Short-Term Outcomes of First Metatarsophalangeal Arthroplasty Using the Silktoe Double-Stemmed Silicone Implant
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
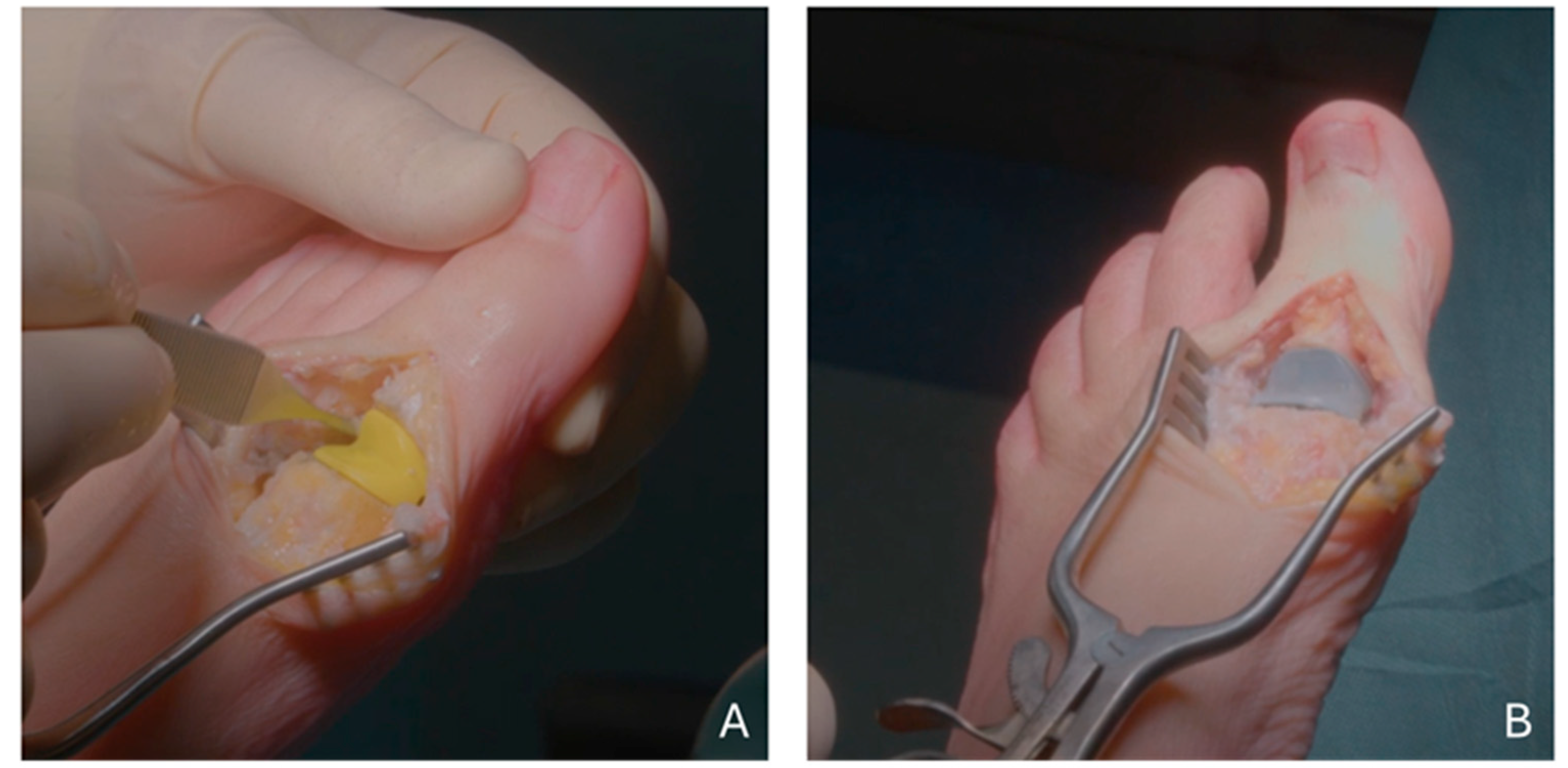
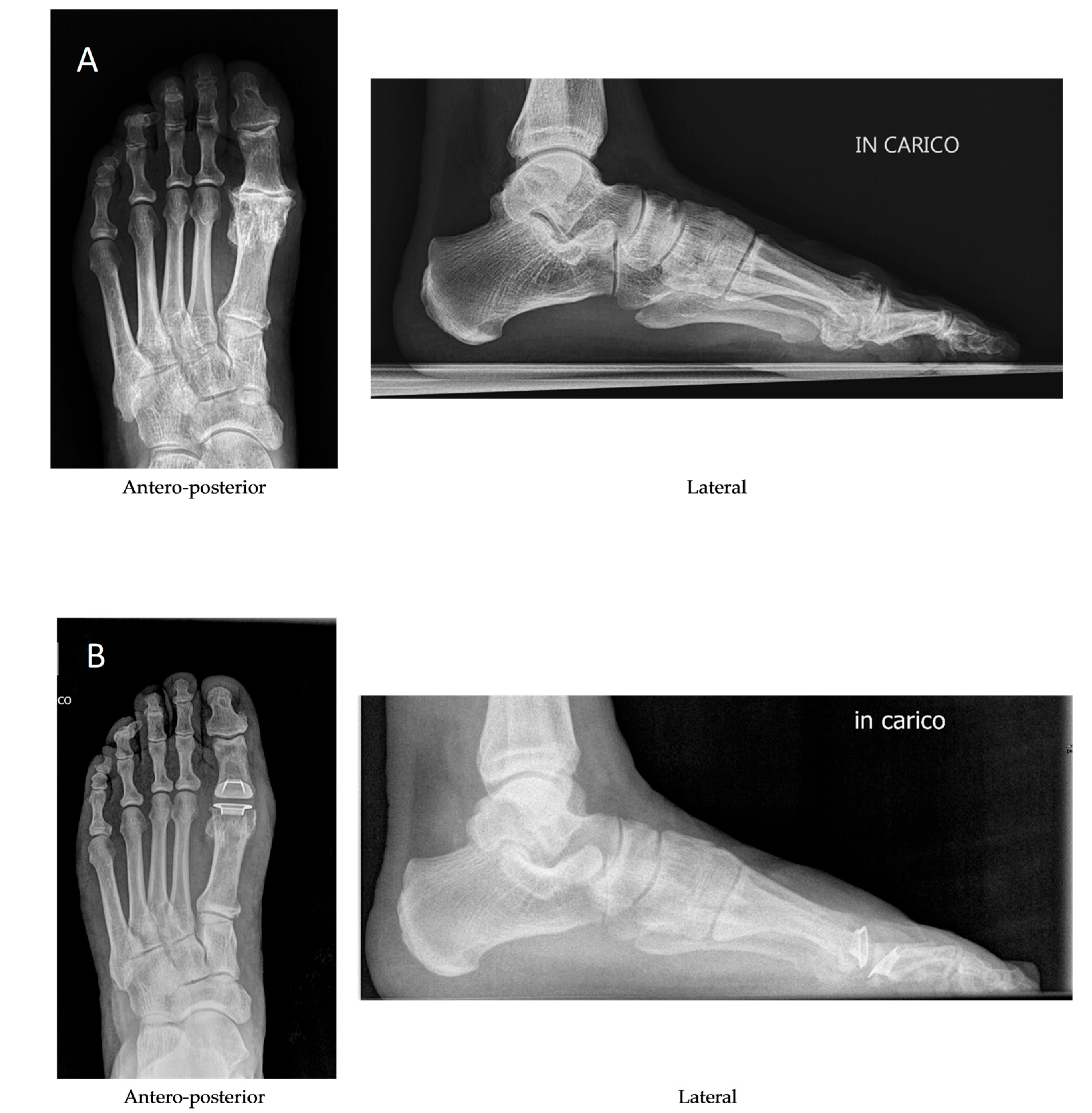
2.2. Operative Technique, Postoperative Care and Follow-Up
2.3. Data Analysis
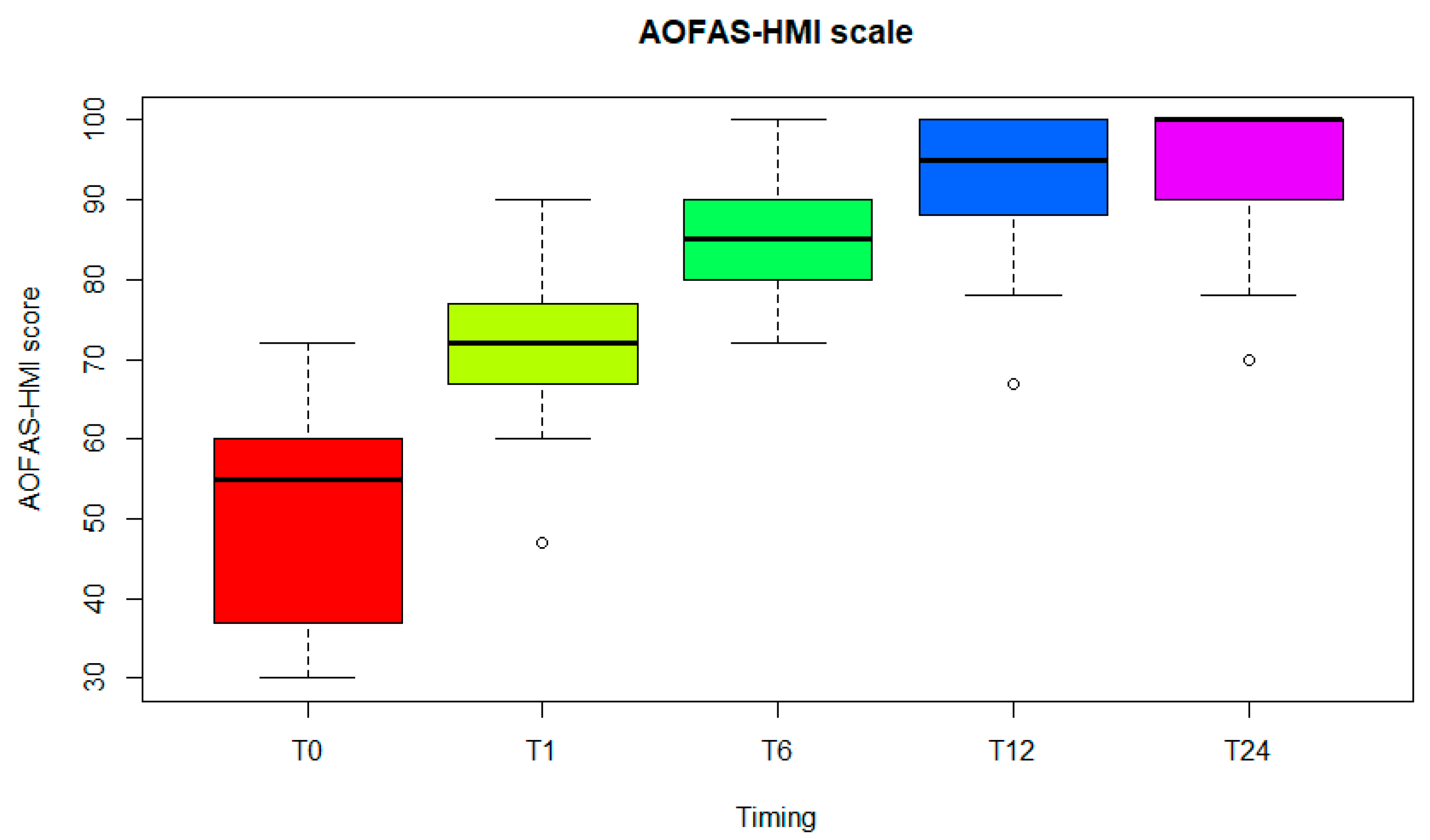
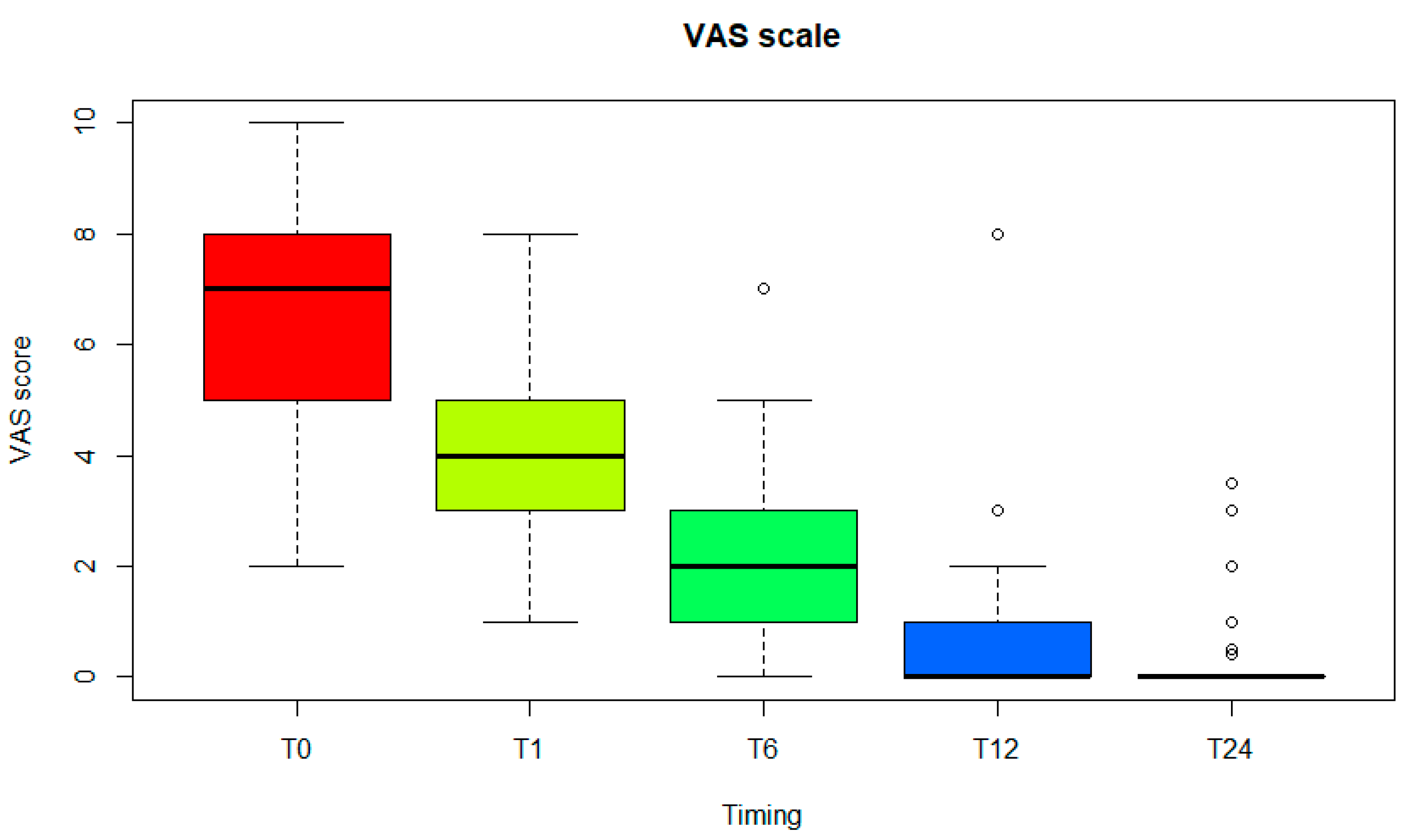
3. Results
4. Discussion
- -
- The use of grommets in most feet prevented abrasive friction and damage to the double-stemmed silicone component [28];
- -
- -
- -
- The sagittal angulation of the metatarsal and phalangeal stems reproduces the alignment of the toe in a neutral position and therefore maintains natural muscle and tendon tensions at rest and while walking.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MTP1 | first metatarsophalangeal |
| PVA | polyvinyl alcohol |
| AOFAS-HMI | American Orthopaedic Foot and Ankle Society-Hallux Metatarsophalangeal-Interphalangeal Scale |
| VAS | Visual Analogue Scale |
References
