Nomogram-Based Prediction of Survival in Stage IV Nasopharyngeal Carcinoma: A Retrospective Single-Center Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Patients and Data Acquisition
2.3. Nutritional Status
2.4. Inflammatory Biomarkers
2.5. Statistical Analysis
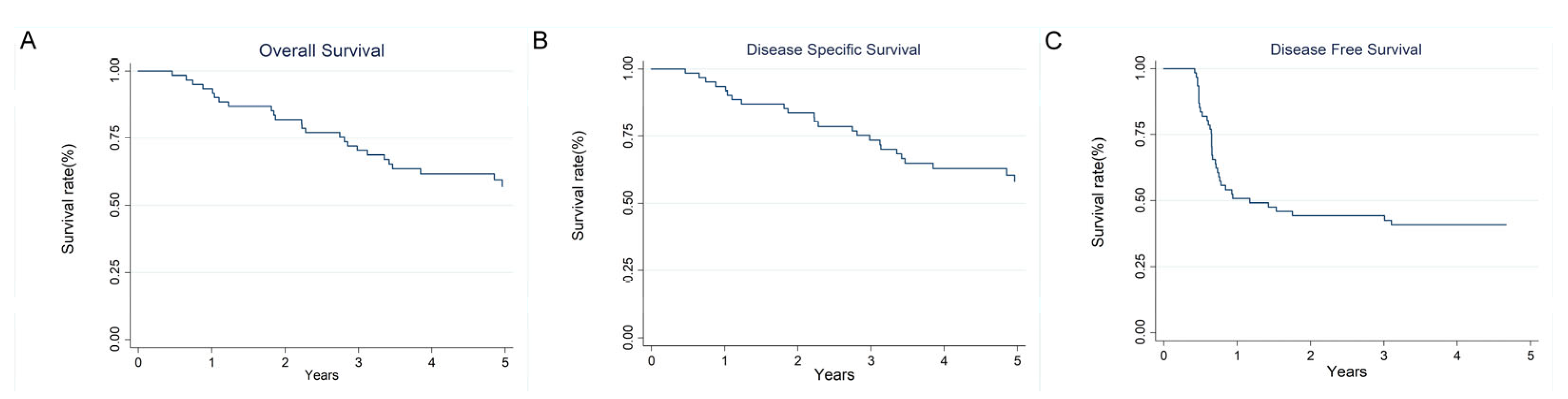
3. Results
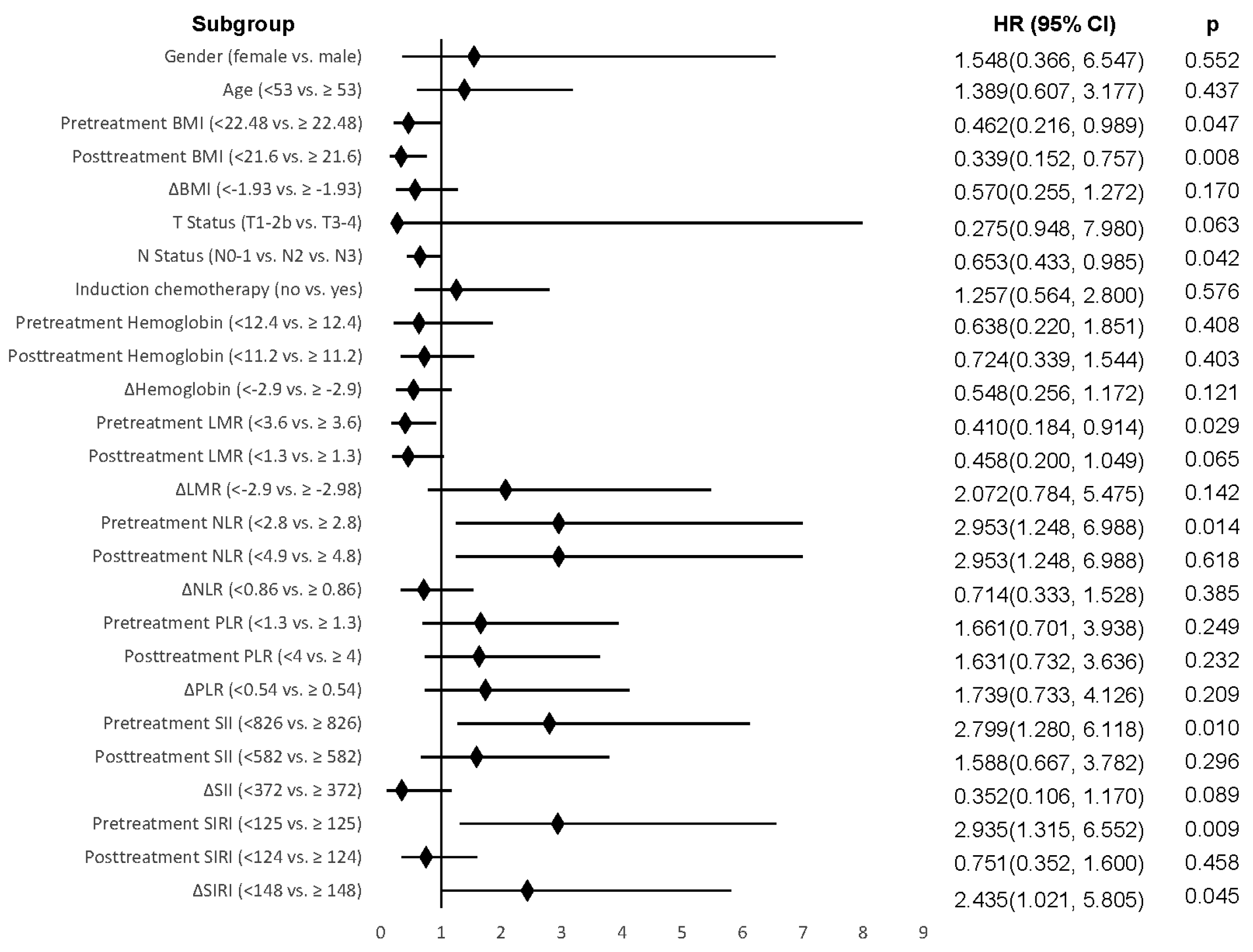
3.1. Univariate Analysis
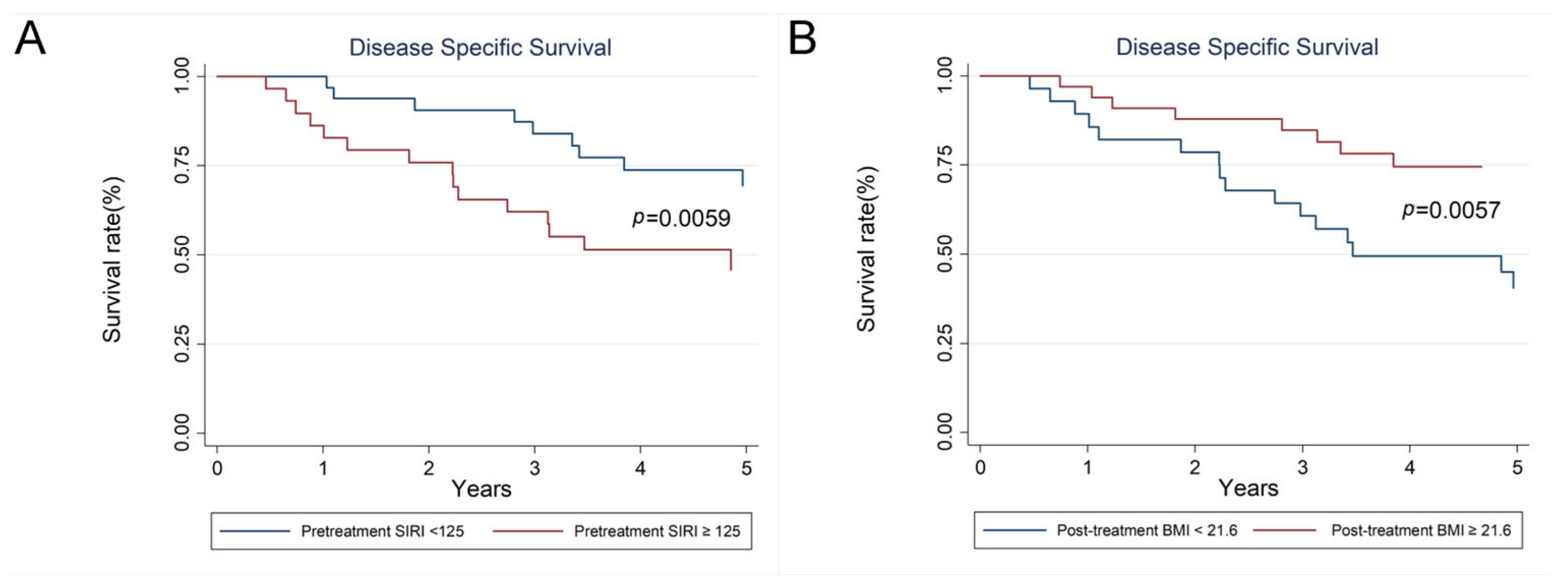
3.2. Multivariate Analysis
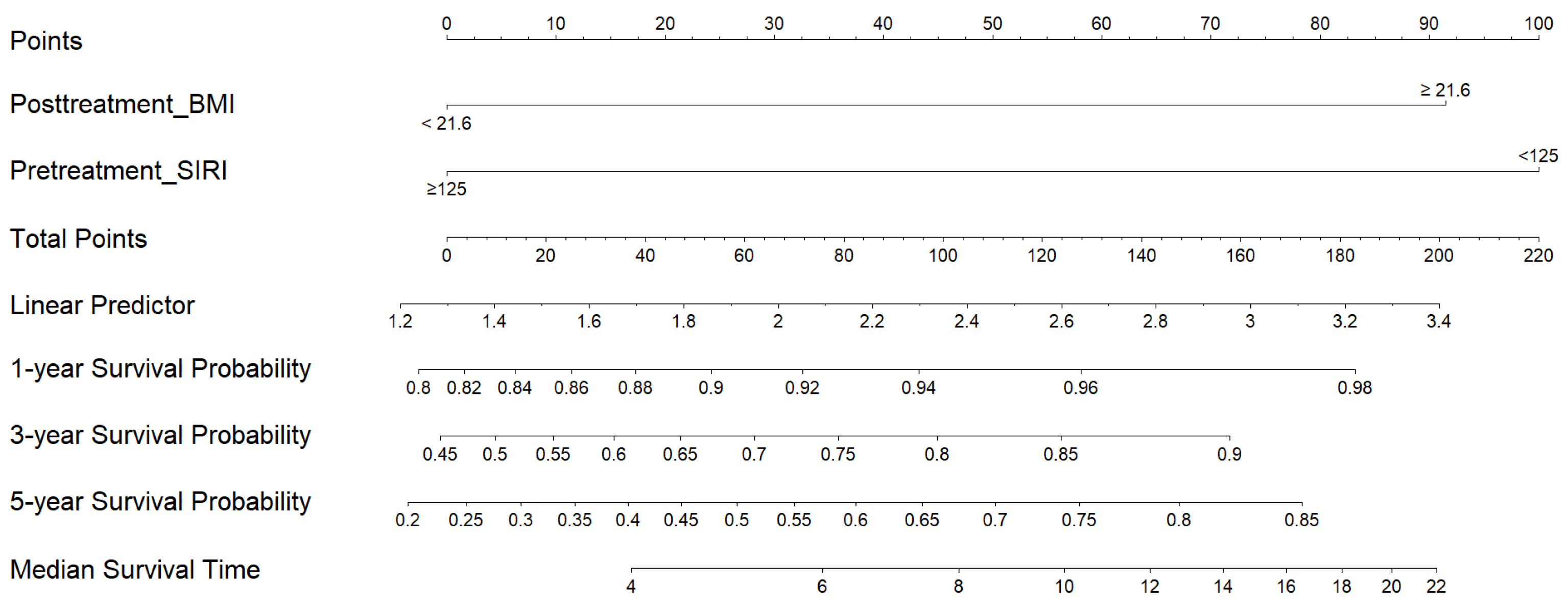
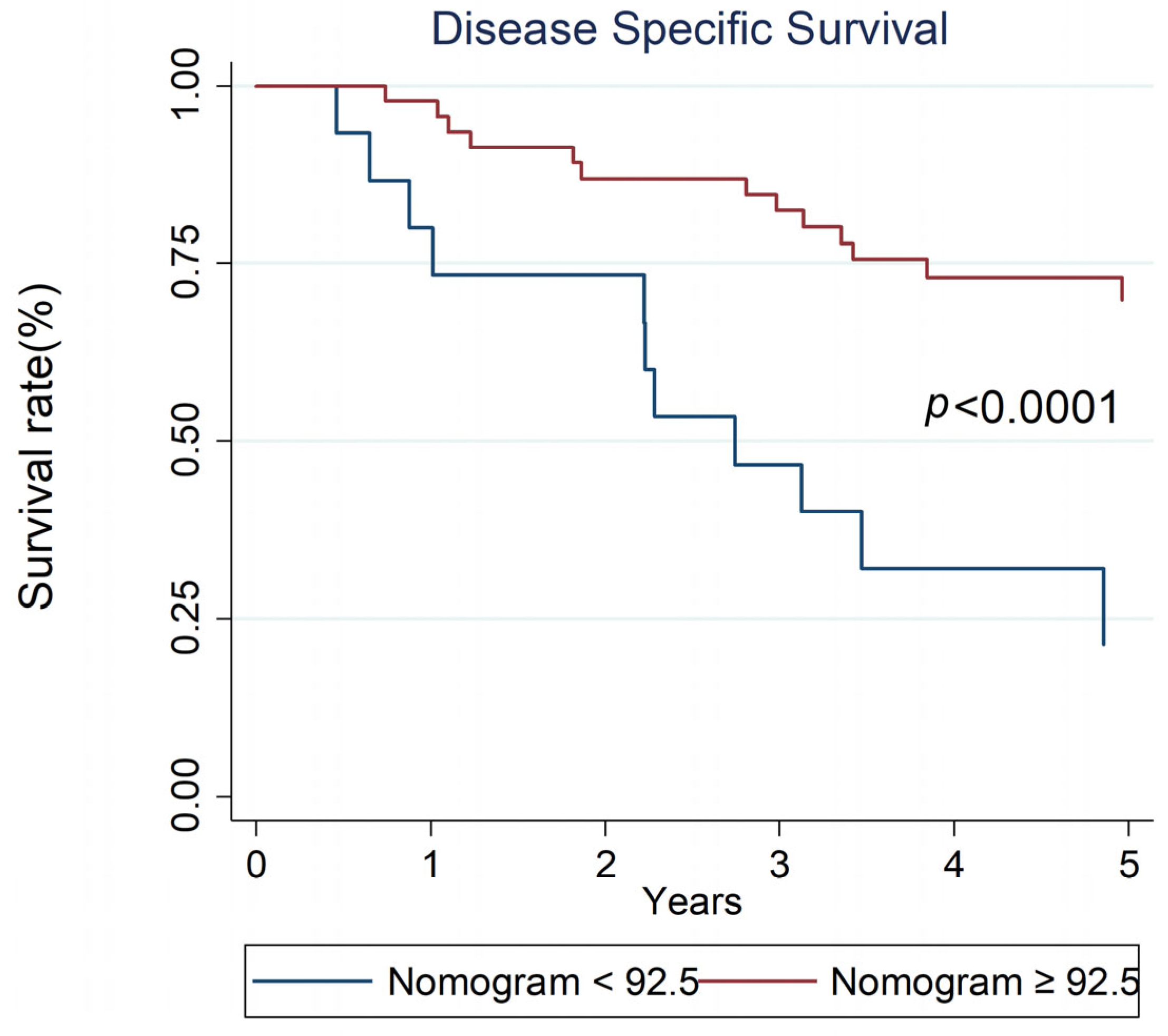
3.3. Nomogram
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NPC | Nasopharyngeal carcinoma |
| WHO | World Health Organization |
| AJCC | American Joint Committee on Cancer |
| TNM | Tumor-node-metastasis |
