Diagnostics 2024, 15, 46. [Google Scholar] [CrossRef]
- Ro, E.; Schooler, G.R.; Morin, C.E.; Khanna, G.; Towbin, A.J. Update on the imaging evaluation of pediatric liver tumors from the ACR Pediatric LI-RADS Working Group. Abdom. Radiol. 2024, 50, 1171–1179. [Google Scholar] [CrossRef]
- Chen, M.; Qiu, M.; Liu, Y.; Zhou, W.; Xie, X.; Zhou, L. Utility of the pediatric liver contrast-enhanced ultrasound criteria in differentiating malignant and benign multifocal lesions. Pediatr. Radiol. 2023, 53, 2004–2012. [Google Scholar] [CrossRef]
- van Wassenaer, E.A.; Benninga, M.A.; van Limbergen, J.L.; D’Haens, G.R.; Griffiths, A.M.; Koot, B.G.P. Intestinal ultrasound in pediatric inflammatory bowel disease: Promising, but work in progress. Inflamm. Bowel Dis. 2022, 28, 783–787. [Google Scholar] [CrossRef]
- Paratore, M.; Garcovich, M.; Ainora, M.E.; Riccardi, L.; Gasbarrini, A.; Zocco, M.A. Dynamic contrast enhanced ultrasound in gastrointestinal diseases: A current trend or an indispensable tool? World J. Gastroenterol. 2023, 29, 4021–4035. [Google Scholar] [CrossRef] [PubMed]
- Gokli, A.; Dillman, J.R.; Humphries, P.D.; Ključevšek, D.; Mentzel, H.-J.; Rubesova, E.; Staboulidou, I.; Ntoulia, A.; Anupindi, S.A.; Back, S.J.; et al. Contrast-enhanced ultrasound of the pediatric bowel. Pediatr. Radiol. 2021, 51, 2214–2228. [Google Scholar] [CrossRef]
- Gokli, A.; Acord, M.R.; Hwang, M.; Medellin-Kowalewski, A.; Rubesova, E.; Anupindi, S.A. Contrast-enhanced US in Pediatric Patients: Overview of Bowel Applications. Radiographics 2020, 40, 1743–1762. [Google Scholar] [CrossRef]
- Benjamin, J.L.; Dennis, R.; White, S.; Munson, D.; Anupindi, S.A.; Piskunowicz, M.; Ntoulia, A.; Back, S.J.; Darge, K.; Rubesova, E.; et al. Improved diagnostic sensitivity of bowel disease of prematurity on contrast-enhanced ultrasound. J. Ultrasound Med. 2020, 39, 1031–1036. [Google Scholar] [CrossRef]
- Hwang, M.; Tierradentro-García, L.O.; Dennis, R.A.; Anupindi, S.A. The role of ultrasound in necrotizing enterocolitis. Pediatr. Radiol. 2022, 52, 702–715. [Google Scholar] [CrossRef] [PubMed]
- Benchimol, E.I.; Fortinsky, K.J.; Gozdyra, P.; Van den Heuvel, M.; Van Limbergen, J.; Griffiths, A.M. Epidemiology of pediatric inflammatory bowel disease: A systematic review of international trends. Inflamm. Bowel Dis. 2011, 17, 423–439. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.; Malter, L.; Hudesman, D. Disease monitoring in inflammatory bowel disease. World J. Gastroenterol. 2015, 21, 11246–11259. [Google Scholar] [CrossRef] [PubMed]
- Kucharzik, T.; Kannengiesser, K.; Petersen, F. The use of ultrasound in inflammatory bowel disease. Ann. Gastroenterol. 2017, 30, 135–144. [Google Scholar] [CrossRef]
- Medellin–Kowalewski, A.; Wilkens, R.; Wilson, A.; Ruan, J.; Wilson, S.R. Quantitative Contrast–Enhanced Ultrasound Parameters in Crohn Disease: Their Role in Disease Activity Determination With Ultrasound. AJR Am. J. Roentgenol. 2016, 206, 64–73. [Google Scholar] [CrossRef]
- Tracy, S.A.; Lazow, S.P.; Castro-Aragon, I.M.; Fujii, A.M.; Estroff, J.A.; Parad, R.B.; Feldman, H.A.; Lee, T.C.; Ngo, P.D.; Weldon, C.B.; et al. Is abdominal sonography a useful adjunct to abdominal radiography in evaluating neonates with suspected necrotizing enterocolitis? J. Am. Coll. Surg. 2020, 230, 903–911.e2. [Google Scholar] [CrossRef]
- Chan, B.; Gordon, S.; Yang, M.; Weekes, J.; Dance, L. Abdominal ultrasound assists the diagnosis and management of necrotizing enterocolitis. Adv. Neonatal Care 2021, 21, 365–370. [Google Scholar] [CrossRef]
- Esposito, F.; Mamone, R.; Di Serafino, M.; Mercogliano, C.; Vitale, V.; Vallone, G.; Sangiovanni, A.; Muto, M.; Russo, A.; Grassi, R.; et al. Diagnostic imaging features of necrotizing enterocolitis: A narrative review. Quant. Imaging Med. Surg. 2017, 7, 336–344. [Google Scholar] [CrossRef]
- Cuna, A.C.; Reddy, N.; Robinson, A.L.; Chan, S.S. Bowel ultrasound for predicting surgical management of necrotizing enterocolitis: A systematic review and meta-analysis. Pediatr. Radiol. 2018, 48, 658–666. [Google Scholar] [CrossRef]