- Joyce, T.J. Implants for the first metatarsophalangeal joint and prospective considerations. Expert. Rev. Med. Devices 2005, 2, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, M.L.; Ugrinich, M. First Metatarsophalangeal Joint Implant Options. Clin. Podiatr. Med. Surg. 2019, 36, 577–596. [Google Scholar] [CrossRef] [PubMed]
- Majeed, H. Silastic replacement of the first metatarsophalangeal joint: Historical evolution, modern concepts and a systematic review of the literature. EFORT Open Rev. 2019, 4, 77–84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Perler, A.D.; Nwosu, V.; Christie, D.; Higgins, K. End-stage osteoarthritis of the great toe/hallux rigidus: A review of the alternatives to arthrodesis: Implant versus osteotomies and arthroplasty techniques. Clin. Podiatr. Med. Surg. 2013, 30, 351–395. [Google Scholar] [CrossRef] [PubMed]
- Yee, G.; Lau, J. Current concepts review: Hallux rigidus. Foot Ankle Int. 2008, 29, 637–646. [Google Scholar] [CrossRef]
- Sullivan, M.R. Hallux rigidus: MTP implant arthroplasty. Foot Ankle Clin. 2009, 14, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Brewster, M. Does total joint replacement or arthrodesis of the first metatarsophalangeal joint yield better functional results? A systematic review of the literature. J. Foot Ankle Surg. 2010, 49, 546–552. [Google Scholar] [CrossRef]
