The Impact of Cardiovascular Diseases on Postoperative Complications in Orthopedic Trauma Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
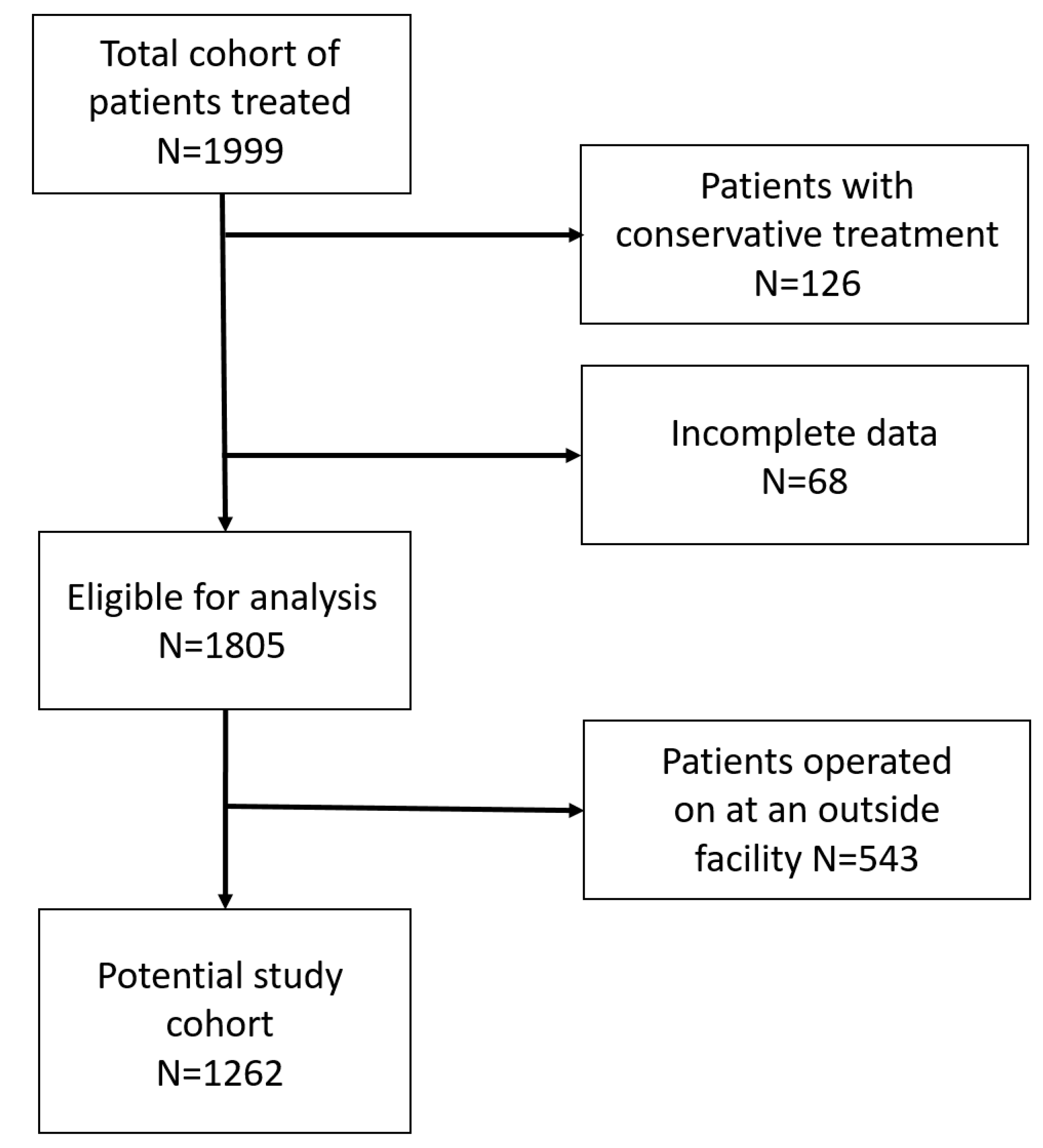
2.3. Exclusion Criteria
2.4. Classification of Postoperative Complication
2.5. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global Cardiovascular Risk, C.; Magnussen, C.; Ojeda, F.M.; Leong, D.P.; Alegre-Diaz, J.; Amouyel, P.; Aviles-Santa, L.; De Bacquer, D.; Ballantyne, C.M.; Bernabe-Ortiz, A.; et al. Global Effect of Modifiable Risk Factors on Cardiovascular Disease and Mortality. N. Engl. J. Med. 2023, 389, 1273–1285. [Google Scholar] [CrossRef]
- Joseph, P.; Leong, D.; McKee, M.; Anand, S.S.; Schwalm, J.D.; Teo, K.; Mente, A.; Yusuf, S. Reducing the Global Burden of Cardiovascular Disease, Part 1: The Epidemiology and Risk Factors. Circ. Res. 2017, 121, 677–694. [Google Scholar] [CrossRef] [PubMed]
- Dzupa, V.; Waldauf, P.; Motovska, Z.; Widimsky, P.; Ondrakova, M.; Bartoska, R.; Jezek, M.; Lena, T.; Popelka, O.; Krbec, M. Risk comparison of bleeding and ischemic perioperative complications after acute and elective orthopedic surgery in patients with cardiovascular disease. Arch. Orthop. Trauma Surg. 2016, 136, 907–911. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Pang, P.; Luo, Z.; Cai, W.; Li, W.; Hao, J. Prevalence and risk factors for proximal deep vein thrombosis at admission in patients with traumatic fractures: A multicenter retrospective study. Front. Cardiovasc. Med. 2024, 11, 1372268. [Google Scholar] [CrossRef]
- Pharaon, S.K.; Schoch, S.; Marchand, L.; Mirza, A.; Mayberry, J. Orthopaedic traumatology: Fundamental principles and current controversies for the acute care surgeon. Trauma Surg. Acute Care Open 2018, 3, e000117. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibanes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Wardle, M.; Nair, A.; Saunders, S.; Armstrong, I.; Charalampopoulos, A.; Elliot, C.; Hameed, A.; Hamilton, N.; Harrington, J.; Keen, C.; et al. Elective lower limb orthopedic arthroplasty surgery in patients with pulmonary hypertension. Pulm. Circ. 2022, 12, e12019. [Google Scholar] [CrossRef]
- Damen, J.A.; Hooft, L.; Schuit, E.; Debray, T.P.; Collins, G.S.; Tzoulaki, I.; Lassale, C.M.; Siontis, G.C.; Chiocchia, V.; Roberts, C.; et al. Prediction models for cardiovascular disease risk in the general population: Systematic review. BMJ 2016, 353, i2416. [Google Scholar] [CrossRef]