- D’Angelo, G.; Impellizzeri, P.; Marseglia, L.; Montalto, A.S.; Russo, T.; Salamone, I.; Romeo, C.; Centorrino, A.; Cannavò, L.; Gitto, E.; et al. Current status of laboratory and imaging diagnosis of neonatal necrotizing enterocolitis. Ital. J. Pediatr. 2018, 44, 84. [Google Scholar] [CrossRef] [PubMed]
- Mishra, V.; Cuna, A.; Singh, R.; Schwartz, D.M.; Chan, S.; Maheshwari, A. Imaging for diagnosis and assessment of necrotizing enterocolitis. Newborn 2022, 1, 182–189. [Google Scholar]
- Rafailidis, V.; Phillips, C.; Yusuf, G.; Sidhu, P. A case of adult intussusception with greyscale, contrast-enhanced ultrasound and computerised tomography correlation. Ultrasound 2017, 25, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Yi, H.; Cai, B.; He, Y.; Huang, S.; Zhang, Y. Feasibility of contrast-enhanced ultrasonography (CEUS) in evaluating renal microvascular perfusion in pediatric patients. BMC Med. Imaging 2022, 22, 194. [Google Scholar] [CrossRef] [PubMed]
- Damasio, M.B.; Ording Müller, L.-S.; Augdal, T.A.; Avni, F.E.; Basso, L.; Bruno, C.; Darge, K.; Ključevšek, D.; Ntoulia, A.; Riccabona, M.; et al. European Society of Paediatric Radiology abdominal imaging task force: Recommendations for contrast-enhanced ultrasound and diffusion-weighted imaging in focal renal lesions in children. Pediatr. Radiol. 2020, 50, 297–304. [Google Scholar] [CrossRef]
- Riccabona, M.; Avni, F.E.; Damasio, M.B.; Ording-Müller, L.-S.; Blickman, J.G.; Darge, K.; Fotter, R.; Lee, E.Y.; Ključevšek, D.; Mentzel, H.-J.; et al. ESPR Uroradiology Task Force and ESUR Paediatric Working Group—Imaging recommendations in paediatric uroradiology, part V: Childhood cystic kidney disease, childhood renal transplantation and contrast-enhanced ultrasonography in children. Pediatr. Radiol. 2012, 42, 1275–1283. [Google Scholar] [CrossRef]
- Ran, X.; Lin, L.; Yang, M.; Niu, G.; Chen, L.; Shao, Y.; Zou, Y.; Wang, B. Contrast-Enhanced Ultrasound Evaluation of Renal Blood Perfusion Changes After Percutaneous Transluminal Renal Angioplasty and Stenting for Severe Atherosclerotic Renal Artery Stenosis. Ultrasound Med. Biol. 2020, 46, 1872–1879. [Google Scholar] [CrossRef]
- Franke, D.; Daugherty, R.J.; Ključevšek, D.; Ntoulia, A.; Rafailidis, V.; Takahashi, M.S.; Damasio, M.B.; Anupindi, S.A.; Back, S.J.; Darge, K.; et al. Contrast-enhanced ultrasound of transplant organs—Liver and kidney—In children. Pediatr. Radiol. 2021, 51, 2284–2302. [Google Scholar] [CrossRef]
- Mueller-Peltzer, K.; Negrão de Figueiredo, G.; Fischereder, M.; Habicht, A.; Rübenthaler, J.; Clevert, D.A. Vascular rejection in renal transplant: Diagnostic value of contrast-enhanced ultrasound (CEUS) compared to biopsy. Clin. Hemorheol. Microcirc. 2018, 69, 77–82. [Google Scholar] [CrossRef]
- Pan, F.-S.; Liu, M.; Luo, J.; Tian, W.-S.; Liang, J.-Y.; Xu, M.; Zhang, Y.; Wang, H.; Chen, L.; Zhao, X.; et al. Transplant renal artery stenosis: Evaluation with contrast-enhanced ultrasound. Eur. J. Radiol. 2017, 90, 42–49. [Google Scholar] [CrossRef]
- Tufano, A.; Drudi, F.M.; Angelini, F.; Polito, E.; Martino, M.; Granata, A.; Pugliese, R.; Ricci, F.; Manenti, G.; Bonomo, L.; et al. Contrast-enhanced ultrasound (CEUS) in the evaluation of renal masses with histopathological validation—Results from a prospective single-center study. Diagnostics 2022, 12, 1209. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Li, N.; Zhao, P.; Wang, Y.; Song, Q.; Song, L.; Zhang, Y.; Liu, X.; Chen, H.; Wang, J.; et al. Contrast-enhanced ultrasound (CEUS) of benign and malignant renal tumors: Distinguishing CEUS features differ with tumor size. Cancer Med. 2023, 12, 2551–2559. [Google Scholar] [CrossRef]
- Sun, D.; Wei, C.; Li, Y.; Lu, Q.; Zhang, W.; Hu, B. Contrast-Enhanced Ultrasonography with Quantitative Analysis allows Differentiation of Renal Tumor Histotypes. Sci. Rep. 2016, 6, 35081. [Google Scholar] [CrossRef]
- Li, J.; Huang, X.; Wang, L.; Wang, X.; Li, Y.; Liu, X.; Zhang, H.; Chen, Y.; Zhou, Q.; Xu, T.; et al. Role of contrast-enhanced ultrasound with the enhancement pattern and qualitative analysis for differentiating hypovascular solid renal lesions. Ultrasound Med. Biol. 2024, 50, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Marschner, C.A.; Rübenthaler, J.; Froelich, M.F.; Schwarze, V.; Clevert, D.-A. Benefits of contrast-enhanced ultrasonography for interventional procedures. Ultrasonography 2021, 40, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Pšeničny, E.; Glušič, M.; Pokorn, M.; Ključevšek, D. Contrast-enhanced ultrasound in detection and follow-up of focal renal infections in children. Br. J. Radiol. 2022, 95, 20220290. [Google Scholar] [CrossRef]
