Proposal of a Risk Stratification Model for Recurrence After Excisional Treatment of High-Grade Cervical Intraepithelial Neoplasia (HG-CIN)
Abstract
1. Introduction
2. Materials and Methods
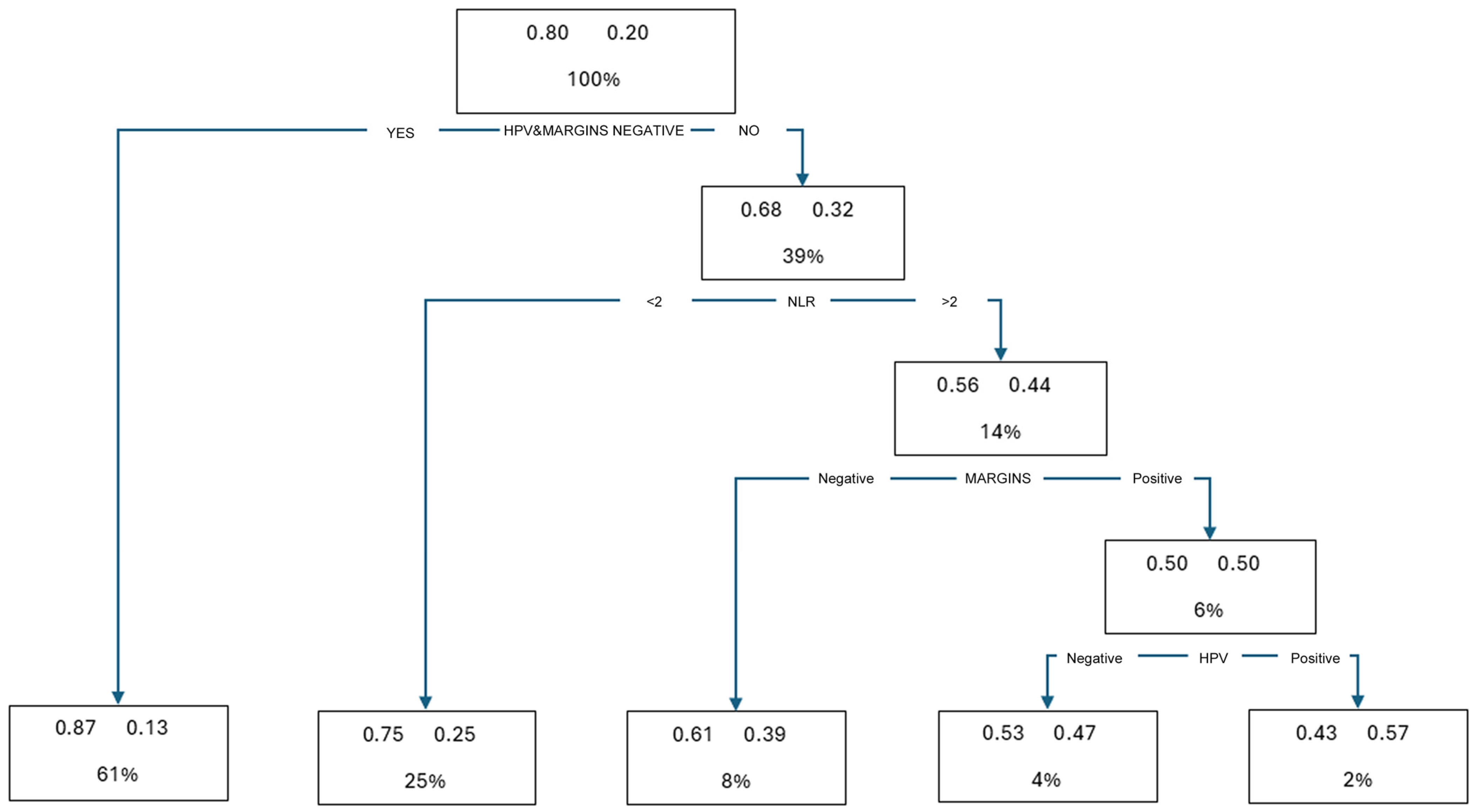
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gray, L.A.; Barnes, M.L.; Lee, J.J. Carcinoma-in-situ and Dysplasia of the Cervix. Ann. Surg. 1960, 151, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Antoine, T. Early diagnosis of cancer of the cervix. Am. J. Obstet. Gynecol. 1954, 68, 466–473. [Google Scholar] [CrossRef]
- Rawson, A.J.; Knoblich, R. A Clinicopathologic Study of 56 Cases Showing Atypical Epithelial Changes of the Cervix Uteri. Am. J. Obstet. Gynecol. 1957, 73, 120–126. [Google Scholar] [CrossRef]
- Petersen, O. Spontaneous course of cervical precancerous conditions. Am. J. Obstet. Gynecol. 1956, 72, 1063–1071. [Google Scholar] [CrossRef]
- Richart, R.M. Natural History of Cervical Intraepithelial Neoplasia. Clin. Obstet. Gynecol. 1967, 10, 748–784. [Google Scholar] [CrossRef]
- Eifel, P.J.; Klopp, A.H.; Berek, J.S.; Konstantinopoulos, P.A. Cancer of the cervix, vagina, and vulva. In DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology; Wolters Kluwer Health Pharma Solutions (Europe): Alphen aan den Rijn, The Netherlands, 2018; pp. 1172–1210. [Google Scholar]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods, and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef] [PubMed]
- AIRT Working Group. I Tumori in Italia—Rapporto 2006. Incidenza, Mortalità e Stime. Epidemiologia e Prevenzione 2006. Available online: https://www.registri-tumori.it (accessed on 18 June 2025).
- Holowaty, P.; Miller, A.B.; Rohan, T.; To, T. Natural History of Dysplasia of the Uterine Cervix. JNCI J. Natl. Cancer Inst. 1999, 91, 252–258. [Google Scholar] [CrossRef]
- Babes, A. Diagnostic du cancer du col uterin par les frottis. Presse Méd. 1928, 36, 451–454. [Google Scholar]
- Doorbar, J. The papillomavirus life cycle. J. Clin. Virol. 2005, 32, 7–15. [Google Scholar] [CrossRef]
- zur Hausen, H. Human Papillomaviruses and Their Possible Role in Squamous Cell Carcinomas. Curr. Top. Microbiol. Immunol. 1977, 78, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Dürst, M.; Gissmann, L.; Ikenberg, H.; zur Hausen, H. Papillomavirus DNA from a cervical carcinoma and its prevalence in cancer biopsy samples from different geographic regions. Proc. Natl. Acad. Sci. USA 1983, 80, 3812–3815. [Google Scholar] [CrossRef] [PubMed]
- Martin-Hirsch, P.P.; Paraskevaidis, E.; Bryant, A.; Dickinson, H.O. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst. Rev. 2013, 2013, CD001318. [Google Scholar] [CrossRef]
