Validity and Reliability of an Artificial Intelligence-Based Posture Estimation Software for Measuring Cervical and Lower-Limb Alignment Versus Radiographic Imaging
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
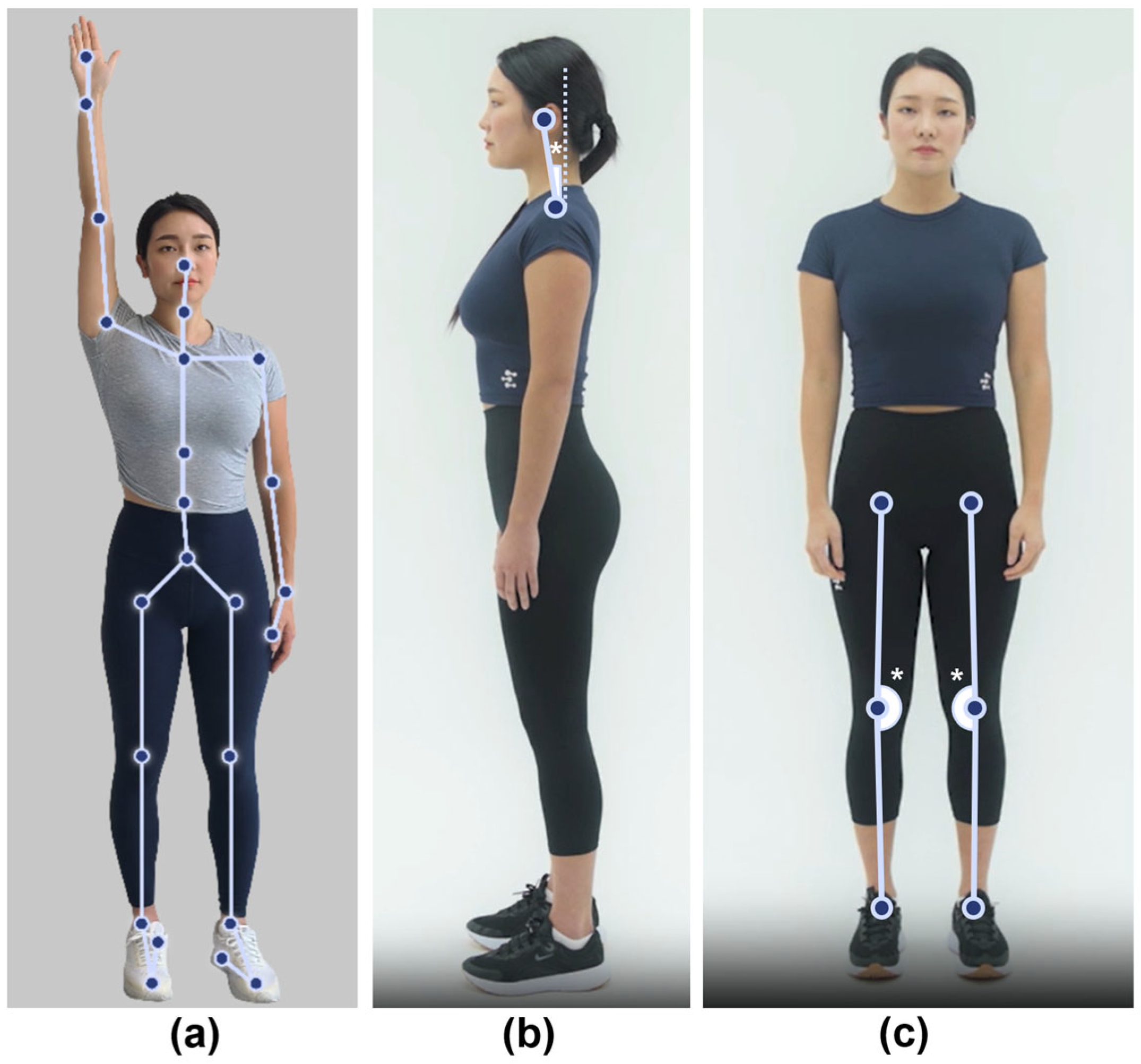
2.2. Body Alignment Assessment Using an AI-Based Posture Estimation Software
2.3. Radiographic Measurements
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Alignment Measurements
3.3. Correlation Between MORA Vu and Radiographic Measurements
3.4. Interrater Reliability of AI-Based Posture Estimation Software Measurements
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
Abbreviations
| AI | artificial intelligence |
| CVA | craniovertebral angle |
| DHKA | digital hip–knee–ankle |
| FHP | forward head posture |
| ICC | intraclass correlation coefficient |
| MSDs | musculoskeletal disorders |
| OA | osteoarthritis |
| RHKA | radiographic hip–knee–ankle |
| SVA | sagittal vertical axis |
References
- Woolf, A.D.; Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 2003, 81, 646–656. [Google Scholar]
- Osborne, R.H.; Nikpour, M.; Busija, L.; Sundararajan, V.; Wicks, I.P. Prevalence and cost of musculoskeletal disorders: A population-based, public hospital system healthcare consumption approach. J. Rheumatol. 2007, 34, 2466–2475. [Google Scholar]
- Palazzo, C.; Ravaud, J.-F.; Papelard, A.; Ravaud, P.; Poiraudeau, S. The burden of musculoskeletal conditions. PLoS ONE 2014, 9, e90633. [Google Scholar] [CrossRef]
- Woolf, A.D.; Erwin, J.; March, L. The need to address the burden of musculoskeletal conditions. Best Pract. Res. Clin. Rheumatol. 2012, 26, 183–224. [Google Scholar] [CrossRef]
- Ferreira, E.A.G.; Duarte, M.; Maldonado, E.P.; Burke, T.N.; Marques, A.P. Postural assessment software (PAS/SAPO): Validation and reliabiliy. Clinics 2010, 65, 675–681. [Google Scholar] [CrossRef]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-dimensional digital photography for child body posture evaluation: Standardized technique, reliable parameters and normative data for age 7–10 years. Scoliosis Spinal Disord. 2017, 12, 38. [Google Scholar] [CrossRef]
- Talapatra, S.; Parvez, M.S.; Saha, P.; Kibria, M.G. Assessing the impact of critical risk factors on the development of musculoskeletal disorders: A structural equation modelling approach. Theor. Issues Ergon. Sci. 2024, 25, 343–368. [Google Scholar] [CrossRef]
- Hopkins, B.B.; Vehrs, P.R.; Fellingham, G.W.; George, J.D.; Hager, R.; Ridge, S.T. Validity and reliability of standing posture measurements using a mobile application. J. Manip. Physiol. Ther. 2019, 42, 132–140. [Google Scholar] [CrossRef]