- Jung, H.J.; Choi, M.H.; Pai, K.S.; Kim, H.G. Diagnostic performance of contrast-enhanced ultrasound for acute pyelonephritis in children. Sci. Rep. 2020, 10, 10715. [Google Scholar] [CrossRef]
- Rinaldo, C.; Grimaldi, D.; Di Serafino, M.; Iacobellis, F.; Verde, F.; Caruso, M.; Capasso, R.; Esposito, M.; Romeo, V.; Imbriaco, M.; et al. An update on pyelonephritis: Role of contrast-enhanced ultrasound (CEUS). J. Ultrasound 2023, 26, 333–342. [Google Scholar] [CrossRef]
- Kim, B.; Lim, H.K.; Choi, M.H.; Woo, J.Y.; Ryu, J.; Kim, S.; Park, C.M.; Lee, W.J.; Han, M.C.; Song, I.C.; et al. Detection of parenchymal abnormalities in acute pyelonephritis by pulse inversion harmonic imaging with or without microbubble ultrasonographic contrast agent: Correlation with computed tomography. J. Ultrasound Med. 2001, 20, 5–14. [Google Scholar] [CrossRef]
- Boccatonda, A.; Stupia, R.; Serra, C. Ultrasound, contrast-enhanced ultrasound and pyelonephritis: A narrative review. World J. Nephrol. 2024, 13, 98300. [Google Scholar] [CrossRef] [PubMed]
- Basiratnia, M.; Noohi, A.H.; Lotfi, M.; Alavi, M.S. Power Doppler sonographic evaluation of acute childhood pyelonephritis. Pediatr. Nephrol. 2006, 21, 1854–1857. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Urologic Imaging; Nikolaidis, P.; Dogra, V.S.; Goldfarb, S.; Gore, J.L.; Harvin, H.J.; Heilbrun, M.E.; Kawashima, A.; Oto, A.; Remer, E.M.; et al. ACR appropriateness criteria® acute pyelonephritis. J. Am. Coll. Radiol. 2018, 15, S232–S239. [Google Scholar] [CrossRef]
- Franke, D.; Anupindi, S.A.; Barnewolt, C.E.; Green, T.G.; Greer, M.-L.C.; Harkanyi, Z.; Johnson, A.M.; Ntoulia, A.; Back, S.J.; Darge, K.; et al. Contrast-enhanced ultrasound of the spleen, pancreas and gallbladder in children. Pediatr. Radiol. 2021, 51, 2229–2252. [Google Scholar] [CrossRef]
- Bartolotta, T.V.; Randazzo, A.; Bruno, E.; Alongi, P.; Taibbi, A. Focal Pancreatic Lesions: Role of Contrast-Enhanced Ultrasonography. Diagnostics 2021, 11, 957. [Google Scholar] [CrossRef] [PubMed]
- Ripollés, T.; Martínez, M.J.; López, E.; Castelló, I.; Delgado, F. Contrast-enhanced ultrasound in the staging of acute pancreatitis. Eur. Radiol. 2010, 20, 2518–2523. [Google Scholar] [CrossRef]
- Ardelean, M.; Şirli, R.; Sporea, I.; Bota, S.; Martie, A.; Popescu, A.; Dănilă, M.; Tudor, A.; Lupuşoru, R.; Lazăr, D.; et al. Contrast-enhanced ultrasound in the pathology of the pancreas—A monocentric experience. Med. Ultrason. 2014, 16, 325–331. [Google Scholar]
- Șirli, R.; Popescu, A. Contrast-enhanced ultrasound for the assessment of pancreatic lesions. In Challenges in Pancreatic Pathology; Seicean, A., Ed.; InTech: Rijeka, Croatia, 2017. [Google Scholar]
- Azemoto, N.; Kumagi, T.; Yokota, T.; Hirooka, M.; Kuroda, T.; Koizumi, M.; Hiraoka, A.; Tokumoto, Y.; Tada, F.; Abe, M.; et al. Utility of contrast-enhanced transabdominal ultrasonography to diagnose early chronic pancreatitis. Biomed. Res. Int. 2015, 2015, 393124. [Google Scholar] [CrossRef]
- Sofia, C.; Solazzo, A.; Cattafi, A.; Chimenz, R.; Cicero, G.; Marino, M.A.; Bartolotta, T.V.; Ascenti, G.; D’Angelo, P.; Blandino, A.; et al. Contrast-enhanced voiding urosonography in the assessment of vesical-ureteral reflux: The time has come. Radiol. Med. 2021, 126, 901–909. [Google Scholar] [CrossRef]
- Kim, D.; Choi, Y.H.; Choi, G.; Lee, S.; Lee, S.; Cho, Y.J.; Kim, J.H.; Park, S.H.; Jang, W.; Seo, J.K.; et al. Contrast-enhanced voiding urosonography for the diagnosis of vesicoureteral reflux and intrarenal reflux: A comparison of diagnostic performance with fluoroscopic voiding cystourethrography. Ultrasonography 2021, 40, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Explore Leading Causes of Death. WISQARS Leading Causes of Death Visualization Tool. 2021. Available online: https://wisqars.cdc.gov/lcd/?o=LCD&y1=2021&y2=2021&ct=10&cc=ALL&g=00&s=0&r=0&ry=0&e=0&ar=lcd1age&at=groups&ag=lcd1age&a1=0&a2=199 (accessed on 12 March 2024).