- Minja, N.W.; Nakagaayi, D.; Aliku, T.; Zhang, W.; Ssinabulya, I.; Nabaale, J.; Amutuhaire, W.; de Loizaga, S.R.; Ndagire, E.; Rwebembera, J.; et al. Cardiovascular diseases in Africa in the twenty-first century: Gaps and priorities going forward. Front. Cardiovasc. Med. 2022, 9, 1008335. [Google Scholar] [CrossRef]
- WHO. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; WHO Technical Report Series 854; WHO: Geneva, Switzerland, 1995; pp. 1–452. [Google Scholar]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46 (Suppl. S1), S19–S40. [Google Scholar] [CrossRef]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z.; Ad Hoc, E.W.G. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M.; Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef]
- Liu, F.L.; Lin, C.S.; Yeh, C.C.; Shih, C.C.; Cherng, Y.G.; Wu, C.H.; Chen, T.L.; Liao, C.C. Risk and outcomes of fracture in peripheral arterial disease patients: Two nationwide cohort studies. Osteoporos. Int. 2017, 28, 3123–3133. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, X.; Qian, H.; Ye, J.; Qian, J.; Hua, J. Correlation between common postoperative complications of prolonged bed rest and quality of life in hospitalized elderly hip fracture patients. Ann. Palliat. Med. 2020, 9, 1125–1133. [Google Scholar] [CrossRef]
- Koudouna, S.; Evangelopoulos, D.S.; Sarantis, M.; Chronopoulos, E.; Dontas, I.A.; Pneumaticos, S. The Effect of Postoperative Physical Therapy Following Hip Fracture: A Literature Review. Cureus 2023, 15, e37676. [Google Scholar] [CrossRef]
- Brassard, P.; Jensen, A.S.; Nordsborg, N.; Gustafsson, F.; Moller, J.E.; Hassager, C.; Boesgaard, S.; Hansen, P.B.; Olsen, P.S.; Sander, K.; et al. Central and peripheral blood flow during exercise with a continuous-flow left ventricular assist device: Constant versus increasing pump speed: A pilot study. Circ. Heart Fail. 2011, 4, 554–560. [Google Scholar] [CrossRef]
- Hess, D.E.; Carstensen, S.E.; Moore, S.; Dacus, A.R. Smoking Increases Postoperative Complications After Distal Radius Fracture Fixation: A Review of 417 Patients From a Level 1 Trauma Center. Hand 2018, 15, 686–691. [Google Scholar] [CrossRef]
- Gallagher, L.T.; Erickson, C.; D’Alessandro, A.; Schaid, T.; Thielen, O.; Hallas, W.; Mitra, S.; Stafford, P.; Moore, E.E.; Silliman, C.C.; et al. Smoking primes the metabolomic response in trauma. J. Trauma Acute Care Surg. 2024, 97, 48–56. [Google Scholar] [CrossRef]
- Kaneko, A.; Naito, K.; Obata, H.; Nagura, N.; Sugiyama, Y.; Goto, K.; Kawakita, S.; Iwase, Y.; Kaneko, K. Influence of Smoking in the Clinical Outcomes of Distal Radius Fractures. J. Hand Microsurg. 2022, 14, 212–215. [Google Scholar] [CrossRef]