- Ter Keurs, E.W.; Wassink, S.; Burger, B.J.; Hubach, P.C. First metatarsophalangeal joint replacement: Long-term results of a double stemmed flexible silicone prosthesis. Foot Ankle Surg. 2011, 17, 224–227. [Google Scholar] [CrossRef]
- Raikin, S.M.; Ahmad, J.; Pour, A.E.; Abidi, N. Comparison of arthrodesis and metallic hemiarthroplasty of the hallux metatarsophalangeal joint. J. Bone Jt. Surg. Am. 2007, 89, 1979–1985. [Google Scholar] [CrossRef]
- Gibson, J.N.; Thomson, C.E. Arthrodesis or total replacement arthroplasty for hallux rigidus: A randomized controlled trial. Foot Ankle Int. 2005, 26, 680–690. [Google Scholar] [CrossRef]
- Garras, D.N.; Durinka, J.B.; Bercik, M.; Miller, A.G.; Raikin, S.M. Conversion arthrodesis for failed first metatarsophalangeal joint hemiarthroplasty. Foot Ankle Int. 2013, 34, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- McNeil, D.S.; Baumhauer, J.F.; Glazebrook, M.A. Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int. 2013, 34, 15–32. [Google Scholar] [CrossRef] [PubMed]
- Brage, M.E.; Ball, S.T. Surgical options for salvage of end-stage hallux rigidus. Foot Ankle Clin. 2002, 7, 49–73. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Guzmán, J.; Gallo Oropeza, R.; Reyes Donado, M.; Martin Oliva, X.; Díaz Sánchez, T. Arthrodesis vs arthroplasty for moderate and severe Hallux rigidus: Systematic review. Foot Ankle Surg. 2024, 30, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Bhimani, R.; Labib, S.A. Metatarsophalangeal Arthroplasty in Hallux Rigidus. Foot Ankle Clin. 2024, 29, 495–505. [Google Scholar] [CrossRef]
- Gross, C.E.; Hsu, A.R.; Lin, J.; Holmes, G.B.; Lee, S. Revision MTP arthrodesis for failed MTP arthroplasty. Foot Ankle Spec. 2013, 6, 471–478. [Google Scholar] [CrossRef]
- Colò, G.; Fusini, F.; Alessio-Mazzola, M.; Samaila, E.M.; Formica, M.; Magnan, B. Interposition arthroplasty with bovine collagenous membrane for hallux rigidus: A long-term results retrospective study. Foot Ankle Surg. 2022, 28, 1473–1478. [Google Scholar] [CrossRef]