| NCCN | National Comprehensive Cancer Network |
| CCRT | Concurrent chemoradiotherapy |
| NLR | Neutrophil-to-lymphocyte ratio |
| Hb | Hemoglobin |
| TME | Tumor microenvironment |
| BMI | Body mass index |
| HNC | Head and neck cancer |
| LMR | Lymphocyte-to-monocyte ratio |
| PLR | Platelet-to-lymphocyte ratio |
| SII | Systemic immune-inflammation index |
| SIRI | Systemic inflammation response index |
| SD | Standard deviation |
| CI | Confidence interval |
| HR | Hazard ratio |
| IQR | Interquartile range |
| OS | Overall survival |
| DSS | Disease-specific survival |
| DFS | Disease-free survival |
| ROC | Receiver operating characteristic |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Cancer Registry. Taiwan Cancer Registry Reporting Manual; Taiwan Cancer Registry: Taipei City, Taiwan, 1979. [Google Scholar]
- Chen, Y.-P.; Chan, A.T.C.; Le, Q.-T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.T.; Ye, W.; Zeng, Y.-X.; Adami, H.-O. The Evolving Epidemiology of Nasopharyngeal Carcinoma. Cancer Epidemiol. Biomark. Prev. 2021, 30, 1035–1047. [Google Scholar] [CrossRef]
- Liao, L.-J.; Hsu, W.-L.; Wang, C.-T.; Lo, W.-C.; Cheng, P.-W.; Shueng, P.-W.; Hsieh, C.-H.; Chiu, Y.L.; Lin, Y.-C. Prognostic impact of pre-treatment neutrophil-to-lymphocyte ratio (NLR) in nasopharyngeal carcinoma: A retrospective study of 180 Taiwanese patients. Clin. Otolaryngol. 2018, 43, 463–469. [Google Scholar] [CrossRef]