- Galivanche, A.R.; FitzPatrick, S.; Dussik, C.; Malpani, R.; Nduaguba, A.; Varthi, A.G.; Grauer, J.N. A Matched Comparison of Postoperative Complications Between Smokers and Nonsmokers Following Open Reduction Internal Fixation of Distal Radius Fractures. J. Hand Surg. Am. 2021, 46, 1–9.e4. [Google Scholar] [CrossRef] [PubMed]
- Maurer, E.; Wallmeier, V.; Reumann, M.; Ehnert, S.; Ihle, C.; Schreiner, A.J.; Flesch, I.; Stollhof, L.E.; Histing, T.; Nussler, A.K. Increased Age, Cardiovascular Comorbidities, COPD, and Diabetes mellitus Determine Excess Mortality in Trauma Patients with SSI or Chronic Wounds. Z. Orthop. Unfall. 2022, 161, 412–421. [Google Scholar]
- Maurer, E.; Wallmeier, V.; Reumann, M.K.; Ehnert, S.; Ihle, C.; Schreiner, A.J.; Flesch, I.; Issack, P.S.; Stollhof, L.E.; Nüssler, P.A.K. Risk of Malnutrition in Orthopedic Trauma Patients with Surgical Site Infections is Associated with Increased Morbidity and Mortality—A 3-Year Follow-up Study. Injury 2020, 51, 2219–2229. [Google Scholar] [CrossRef]
- Sagherian, B.H.; Hoballah, J.J.; Tamim, H. Comparing the 30-Day Complications Between Smokers and Nonsmokers Undergoing Surgical Fixation of Ankle Fractures. Foot Ankle Orthop. 2022, 7, 24730114221115677. [Google Scholar] [CrossRef] [PubMed]
- Freigang, V.; Muller, K.; Ernstberger, A.; Kaltenstadler, M.; Bode, L.; Pfeifer, C.; Alt, V.; Baumann, F. Reduced Recovery Capacity After Major Trauma in the Elderly: Results of a Prospective Multicenter Registry-Based Cohort Study. J. Clin. Med. 2020, 9, 2356. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.J.; Manalili, K.; Jolley, R.J.; Zelinsky, S.; Quan, H.; Lu, M. How to practice person-centred care: A conceptual framework. Health Expect. 2018, 21, 429–440. [Google Scholar] [CrossRef]
- Søgaard, M.B.; Andresen, K.; Kristiansen, M. Systematic review of patient-engagement interventions: Potentials for enhancing person-centred care for older patients with multimorbidity. BMJ Open 2021, 11, e048558. [Google Scholar] [CrossRef]
- McIsaac, D.I.; Talarico, R.; Jerath, A.; Wijeysundera, D.N. Days alive and at home after hip fracture: A cross-sectional validation of a patient-centred outcome measure using routinely collected data. BMJ Qual. Saf. 2023, 32, 546–556. [Google Scholar] [CrossRef]
- Murphy, R.; Waters, R.; Murphy, A.; McDermott, S.; Reddin, C.; Hernon, O.; Davies, N.; Alvarez-Iglesias, A.; Twomey, E.; O’Shea, E. Risk-Based Screening of Atrial Fibrillation in General Practice (R-BEAT): A randomised Cross-over Trial. QJM Int. J. Med. 2025, 118, 166–173. [Google Scholar] [CrossRef]