- Santesso, N.; Mustafa, R.A.; Wiercioch, W.; Kehar, R.; Gandhi, S.; Chen, Y.; Cheung, A.; Hopkins, J.; Khatib, R.; Ma, B.; et al. Systematic reviews and meta- analyses of benefits and harms of cryotherapy, LEEP, and cold knife conization to treat cervical intraepithelial neoplasia. Int. J. Gynecol. Obstet. 2016, 132, 266–271. [Google Scholar] [CrossRef]
- Castle, P.E.; Murokora, D.; Perez, C.; Alvarez, M.; Quek, S.C.; Campbell, C. Treatment of cervical intraepithelial lesions. Int. J. Gynecol. Obstet. 2017, 138, 20–25. [Google Scholar] [CrossRef]
- Kocken, M.; Helmerhorst, T.J.; Berkhof, J.; Louwers, J.A.; Nobbenhuis, M.A.E.; Bais, A.G.; Hogewoning, C.J.A.; Zaal, A.; Verheijen, R.H.M.; Snijders, P.J.F.; et al. Risk of recurrent high-grade cervical intraepithelial neoplasia after successful treatment: A long-term multi-cohort study. Lancet Oncol. 2011, 12, 441–450. [Google Scholar] [CrossRef]
- Simões, R.B.; Campaner, A.B. Post-cervical conization outcomes in patients with high-grade intraepithelial lesions. APMIS 2013, 121, 1153–1161. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.H.; Liu, F.S.; Kuo, C.J.; Chang, C.C.; Ho, E.S.C. Prediction of Persistence or Recurrence After Conization for Cervical Intraepithelial Neoplasia III. Obstet. Gynecol. 2006, 107, 830–835. [Google Scholar] [CrossRef]
- Bogani, G.; Di Donato, V.; Sopracordevole, F.; Ciavattini, A.; Ghelardi, A.; Lopez, S.; Simoncini, T.; Plotti, F.; Casarin, J.; Serati, M.; et al. Recurrence rate after loop electrosurgical excision procedure (LEEP) and laser Conization: A 5-year follow-up study. Gynecol. Oncol. 2020, 159, 636–641. [Google Scholar] [CrossRef]
- Hoffman, S.R.; Le, T.; Lockhart, A.; Sanusi, A.; Dal Santo, L.; Davis, M.; McKinney, D.A.; Brown, M.; Poole, C.; Willame, C.; et al. Patterns of persistent HPV infection after treatment for cervical intraepithelial neoplasia (CIN): A systematic review. Int. J. Cancer. 2017, 141, 8–23. [Google Scholar] [CrossRef]
- Bogani, G.; Pinelli, C.; Chiappa, V.; Martinelli, F.; Lopez, S.; Ditto, A.; Raspagliesi, F. Age-specific predictors of cervical dysplasia recurrence after primary conization: Analysis of 3212 women. J. Gynecol. Oncol. 2020, 31, e60. [Google Scholar] [CrossRef]
- Mariani, L.; Sandri, M.T.; Preti, M.; Origoni, M.; Costa, S.; Cristoforoni, P.; Bottari, F.; Sideri, M. HPV-Testing in Follow-up of Patients Treated for CIN2+ Lesions. J. Cancer 2016, 7, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Andersson, S.; Megyessi, D.; Belkić, K.; Alder, S.; Östensson, E.; Mints, M. Age, margin status, high-risk human papillomavirus and cytology independently predict recurrent high-grade cervical intraepithelial neoplasia up to 6 years after treatment. Oncol. Lett. 2021, 22, 684. [Google Scholar] [CrossRef]