- Centers for Disease Control and Prevention. Underlying Cause of Death, 2018–2021, Single Race Results Form. 2021. Available online: https://wonder.cdc.gov/controller/datarequest/D158;jsessionid=302F1E538CFED249AED2C78B127B (accessed on 4 March 2024).
- Richards, J.R.; McGahan, J.P. Focused assessment with sonography in Trauma (FasT) in 2017: What Radiologist can learn. Radiology 2017, 283, 30–48. [Google Scholar] [CrossRef] [PubMed]
- Paltiel, H.J.; Barth, R.A.; Bruno, C.; Chen, A.E.; Deganello, A.; Harkanyi, Z.; Johnson, A.M.; Ntoulia, A.; Back, S.J.; Darge, K.; et al. Contrast-enhanced ultrasound of blunt abdominal trauma in children. Pediatr. Radiol. 2021, 51, 2253–2269. [Google Scholar] [CrossRef]
- Zhang, Z.; Hong, Y.; Liu, N.; Chen, Y. Diagnostic accuracy of contrast enhanced ultrasound in patients with blunt abdominal trauma presenting to the emergency department: A systematic review and meta-analysis. Sci. Rep. 2017, 7, 4446. [Google Scholar] [CrossRef] [PubMed]
- Mortelé, K.J.; Mortelé, B.; Silverman, S.G. CT features of the accessory spleen. AJR Am. J. Roentgenol. 2004, 183, 1653–1657. [Google Scholar] [CrossRef]
- Trujillo, S.G.; Saleh, S.; Burkholder, R.; Shibli, F.; Shah, B. Accessory spleen: A rare and incidental finding in the stomach wall. Cureus 2022, 14, e24977. [Google Scholar] [CrossRef]
- George, M.; Evans, T.; Lambrianides, A.L. Accessory spleen in pancreatic tail. J. Surg. Case Rep. 2012, 2012, rjs004. [Google Scholar] [CrossRef]
- Zugail, A.S.; Ahallal, Y.; Comperat, E.-M.; Guillonneau, B. Splenorenal fusion mimicking renal cancer: One case report and literature review. Urol. Ann. 2019, 11, 211–213. [Google Scholar] [CrossRef]
- Xu, S.-Y.; Sun, K.; Xie, H.-Y.; Zhou, L.; Zheng, S.-S.; Wang, W. Accessory spleen located in the right parietal peritoneum: The first case report. Medicine 2017, 96, e7957. [Google Scholar] [CrossRef]
- Wand, O.; Tayer-Shifman, O.E.; Khoury, S.; Hershko, A.Y. A practical approach to infarction of the spleen as a rare manifestation of multiple common diseases. Ann. Med. 2018, 50, 494–500. [Google Scholar] [CrossRef]
- Catalano, O.; Sandomenico, F.; Vallone, P.; D’Errico, A.G.; Siani, A. Contrast-enhanced sonography of the spleen. In Semin Ultrasound CT MR; WB Saunders: Philadelphia, PA, USA, 2006; Volume 27, pp. 426–433. [Google Scholar]
- Reichlin, M.; Bosbach, S.J.; Minotti, B. Splenic Infarction Diagnosed by Contrast-enhanced Ultrasound in Infectious Mononucleosis—An Appropriate Diagnostic Option: A Case Report with Review of the Literature. J. Med. Ultrasound. 2022, 30, 140–142. [Google Scholar] [CrossRef] [PubMed]
- Zavariz, J.D.; Konstantatou, E.; Deganello, A.; Bosanac, D.; Huang, D.Y.; Sellars, M.E.; Patel, N.; Alhasan, R.; Westwood, M.; Sidhu, P.S.; et al. Common and uncommon features of focal splenic lesions on contrast-enhanced ultrasound: A pictorial review. Radiol. Bras. 2017, 50, 395–404. [Google Scholar] [CrossRef]
- Radcliffe, C.; Tang, Z.; Gisriel, S.D.; Grant, M. Splenic abscess in the new millennium: A descriptive, retrospective case series. Open Forum. Infect Dis. 2022, 9, ofac085. [Google Scholar] [CrossRef] [PubMed]
- Roman, A.; Iancu, C.; Andreica, V.; Socaciu, M.; Anton, O.; Sechel, R.; Pop, D.; Mera, M.; Muresan, M.; Zaharie, F.; et al. Splenic cystic lymphangioma with atypical ultrasound findings. J. Med. Ultrason. 2016, 43, 99–105. [Google Scholar] [CrossRef]
- Stang, A.; Keles, H.; Hentschke, S.; von Seydewitz, C.U.; Dahlke, J.; Malzfeldt, E.; Schneider, G.; Bücker, A.; Forsting, M.; Huppertz, A.; et al. Differentiation of benign from malignant focal splenic lesions using sulfur hexafluoride-filled microbubble contrast-enhanced pulse-inversion sonography. AJR Am. J. Roentgenol. 2009, 193, 709–721. [Google Scholar] [CrossRef]
- Lei, Y.; Huang, Q.; Li, X.; Zheng, X.; Liu, M. Characteristics and survival outcomes of primary splenic cancers: A SEER population-based study. Medicine 2022, 101, e28539. [Google Scholar] [CrossRef] [PubMed]