- Miguel, C.B.; Andrade, R.d.S.; Mazurek, L.; Martins-de-Abreu, M.C.; Miguel-Neto, J.; Barbosa, A.d.M.; Silva, G.P.; Góes-Neto, A.; Soares, S.d.C.; Lazo-Chica, J.E. Emerging pharmacological interventions for chronic venous insufficiency: A comprehensive systematic review and meta-analysis of efficacy, safety, and therapeutic advances. Pharmaceutics 2025, 17, 59. [Google Scholar] [CrossRef] [PubMed]
- Paladugu, S.V.; Savlania, A.; Hari, G.; Singla, T.; Gorsi, U.; Kaman, L. Impact of static foot disorder and ankle range of motion in chronic venous insufficiency patients. Phlebology 2025. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.-R.; Liu, M.-Y.; Ni, Q.-H.; Cai, F.; Tang, F.; Yu, Z.-Y.; Zhang, J.-B.; Zhang, L.; Zhang, W.W.; Li, C.-M. Clinical Guidelines on Compression Therapy in Venous Diseases. Ann. Vasc. Surg. 2024, 110, 183–203. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.L. Valvular heart disease: The oncoming tsunami. In European Heart Journal-Cardiovascular Imaging; Oxford University Press: Oxford, UK, 2024; Volume 25, pp. 1059–1060. [Google Scholar]
- Sengupta, P.P.; Kluin, J.; Lee, S.-P.; Oh, J.K.; Smits, A.I. The future of valvular heart disease assessment and therapy. Lancet 2024, 403, 1590–1602. [Google Scholar] [CrossRef]
| Characteristics | All | Upper Arm | Lower Arm | Femur | Tibia |
|---|---|---|---|---|---|
| N = 1262 | N = 94 | N = 155 | N = 119 | N = 297 | |
| Age (years) | 57.2 ± 17.6 | 59.3 ± 16.3 | 53.1 ± 18.0 | 65.3 ± 19.2 | 50.1 ± 16.0 |
| Men | 655 (51.9%) | 37 (39.4%) | 62 (40.0%) | 305 (65.3%) | 305 (65.3%) |
| Size (cm) | 171.5 ± 9.6 | 169.2 ± 9.2 | 171.6 ± 9.0 | 171.1 ± 10.9 | 173.7 ± 8.9 |
| BMI (kg/m2) | 27.1 ± 5.0 | 26.5 ± 4.9 | 26.6 ± 4.9 | 25.3 ± 4.8 | 27.2 ± 4.8 |
| Smoking status | |||||
| Non-smoker | 681 (54.0%) | 55 (58.5%) | 99 (63.9%) | 68 (57.1%) | 144 (48.5%) |
| Smoker | 581 (46.0%) | 39 (41.5%) | 56 (36.1%) | 51 (42.9%) | 153 (51.5%) |
| Mobility | |||||
| Unrestricted | 1028 (81.5%) | 83 (88.3%) | 151 (97.4%) | 75 (63.0%) | 251 (84.5%) |
| Restricted | 234 (18.5%) | 11 (11.7%) | 4 (2.6%) | 44 (37.0%) | 46 (15.5%) |
| CCI | |||||
| 0 points | 885 (70.1%) | 71 (75.5%) | 135 (87.1%) | 57 (47.9%) | 236 (79.5%) |
| 1–2 points | 267 (21.2%) | 19 (20.2%) | 17 (11.0%) | 43 (36.1%) | 45 (15.2%) |
| 3–4 points | 82 (6.5%) | 3 (3.2%) | 2 (1.3%) | 13 (10.9%) | 9 (3.0%) |
| >4 points | 28 (2.2%) | 1 (1.1%) | 1 (0.6%) | 6 (5.0%) | 7 (2.4%) |
| NRS | |||||
| NRS < 3 | 1056 (83.7%) | 78 (83.5%) | 144 (92.9%) | 76 (63.9%) | 256 (86.2%) |
| NRS ≥ 3 | 205 (16.3%) | 15 (16.5%) | 11 (7.1%) | 43 (36.1%) | 41 (13.8%) |
