The Clinical Significance and Potential of Complex Diagnosis for a Large Scar Area Following Myocardial Infarction
Abstract
1. Introduction
Aim
2. Materials and Methods
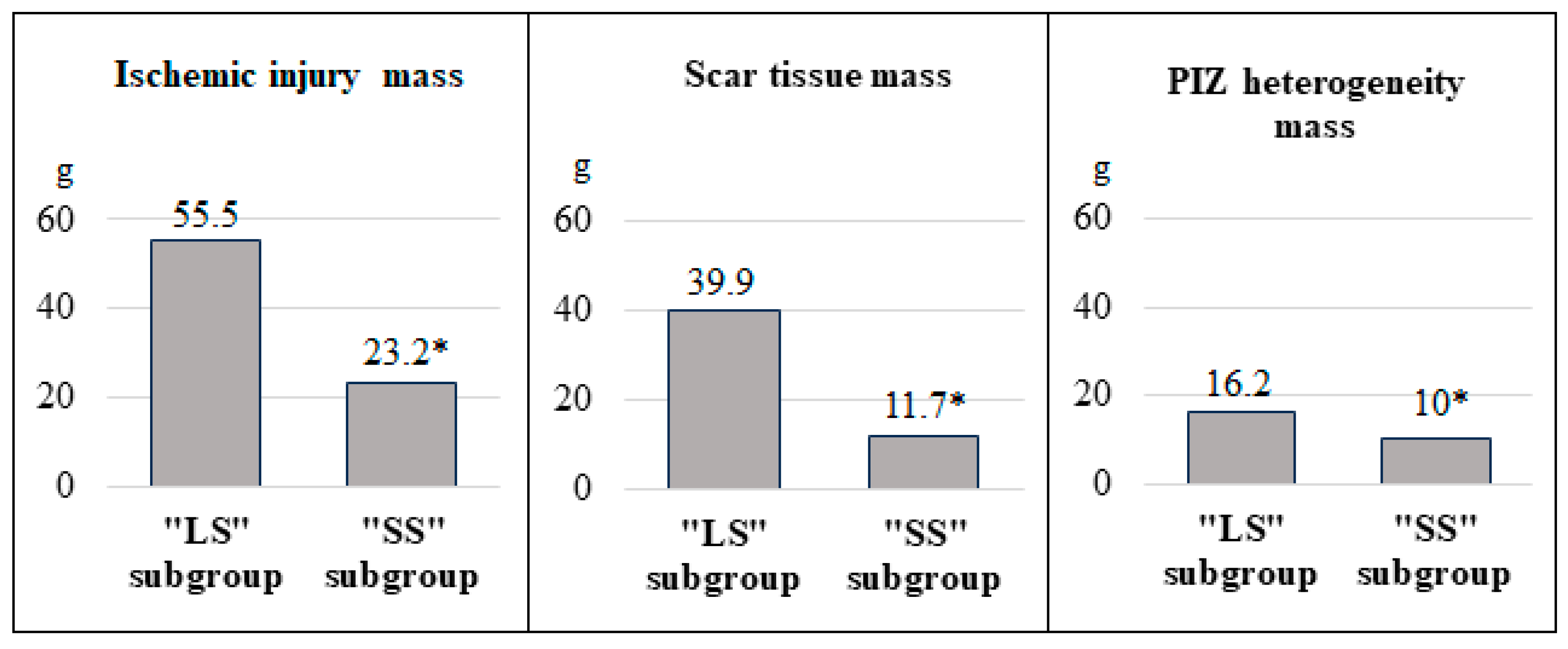
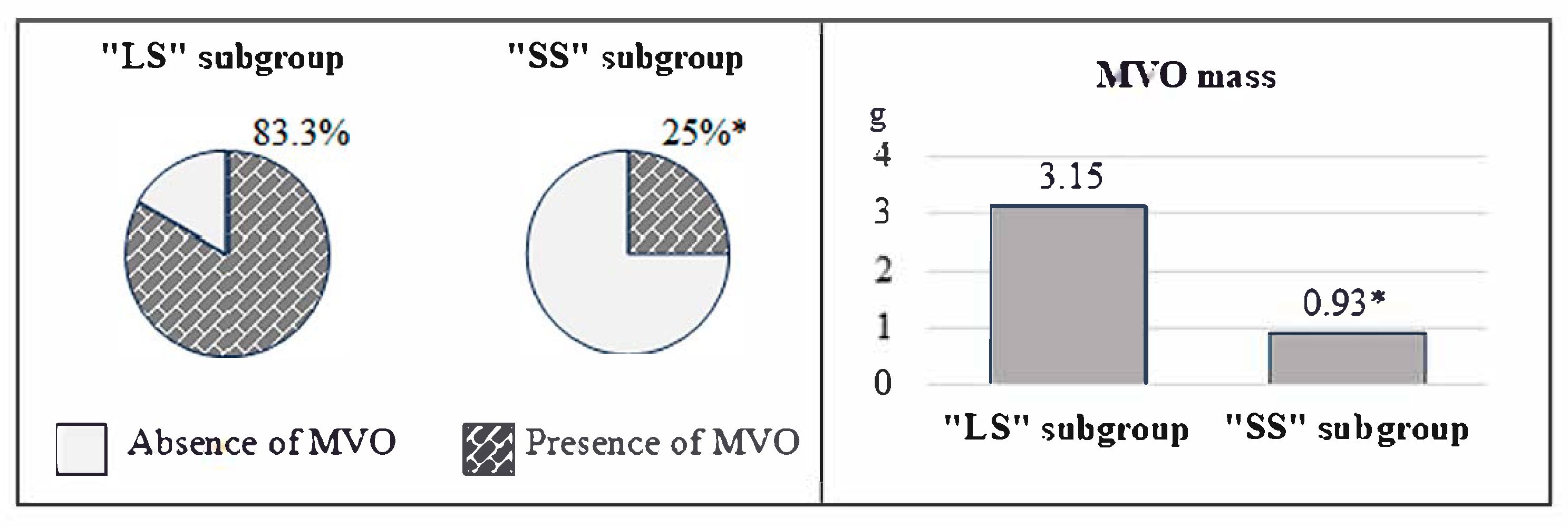
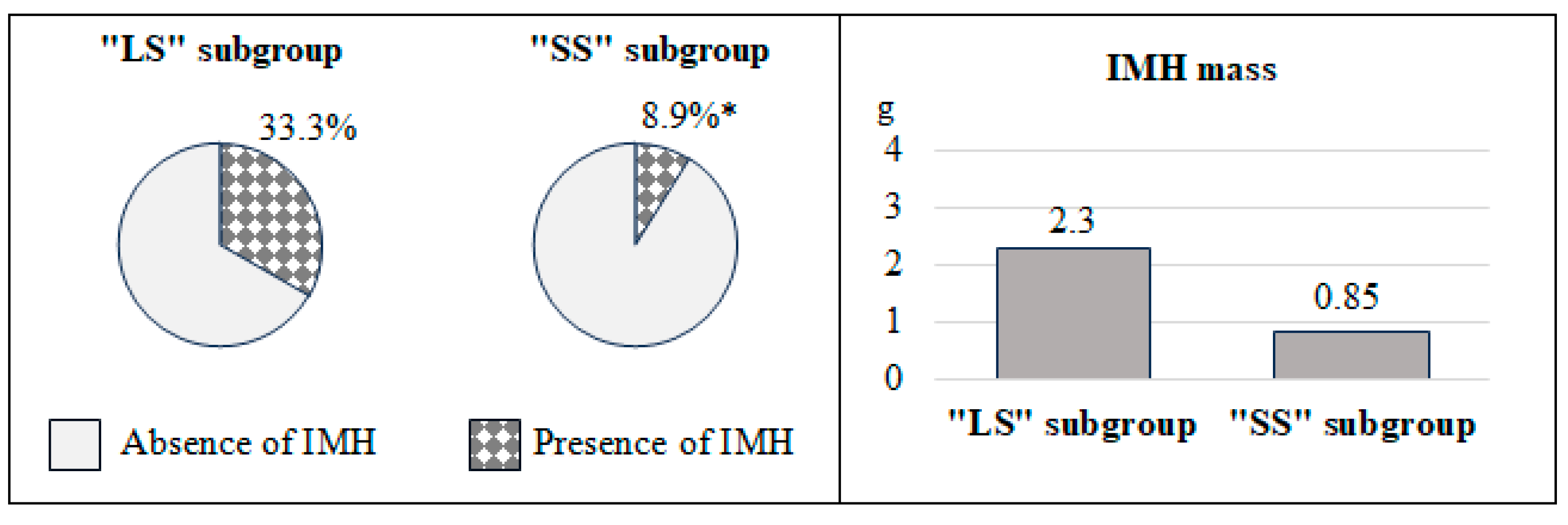
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Safiri, S.; Karamzad, N.; Singh, K.; Carson-Chahhoud, K.; Adams, C.; Nejadghaderi, S.A.; Almasi-Hashiani, A.; Sullman, M.; Mansournia, M.A.; Bragazzi, N.L.; et al. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990–2019. Eur. J. Prev. Cardiol. 2022, 29, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Morddarvanjoghi, F.; Abdolmaleki, A.; Rasoulpoor, S.; Khaleghi, A.A.; Hezarkhani, L.A.; Shohaimi, S.; Mohammadi, M. The global prevalence of myocardial infarction: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2023, 23, 206. [Google Scholar] [CrossRef] [PubMed]
- Socialstyrelsen. Statistics on Myocardial Infarctions 2022. Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2023-11-8839.pdf (accessed on 25 February 2025).