- Ballestri, S.; Lonardo, A.; Romagnoli, D.; Losi, L.; Loria, P. Primary lymphoma of the spleen mimicking simple benign cysts: Contrast-enhanced ultrasonography and other imaging findings. J. Med. Ultrason. 2015, 42, 251–255. [Google Scholar] [CrossRef]
- Sutherland, T.; Temple, F.; Hennessy, O.; Lee, W.-K. Contrast-enhanced ultrasound features of primary splenic lymphoma. J. Clin. Ultrasound 2010, 38, 317–319. [Google Scholar] [CrossRef]
- Omar, A.; Freeman, S. Contrast-enhanced ultrasound of the spleen. Ultrasound 2016, 24, 41–49. [Google Scholar] [CrossRef]
- Cokkinos, D.D.; Partovi, S.; Rafailidis, V.; Sierrou, C.; Fragkouli, T.; Tsolaki, S.; Alzyoud, K.; Vlachou, M.; Kalogeropoulos, I.; Ntoulia, A.; et al. Role and added value of contrast-enhanced ultrasound of the painful scrotum in the emergency setting. J. Ultrasound 2023, 26, 563–575. [Google Scholar] [CrossRef] [PubMed]
- Tenuta, M.; Sesti, F.; Bonaventura, I.; Mazzotta, P.; Pofi, R.; Gianfrilli, D.; Isidori, A.M.; Minnetti, M.; Greco, E.A.; Calogero, A.E.; et al. Use of contrast-enhanced ultrasound in testicular diseases: A comprehensive review. Andrology 2021, 9, 1369–1382. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.Y.; Pesapane, F.; Rafailidis, V.; Deganello, A.; Sellars, M.E.; Sidhu, P.S. The role of multiparametric ultrasound in the diagnosis of paediatric scrotal pathology. Br. J. Radiol. 2020, 93, 20200063. [Google Scholar] [CrossRef] [PubMed]
- Kitami, M. Ultrasonography of pediatric urogenital emergencies: Review of classic and new techniques. Ultrasonography 2017, 36, 222–238. [Google Scholar] [CrossRef]
- Bertolotto, M.; Cantisani, V.; Valentino, M.; Pavlica, P.; Derchi, L.E. Pitfalls in imaging for acute scrotal pathology. Semin. Roentgenol. 2016, 51, 60–69. [Google Scholar] [CrossRef]
- Pozza, C.; Tenuta, M.; Sesti, F.; Bertolotto, M.; Huang, D.Y.; Sidhu, P.S.; Cantisani, V.; Greco, E.A.; Isidori, A.M.; Maggi, M.; et al. Multiparametric ultrasound for diagnosing testicular lesions: Everything you need to know in daily clinical practice. Cancers 2023, 15, 5332. [Google Scholar] [CrossRef]
- Mentzel, H.-J.; Glutig, K.; Gräger, S.; Krüger, P.-C.; Waginger, M. Ultrasound elastography in children—Nice to have for scientific studies or arrived in clinical routine? Mol. Cell Pediatr. 2022, 9, 11. [Google Scholar] [CrossRef]
- Yusuf, G.; Konstantatou, E.; Sellars, M.E.; Huang, D.Y.; Sidhu, P.S. Multiparametric Sonography of Testicular Hematomas: Features on Grayscale, Color Doppler, and Contrast-Enhanced Sonography and Strain Elastography. J. Ultrasound Med. 2015, 34, 1319–1328. [Google Scholar] [CrossRef]
- Valentino, M.; Bertolotto, M.; Derchi, L.; Bertaccini, A.; Pavlica, P.; Martorana, G.; Serio, G.; Barozzi, L.; Belgrano, E.; Cova, M.A.; et al. Role of contrast-enhanced ultrasound in acute scrotal diseases. Eur. Radiol. 2011, 21, 1831–1840. [Google Scholar] [CrossRef]
- Stenzel, M.; Mentzel, H.-J. Ultrasound elastography and contrast-enhanced ultrasound in infants, children and adolescents. Eur. J. Radiol. 2014, 83, 1560–1569. [Google Scholar] [CrossRef]
- Dietrich, C.F.; Ferraioli, G.; Sirli, R.; Popescu, A.; Sporea, I.; Pienar, C.; Saftoiu, A.; Dong, Y.; Friedrich-Rust, M.; Cui, X.W.; et al. General advice in ultrasound-based elastography of pediatric patients. Med. Ultrason. 2019, 21, 315–326. [Google Scholar] [CrossRef] [PubMed]
- Habibi, H.A.; Cicek, R.Y.; Kandemirli, S.G.; Ure, E.; Ucar, A.K.; Aslan, M.; Kizilkaya, M.; Aydin, S.; Tutar, O.; Demir, M.K.; et al. Acoustic radiation force impulse (ARFI) elastography in the evaluation of renal parenchymal stiffness in patients with ureteropelvic junction obstruction. J. Med. Ultrason. 2017, 44, 167–172. [Google Scholar] [CrossRef]
- Močnik, M.; Marčun Varda, N. Ultrasound elastography in children. Children 2023, 10, 1296. [Google Scholar] [CrossRef] [PubMed]