| Average number of comorbidities | 2.5 ± 2.5 | 2.2 ± 1.9 | 1.5 ± 1.8 | 1.4 ± 1.7 | 1.7 ± 2.0 |
| Average number of cardiovascular comorbidities | 0.9 ± 1.2 | 0.7 ± 1.0 | 0.5 ± 9.6 | 3.1 ± 2.7 | 0.6 ± 1.0 |
| Medication intake | 790 (62.6%) | 63 (67.0%) | 71 (45.8%) | 87 (73.1%) | 143 (48.1%) |
| Complication classification | 328 (26.0%) | 21 (22.3%) | 24 (15.5%) | 51 (42.9%) | 74 (24.9%) |
| Clavien–Dindo | |||||
| Clavien–Dindo 0 | 643 (51.0%) | 39 (41.5%) | 85 (54.8%) | 49 (41.2%) | 153 (51.5%) |
| Clavien–Dindo I | 291 (23.0%) | 34 (36.2%) | 48 (29.7%) | 19 (16.0%) | 70 (23.6%) |
| Clavien–Dindo II | 135 (10.7%) | 10 (10.6%) | 9 (5.8%) | 25 (21.0%) | 32 (10.8%) |
| Clavien–Dindo III | 122 (9.7%) | 9 (9.6%) | 12 (7.7%) | 8 (6.7%) | 35 (11.8%) |
| Clavien–Dindo IV | 70 (5.5%) | 1 (2.1%) | 3 (1.9%) | 18 (15.1%) | 7 (2.4%) |
| Clavien–Dindo V | 1 (0.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Cardiovascular Disease | All | No Complication | Complication | p-Value |
|---|---|---|---|---|
| N = 1262 | N = 934 | N = 328 | ||
| Hypertension | 507 (40.2%) | 365 (39.1%) | 142 (43.3%) | 0.19 |
| CHD/AP | 111 (8.9%) | 66 (7.1%) | 45 (13.7%) | <0.001 |
| Heart failure | 76 (6.0%) | 42 (4.5%) | 34 (10.4%) | <0.001 |
| Heart valve disease | 52 (4.1%) | 29 (3.1%) | 23 (7.1%) | 0.003 |
| Cardiac arrhythmia | 113 (9.0%) | 67 (7.2%) | 46 (14.0%) | <0.001 |
| Infectious heart diseases | 4 (0.3%) | 1 (0.1%) | 3 (1.0%) | 0.06 |
| Pulmonary heart diseases | 28 (2.2%) | 15 (1.6%) | 13 (4.0%) | 0.017 |
| Cerebrovasc. diseases/TIA | 48 (3.8%) | 30 (3.2%) | 18 (5.5%) | 0.09 |
| PAD | 40 (3.2%) | 24 (2.6%) | 16 (4.9%) | 0.045 |
| CVI | 76 (6.0%) | 41 (4.4%) | 35 (10.7%) | <0.001 |
| Other cardiovasc. diseases | 7 (0.6%) | 4 (0.4%) | 3 (1.0%) | 0.08 |
| Cardiovascular Disease | Upper Arm | No Complication | Complication | p-Value |
|---|---|---|---|---|
| N = 94 | N = 73 | N = 21 | ||
| Hypertension | 37 (39.2%) | 28 (38.4%) | 9 (42.9%) | 0.80 |
| CHD/AP | 9 (9.6%) | 7 (9.6%) | 2 (9.5%) | 1.00 |
| Heart failure | 7 (7.4%) | 5 (6.8%) | 2 (9.5%) | 0.65 |
| Heart valve disease | 1 (1.0%) | 1 (1.4%) | 0 (0.0%) | 1.00 |
| Cardiac arrhythmia | 9 (9.6%) | 6 (8.2%) | 3 (14.3%) | 0.41 |
| Infectious heart diseases | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Pulmonary heart diseases | 1 (1.0%) | 0 (0.0%) | 1 (4.8%) | 0.22 |
| Cerebrovasc. diseases/TIA | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| pAVD | 1 (1.0%) | 1 (1.4%) | 0 (0.0%) | 1.00 |
| CVI | 3 (3.2%) | 3 (4.1%) | 0 (0.0%) | 1.00 |
| Other cardiovasc. diseases | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Cardiovascular Disease | Lower Arm | No Complication | Complication | p-Value |
