Diagnostic Challenges and Perinatal Outcomes: A Case Series on a Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Variables
- Maternal characteristics: maternal age and obstetric history.
- Diagnostic characteristics: gestational age at the time of diagnosis.
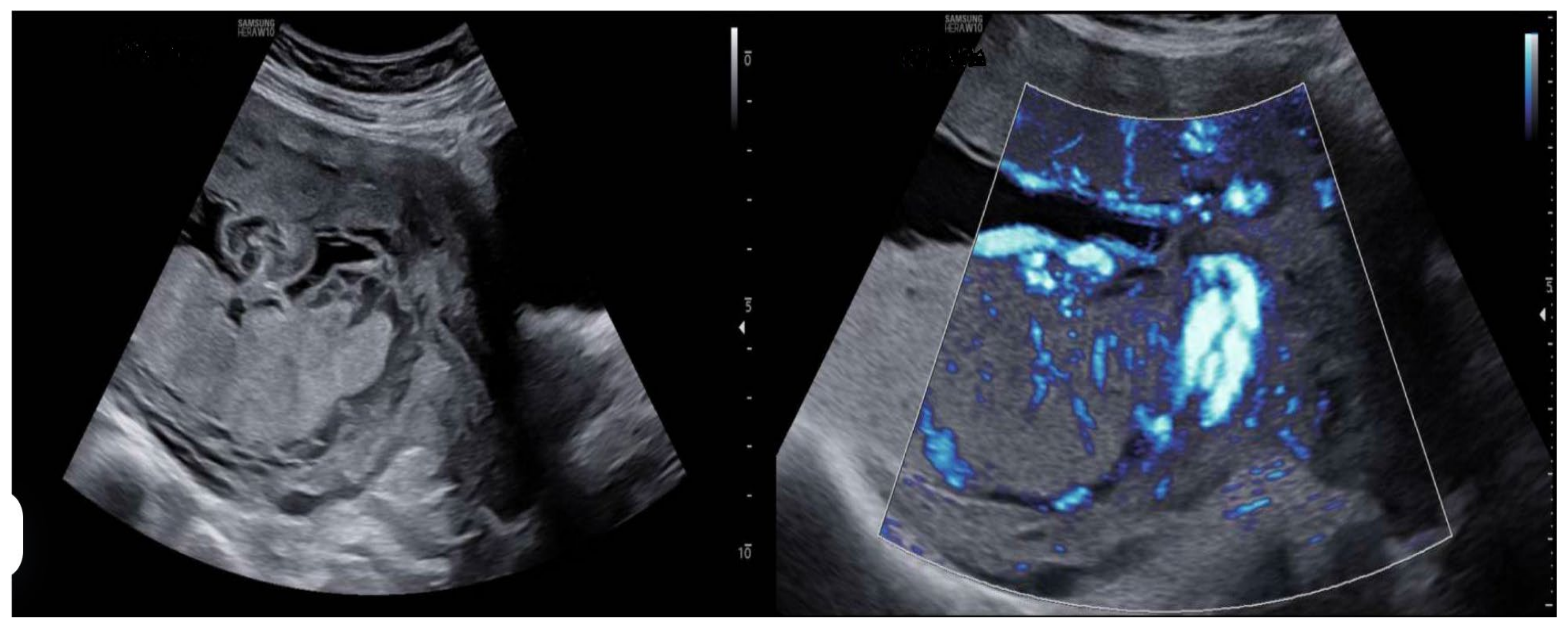
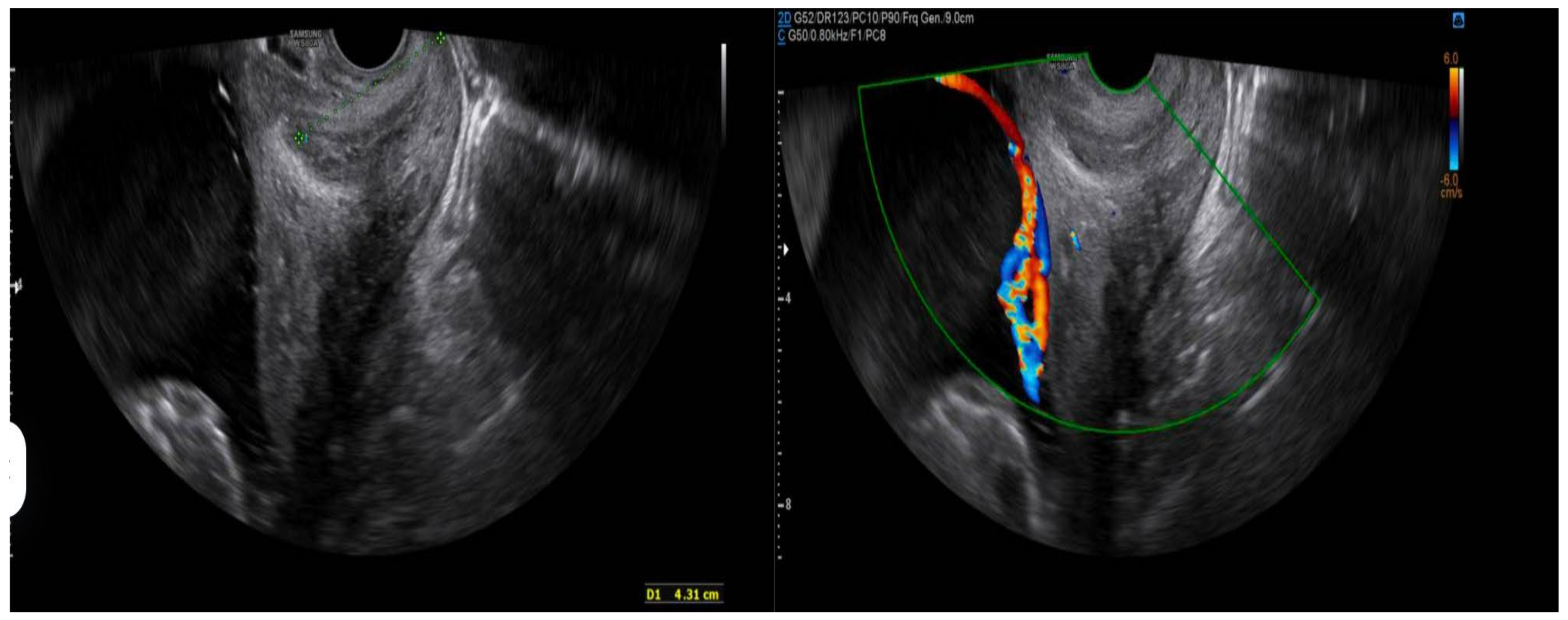
- Prenatal ultrasound evaluation: morphological description of the main placenta and accessory lobe, precise determination of umbilical cord insertion site, color Doppler assessment of vascular connections between lobes, and transvaginal ultrasound to rule out vasa previa.
- Pregnancy outcomes: gestational age at delivery, mode of delivery (spontaneous vaginal, instrumental, or cesarean), and cesarean indications when applicable.
- Maternal and fetal complications: antepartum hemorrhage, placental abruption, retained placenta, postpartum hemorrhage, preterm labor (threatened preterm birth), and intrapartum fetal compromise.
- Neonatal outcomes: birth weight, Apgar scores at 1 and 5 min, and neonatal morbidity and mortality.
2.2. Ultrasound Evaluation Protocol
- Complete morphological evaluation of the placenta.
- Accurate identification of umbilical cord insertion site.
- Color Doppler assessment to identify vascular connections between lobes.
- Transvaginal ultrasound to rule out vasa previa in selected cases.
2.3. Clinical Follow-Up
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. General Characteristics of the Study Population
3.2. Ultrasound Diagnosis
3.3. Assessment of Diagnostic Quality
3.4. Obstetric Outcomes
- Three cases (33.3%) resulted in spontaneous vaginal delivery.
- Two cases (22.2%) required instrumental delivery.
- Four cases (44.4%) were delivered via cesarean section.
3.5. Maternal and Fetal Complications, Neonatal Outcomes
- Intrapartum fetal compromise manifesting as bradycardia during the expulsive phase (two cases).
- Placental abruption (one case).
- Threatened preterm labor (one case)
- The following results were obtained with respect to neonatal outcomes:
- Eight out of the nine pregnancies (88.9%) reached full term (≥37 weeks of gestation).
- Birth weight was appropriate for gestational age in all cases.
- Apgar scores were favorable (≥7 at 5 min) in seven of the nine cases (77.8%). Complete Apgar data were unavailable for one case. One case of neonatal death (11.1%) was recorded and was associated with an instance of placental abruption.