- Forna, L.; Bozomitu, L.; Lupu, V.V.; Lupu, A.; Trandafir, L.M.; Adam Raileanu, A.; Ciobotaru-Orășanu, C.; Tănase, A.; Brănișteanu, D.; Pricop, M.; et al. Pediatric perspectives on liver cirrhosis: Unravelling clinical patterns and therapeutic challenges. J. Clin. Med. 2024, 13, 4275. [Google Scholar] [CrossRef] [PubMed]
- Sönmez, S.; Boşat, M.; Yurtseven, N.; Yurtseven, E. The role of elastography in the assessment of chronic liver disease in children. Afr. Health Sci. 2019, 19, 2806–2811. [Google Scholar] [CrossRef]
- Andersen, S.B.; Ewertsen, C.; Carlsen, J.F.; Henriksen, B.M.; Nielsen, M.B. Ultrasound Elastography Is Useful for Evaluation of Liver Fibrosis in Children-A Systematic Review. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 389–399. [Google Scholar] [CrossRef]
- Teufel-Schäfer, U.; Flechtenmacher, C.; Fichtner, A.; Hoffmann, G.F.; Schenk, J.P.; Engelmann, G. Transient elastography correlated to four different histological fibrosis scores in children with liver disease. Eur. J. Pediatr. 2021, 180, 2237–2244. [Google Scholar] [CrossRef]
- Dardanelli, E.P.; Orozco, M.E.; Lostra, J.; Laprida, C.; Lulkin, S.; Bosaleh, A.P.; Russo, R.; Marcolongo, M.; Gismondi, M.I.; Fassio, E.; et al. Bidimensional shear-wave elastography for assessing liver fibrosis in children: A proposal of reference values that correlate with the histopathological Knodell–Ishak score. Pediatr. Radiol. 2020, 50, 817–826. [Google Scholar] [CrossRef]
- Lee, S.; Choi, Y.H.; Cho, Y.J.; Lee, S.B.; Cheon, J.-E.; Kim, W.S.; Kim, I.O.; Yoo, S.Y.; Kim, M.J.; Lee, M.J.; et al. The usefulness of noninvasive liver stiffness assessment using shear-wave elastography for predicting liver fibrosis in children. BMC Med. Imaging 2021, 21, 68. [Google Scholar] [CrossRef]
- Raizner, A.; Shillingford, N.; Mitchell, P.D.; Harney, S.; Raza, R.; Serino, J.; Lau, E.; Atkinson, E.; Fishman, D.S.; Jonas, M.M.; et al. Hepatic inflammation may influence liver stiffness measurements by transient elastography in children and young adults. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 512–517. [Google Scholar] [CrossRef]
- Xu, Z.; Zhao, J.; Liu, J.; Dong, Y.; Wang, F.; Yan, J.; Li, J.; Wu, Z.; Zhang, Y.; Chen, C.; et al. Assessment of liver fibrosis by transient elastography in young children with chronic hepatitis B virus infection. Hepatol. Int. 2021, 15, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Peng, S.; Ouyang, W.; Tan, Y.; Jiang, T.; Tang, L.; Li, X.; Zhang, H.; Huang, Y.; Wang, Y.; et al. Assessment of liver fibrosis by transient elastography and multi-parameters model in young children with chronic hepatitis B virus infection. BMC Infect. Dis. 2022, 22, 160. [Google Scholar] [CrossRef]
- Galal, S.M.; Soror, S.M.; Hussien, O.; Moustafa, E.F.; Hassany, S.M. Noninvasive assessment of liver fibrosis in children with chronic hepatitis C: Shear wave elastography and APRI versus liver biopsy. Arab. J. Gastroenterol. 2020, 21, 253–259. [Google Scholar] [CrossRef]
- Enaud, R.; Frison, E.; Missonnier, S.; Fischer, A.; de Ledinghen, V.; Perez, P.; Reix, P.; Desmazes-Dufeu, N.; Dubus, J.C.; Bui, S.; et al. Cystic fibrosis and noninvasive liver fibrosis assessment methods in children. Pediatr. Res. 2022, 91, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Yoon, H.M.; Kim, K.M.; Oh, S.H.; Namgoong, J.-M.; Kim, D.Y.; Kim, W.S.; Cheon, J.E.; Kim, I.O.; Kim, J.H.; et al. Assessment of native liver fibrosis using ultrasound elastography and serological fibrosis indices in children with biliary atresia after the Kasai procedure. Acta Radiol. 2021, 62, 1088–1096. [Google Scholar] [CrossRef]
- Caruso, M.; Cuocolo, R.; Di Dato, F.; Mollica, C.; Vallone, G.; Romeo, V.; Imbriaco, M.; Salvatore, M.; Di Paolo, M.; Giugliano, A.; et al. Ultrasound, shear-wave elastography, and magnetic resonance imaging in native liver survivor patients with biliary atresia after Kasai portoenterostomy: Correlation with medical outcome after treatment. Acta Radiol. 2020, 61, 1300–1308. [Google Scholar] [CrossRef]
