Comparison of Trauma Scoring Systems for Predicting Mortality in Emergency Department Patients with Traffic-Related Multiple Trauma
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
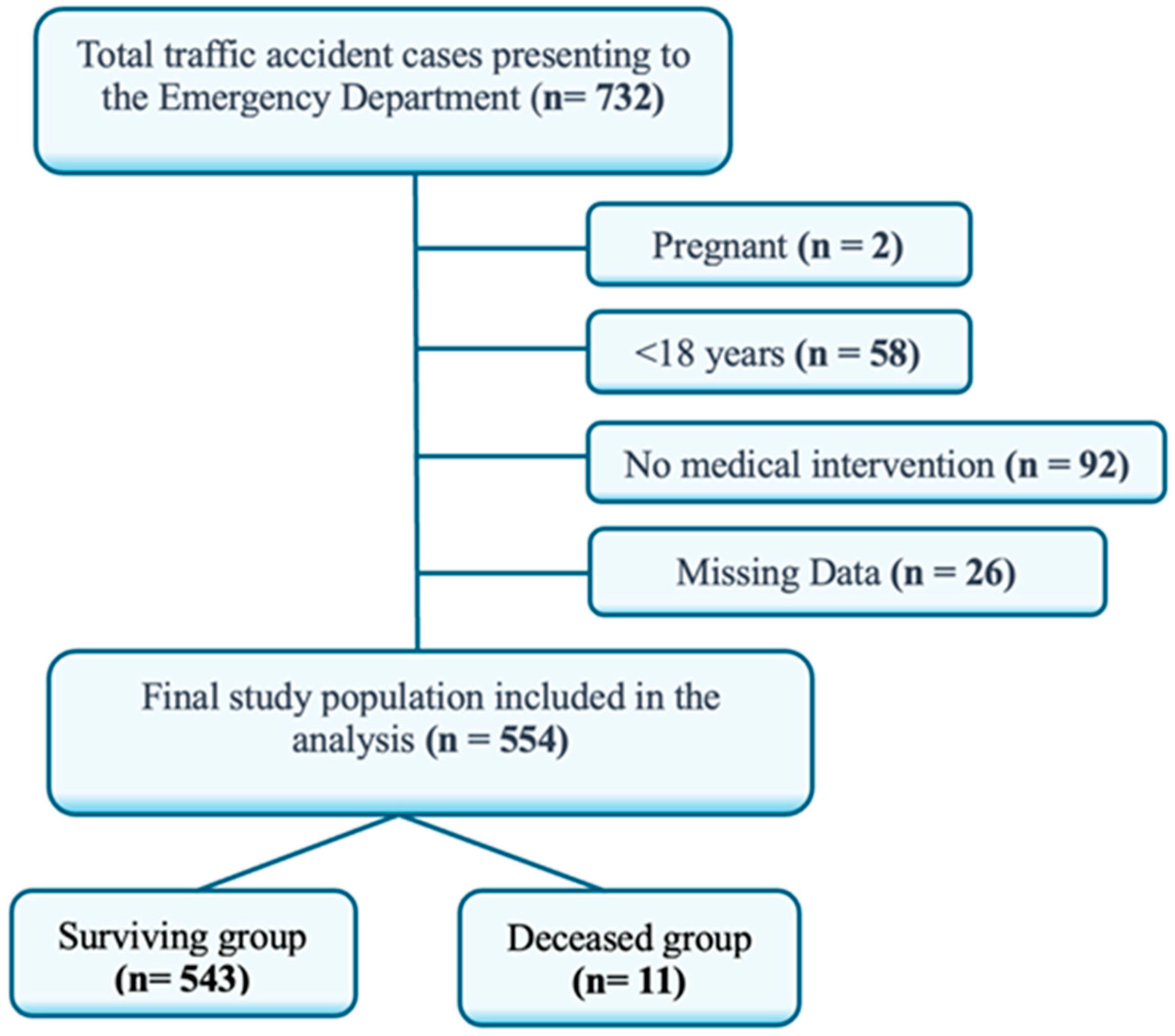
2.2. Participants
2.3. Variables and Data Collection
2.4. Statistical Analysis
3. Results
3.1. Demographics of Patients
3.2. Laboratory Findings and Trauma Scoring Systems
3.3. Correlations Among Trauma Scoring Systems
4. Discussion
4.1. Laboratory Parameters and Trauma Scoring Systems
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RTS | Revised Trauma Score |
| ISS | Injury Severity Score |
| AIS | Abbreviated Injury Score |
| NISS | New Injury Severity Score |
| GCS | Glasgow Coma Scale |
| TRISS | Trauma and Injury Severity Score |
| APACHE II | Acute Physiology and Chronic Health Evaluation II |
| ED | Emergency department |
References
- Turculeţ, C.Ş.; Georgescu, T.F.; Iordache, F.; Ene, D.; Gaşpar, B.; Beuran, M. Polytrauma: The European Paradigm. Chirurgia 2021, 116, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, N.K.; Handolin, L.E.; Heinänen, M.T. Severe Traffic Injuries in the Helsinki Trauma Registry between 2009–2018. Injury 2020, 51, 2946–2952. [Google Scholar] [CrossRef]
- Hakkenbrak, N.A.G.; Harmsen, A.M.K.; Zuidema, W.P.; Reijnders, U.J.L.; Schober, P.; Bloemers, F.W. Classification of trauma-related preventable death; a Delphi procedure in The Netherlands. Injury 2025, 14, 112437. [Google Scholar] [CrossRef]
- Garcia, M.F.; Gomes, R.T.; Pugliesi, E.C.; Santos, J.P.V.D.; Martino, F.; Gomes, K.H.V.; Pasquareli, D.R.G.; Lenza, R.D.M. Comparison between Injury Severity Score (ISS) and New Injury Severity Score (NISS) in predicting mortality of thoracic trauma in a tertiary hospital. Rev. Col. Bras. Cir. 2024, 51, e20243652. [Google Scholar] [CrossRef]