|---|---|---|---|---|
| N = 155 | N = 131 | N = 24 | ||
| Hypertension | 43 (27.7%) | 35 (26.7%) | 8 (33.3%) | 0.62 |
| CHD/AP | 5 (3.2%) | 5 (3.8%) | 0 (0.0%) | 1.00 |
| Heart failure | 2 (1.3%) | 2 (1.5%) | 0 (0.0%) | 1.00 |
| Heart valve disease | 2 (1.3%) | 1 (0.8%) | 1 (4.2%) | 0.29 |
| Cardiac arrhythmia | 6 (3.9%) | 3 (2.3%) | 3 (12.5%) | 0.048 |
| Infectious heart diseases | 1 (0.6%) | 1 (0.8%) | 0 (0.0%) | 1.00 |
| Pulmonary heart diseases | 3 (1.9%) | 1 (0.8%) | 2 (8.3%) | 0.40 |
| Cerebrovasc. diseases/TIA | 2 (1.3%) | 1 (0.8%) | 1 (4.2%) | 0.29 |
| pAVD | 1 (0.6%) | 1 (0.8%) | 0 (0.0%) | 1.00 |
| CVI | 5 (3.2%) | 4 (3.1%) | 1 (4.2%) | 0.57 |
| Other cardiovasc. diseases | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Cardiovascular Disease | Femur | No Complication | Complication | p-Value |
|---|---|---|---|---|
| N = 119 | N = 68 | N = 51 | ||
| Hypertension | 59 (49.6%) | 34 (50.0%) | 25 (49.0%) | 1.00 |
| CHD/AP | 24 (20.2%) | 10 (14.7%) | 14 (27.5%) | 0.11 |
| Heart failure | 16 (13.4%) | 8 (12.5%) | 8 (15.7%) | 0.59 |
| Heart valve disease | 10 (8.4%) | 4 (5.9%) | 6 (11.8%) | 0.32 |
| Cardiac arrhythmia | 21 (17.6%) | 9 (13.2%) | 12 (23.5%) | 0.16 |
| Infectious heart diseases | 2 (1.7%) | 0 (0.0%) | 2 (3.9%) | 0.18 |
| Pulmonary heart diseases | 3 (2.5%) | 1 (1.5%) | 2 (3.9%) | 0.58 |
| Cerebrovasc. diseases/TIA | 8 (6.7%) | 4 (5.9%) | 4 (7.8%) | 0.72 |
| pAVD | 6 (5.0%) | 3 (4.4%) | 3 (5.9%) | 1.00 |
| CVI | 9 (7.6%) | 4 (5.9%) | 5 (9.8%) | 0.50 |
| Other cardiovasc. diseases | 1 (0.1%) | 0 (0.0%) | 1 (2.0%) | 0.42 |
| Cardiovascular Disease | Lower Leg | No Complication | Complication | p-Value |
|---|---|---|---|---|
| N = 279 | N = 223 | N = 74 | ||
| Hypertension | 79 (28.3%) | 56 (25.2%) | 23 (31.1%) | 0.36 |
| CHD/AP | 15 (5.4%) | 8 (3.6%) | 7 (9.5%) | 0.06 |
| Heart failure | 10 (3.6%) | 5 (2.2%) | 5 (6.8%) | 0.13 |
| Heart valve disease | 9 (3.2%) | 4 (1.8%) | 5 (6.6%) | 0.046 |
| Cardiac arrhythmia | 15 (5.4%) | 9 (4.0%) | 6 (8.1%) | 0.22 |
| Infectious heart diseases | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Pulmonary heart diseases | 3 (1.1%) | 1 (0,4%) | 2 (2.7%) | 0.15 |
| Cerebrovasc. diseases/TIA | 6 (2.2%) | 4 (1.8%) | 2 (2.7%) | 0.64 |
| pAVD | 9 (3.2%) | 5 (2.2%) | 4 (5.4%) | 0.23 |
| CVI | 15 (5.4%) | 7 (3.1%) | 8 (10.8%) | 0.015 |
| Other cardiovasc. diseases | 1 (0.4%) | 1 0.4%) | 0 (0.0%) | 1.00 |
| Characteristics | All N = 1262 | Upper Arm N = 94 | Lower Arm N = 155 | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% KI) | p-Value | Odds Ratio (95% KI) | p-Value | Odds Ratio (95% KI) | p-Value | |