- Zhou, W.; Li, X.; Zhang, N.; Liao, B.; Xie, X.; Zhang, X.; Chen, S.; Tang, Y.; Zhang, Y.; Wang, W.; et al. The combination of conventional ultrasound and shear-wave elastography in evaluating the segmental heterogeneity of liver fibrosis in biliary atresia patients after Kasai portoenterostomy. Pediatr. Surg. Int. 2021, 37, 1099–1108. [Google Scholar] [CrossRef] [PubMed]
- Sağlam, N.Ö.; Aksoy, S.; Kazancı, S.Y.; Palabıyık, F.; Hatipoğlu, S.S.; İnci, E. The performance of shear wave elastography on evaluating liver changes in obese and overweight children. Turk. J. Pediatr. 2021, 63, 575–583. [Google Scholar] [CrossRef]
- Lawrence, A.E.; Dienhart, M.; Cooper, J.N.; Lodwick, D.; Lopez, J.J.; Fung, B.; Danziger-Isakov, L.; Nadler, E.P.; Besner, G.E.; Gittes, G.K.; et al. Ultrasound elastography as a non-invasive method to monitor liver disease in children with short bowel syndrome: Updated results. J. Pediatr. Surg. 2019, 54, 1179–1183. [Google Scholar] [CrossRef]
- Kim, D.W.; Yoon, H.M.; Jung, A.Y.; Lee, J.S.; Oh, S.H.; Kim, K.M.; Kim, W.S.; Cheon, J.E.; Kim, I.O.; Kim, J.H.; et al. Diagnostic performance of ultrasound elastography for evaluating portal hypertension in children: A systematic review and meta-analysis. J. Ultrasound Med. 2019, 38, 747–759. [Google Scholar] [CrossRef]
- Vinciguerra, T.; Brunati, A.; David, E.; Longo, F.; Pinon, M.; Ricceri, F.; Smilari, P.; Bognanno, G.; Farinella, E.; Dalla Pozza, L.; et al. Transient elastography for non-invasive evaluation of post-transplant liver graft fibrosis in children. Pediatr. Transplant. 2018, 22, e13125. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.; Nastasio, S.; Mitchell, P.D.; Fawaz, R.; Elisofon, S.A.; Vakili, K.; Mazariegos, G.V.; Jonas, M.M.; Soriano, H.E.; Lerret, S.M.; et al. Transient elastography assessment of liver allograft fibrosis in pediatric transplant recipients. Pediatr. Transplant. 2020, 24, e13736. [Google Scholar] [CrossRef]
- Hartung, E.A.; Wen, J.; Poznick, L.; Furth, S.L.; Darge, K. Ultrasound elastography to quantify liver disease severity in autosomal recessive polycystic kidney disease. J. Pediatr. 2019, 209, 107–115.e5. [Google Scholar] [CrossRef]
- Hwang, J.; Yoon, H.M.; Jung, A.Y.; Lee, J.S.; Kim, K.M.; Oh, S.H.; Kim, D.Y.; Kim, W.S.; Cheon, J.E.; Kim, I.O.; et al. Diagnostic performance of ultrasound elastography and serologic fibrosis indices for evaluation of hepatic involvement in Wilson disease. J. Ultrasound Med. 2020, 39, 2231–2242. [Google Scholar] [CrossRef]
- Stefanescu, A.C.; Pop, T.L.; Stefanescu, H.; Miu, N. Transient elastography of the liver in children with Wilson’s disease: Preliminary results. J. Clin. Ultrasound 2016, 44, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Özdemir Çiçek, S.; Karaman, Z.F.; Şahin, N.; Paç Kısaarslan, A.; Poyrazoğlu, M.H.; Düşünsel, R. Evaluation of liver elasticity with shear-wave elastography in juvenile idiopathic arthritis patients receiving methotrexate. Pediatr. Int. 2022, 64, e15239. [Google Scholar] [CrossRef] [PubMed]
- Tran, L.C.; Ley, D.; Bourdon, G.; Coopman, S.; Lerisson, H.; Tillaux, C.; Belarbi, N.; Ducou le Pointe, H.; Giorgi, R.; Franchi-Abella, S.; et al. Noninvasive pediatric liver fibrosis measurement: Two-dimensional shear wave elastography compared with transient elastography. Front. Pediatr. 2022, 10, 849815. [Google Scholar] [CrossRef] [PubMed]
- Yoǧurtçuoǧlu, B.; Damar, Ç. Renal elastography measurements in children with acute glomerulonephritis. Ultrasonography 2021, 40, 575–583. [Google Scholar] [CrossRef]
- Correas, J.-M.; Anglicheau, D.; Joly, D.; Gennisson, J.-L.; Tanter, M.; Hélénon, O. Ultrasound-based imaging methods of the kidney-recent developments. Kidney Int. 2016, 90, 1199–1210. [Google Scholar] [CrossRef]
- Maralescu, F.-M.; Vaduva, A.; Schiller, A.; Petrica, L.; Sporea, I.; Popescu, A.; Lupu, A.; Duta, C.; Sirli, R.; Bota, S.; et al. Relationship between novel elastography techniques and renal fibrosis—Preliminary experience in patients with chronic glomerulonephritis. Biomedicines 2023, 11, 365. [Google Scholar] [CrossRef]