- Oliveira, C.A.D.; Russomano, F.B.; Gomes Júnior, S.C.D.S.; Corrêa, F.D.M. Risk of persistent high-grade squamous intraepithelial lesion after electrosurgical excisional treatment with positive margins: A meta-analysis. Sao Paulo Med. J. 2012, 130, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Onuki, M.; Matsumoto, K.; Sakurai, M.; Ochi, H.; Minaguchi, T.; Satoh, T.; Yoshikawa, H. Posttreatment human papillomavirus testing for residual or recurrent high-grade cervical intraepithelial neoplasia: A pooled analysis. J. Gynecol. Oncol. 2016, 27, e3. [Google Scholar] [CrossRef]
- Cecchini, S.; Carozzi, F.; Confortini, M.; Zappa, M.; Ciatto, S. Persistent Human Papilloma Virus Infection as an Indicator of Risk of Recurrence of High-Grade Cervical Intraepithelial Neoplasia Treated by the Loop Electrosurgical Excision Procedure. Tumori J. 2004, 90, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Katki, H.A.; Schiffman, M.; Castle, P.E.; Fetterman, B.; Poitras, N.E.; Lorey, T.; Cheung, L.C.; Raine-Bennett, T.; Gage, J.C.; Kinney, W.K. Five-Year Risk of Recurrence After Treatment of CIN 2, CIN 3, or AIS. J. Low Genit. Tract Dis. 2013, 17 (Suppl. S1), S78–S84. [Google Scholar] [CrossRef] [PubMed]
- Bruhn, L.V.; Hyldig, N.; Schledermann, D. HPV Test as Test of Cure After Conization for CIN2+: A Nationwide Register-Based Cohort Study. J. Low. Genit. Tract Dis. 2022, 26, 287–292. [Google Scholar] [CrossRef]
- Kreimer, A.R.; Schiffman, M.; Herrero, R.; Hildesheim, A.; González, P.; Burk, R.D.; Porras, C.; Sherman, M.E.; Demuth, F.; Cheung, L. Long-term risk of recurrent cervical human papillomavirus infection and precancer and cancer following excisional treatment. Int. J. Cancer 2012, 131, 211–218. [Google Scholar] [CrossRef]
- Swift, B.E.; Wang, L.; Jembere, N.; Kupets, R. Risk of Recurrence After Treatment for Cervical Intraepithelial Neoplasia 3 and Adenocarcinoma in Situ of the Cervix: Recurrence of CIN 3 and AIS of Cervix. J. Low. Genit. Tract Dis. 2020, 24, 252–258. [Google Scholar] [CrossRef]
- Serati, M.; Siesto, G.; Carollo, S.; Formenti, G.; Riva, C.; Cromi, A.; Ghezzi, F. Risk factors for cervical intraepithelial neoplasia recurrence after conization: A 10-year study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 165, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Sand, F.; Frederiksen, K.; Kjaer, S.K. Risk of recurrent disease following conization of cervical intraepithelial neoplasia grade 3 according to post-conization HPV status and surgical margins. Gynecol. Oncol. 2022, 165, 472–477. [Google Scholar] [CrossRef]