- Hida, M.; Wada, C.; Imai, R.; Kitagawa, K.; Okamatsu, S.; Ohnishi, T.; Kawashima, S. Spinal postural alignment measurements using markerless digital photography. J. Orthop. Surg. 2020, 28, 2309499020960834. [Google Scholar] [CrossRef]
- De Carvalho, D.E.; Soave, D.; Ross, K.; Callaghan, J.P. Lumbar spine and pelvic posture between standing and sitting: A radiologic investigation including reliability and repeatability of the lumbar lordosis measure. J. Manip. Physiol. Ther. 2010, 33, 48–55. [Google Scholar] [CrossRef]
- Lebl, D.R.; Bono, C.M. Update on the diagnosis and management of cervical spondylotic myelopathy. J. Am. Acad. Orthop. Surg. 2015, 23, 648–660. [Google Scholar] [CrossRef]
- Cohen, L.; Kobayashi, S.; Simic, M.; Dennis, S.; Refshauge, K.; Pappas, E. Non-radiographic methods of measuring global sagittal balance: A systematic review. Scoliosis Spinal Disord. 2017, 12, 30. [Google Scholar] [CrossRef]
- Porto, A.B.; Okazaki, V.H. Thoracic kyphosis and lumbar lordosis assessment by radiography and photogrammetry: A review of normative values and reliability. J. Manip. Physiol. Ther. 2018, 41, 712–723. [Google Scholar] [CrossRef]
- Gadotti, I.C.; Armijo-Olivo, S.; Silveira, A.; Magee, D. Reliability of the craniocervical posture assessment: Visual and angular measurements using photographs and radiographs. J. Manip. Physiol. Ther. 2013, 36, 619–625. [Google Scholar] [CrossRef]
- Ferreira, E.A.; Duarte, M.; Maldonado, E.P.; Bersanetti, A.A.; Marques, A.P. Quantitative assessment of postural alignment in young adults based on photographs of anterior, posterior, and lateral views. J. Manip. Physiol. Ther. 2011, 34, 371–380. [Google Scholar] [CrossRef]
- Furlanetto, T.S.; Candotti, C.T.; Sedrez, J.A.; Noll, M.; Loss, J.F. Evaluation of the precision and accuracy of the DIPA software postural assessment protocol. Eur. J. Physiother. 2017, 19, 179–184. [Google Scholar] [CrossRef]
- Kawasaki, T.; Ohji, S.; Aizawa, J.; Sakai, T.; Hirohata, K.; Kuruma, H.; Koseki, H.; Okawa, A.; Jinno, T. Correlation between the photographic cranial angles and radiographic cervical spine alignment. Int. J. Environ. Res. Public Health 2022, 19, 6278. [Google Scholar] [CrossRef]
- Moon, Y.J.; Ahn, T.Y.; Suh, S.W.; Park, K.-B.; Chang, S.Y.; Yoon, D.-K.; Kim, M.-S.; Kim, H.; Jeon, Y.D.; Yang, J.H. A preliminary diagnostic model for forward head posture among adolescents using forward neck tilt angle and radiographic sagittal alignment parameters. Diagnostics 2024, 14, 394. [Google Scholar] [CrossRef]
- Martini, M.L.; Neifert, S.N.; Chapman, E.K.; Mroz, T.E.; Rasouli, J.J. Cervical spine alignment in the sagittal axis: A review of the best validated measures in clinical practice. Glob. Spine J. 2021, 11, 1307–1312. [Google Scholar] [CrossRef]