- Iyama, T.; Sugihara, T.; Takata, T.; Isomoto, H. Renal ultrasound elastography: A review of the previous reports on chronic kidney diseases. Appl. Sci. 2021, 11, 9677. [Google Scholar] [CrossRef]
- Bolboacă, S.D.; Elec, F.I.; Elec, A.D.; Muntean, A.M.; Socaciu, M.A.; Iacob, G.; Băcilă, C.; Tudor, A.; Mitre, A.; Şirli, R.; et al. Shear-wave elastography variability analysis and relation with kidney allograft dysfunction: A single-center study. Diagnostics 2020, 10, 41. [Google Scholar] [CrossRef] [PubMed]
- Pfahler, M.H.C.; Kratzer, W.; Leichsenring, M.; Graeter, T.; Schmidt, S.A.; Wendlik, I.; Meier, C.; Ott, M.; Mason, R.A.; Schmidberger, J.; et al. Point shear wave elastography of the pancreas in patients with cystic fibrosis: A comparison with healthy controls. Abdom. Radiol. 2018, 43, 2384–2390. [Google Scholar] [CrossRef]
- Salah, N.Y.; Madkour, S.S.; Soliman, K.S. Pancreatic shear wave elastography in children with type 1 diabetes: Relation to diabetes duration, glycemic indices, fasting C-peptide and diabetic complications. Pediatr. Radiol. 2022, 52, 2348–2358. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, I.; Brauch, C.; Poynard, T.; Baumann, U. Spleen stiffness measurement by transient elastography to diagnose portal hypertension in children. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Button, H.; Fitzpatrick, E.; Davenport, M.; Burford, C.; Alexander, E.; Dhawan, A.; Kelly, D.; McKiernan, P.; Hadzic, N.; Mirza, D.; et al. Transient elastography measurements of spleen stiffness as a predictor of clinically significant varices in children. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 446–451. [Google Scholar]
- Uchida, H.; Sakamoto, S.; Kobayashi, M.; Shigeta, T.; Matsunami, M.; Sasaki, K.; Kasahara, M.; Nakai, T.; Urushihara, N.; Kitagawa, N.; et al. The degree of spleen stiffness measured on acoustic radiation force impulse elastography predicts the severity of portal hypertension in patients with biliary atresia after portoenterostomy. J. Pediatr. Surg. 2015, 50, 559–564. [Google Scholar] [CrossRef]
- Hu, X.; Huang, X.; Hou, J.; Ding, L.; Su, C.; Meng, F. Diagnostic accuracy of spleen stiffness to evaluate portal hypertension and esophageal varices in chronic liver disease: A systematic review and meta-analysis. Eur. Radiol. 2021, 31, 2392–2404. [Google Scholar] [CrossRef]
- Sintusek, P.; Siriporn, N.; Punpanich, D.; Chongsrisawat, V.; Poovorawan, Y. Spleen and Liver Stiffness to Detect Esophageal Varices in Children with Biliary Atresia. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 411–415. [Google Scholar] [CrossRef]








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lemessa, N.F.; Sultan, L.R.; Martinez-Correa, S.; Davis, L.M.; Hwang, M. Expanding Role of Contrast-Enhanced Ultrasound and Elastography in the Evaluation of Abdominal Pathologies in Children. Diagnostics 2025, 15, 1680. https://doi.org/10.3390/diagnostics15131680
Lemessa NF, Sultan LR, Martinez-Correa S, Davis LM, Hwang M. Expanding Role of Contrast-Enhanced Ultrasound and Elastography in the Evaluation of Abdominal Pathologies in Children. Diagnostics. 2025; 15(13):1680. https://doi.org/10.3390/diagnostics15131680
Chicago/Turabian StyleLemessa, Natae Fekadu, Laith R. Sultan, Santiago Martinez-Correa, Laura May Davis, and Misun Hwang. 2025. "Expanding Role of Contrast-Enhanced Ultrasound and Elastography in the Evaluation of Abdominal Pathologies in Children" Diagnostics 15, no. 13: 1680. https://doi.org/10.3390/diagnostics15131680
APA StyleLemessa, N. F., Sultan, L. R., Martinez-Correa, S., Davis, L. M., & Hwang, M. (2025). Expanding Role of Contrast-Enhanced Ultrasound and Elastography in the Evaluation of Abdominal Pathologies in Children. Diagnostics, 15(13), 1680. https://doi.org/10.3390/diagnostics15131680