- Dani, S.S.; Lone, A.N.; Javed, Z.; Khan, M.S.; Khan, M.Z.; Kaluski, E.; Virani, S.S.; Shapiro, M.D.; Cainzos-Achirica, M.; Nasir, K.; et al. Trends in Premature Mortality from Acute Myocardial Infarction in the United States, 1999 to 2019. J. Am. Heart Assoc. 2022, 11, e021682. [Google Scholar] [CrossRef]
- Kim, M.S.; Kim, M.J.; Jeong, H.J.; Hwang, S.W.; Kim, K.B. Effect of patent complete revascularization on the akinetic myocardial segments. Interdiscip. Cardiovasc. Thorac. Surg. 2024, 39, ivae143. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. Acute Cardiovasc. Care 2024, 13, 55–161. [Google Scholar] [CrossRef]
- Beijnink, C.W.; van der Hoeven, N.W.; Konijnenberg, L.S.; Kim, R.J.; Bekkers, S.C.; Kloner, R.A.; Everaars, H.; El Messaoudi, S.; van Rossum, A.C.; van Royen, N.; et al. Cardiac MRI to Visualize Myocardial Damage after ST-Segment Elevation Myocardial Infarction: A Review of Its Histologic Validation. Radiology 2021, 301, 4–18. [Google Scholar] [CrossRef]
- Terenicheva, M.A.; Stukalova, O.V.; Shakhnovich, R.M.; Ternovoy, S.K. The role of cardiac magnetic resonance imaging in defining the prognosis of patients with acute ST-segment elevation myocardial infarction. Part 2. Assessment of the disease prognosis. Terapevticheskii Arkh. 2022, 94, 552–557. [Google Scholar] [CrossRef]
- Garcia, M.J.; Kwong, R.Y.; Scherrer-Crosbie, M.; Taub, C.C.; Blankstein, R.; Lima, J.; Bonow, R.O.; Eshtehardi, P.; Bois, J.P. American Heart Association Council on Cardiovascular Radiology and Intervention and Council on Clinical Cardiology. State of the Art: Imaging for Myocardial Viability: A Scientific Statement from the American Heart Association. Circ. Cardiovasc. Imaging 2020, 13, e000053. [Google Scholar] [CrossRef]
- Heidary, S.; Patel, H.; Chung, J.; Yokota, H.; Gupta, S.N.; Bennett, M.V.; Katikireddy, C.; Nguyen, P.; Pauly, J.M.; Terashima, M.; et al. Quantitative tissue characterization of infarct core and border zone in patients with ischemic cardiomyopathy by magnetic resonance is associated with future cardiovascular events. J. Am. Coll. Cardiol. 2010, 55, 2762–2768. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth universal definition of myocardial infarction. Circulation 2018, 138, 618–651. [Google Scholar] [CrossRef]
- Baessler, B.; Mannil, M.; Oebel, S.; Maintz, D.; Alkadhi, H.; Manka, R. Subacute and chronic left ventricular myocardial scar: Accuracy of texture analysis on nonenhanced cine MR images. Radiology 2018, 286, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Bendary, A.; Afifi, M.; Tawfik, W.; Mahros, M.; Ramzy, A.; Salem, M. The predictive value of global longitudinal strain on late infarct size in patients with anterior ST-segment elevation myocardial infarction treated with a primary percutaneous coronary intervention. Int. J. Cardiovasc. Imaging 2019, 35, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Sarkisian, L.; Saaby, L.; Poulsen, T.S.; Gerke, O.; Jangaard, N.; Hosbond, S.; Diederichsen, A.C.P.; Thygesen, K.; Mickley, H. Clinical characteristics and outcomes of patients with myocardial infarction, myocardial injury, and nonelevated troponins. Am. J. Med. 2016, 129, 446.e5–446.e21. [Google Scholar] [CrossRef]