- Farzaneh, F.; Faghih, N.; Hosseini, M.S.; Arab, M.; Ashrafganjoei, T.; Bahman, A. Evaluation of Neutrophil–Lymphocyte Ratio as a Prognostic Factor in Cervical Intraepithelial Neoplasia Recurrence. Asian Pac. J. Cancer Prev. 2019, 20, 2365–2372. [Google Scholar] [CrossRef]
- Origoni, M.; Cantatore, F.; Candotti, G.; Candiani, M. Prognostic Significance of Neutrophil/Lymphocytes Ratio (NLR) in Predicting Recurrence of Cervical Dysplasia. BioMed Res. Int. 2022, 2022, 1149789. [Google Scholar] [CrossRef] [PubMed]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic Role of Neutrophil- to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. JNCI J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef]
- Mizunuma, M.; Yokoyama, Y.; Futagami, M.; Aoki, M.; Takai, Y.; Mizunuma, H. The pretreatment neutrophil-to-lymphocyte ratio predicts therapeutic response to radiation therapy and concurrent chemoradiation therapy in uterine cervical cancer. Int. J. Clin. Oncol. 2015, 20, 989–996. [Google Scholar] [CrossRef]
- Ethier, J.L.; Desautels, D.N.; Templeton, A.J.; Oza, A.; Amir, E.; Lheureux, S. Is the neutrophil-to-lymphocyte ratio prognostic of survival outcomes in gynecologic cancers? A systematic review and meta-analysis. Gynecol. Oncol. 2017, 145, 584–594. [Google Scholar] [CrossRef]
- Wang, L.; Jia, J.; Lin, L.; Guo, J.; Ye, X.; Zheng, X.; Chen, Y. Predictive value of hematological markers of systemic inflammation for managing cervical cancer. Oncotarget 2017, 8, 44824–44832. [Google Scholar] [CrossRef] [PubMed]
- Bottari, F.; Iacobone, A.D.; Passerini, R.; Preti, E.P.; Sandri, M.T.; Cocuzza, C.E.; Gary, D.S.; Andrews, J.C. Human Papillomavirus Genotyping Compared With a Qualitative High-Risk Human Papillomavirus Test After Treatment of High-Grade Cervical Intraepithelial Neoplasia: A Systematic Review. Obstet. Gynecol. 2019, 134, 452–462. [Google Scholar] [CrossRef]
- Iacobone, A.D.; Radice, D.; Sandri, M.T.; Preti, E.P.; Guerrieri, M.E.; Vidal Urbinati, A.M.; Pino, I.; Franchi, D.; Passerini, R.; Bottari, F. Human papillomavirus same genotype persistence and risk of cervical intraepithelial neoplasia2+ recurrence. Cancers 2021, 13, 3664. [Google Scholar] [CrossRef]