- Kim, J.; Heo, Y.J.; Kim, Y. Comparison of Trauma Mortality Prediction Models with Updated Survival Risk Ratios in Korea. J. Korean Med. Sci. 2025, 40, e51. [Google Scholar] [CrossRef]
- Atik, B.; Kilinc, G.; Yarar, V. Predictive value of prognostic factors at multiple trauma patients in intensive care admission. Bratisl. Lek. Listy 2021, 122, 277–279. [Google Scholar] [CrossRef] [PubMed]
- Yousefi, M.R.; Karajizadeh, M.; Ghasemian, M.; Paydar, S. Comparing NEWS2, TRISS, and RTS in predicting mortality rate in trauma patients based on prehospital data set: A diagnostic study. BMC Emerg. Med. 2024, 24, 163. [Google Scholar] [CrossRef] [PubMed]
- Samuthtai, W.; Patumanond, J.; Samutrtai, P.; Charernboon, T.; Jearwattanakanok, K.; Khorana, J. Clinical Prediction Scoring Scheme for 24 h Mortality in Major Traumatic Adult Patients. Healthcare 2022, 10, 577. [Google Scholar] [CrossRef]
- Ali, S.; Bhatti, T.; Rimsha, S.; Hashmi, R.M.; Khan, S.; Rind, W.; Mussab, R.M. The Predictive Accuracy of the New Trauma Score and the Revised Trauma Score in Predicting the Mortality of Patients Presenting to the Emergency Department of a Tertiary Care Hospital in Karachi. Cureus 2024, 16, e76421. [Google Scholar] [CrossRef]
- Ashrafian Fard, S.; Ahmadi, S.; Ebrahimi Bakhtavar, H.; Sadeghi Bazargani, H.; Rahmani, F. TERMINAL-24 Score in Predicting Early and In-hospital Mortality of Trauma Patients: A Cross-sectional. Arch. Acad. Emerg. Med. 2025, 13, e25. [Google Scholar]
- Global Road Safety Status Report 2018. World Health Organization 2018, Geneva. 2022. Available online: https://www.who.int/violence_injury_prevention/road_safety_status/2018/en/ (accessed on 7 May 2025).