- Hayıroğlu, M.İ.; Çınar, T.; Çinier, G.; Pay, L.; Yumurtaş, A.Ç.; Tezen, O.; Eren, S.; Kolak, Z.; Çetin, T.; Özcan, S.; et al. Comparison of mortality prediction scores in elderly patients with ICD for heart failure with reduced ejection fraction. Aging Clin. Exp. Res. 2022, 34, 653–660. [Google Scholar] [CrossRef]
- Jenča, D.; Melenovsky, V.; Stehlik, J.; Stanek, V.; Kettner, J.; Kautzner, J.; Adamkova, V.; Wohlfahrt, P. Heart failure after myocardial infarction: Incidence and predictors. ESC Heart Fail. 2021, 8, 222–237. [Google Scholar] [CrossRef]
- Han, M.M.; Zhao, W.S.; Wang, X.; He, S.; Xu, X.R.; Dang, C.J.; Zhang, J.; Liu, J.M.; Chen, M.L.; Xu, L.; et al. Echocardiographic parameters predict short-and long-term adverse cardiovascular events in patients with acute myocardial infarction. Int. J. Gen. Med. 2021, 14, 2297–2303. [Google Scholar] [CrossRef]
- Khan, J.N.; McCann, G.P. Cardiovascular magnetic resonance imaging assessment of outcomes in acute myocardial infarction. World J. Cardiol. 2017, 9, 109–133. [Google Scholar] [CrossRef]
- Peng, F.; Zheng, T.; Tang, X.; Liu, Q.; Sun, Z.; Feng, Z.; Zhao, H.; Gong, L. Magnetic resonance texture analysis in myocardial infarction. Front. Cardiovasc. Med. 2021, 8, 724271. [Google Scholar] [CrossRef]
- Stone, G.W.; Selker, H.P.; Thiele, H.; Patel, M.R.; Udelson, J.E.; Ohman, E.M.; Maehara, A.; Eitel, I.; Granger, C.B.; Jenkins, P.L.; et al. Relationship between infarct size and outcomes following primary PCI: Patient-level analysis from 10 randomized trials. J. Am. Coll. Cardiol. 2016, 67, 1674–1683. [Google Scholar] [CrossRef]
- Eitel, I.; Stiermaier, T.; Lange, T.; Rommel, K.P.; Koschalka, A.; Kowallick, J.T.; Lotz, J.; Kutty, S.; Gutberlet, M.; Hasenfub, G.; et al. Cardiac magnetic resonance myocardial feature tracking for optimized prediction of cardiovascular events following myocardial infarction. JACC Cardiovasc. Imaging 2018, 11, 1433–1444. [Google Scholar] [CrossRef]
- Redfors, B.; Mohebi, R.; Giustino, G.; Chen, S.; Selker, H.P.; Thiele, H.; Patel, M.R.; Udelson, J.E.; Ohman, E.M.; Eitel, I.; et al. Time delay, infarct size, and microvascular obstruction after primary percutaneous coronary intervention for ST-segment–elevation myocardial infarction. Circ. Cardiovasc. Interv. 2021, 14, e009879. [Google Scholar] [CrossRef] [PubMed]
- Richardson, W.J.; Clarke, S.A.; Quinn, T.A.; Holmes, J.W. Physiological implications of myocardial scar structure. Compr. Physiol. 2015, 5, 1877–1909. [Google Scholar] [CrossRef] [PubMed]
- Souto, A.L.M.; Souto, R.M.; Teixeira, I.C.R.; Nacif, M.S. Myocardial viability on cardiac magnetic resonance. Arq. Bras. Cardiol. 2017, 108, 458–469. [Google Scholar] [CrossRef] [PubMed]
- Krikunov, P.V.; Vasyuk, Y.A.; Krikunova, O.V. Predictive value of echocardiography in post myocardial infarction setting. Part 1. Russ. J. Cardiol. 2017, 12, 120–128. [Google Scholar] [CrossRef]