- Melnikow, J.; McGahan, C.; Sawaya, G.F.; Ehlen, T.; Coldman, A. Cervical intraepithelial neoplasia outcomes after treatment: Long-term follow-up from the British Columbia Cohort Study. J. Natl. Cancer Inst. 2009, 101, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Dominoni, M.; Barcellini, A.; Pasquali, M.F.; De Silvestri, A.; Ferretti, V.V.; Cesari, S.; Fiandrino, G.; Orlandi, E.; Gardella, B. The Role of Neutrophil-Lymphocytes Ratio in the Prognosis of CIN2+ Recurrence after Excisional Treatment. Gynecol. Obstet. Investig. 2024, 89, 295–303. [Google Scholar] [CrossRef]
- Herrera-Gomez, A.; Porter, R.M. Mixed linear-nonlinear least squares regression. arXiv 2017, arXiv:1703.04181v1. [Google Scholar] [CrossRef]
- Kyrgiou, M.; Mitra, A.; Arbyn, M.; Stasinou, S.M.; Martin-Hirsch, P.; Bennett, P.; Paraskevaidis, E. Fertility, and early pregnancy outcomes after treatment for cervical intraepithelial neoplasia: Systematic review and meta-analysis. BMJ 2014, 349, g6192. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kyrgiou, M.; Mitra, A.; Arbyn, M.; Paraskevaidi, M.; Athanasiou, A.; Martin-Hirsch, P.P.; Bennett, P.; Paraskevaidis, E. Fertility, and early pregnancy outcomes after conservative treatment for cervical intraepithelial neoplasia. Cochrane Database Syst. Rev. 2015, 9, CD008478. [Google Scholar] [CrossRef]
- Arbyn, M.; Redman, C.W.E.; Verdoodt, F.; Kyrgiou, M.; Tzafetas, M.; Ghaem-Maghami, S.; Petry, K.U.; Leeson, S.; Bergeron, C.; Nieminen, P.; et al. Incomplete excision of cervical precancer as a predictor of treatment failure: A systematic review and meta- analysis. Lancet Oncol. 2017, 18, 1665–1679. [Google Scholar] [CrossRef]
- Ghaem-Maghami, S.; Sagi, S.; Majeed, G.; Soutter, W.P. Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: A meta-analysis. Lancet Oncol. 2007, 8, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Bonde, J.; Bottari, F.; Iacobone, A.D.; Cocuzza, C.E.; Sandri, M.T.; Bogliatto, F.; Khan, K.S.; Ejegod, D.M.; Gary, D.S.; Andrews, J.C. Human Papillomavirus Same Genotype Persistence and Risk: A Systematic Review. J. Low. Genit. Tract Dis. 2021, 25, 27–37. [Google Scholar] [CrossRef]
- Kechagias, K.S.; Kalliala, I.; Bowden, S.J.; Athanasiou, A.; Paraskevaidi, M.; Paraskevaidis, E.; Dillner, J.; Nieminen, P.; Strander, B.; Sasieni, P. Role of human papillomavirus (HPV) vaccination on HPV infection and recurrence of HPV related disease after local surgical treatment: Systematic review and meta-analysis. BMJ 2022, 378, e070135. [Google Scholar] [CrossRef]
- Mitra, A.; MacIntyre, D.A.; Marchesi, J.R.; Lee, Y.S.; Bennett, P.R.; Kyrgiou, M. The vaginal microbiota, human papillomavirus infection and cervical intraepithelial neoplasia: What do we know and where are we going next? Microbiome 2016, 4, 58. [Google Scholar] [CrossRef]