- Kenarangi, T.; Rahmani, F.; Yazdani, A.; Ahmadi, G.D.; Lotfi, M.; Khalaj, T.A. Comparison of GAP, RGAP, and new trauma score (NTS) systems in predicting mortality of traffic accidents that injure hospitals at Mashhad University of Medical Sciences. Heliyon 2024, 10, e36004. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.J.; Huang, X.F.; Xie, F.K.; Zhang, J.; Jiang, X.H.; Yu, A.Y. Road traffic mortality in Zunyi city, China: A 10-year data analysis (2013–2022). Chin. J. Traumatol. 2025, 28, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Kent, T.; Miller, J.; Shreve, C.; Allenback, G.; Wentz, B. Comparison of injuries among motorcycle, moped and bicycle traffic accident victims. Traffic Inj. Prev. 2022, 23, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Serviá, L.; Badia, M.; Montserrat, N.; Trujillano, J. Severity scores in trauma patients admitted to ICU: Physiological and anatomic models. Med. Intensiv. 2019, 43, 26–34.20. [Google Scholar] [CrossRef]
- Höke, M.H.; Usul, E.; Özkan, S. Comparison of Trauma Severity Scores (ISS, NISS, RTS, BIG Score, and TRISS) in Multiple Trauma Patients. J. Trauma. Nurs. 2021, 28, 100–106. [Google Scholar] [CrossRef]
- Wu, S.C.; Chou, S.E.; Liu, H.T.; Hsieh, T.M.; Su, W.T.; Chien, P.C.; Hsieh, C.H. Performance of prognostic scoring systems in trauma patients in the intensive care unit of a trauma center. Int. J. Environ. Res. Public Health 2020, 17, 7226. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Huang, Y.; Zeng, D. Analysis of clinical indicators and survival prediction in trauma patients. Technol. Health Care 2025, 33, 1548–1559. [Google Scholar] [CrossRef]
- Kilinc, M.; Çelik, E.; Demir, I.; Aydemir, S.; Akelma, H. Association of Inflammatory and Metabolic Markers with Mortality in Patients with Postoperative Femur Fractures in the Intensive Care Unit. Medicina 2025, 61, 538. [Google Scholar] [CrossRef]
- Unger, B.; Sarfati, A.; Botrel, T.; Pascal-Moussellard, H.; Raux, M.; James, A.; Marie-Hardy, L. Description and prognostic factors of a cohort of polytraumatized patients with spinal injury in a level I trauma center. Injury 2025, 56, 112319. [Google Scholar] [CrossRef]
- Ivanova, S.; Hilverdink, E.F.; Bastian, J.D.; Jakob, D.A.; Exadaktylos, A.K.; Keel, M.J.B.; Schefold, J.C.; Anwander, H.; Lustenberger, T. Short- and Long-Term Mortality in Severely Injured Older Trauma Patients: A Retrospective Analysis. J. Clin. Med. 2025, 14, 2064. [Google Scholar] [CrossRef]
- Gupta, J.; Kshirsagar, S.; Naik, S.; Pande, A. Comparative evaluation of mortality predictors in trauma patients: A prospective single-center observational study assessing Injury Severity Score, Revised Trauma Score, Trauma and Injury Severity Score, and Acute Physiology and Chronic Health Evaluation II scores. Indian J. Crit. Care Med. 2024, 28, 475–482. [Google Scholar] [PubMed]
- Javali, R.H.; Krishnamoorthy, K.; Patil, A.; Srinivasarangan, M.; Suraj, S.; Sriharsha, S. Comparison of Injury Severity Score, New Injury Severity Score, Revised Trauma Score and Trauma and Injury Severity Score for mortality prediction in elderly trauma patients. Indian J. Crit. Care Med. 2019, 23, 73–77. [Google Scholar] [PubMed]
- Galvagno, S.M., Jr.; Massey, M.; Bouzat, P.; Vesselinov, R.; Levy, M.J.; Millin, M.G.; Stein, D.M.; Scalea, T.M.; Hirshon, J.M. Correlation between the Revised Trauma Score and Injury Severity Score: Implications for prehospital trauma triage. Prehosp. Emerg. Care 2019, 23, 263–270. [Google Scholar] [CrossRef] [PubMed]

| Demographic Characteristics | ||
| Age (Median (IQR 25–75)) | 36 (25–54) | |
| Gender n (%) | Male n (%) | 374 (67.5%) |
| Female n (%) | 180 (32.5%) | |
| Number of Comorbidities n (%) | No | 509 (91.9%) |
| 1 | 25 (4.5%) | |
| 2 or more | 20 (3.6%) | |
| Trauma Characteristics | ||