- Lee, S.H.; Hyun, S.-J.; Jain, A. Cervical sagittal alignment: Literature review and future directions. Neurospine 2020, 17, 478. [Google Scholar] [CrossRef]
- Lee, H.J.; You, S.T.; Sung, J.H.; Kim, I.S.; Hong, J.T. Analyzing the significance of T1 slope minus cervical lordosis in patients with anterior cervical discectomy and fusion surgery. J. Korean Neurosurg. Soc. 2021, 64, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420. [Google Scholar] [CrossRef] [PubMed]
- Childs, J.D.; Cleland, J.A.; Elliott, J.M.; Teyhen, D.S.; Wainner, R.S.; Whitman, J.M.; Sopky, B.J.; Godges, J.J.; Flynn, T.W. American Physical Therapy Association. Neck pain: Clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2008, 38, A1–A34. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.H.T.; Chiu, T.T.W.; Poon, A.T.K. The relationship between head posture and severity and disability of patients with neck pain. Man. Ther. 2008, 13, 148–154. [Google Scholar] [CrossRef]
- Subbarayalu, A.V. Measurement of craniovertebral angle by the modified head posture spinal curvature instrument: A reliability and validity study. Physiother. Theory Pract. 2016, 32, 144–152. [Google Scholar] [CrossRef]
- Bagheri, I.; Alizadeh, S.; Irankhah, E. Design and Implementation of Wireless IMU-based Posture Correcting Biofeedback System. In Proceedings of the Conference on Mechanical, Electrical and Computer Engineering, Istanbul, Turkey, 13 May 2020. [Google Scholar]
- Lee, S.-H.; Kim, K.-T.; Seo, E.-M.; Suk, K.-S.; Kwack, Y.-H.; Son, E.-S. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. Clin. Spine Surg. 2012, 25, E41–E47. [Google Scholar] [CrossRef]
- Saiki, Y.; Kabata, T.; Ojima, T.; Kajino, Y.; Inoue, D.; Ohmori, T.; Yoshitani, J.; Ueno, T.; Yamamuro, Y.; Taninaka, A. Reliability and validity of OpenPose for measuring hip–knee–ankle angle in patients with knee osteoarthritis. Sci. Rep. 2023, 13, 3297. [Google Scholar] [CrossRef]
- Clément, J.; Blakeney, W.; Hagemeister, N.; Desmeules, F.; Mezghani, N.; Lowry, V.; Vendittoli, P.-A. Hip–knee–ankle (HKA) angle modification during gait in healthy subjects. Gait Posture 2019, 72, 62–68. [Google Scholar] [CrossRef]


| Parameter | Description |
|---|---|
| Cervical tilt | The angle between the vertical line from the center of the T1 upper endplate (T1UEP) and the line from the center of T1UEP to the tip of the dens |
| Cranial tilt | The angle between the line from the center of the T1UEP to the dens and the sagittal vertical axis from the T1UEP |
| C7 slope | The angle between the C7 upper endplate line and the horizontal plane |
| T1 slope | The angle between the T1UEP line and the horizontal plane |
| C2–7 Cobb angle | The angle formed by the intersection of perpendicular lines from the lines parallel to the lower endplates of C2 and C7 |