4. Discussion
4.1. Incidence and Diagnosis
4.2. Quality of Ultrasound Diagnosis
4.3. Obstetric Outcomes and Complications
4.4. Postpartum Confirmation
4.5. Neonatal Outcomes
4.6. Clinical Implications
4.7. Study Limitations
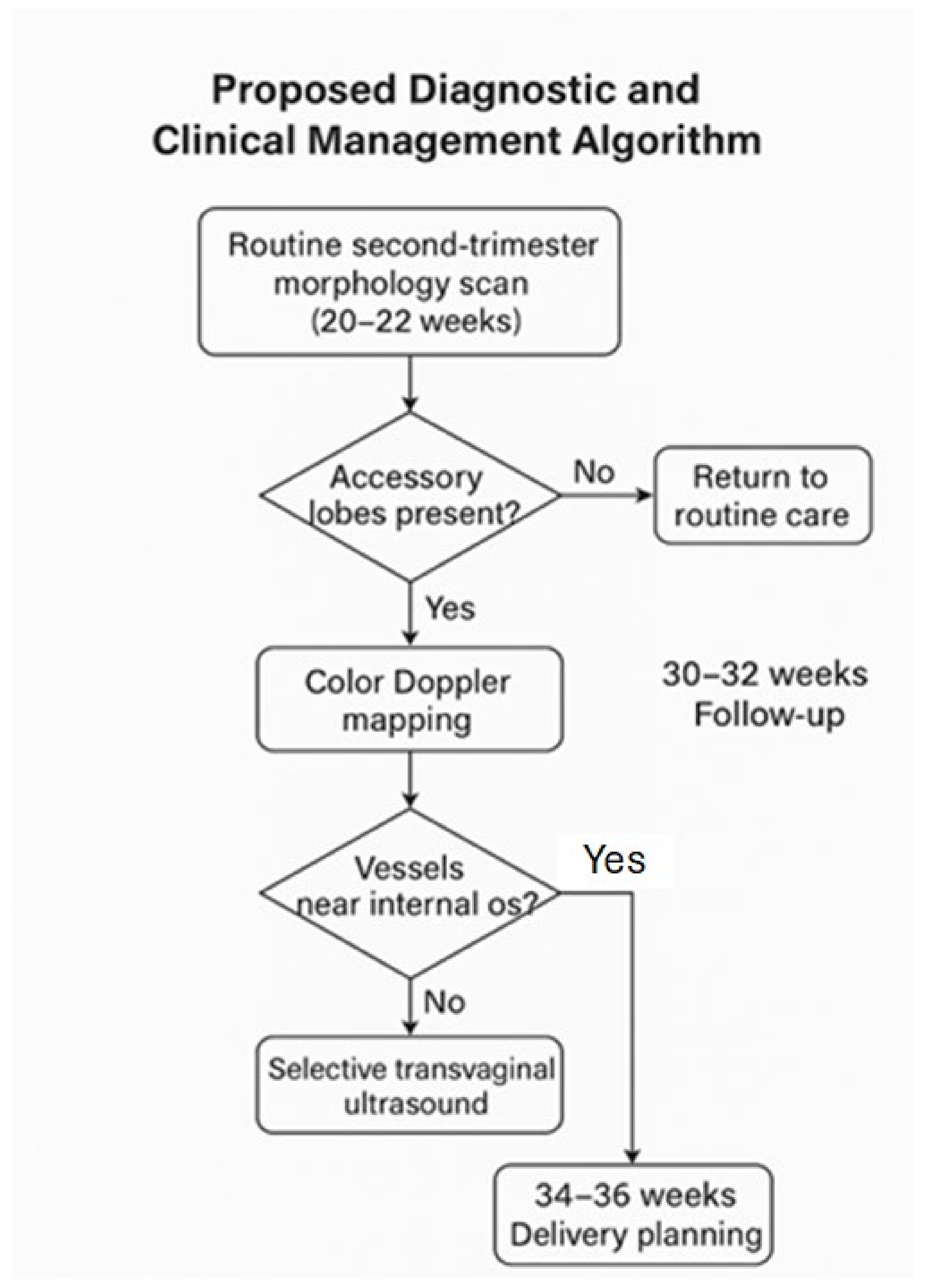
4.8. Proposed Diagnostic and Clinical Management Algorithm
- 1.
- Routine second-trimester morphology scan (20–22 weeks)
- Systematic evaluation of placental shape and continuity.
- Assess for separate echogenic masses suggestive of accessory lobes.
- 2.
- Color Doppler mapping
- Identify vessels traversing fetal membranes between lobes.
- Evaluate the umbilical cord insertion site (central, marginal, velamentous).
- 3.
- Selective transvaginal ultrasound
- Indicated when accessory lobes are low-lying or Doppler imaging reveals vessels near the internal cervical os.
- 4.
- Follow-up and delivery planning
- Intensified monitoring if velamentous insertion or interlobar vessels are present.