- Cook, E.; Cook, J.; Rosenblum, B.; Landsman, A.; Giurini, J.; Basile, P. Meta-analysis of first metatarsophalangeal joint implant arthroplasty. J. Foot Ankle Surg. 2009, 48, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Fieschi, S.; Saffarini, M.; Manzi, L.; Fieschi, A. Mid-term outcomes of first metatarsophalangeal arthroplasty using the Primus FGT double-stemmed silicone implants. Foot Ankle Surg. 2017, 23, 142–147. [Google Scholar] [CrossRef]
- Santandrea, A.; Mercurio, D.; Giardini, P.; Cortese, F. Protesi metatarso-falangee. Lo Scalpello-Otodi Educ. 2019, 33, 155–160. [Google Scholar] [CrossRef]
- Fletcher, W.R.; Collins, T.; Fox, A.; Pillai, A. Mid-term efficacy of the Cartiva synthetic cartilage implant in symptomatic hallux rigidus. Bone Jt. Open 2024, 5, 799–805. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Swanson, A.B. Implant arthroplasty for the great toe. Clin. Orthop. Relat. Res. 1972, 85, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Esway, J.E.; Conti, S.F. Joint replacement in the hallux metatarsophalangeal joint. Foot Ankle Clin. 2005, 10, 97–115. [Google Scholar] [CrossRef] [PubMed]
- ISO 14949: 2001; Implants for Surgery—Two-Part Addition-Cure Silicone Elastomers. ISO: Geneva, Switzerland, 2001.