- Yang, Z.; Zhang, Y.; Stubbe-Espejel, A.; Zhao, Y.; Liu, M.; Li, J.; Zhao, Y.; Tong, G.; Liu, N.; Qi, L. Vaginal microbiota and personal risk factors associated with HPV status conversion—A new approach to reduce the risk of cervical cancer? PLoS ONE 2022, 17, e0270521. [Google Scholar] [CrossRef]
- Kyrgiou, M.; Moscicki, A.B. Vaginal microbiome and cervical cancer. Semin. Cancer Biol. 2022, 86 Pt 3, 189–198. [Google Scholar] [CrossRef]
- Li, X.; Xiang, F.; Liu, T.; Chen, Z.; Zhang, M.; Li, J.; Kang, X.; Wu, R. Leveraging existing 16S rRNA gene surveys to decipher microbial signatures and dysbiosis in cervical carcinogenesis. Sci. Rep. 2024, 14, 11532. [Google Scholar] [CrossRef] [PubMed]
- Bogani, G.; Lalli, L.; Sopracordevole, F.; Ciavattini, A.; Ghelardi, A.; Simoncini, T.; Plotti, F.; Casarin, J.; Serati, M.; Pinelli, C.; et al. Development of a Nomogram Predicting the Risk of Persistence/Recurrence of Cervical Dysplasia. Vaccines 2022, 10, 579. [Google Scholar] [CrossRef] [PubMed]
- Zahorec, R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl. Lek. Listy. 2021, 122, 474–488. [Google Scholar] [CrossRef] [PubMed]
- Zou, P.; Yang, E.; Li, Z. Neutrophil-to-lymphocyte ratio is an independent predictor for survival outcomes in cervical cancer: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 21917. [Google Scholar] [CrossRef]
- Chun, S.; Shin, K.; Kim, K.H.; Kim, H.Y.; Eo, W.; Lee, J.Y.; Namkung, J.; Kwon, S.H.; Koh, S.B.; Kim, H.B. The Neutrophil-Lymphocyte Ratio Predicts Recurrence of Cervical Intraepithelial Neoplasia. J. Cancer 2017, 8, 2205–2211. [Google Scholar] [CrossRef]
- Hajizadeh, N.; Baghestani, A.R.; Pourhoseingholi, M.A.; Khadem Maboudi, A.A.; Farzaneh, F.; Faghih, N. Evaluation of the Factors Affecting the Cure Rate of Cervical Intra-Epithelial Neoplasia Recurrence Using Defective Models. J. Res. Health Sci. 2021, 21, e00524. [Google Scholar] [CrossRef]
- Ghaem-Maghami, S.; De-Silva, D.; Tipples, M.; Lam, S.; Perryman, K.; Soutter, W. Determinants of success in treating cervical intraepithelial neoplasia. BJOG 2011, 118, 679–684. [Google Scholar] [CrossRef]
- Linee Guida Condivise per la Prevenzione del Carcinoma Della Cervice Uterina. Raccomandazioni per la Gestione Delle Donne in Follow-Up Post Trattamento per CIN2 e CIN3 Raccomandazioni Pubblicate nel Sistema Nazionale Linee Guida Roma, 14 Ottobre 2021—ISCi in Collaborazione con AIO, AOGOI, SIAPEC-IAV, SICi, SICPCV, SIGO, SItI, SIV-ISV. Available online: https://gisci.it/documenti/linee-guida/LG_197_GISCi_Biomarcatori-screening-cervicale_29ago24.pdf (accessed on 23 March 2023).