| 244 (44%) | |
| 167 (29.9%) | |
| 97 (16.6%) | |
| 342 (61.7%) | |
| Laboratory Parameter | Deceased Group Median (IQR 25–75) | Surviving Group Median (IQR 25–75) | p-Value |
|---|---|---|---|
| WBC | 15 × 103 (12 × 103–18 × 103) | 10 × 103 (8 × 103–12 × 103) | <0.05 |
| Hematocrit (%) | 30 (25–35) | 40 (35–45) | <0.05 |
| Bicarbonate (mEq/L) | 18 (15–20) | 22 (20–24) | <0.05 |
| Sodium (mEq/L) | 140 (138–142) | 141 (139–143) | 0.15 |
| Potassium (mEq/L) | 4.5 (4.0–5.0) | 4.4 (4.2–4.6) | 0.20 |
| Scoring System | Surviving Group Median (IQR 25–75) | Deceased Group Median (IQR 25–75) | p * |
|---|---|---|---|
| APACHE II | 5 (4–8) | 20 (14.5–25) | <0.001 |
| AIS | 1 (1–2) | 2 (2–3.5) | <0.001 |
| ISS | 2 (1–4) | 12 (7.5–15.5) | <0.001 |
| NISS | 2 (1–6) | 12 (12–22) | <0.001 |
| RTS | 7.84 (7.84–7.84) | 4.09 (3.46–6.64) | <0.001 |
| GCS | 15 (15–15) | 4 (3–11) | <0.001 |
| TRISS | 0.997 (0.986–0.997) | 0.773 (0.451–0.918) | <0.001 |
| Scoring System | RTS | AIS | APACHE II | ISS | NISS | GCS | TRISS |
|---|---|---|---|---|---|---|---|
| RTS | — | Rho: −0.324 | Rho: −0.313 | Rho:−0.321 | Rho: −0.309 | Rho: 0.119 | Rho: −0.283 |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p = 0.007 | p < 0.001 | ||
| AIS | — | Rho: 0.268 | Rho: 0.884 | Rho: 0.877 | Rho: −0.437 | Rho: −0.675 | |
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |||
| APACHE II | — | Rho: 0.243 | Rho: 0.234 | Rho: −0.362 | Rho: −0.524 | ||
| p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | ||||
| ISS | — | Rho: 0.971 | Rho: −0.430 | Rho: −0.741 | |||
| p < 0.001 | p < 0.001 | p < 0.001 | |||||
| NISS | — | Rho: −0.422 | Rho: −0.716 | ||||
| p < 0.001 | p < 0.001 | ||||||
| GCS | — | Rho: −0.395 | |||||
| p < 0.001 | |||||||
| TRISS | — |
| Scoring System | Cutoff Points | Sensitivity 95% CI | Specificity 95% CI | PLR 95% CI | NLR 95% CI | AUC 95% CI | p |
|---|---|---|---|---|---|---|---|
| APACHE II | ≥10.5 | 1 (0.72–1) | 0.89 (0.86–0.91) | 8.9 (7.0–11.3) | 0 | 0.97 (0.95–0.99) | 0.0001 |
| RTS | <7.01 | 0.82 (0.48–0.98) | 0.98 (0.96–0.99) | 34.17 (18.6–62.6) | 0.19 (0.05–0.67) | 0.90 (0.77–0.96) | 0.0001 |
| AIS | ≥1.50 | 0.91 (0.59–0.99) | 0.66 (0.62–0.70) | 2.65 (2.13–3.3) | 0.14 (0.02–0.91) | 0.86 (0.79–0.93) | 0.0001 |
| NISS | ≥8.50 | 0.90 (0.58–0.99) | 0.81 (0.77–0.84) | 4.79 (3.71–6.18) | 0.11 (0.02–0.71) | 0.92 (0.88–0.96) | 0.0001 |
| ISS | ≥4.50 | 0.82 (0.48–0.98) | 0.74 (0.70–0.78) | 3.22 (2.35–4.41) | 0.24 (0.07–0.84) | 0.91 (0.86–0.96) | 0.0001 |
| GCS | <9.50 | 0.73 (0.39–0.94) | 0.99 (0.97–0.99) | 66.18 (27.6–99.6) | 0.28 (0.11–0.73) | 0.98 (0.96–0.99) | 0.0001 |
| TRISS | <0.972 | 1 (0.71–1) | 0.90 (0.58–0.99) | 17.55 (12.5–24.7) | 0 | 0.98 (0.97–0.99) | 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaya, M.; Yildirim, H.; Toprak, M.; Ulu, M. Comparison of Trauma Scoring Systems for Predicting Mortality in Emergency Department Patients with Traffic-Related Multiple Trauma. Diagnostics 2025, 15, 1563. https://doi.org/10.3390/diagnostics15121563
Kaya M, Yildirim H, Toprak M, Ulu M. Comparison of Trauma Scoring Systems for Predicting Mortality in Emergency Department Patients with Traffic-Related Multiple Trauma. Diagnostics. 2025; 15(12):1563. https://doi.org/10.3390/diagnostics15121563
Chicago/Turabian StyleKaya, Murtaza, Harun Yildirim, Mehmet Toprak, and Mehmed Ulu. 2025. "Comparison of Trauma Scoring Systems for Predicting Mortality in Emergency Department Patients with Traffic-Related Multiple Trauma" Diagnostics 15, no. 12: 1563. https://doi.org/10.3390/diagnostics15121563
APA StyleKaya, M., Yildirim, H., Toprak, M., & Ulu, M. (2025). Comparison of Trauma Scoring Systems for Predicting Mortality in Emergency Department Patients with Traffic-Related Multiple Trauma. Diagnostics, 15(12), 1563. https://doi.org/10.3390/diagnostics15121563