- EN ISO 5832-3:2021; Implants for Surgery—Metallic Materials—Part 3: Wrought Titanium 6-Aluminium 4-Vanadium Alloy. ISO: Geneva, Switzerland, 2021.
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Scott, J.; Huskisson, E.C. Graphic representation of pain. Pain 1976, 2, 175–184. [Google Scholar] [CrossRef]
- van Duijvenbode, D.C.; Bulstra, G.H.; Nijsse, B.A. Nineteen-year follow-up of the silastic double stemmed hinge prosthesis of the first metatarsophalangeal joint. Foot Ankle Surg. 2013, 19, 27–30. [Google Scholar] [CrossRef]
- Morgan, S.; Ng, A.; Clough, T. The long-term outcome of silastic implant arthroplasty of the first metatarsophalangeal joint: A retrospective analysis of one hundred and eight feet. Int. Orthop. 2012, 36, 1865–1869. [Google Scholar] [CrossRef]
- Sung, W.; Weil, L., Jr.; Weil Sr, L.S.; Stark, T. Total first metatarsophalangeal joint implant arthroplasty: A 30-year retrospective. Clin. Podiatr. Med. Surg. 2011, 28, 755–761. [Google Scholar] [CrossRef]
- Lawrence, B.R.; Thuen, E. A retrospective review of the primus first MTP joint double-stemmed silicone implant. Foot Ankle Spec. 2013, 6, 94–100. [Google Scholar] [CrossRef]
- Sethi, M.; Limaye, N.; Alderton, E.; Limaye, R.; Kulkarni, A. Silastic Joint Arthroplasty as a Joint-Preserving Alternative for End-Stage Hallux Rigidus: Outcomes From 112 First Metatarsophalangeal Joint Arthroplasties. Cureus 2023, 15, e46561. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sorbie, C.; Saunders, G.A. Hemiarthroplasty in the treatment of hallux rigidus. Foot Ankle Int. 2008, 29, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Wetke, E.; Zerahn, B.; Kofoed, H. Prospective analysis of a first MTP total joint replacement. Evaluation by bone mineral densitometry, pedobarography, and visual analogue score for pain. Foot Ankle Surg. 2012, 18, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Papalia, R.; Palumbo, A.; Del Buono, A.; Denaro, V. Quantitative review of operative management of hallux rigidus. Br. Med. Bull. 2011, 98, 75–98. [Google Scholar] [CrossRef][Green Version]
- Deheer, P.A. The case against first metatarsal phalangeal joint implant arthroplasty. Clin. Podiatr. Med. Surg. 2006, 23, 709–723. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Jung, J.H.; Kang, S.H.; Choi, G.W.; Kim, H.J. Implant Arthroplasty versus Arthrodesis for the Treatment of Advanced Hallux Rigidus: A Meta-analysis of Comparative Studies. J. Foot Ankle Surg. 2019, 58, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Arbuthnot, J.E.; Cheung, G.; Balain, B.; Denehey, T.; Higgins, G.; Trevett, M.C. Replacement arthroplasty of the first metatarsophalangeal joint using a ceramic-coated endoprosthesis for the treatment of hallux rigidus. J. Foot Ankle Surg. 2008, 47, 500–504. [Google Scholar] [CrossRef]
- Daniilidis, K.; Martinelli, N.; Marinozzi, A.; Denaro, V.; Gosheger, G.; Pejman, Z.; Buchhorn, T. Recreational sport activity after total replacement of the first metatarsophalangeal joint: A prospective study. Int. Orthop. 2010, 34, 973–979. [Google Scholar] [CrossRef]