- Schwaiger, J.P.; Reinstadler, S.J.; Tiller, C.; Holzknecht, M.; Reindl, M.; Mayr, A.; Graziadei, I.; Müller, S.; Metzler, B.; Klug, G. Baseline LV ejection fraction by cardiac magnetic resonance and 2D echocardiography after ST-elevation myocardial infarction–influence of infarct location and prognostic impact. Eur. Radiol. 2020, 30, 663–671. [Google Scholar] [CrossRef]
- Golcuk, E.; Yalin, K.; Aksu, T.; Tiryakioglu, S.K.; Bilge, A.K.; Adalet, K. Peri-infarction zone as a risk marker for patients with postmyocardial infarction. Am. J. Med. Sci. 2016, 351, 452–458. [Google Scholar] [CrossRef]
- Wu, K.C. CMR of microvascular obstruction and hemorrhage in myocardial infarction. J. Cardiovasc. Magn. Reson. 2012, 14, 68. [Google Scholar] [CrossRef]
- Niccoli, G.; Scalone, G.; Lerman, A.; Crea, F. Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 2016, 37, 1024–1033. [Google Scholar] [CrossRef]
- Galli, M.; Niccoli, G.; De Maria, G.; Brugaletta, S.; Montone, R.A.; Vergallo, R.; Benenati, S.; Magnani, G.; D’Amario, D.; Porto, I.; et al. Coronary microvascular obstruction and dysfunction in patients with acute myocardial infarction. Nat. Rev. Cardiol. 2024, 21, 283–298. [Google Scholar] [CrossRef]
- Bonfig, N.L.; Soukup, C.R.; Shah, A.A.; Olet, S.; Davidson, S.J.; Schmidt, C.W.; Peterson, R.; Henry, T.D.; Traverse, J.H. Increasing myocardial edema is associated with greater microvascular obstruction in ST-segment elevation myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2022, 323, H818–H824. [Google Scholar] [CrossRef]
- Smulders, M.W.; Van Assche, L.M.R.; Bekkers, S.C.; Nijveldt, R.; Beijnink, C.W.; Kim, H.W.; Hayes, B.; Parker, M.A.; Kaolawanich, Y.; Judd, R.M.; et al. Epicardial surface area of infarction: A stable surrogate of microvascular obstruction in acute myocardial infarction. Circ. Cardiovasc. Imaging 2021, 14, e010918. [Google Scholar] [CrossRef] [PubMed]
- Reinstadler, S.J.; Stiermaier, T.; Reindl, M.; Feistritzer, H.J.; Fuernau, G.; Eitel, C.; Desch, S.; Klug, G.; Thiele, H.; Metzler, B.; et al. Intramyocardial haemorrhage and prognosis after ST-elevation myocardial infarction. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Xia, R.; Zhu, T.; Zhang, Y.; He, B.; Chen, Y.; Wang, L.; Zhou, Y.; Liao, J.; Zheng, J.; Li, Y.; et al. Myocardial infarction size as an independent predictor of intramyocardial haemorrhage in acute reperfused myocardial ischaemic rats. Eur. J. Med. Res. 2022, 27, 220. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.L.; Phan, J.A.; Hee, L.; Moses, D.A.; Otton, J.; Terreblanche, O.D.; Xiong, J.; Premawardhana, U.; Rajaratnam, R.; Juergens, C.P.; et al. High-sensitivity troponin T predicts infarct scar characteristics and adverse left ventricular function by cardiac magnetic resonance imaging early after reperfused acute myocardial infarction. Am. Heart J. 2015, 170, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Mathbout, M.; Asfour, A.; Leung, S.; Lolay, G.; Idris, A.; Abdel-Latif, A.; Ziada, K.M. NT-proBNP level predicts extent of myonecrosis and clinical adverse outcomes in patients with ST-elevation myocardial infarction: A pilot study. Med. Res. Arch. 2020, 8. [Google Scholar] [CrossRef][Green Version]