| Craniovertebral angle | The angle between the horizontal line and the line from the distal tip of the C7 spinous process to the external auditory canal |
| C2–7 sagittal vertical axis | The distance between the plumb line from the center of C2 and the posterosuperior corner of the C7 vertebral body |
| Parameter | Evaluator A | Evaluator B | Evaluator C | Overall |
|---|---|---|---|---|
| FHP angles (°) | 15.1 ± 4.3 | 15.1 ± 3.6 | 15.1 ± 4.3 | 15.1 ± 4.1 |
| DHKA angles (°) | 177.3 ± 2.9 | 177.2 ± 3.0 | 177.4 ± 3.0 | 177.3 ± 2.9 |
| Parameter | Values |
|---|---|
| Cervical tilt (°) | 16.7 ± 5.7 |
| Cranial tilt (°) | 7.7 ± 4.8 |
| T1 slope (°) | 23.2 ± 6.8 |
| C7 slope (°) | 20.9 ± 7.4 |
| C2–7 Cobb angle (°) | 11.9 ± 9.7 |
| CVA (°) | 63.7 ± 5.4 |
| C2–7 SVA (cm) | 2.1 ± 1.0 |
| RHKA angle (°) | 178.2 ± 2.5 |
| Comparison | Correlation Coefficient (r) | p-Value |
|---|---|---|
| FHP angle vs. cervical tilt | −0.048 | 0.783 |
| FHP angle vs. cranial tilt | 0.611 | <0.001 |
| FHP angle vs. T1 slope | 0.417 | 0.011 |
| FHP angle vs. C7 slope | 0.424 | 0.010 |
| FHP angle vs. C2–7 Cobb angle | 0.032 | 0.852 |
| FHP angle vs. CVA | −0.712 | <0.001 |
| FHP angle vs. C2–7 SVA | 0.704 | <0.001 |
| DHKA angle vs. RHKA angle | 0.754 | <0.001 |
| Parameter | ICC |
|---|---|
| FHP angle | 0.84 |
| DHKA angle | 0.90 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.C.; Lee, S.; Yoon, J.; Choi, C.-H.; Yoon, C.; Ha, Y.-C. Validity and Reliability of an Artificial Intelligence-Based Posture Estimation Software for Measuring Cervical and Lower-Limb Alignment Versus Radiographic Imaging. Diagnostics 2025, 15, 1340. https://doi.org/10.3390/diagnostics15111340
Park SC, Lee S, Yoon J, Choi C-H, Yoon C, Ha Y-C. Validity and Reliability of an Artificial Intelligence-Based Posture Estimation Software for Measuring Cervical and Lower-Limb Alignment Versus Radiographic Imaging. Diagnostics. 2025; 15(11):1340. https://doi.org/10.3390/diagnostics15111340
Chicago/Turabian StylePark, Sung Cheol, Sanghee Lee, Jisoo Yoon, Chi-Hyun Choi, Chan Yoon, and Yong-Chan Ha. 2025. "Validity and Reliability of an Artificial Intelligence-Based Posture Estimation Software for Measuring Cervical and Lower-Limb Alignment Versus Radiographic Imaging" Diagnostics 15, no. 11: 1340. https://doi.org/10.3390/diagnostics15111340
APA StylePark, S. C., Lee, S., Yoon, J., Choi, C.-H., Yoon, C., & Ha, Y.-C. (2025). Validity and Reliability of an Artificial Intelligence-Based Posture Estimation Software for Measuring Cervical and Lower-Limb Alignment Versus Radiographic Imaging. Diagnostics, 15(11), 1340. https://doi.org/10.3390/diagnostics15111340