- Rossi, P.G.; Ricciardi, A.; Cohet, C.; Palazzo, F.; Furnari, G.; Valle, S.; Largeron, N.; Federici, A. Epidemiology and costs of cervical cancer screening and cervical dysplasia in Italy. BMC Public Health 2009, 9, 71. [Google Scholar] [CrossRef]
| A1 | A2 | A3 |
|---|---|---|
| 1 | 1 | 1 |
| 1 | 1 | 0 |
| 1 | 0 | 1 |
| 0 | 1 | 1 |
| 1 | 0 | 0 |
| 0 | 1 | 0 |
| 0 | 0 | 1 |
| 0 | 0 | 0 |
| Patient Age | min | 18 | |
| max | 73 | ||
| mean | 38.4 | ||
| median | 37.5 | ||
| Cone Histology | CIN1 | 39 (9.1%) | |
| CIN2 | 192 (44.9%) | ||
| CIN3 | 162 (37.9%) | ||
| CIS | 33 (7.7%) | ||
| G-CIN2 | 1 (0.2%) | ||
| G-CIN3 | 1 (0.2%) | ||
| Post-Treatment hrHPV | positive | 115 (27%) | |
| negative | 313 (73%) | ||
| Surgical Margins | positive | 65 (15.2%) | |
| negative | 363 (84.8%) | ||
| Recurrences | yes | 86 (20.1%) | at 12 months: 78 (90.6%) |
| at 24 months: 8 (9.4%) | |||
| no | 342 (79.9%) |
| Variables | p-Value | OR | 95% CI | |
|---|---|---|---|---|
| NLR ≥ 2 + HPV persistence | 0.000 | 3.417 | 1.733 | 6.737 |
| NLR ≥ 2 + Margins | 0.000 | 4.507 | 2.006 | 10.126 |
| HPV persistence + Margins | 0.000 | 6.913 | 2.202 | 21.705 |
| NLR ≥ 2 + HPV persistence + Margins | 0.027 | 5.512 | 1.210 | 25.109 |
| No Risk Factors | 0.000 | 0.243 | 0.127 | 0.463 |
| Margins | hrHPV | NLR ≥ 2 | % Recurrence Risk | |
|---|---|---|---|---|
| + | + | + | 69.42 |  |
| + | + | − | 53.34 | |
| + | − | + | 42.84 | |
| − | + | + | 36.79 | |
| + | − | − | 27.69 | |
| − | + | − | 22.99 | |
| − | − | + | 19.35 | |
| − | − | − | 7.48 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cantatore, F.; Agrillo, N.; Camussi, A.; Colella, L.; Origoni, M. Proposal of a Risk Stratification Model for Recurrence After Excisional Treatment of High-Grade Cervical Intraepithelial Neoplasia (HG-CIN). Diagnostics 2025, 15, 1585. https://doi.org/10.3390/diagnostics15131585
Cantatore F, Agrillo N, Camussi A, Colella L, Origoni M. Proposal of a Risk Stratification Model for Recurrence After Excisional Treatment of High-Grade Cervical Intraepithelial Neoplasia (HG-CIN). Diagnostics. 2025; 15(13):1585. https://doi.org/10.3390/diagnostics15131585
Chicago/Turabian StyleCantatore, Francesco, Nadia Agrillo, Alessandro Camussi, Lucrezia Colella, and Massimo Origoni. 2025. "Proposal of a Risk Stratification Model for Recurrence After Excisional Treatment of High-Grade Cervical Intraepithelial Neoplasia (HG-CIN)" Diagnostics 15, no. 13: 1585. https://doi.org/10.3390/diagnostics15131585
APA StyleCantatore, F., Agrillo, N., Camussi, A., Colella, L., & Origoni, M. (2025). Proposal of a Risk Stratification Model for Recurrence After Excisional Treatment of High-Grade Cervical Intraepithelial Neoplasia (HG-CIN). Diagnostics, 15(13), 1585. https://doi.org/10.3390/diagnostics15131585