- Coutts, A.; Kilmartin, T.E.; Ellis, M.J. The long-term patient focused outcomes of the Keller’s arthroplasty for the treatment of hallux rigidus. Foot 2012, 22, 167–171. [Google Scholar] [CrossRef]
- Erkocak, O.F.; Senaran, H.; Altan, E.; Aydin, B.K.; Acar, M.A. Short-term functional outcomes of first metatarsophalangeal total joint replacement for hallux rigidus. Foot Ankle Int. 2013, 34, 1569–1579. [Google Scholar] [CrossRef]
- Kline, A.J.; Hasselman, C.T. Metatarsal head resurfacing for advanced hallux rigidus. Foot Ankle Int. 2013, 34, 716–725. [Google Scholar] [CrossRef]
| MTP1 Arthroplasty n = 37 | |
|---|---|
| Age | 59.8 ± 10.2 (30–81) |
| Women | 23 (62.1%) |
| Indications | |
| Hallux rigidus | 30 (81.1%) |
| Hallux rigidus plus valgus | 4 (10.8%) |
| Painful or unstable joint following previous surgery | 2 (5.4%) |
| Hallux rigidus due to gout | 1 (2.7%) |
| Mean ± SD | Median | Range | |
|---|---|---|---|
| Pain | 37.3 ± 5.6 | 40 | 20–40 |
| Function | |||
| Activity limitation | 9.9 ± 0.5 | 10 | 7–10 |
| Footwear requirements | 9.5 ± 1.6 | 10 | 5–10 |
| MPT joint motion | 8.7 ± 2.3 | 10 | 5–10 |
| IP joint motion | 5 ± 0.0 | 5 | 5–5 |
| MPT-IP stability in all directions | 5 ± 0.0 | 5 | 5–5 |
| Callus related to hallux MPT-IP | 5 ± 0.0 | 5 | 5–5 |
| Alignment | 14.2 ± 2.2 | 15 | 8–15 |
| Total | 94.6 ± 7.6 | 100 | 70–100 |
| Reference | Year | Follow-Up Period (Years) | Number of Arthroplasties Performed | Silicone Spacer Model | AOFAS-HMI a (Mean Score) | Survival a (%) | VAS a (Score) |
|---|---|---|---|---|---|---|---|
| This study | 2025 | 2.0 | 37 | Silktoe | 94.6 | 100 | 0.4 |
| [8] | 2010 | 9.0 | 59 | Swanson | 83.0 | 85.9 | n.a. |
| [19] | 2015 | 5.0 | 70 | Primus | 88.9 | 100 | n.a. |
| [20] | 2019 | 2.0 | 41 | Primus | 89.0 | n.a. | 0.8 |
| [28] | 2012 | 19.0 | 42 | Swanson | n.a. | 97.2 | n.a. |
| [29] | 2012 | 8.5 | 108 | n.a. | 77.5 | 97.1 | 2.3 b |
| [30] | 2011 | 7.2 | 92 | n.a. | 82.4 | 95.2 | n.a. |
| [31] | 2013 | 5.5 | 70 | Primus | 87.4 | 94.9 | 2.5 b |
| [32] | 2023 | 4.0 | 112 | Swanson | n.a | 99.1 | 1.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fieschi, S.; Redaelli, C.; Fazzini, A. Short-Term Outcomes of First Metatarsophalangeal Arthroplasty Using the Silktoe Double-Stemmed Silicone Implant. Diagnostics 2025, 15, 1349. https://doi.org/10.3390/diagnostics15111349
Fieschi S, Redaelli C, Fazzini A. Short-Term Outcomes of First Metatarsophalangeal Arthroplasty Using the Silktoe Double-Stemmed Silicone Implant. Diagnostics. 2025; 15(11):1349. https://doi.org/10.3390/diagnostics15111349
Chicago/Turabian StyleFieschi, Stefano, Costanza Redaelli, and Anita Fazzini. 2025. "Short-Term Outcomes of First Metatarsophalangeal Arthroplasty Using the Silktoe Double-Stemmed Silicone Implant" Diagnostics 15, no. 11: 1349. https://doi.org/10.3390/diagnostics15111349
APA StyleFieschi, S., Redaelli, C., & Fazzini, A. (2025). Short-Term Outcomes of First Metatarsophalangeal Arthroplasty Using the Silktoe Double-Stemmed Silicone Implant. Diagnostics, 15(11), 1349. https://doi.org/10.3390/diagnostics15111349