- Consider elective cesarean delivery at 34–36 weeks if vasa previa is confirmed.
- Ensure active management during the third stage of labor to prevent retained placental tissue.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heller, H.T.; Mullen, K.M.; Gordon, R.W.; Reiss, R.E.; Benson, C.B. Outcomes of pregnancies with a placental variant detected on routine first-trimester sonography. J. Ultrasound Med. 2014, 33, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Fadl, S.; Moshiri, M.; Fligner, C.L.; Katz, D.S.; Dighe, M. Placental imaging: Normal appearance with review of pathologic findings. Radiographics 2017, 37, 979–998. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Kato, M. Clinical significance of pregnancies complicated by velamentous umbilical cord insertion associated with placental morphological abnormalities. J. Clin. Med. Res. 2015, 7, 853–856. [Google Scholar] [CrossRef] [PubMed]
- Melcer, Y.; Maymon, R.; Jauniaux, E. Vasa previa: Prenatal diagnosis and management. Curr. Opin. Obstet. Gynecol. 2018, 30, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Shaw, C.J.; Kilby, M.D. Improving the detection of vasa previa: A systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2022, 59, 15–23. [Google Scholar]
- Ebbing, C.; Kiserud, T.; Johnsen, S.L.; Albrechtsen, S.; Rasmussen, S. Prevalence, risk factors and outcomes of velamentous and marginal cord insertions: A population-based study of 634,741 pregnancies. PLoS ONE 2013, 8, e70380. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, S.; Ueda, Y.; Matsuzaki, S.; Sakaguchi, H.; Kakuda, M.; Lee, M.; Takemoto, Y.; Hayashida, H.; Maeda, M.; Kakubari, R.; et al. Relationship between Abnormal Placenta and Obstetric Outcomes: A Meta-Analysis. Biomedicines 2023, 11, 1522. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, S.A.; Lavery, J.A.; Ananth, C.V.; Vintzileos, A. Placental implantation abnormalities and risk of preterm delivery: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2015, 213 (Suppl. S4), S78–S90. [Google Scholar] [CrossRef] [PubMed]
- Nardozza, L.M.M.; Caetano, A.C.R.; Zamarian, A.C.P.; Mazzola, J.B.; Silva, C.P.; Marçal, V.M.G.; Araujo Júnior, E. Fetal growth restriction: Current knowledge. Arch. Gynecol. Obstet. 2017, 295, 1061–1077. [Google Scholar] [CrossRef] [PubMed]
- Siargkas, A.; Pachi, C.; Nigdelis, M.P.; Stavros, S.; Domali, E.; Mamopoulos, A.; Tsakiridis, I.; Dagklis, T. The Association of Placental Grading with Perinatal Outcomes: A Systematic Review and Meta-Analysis. Diagnostics 2025, 15, 1264. [Google Scholar] [CrossRef]
- Gizzo, S.; Noventa, M.; Vitagliano, A.; Quaranta, M.; Giovanni, V.D.; Borgato, S.; Saccardi, C.; D’Antona, D. Sonographic assessment of placental location: A mere notional description or an important key to improve both pregnancy and perinatal obstetrical care? A large cohort study. Int. J. Clin. Exp. Med. 2015, 8, 13056–13066. [Google Scholar] [PubMed]
- Nkwabong, E.; Njikam, F.; Kalla, G. Outcome of pregnancies with marginal umbilical cord insertion. J. Matern. Neonatal. Med. 2021, 34, 1133–1137. [Google Scholar] [CrossRef] [PubMed]
- Bhide, A.; Acharya, G.; Baschat, A.; Bilardo, C.M.; Brezinka, C.; Cafici, D.; Ebbing, C.; Hernandez-Andrade, E.; Kalache, K.; Kingdom, J.; et al. ISUOG practice guidelines: Use of Doppler velocimetry in obstetrics. Ultrasound Obstet. Gynecol. 2021, 58, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Stickler, M.; Graham, S.; Conway, R.P.; Franks, A.M. Succenturiate placental lobe abruption: A placental pathology complicating a dangerous delivery. Marshall J. Med. 2022, 9, 4. [Google Scholar] [CrossRef]