| Indicators | Modeling Group (n = 92) | Validation Group (n = 31) | p |
|---|---|---|---|
| Age, years | 57 (52; 61) | 58 (50; 64) | 0.392 |
| Male, n (%) | 85 (92.4) | 27 (87.1) | 0.371 |
| Female, n (%) | 7 (7.6) | 4 (12.9) | 0.371 |
| BMI, kg/m2 | 27.5 ± 3.8 | 28.1 ± 3.8 | 0.361 |
| Tobacco smoking, n (%) | 72 (78.3) | 19 (61.3) | 0.062 |
| History of CHD, n (%) | 23 (25) | 4 (12.9) | 0.159 |
| AH, n (%) | 83 (90.2) | 30 (96.8) | 0.245 |
| AH duration, years | 8 (8.7) | 4 (12.9) | 0.496 |
| Pharmacoinvasive revascularization, n (%) | 31 (33.7) | 15 (48.4) | 0.144 |
| Primary PCI, n (%) | 61 (66.3) | 16 (51.6) | 0.146 |
| “Pain-to-needle” time, min | 102.5 (53; 150) | 110 (90; 270) | 0.341 |
| “Pain-to-balloon” time, min | 287.5 (210; 460) | 275 (190; 460) | 0.422 |
| STEMI, n (%)/NSTEMI, n (%) | 86 (93.5)/6 (6.5) | 28 (90)/3 (10) | 0.560 |
| Q-MI, n (%)/notQ-MI, n (%) | 53 (57.6)/39 (42.4) | 18 (58.1)/13 (41.9) | 0.961 |
| Drug therapy | |||
| Lipid-lowering therapy, n (%) | 92 (100) | 31 (100) | 1.000 |
| Dual antiplatelet therapy, n (%) | 92 (100) | 31 (100) | 1.000 |
| RAAS inhibitors, n (%) | 88 (95.7) | 28 (90.3) | 0.261 |
| β-blockers, n (%) | 82 (89.1) | 31 (100) | 0.055 |
| Calcium channel blockers, n (%) | 13 (14.1) | 3 (9.7) | 0.529 |
| Diuretics, n (%) | 28 (30.4) | 15 (48.4) | 0.069 |
| Indicators | “LS” Subgroup (n = 36) | “SS” Subgroup (n = 56) | p |
|---|---|---|---|
| Age, years | 58 (52; 61) | 56 (52; 60) | 0.462 |
| Male, n (%) | 32 (88.9) | 3 (5.4) | 0.315 |
| Female, n (%) | 4 (11.1) | 53 (94.6) | 0.315 |
| BMI, kg/m2 | 27.6 ± 4 | 27.4 ± 3.7 | 0.792 |
| Tobacco smoking, n (%) | 25 (69.4) | 45 (80.4) | 0.227 |
| History of CHD, n (%) | 7 (19.4) | 16 (28.6) | 0.320 |
| CHD duration, years | 1.5 (0.5; 10) | 1 (1; 2.5) | 0.616 |
| AH, n (%) | 27 (75) | 48 (85.7) | 0.197 |
| AH duration, years | 5 (3; 9) | 5 (2; 9) | 0.397 |
| Diabetes mellitus, n (%) | 3 (8.3) | 1 (1.8) | 0.136 |
| Pharmacoinvasive revascularization, n (%) | 12 (33.3) | 19 (33.9) | 0.953 |
| Primary PCI, n (%) | 24 (66.7) | 37 (66.1) | 0.953 |
| “Pain-to-needle” time, min | 120 (80; 369.5) | 72.5 (44; 120) | 0.150 |
| “Pain-to-balloon” time, min | 360 (210; 625) | 242.5 (150; 380) | 0.009 |
| STEMI, n (%)/NSTEMI, n (%) | 35 (97)/1 (3) | 51 (91)/5 (9) | 0.244 |
| Q-MI, n (%)/notQ-MI, n (%) | 31 (86.1)/ 5 (13.9) | 22 (39.3)/ 34 (60.7) | <0.001 |
| SBP, mm Hg | 123 (116; 130) | 121.5 (115; 130.5) | 0.737 |
| DBP, mm Hg | 80 (71; 81) | 80 (74.5; 85) | 0.266 |
| HR, bpm | 71 ± 9.4 | 69 ± 10 | 0.336 |
| Drug therapy | |||
| Lipid-lowering therapy, n (%) | 36 (100) | 56 (100) | 1.000 |
| Dual antiplatelet therapy, n (%) | 36 (100) | 56 (100) | 1.000 |
| RAAS inhibitors, n (%) | 34 (94.4) | 54 (96.4) | 0.647 |