| Age (years) | 1.00 (0.99–1.01) | 0.72 | 1.00 (0.96–1.03) | 0.85 | 0.99 (0.96–1.02) | 0.43 |
| Sex (male) | 1.06 (0.80–1.40) | 0.68 | 1.23 (0.40–3.16) | 0.82 | 0.71 (0.25–2.02) | 0.52 |
| No of cardiovascular diseases | 1.21 (1.08–1.37) | 0.002 | 1.19 (0.64–2.22) | 0.58 | 2.03 (1.12–3.67) | 0.019 |
| Smoker | 1.56 (1.20–2.04) | <0.001 | 1.02 (0.38–2.78) | 0.97 | 2.40 (0.93–6.25) | 0.07 |
| NRS | 1.75 (1.24–2.48) | 0.002 | 1.32 (0.30–5.77) | 0.71 | 0.520 (0.49–5.47) | 0.59 |
| Mobility | 1.65 (1.19–2.30) | 0.003 | 0.53 (0.08–3.48) | 0.51 | 1.00 (0.00–0.00) | 1.00 |
| Characteristics | All N = 1262 | Femur N = 119 | Lower Leg N = 279 | |||
|---|---|---|---|---|---|---|
| Odds Ratio (95% KI) | p-Value | Odds Ratio (95% KI) | p-Value | Odds Ratio (95% KI) | p-Value | |
| Age (years) | 1.00 (0.99–1.01) | 0.72 | 1.01 (0.98–1.04) | 0.46 | 0.99 (0.97–1.01) | 0.32 |
| Sex (men) | 1.06 (0.80–1.40) | 0.68 | 1.54 (0.59–3.98) | 0.38 | 1.05 (0.58–1.90) | 0.88 |
| No. of cardiovascular diseases | 1.21 (1.08–1.37) | 0.002 | 1.05 (0.78–1.40) | 0.76 | 1.44 (1.07–1.94) | 0.015 |
| Smoker | 1.56 (1.20–2.04) | <0.001 | 2.01 (0.82–4.96) | 0.13 | 2.06 (1.16–3.64) | 0.013 |
| NRS | 1.75 (1.24–2.48) | 0.002 | 1.49 (0.61–3.64) | 0.36 | 1.89 (0.88–4.04) | 0.10 |
| Mobility | 1.65 (1.19–2.30) | 0.003 | 2.18 (0.90–5.24) | 0.08 | 2.08 (1.01–4.26) | 0.046 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erne, F.; Mühlberger, L.; Ihle, C.; Ehnert, S.; Histing, T.; Nüssler, A.K.; Maurer, E. The Impact of Cardiovascular Diseases on Postoperative Complications in Orthopedic Trauma Patients. Diagnostics 2025, 15, 1576. https://doi.org/10.3390/diagnostics15131576
Erne F, Mühlberger L, Ihle C, Ehnert S, Histing T, Nüssler AK, Maurer E. The Impact of Cardiovascular Diseases on Postoperative Complications in Orthopedic Trauma Patients. Diagnostics. 2025; 15(13):1576. https://doi.org/10.3390/diagnostics15131576
Chicago/Turabian StyleErne, Felix, Larissa Mühlberger, Christoph Ihle, Sabrina Ehnert, Tina Histing, Andreas K. Nüssler, and Elke Maurer. 2025. "The Impact of Cardiovascular Diseases on Postoperative Complications in Orthopedic Trauma Patients" Diagnostics 15, no. 13: 1576. https://doi.org/10.3390/diagnostics15131576
APA StyleErne, F., Mühlberger, L., Ihle, C., Ehnert, S., Histing, T., Nüssler, A. K., & Maurer, E. (2025). The Impact of Cardiovascular Diseases on Postoperative Complications in Orthopedic Trauma Patients. Diagnostics, 15(13), 1576. https://doi.org/10.3390/diagnostics15131576