- Burton, G.J.; Jauniaux, E. Pathophysiology of placental-derived fetal growth restriction. Am. J. Obstet. Gynecol. 2018, 218, S745–S761. [Google Scholar] [CrossRef] [PubMed]
- Oyelese, Y.; Smulian, J.C. Placenta previa, placenta accreta, and vasa previa. Obstet. Gynecol. 2006, 107, 927–941. [Google Scholar] [CrossRef] [PubMed]
| Year | GA (wks) | Anomaly | Labor Onset | Delivery Type | Complications | Weight | Apgar |
|---|---|---|---|---|---|---|---|
| 2023 | 21 + 3 | Succenturiate placenta + IV | Cesarean (breech) | Central extrafundal cesarean | - | 3280 | 9/10 |
| 2023 | 38 + 2 | Succenturiate placenta | Cesarean (breech) | Cesarean | - | 2930 | 9/10 |
| 2022 | 41 + 3 | Succenturiate placenta | Induction due to EVP | Vaginal (eutocic) | - | 3180 | 9/10 |
| 2017 | 34 + 4 | Succenturiate placenta | Spontaneous | Vaginal (eutocic) | IUGR 34w | 2340 | 9/10 |
| 2012 | 39 + 1 | Succenturiate placenta | Spontaneous | Extrafundal vaginal delivery | - | 2890 | 9/10 |
| 2011 | 39 + 1 | Succenturiate placenta | Spontaneous | Instrumental (PFBF) | Expulsive bradycardia | 2640 | 9/10 |
| 2005 | 39 + 3 | Succenturiate placenta + IV | Spontaneous | Emergency cesarean for PROM + S | - | 2670 | 9/10 |
| 2013 | 42 + 2 | Succenturiate placenta + IV | Spontaneous | Instrumental (PFBF) | Expulsive bradycardia | 2960 | 9/10 |
| 2007 | 37 + 6 | Succenturiate placenta + IV | Spontaneous | Emergency cesarean | Abruption (PDNIP) | 2650 | 0/1 |
| Characteristic | n (%) or Mean ± SD |
|---|---|
| Diagnosis | |
| Isolated succenturiate placenta | 5 (55.6%) |
| Succenturiate placenta + velamentous cord insertion | 4 (44.4%) |
| Succenturiate placenta + vasa previa | 0 (0%) |
| Pregnancy Outcome | |
| Spontaneous vaginal delivery | 3 (33.3%) |
| Instrumental delivery | 2 (22.2%) |
| Cesarean section | 4 (44.4%) |
| Maternal–Fetal Complications | |
| Intrapartum fetal bradycardia | 2 (22.2%) |
| Placental abruption (DPPNI) | 1 (11.1%) |
| Threatened preterm labor (TPL) | 1 (11.1%) |
| No complications | 5 (55.6%) |
| Neonatal Outcomes | |
| Term birth (≥37 weeks) | 8 (88.9%) |
| Favorable Apgar score (≥7 at 5 min) | 7 (77.8%) |
| Appropriate birth weight for gestational age | 9 (100%) |
| Neonatal mortality | 1 (11.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moral-Moral, C.M.; Porras-Caballero, L.; Blasco-Alonso, M.; Cuenca-Marín, C.; Monis-Rodriguez, S.; Gonzalez-Mesa, E.; Narbona-Arias, I.; Jimenez-Lopez, J.S. Diagnostic Challenges and Perinatal Outcomes: A Case Series on a Retrospective Study. Diagnostics 2025, 15, 1329. https://doi.org/10.3390/diagnostics15111329
Moral-Moral CM, Porras-Caballero L, Blasco-Alonso M, Cuenca-Marín C, Monis-Rodriguez S, Gonzalez-Mesa E, Narbona-Arias I, Jimenez-Lopez JS. Diagnostic Challenges and Perinatal Outcomes: A Case Series on a Retrospective Study. Diagnostics. 2025; 15(11):1329. https://doi.org/10.3390/diagnostics15111329
Chicago/Turabian StyleMoral-Moral, Carmen Maria, Lorena Porras-Caballero, Marta Blasco-Alonso, Celia Cuenca-Marín, Susana Monis-Rodriguez, Ernesto Gonzalez-Mesa, Isidoro Narbona-Arias, and Jesus S. Jimenez-Lopez. 2025. "Diagnostic Challenges and Perinatal Outcomes: A Case Series on a Retrospective Study" Diagnostics 15, no. 11: 1329. https://doi.org/10.3390/diagnostics15111329
APA StyleMoral-Moral, C. M., Porras-Caballero, L., Blasco-Alonso, M., Cuenca-Marín, C., Monis-Rodriguez, S., Gonzalez-Mesa, E., Narbona-Arias, I., & Jimenez-Lopez, J. S. (2025). Diagnostic Challenges and Perinatal Outcomes: A Case Series on a Retrospective Study. Diagnostics, 15(11), 1329. https://doi.org/10.3390/diagnostics15111329