| β-blockers, n (%) | 33 (91.7) | 49 (87.5) | 0.527 |
| Calcium channel blockers, n (%) | 5 (13.9) | 8 (14.3) | 0.957 |
| Diuretics, n (%) | 14 (38.9) | 14 (25) | 0.157 |
| Indicators | “LS” Subgroup (n = 36) | “SS” Subgroup (n = 56) | p |
|---|---|---|---|
| Magnetic resonance imaging | |||
| EDVI, mL/m2 | 84 (72.2; 97.3) | 73.8 (65.7; 85.5) | 0.016 |
| ESVI, mL/m2 | 40.7 (35.6; 48.9) | 33.5 (28.4; 38.3) | <0.001 |
| LVEF, % | 49.1 ± 7.6 | 55.6 ± 5 | <0.001 |
| LVMMI, g/m2 | 60.8 (54.9; 72.6) | 58 (52.9; 64.2) | 0.175 |
| RWT | 0.39 (0.34; 0.46) | 0.43 (0.38; 0.54) | 0.076 |
| LCI | 1.95 (1.58; 2.3) | 1.31 (1.1; 1.5) | <0.001 |
| Echocardiography | |||
| EDVI, mL/m2 | 62.4 (52.8; 70.5) | 56.6 (44.9; 63.9) | 0.037 |
| ESVI, mL/m2 | 28.7 (22.6; 37.2) | 23.4 (18.7; 33.4) | 0.005 |
| LVEF, % | 50.9 ± 10.1 | 55.4 ± 8.8 | 0.027 |
| LVMMI, g/m2 | 113.5 (95.6; 145.5) | 107 (92.1; 124) | 0.216 |
| RWT | 0.39 (0.34; 0.49) | 0.48 (0.39; 0.55) | 0.003 |
| Indicators | β | SE | B | p |
|---|---|---|---|---|
| One-factor analysis | ||||
| “Pain-to-balloon” time ≥ 300 min | 0.252 | 0.111 | 0.245 | 0.026 |
| Q-MI | 0.462 | 0.093 | 0.457 | <0.001 |
| CHD duration | 0.431 | 0.197 | 0.065 | 0.040 |
| HscTn I, pg/mL | 0.477 | 0.093 | 0.000 | <0.001 |
| NT-proBNP, pg/mL | 0.418 | 0.104 | 0.001 | <0.001 |
| EDVI, mL/m2 | 0.245 | 0.102 | 0.008 | 0.019 |
| ESVI, mL/m2 | 0.299 | 0.101 | 0.015 | 0.004 |
| LVEF, % | −0.231 | 0.103 | −0.012 | 0.027 |
| RWT | −0.287 | 0.101 | −1.118 | 0.006 |
| RWT > 0.42 | −0.249 | 0.102 | −0.244 | 0.017 |
| Multifactorial analysis | ||||
| Free term | – | – | 0.235 | 0.011 |
| HscTn I, pg/mL | 0.353 | 0.096 | <0.001 | <0.001 |
| NT-proBNP, pg/mL | 0.337 | 0.096 | <0.001 | 0.001 |
| RWT > 0.42 | −0.226 | 0.095 | −0.225 | 0.020 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oleynikov, V.; Salyamova, L.; Alimov, N.; Donetskaya, N.; Avdeeva, I.; Averyanova, E. The Clinical Significance and Potential of Complex Diagnosis for a Large Scar Area Following Myocardial Infarction. Diagnostics 2025, 15, 1611. https://doi.org/10.3390/diagnostics15131611
Oleynikov V, Salyamova L, Alimov N, Donetskaya N, Avdeeva I, Averyanova E. The Clinical Significance and Potential of Complex Diagnosis for a Large Scar Area Following Myocardial Infarction. Diagnostics. 2025; 15(13):1611. https://doi.org/10.3390/diagnostics15131611
Chicago/Turabian StyleOleynikov, Valentin, Lyudmila Salyamova, Nikolay Alimov, Natalia Donetskaya, Irina Avdeeva, and Elena Averyanova. 2025. "The Clinical Significance and Potential of Complex Diagnosis for a Large Scar Area Following Myocardial Infarction" Diagnostics 15, no. 13: 1611. https://doi.org/10.3390/diagnostics15131611
APA StyleOleynikov, V., Salyamova, L., Alimov, N., Donetskaya, N., Avdeeva, I., & Averyanova, E. (2025). The Clinical Significance and Potential of Complex Diagnosis for a Large Scar Area Following Myocardial Infarction. Diagnostics, 15(13), 1611. https://doi.org/10.3390/diagnostics15131611