- Liu, Z.; Chang, E.T.; Liu, Q.; Cai, Y.; Zhang, Z.; Chen, G.; Xie, S.-H.; Cao, S.-M.; Shao, J.-Y.; Jia, W.-H.; et al. Oral Hygiene and Risk of Nasopharyngeal Carcinoma—A Population-Based Case–Control Study in China. Cancer Epidemiol. Biomark. Prev. 2016, 25, 1201–1207. [Google Scholar] [CrossRef]
- Huang, S.-F.; Hsiao, J.-H.; Young, C.-K.; Chien, H.-T.; Kuo, C.-F.; See, L.-C.; Luo, S.-F.; Huang, L.-H.; Liao, C.-T.; Chang, T.-C.J. Familial aggregation of nasopharyngeal carcinoma in Taiwan. Oral. Oncol. 2017, 73, 10–15. [Google Scholar] [CrossRef]
- Guo, R.; Tang, L.-L.; Mao, Y.-P.; Du, X.-J.; Chen, L.; Zhang, Z.-C.; Liu, L.-Z.; Tian, L.; Luo, X.-T.; Xie, Y.-B.; et al. Proposed modifications and incorporation of plasma Epstein-Barr virus DNA improve the TNM staging system for Epstein-Barr virus-related nasopharyngeal carcinoma. Cancer 2019, 125, 79–89. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network I. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Head and Neck Cancers (Version 3.2024). 2024. [Updated 29 February 2024]. Available online: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf (accessed on 10 April 2025).
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.L.; Chen, Y.P.; Mao, Y.P.; Wang, Z.X.; Guo, R.; Chen, L.; Tian, L.; Lin, A.-H.; Li, L.; Sun, Y.; et al. Validation of the 8th Edition of the UICC/AJCC Staging System for Nasopharyngeal Carcinoma from Endemic Areas in the Intensity-Modulated Radiotherapy Era. J. Natl. Compr. Cancer Netw. 2017, 15, 913–919. [Google Scholar] [CrossRef]
- Long, G.; Tang, W.; Fu, X.; Liu, D.; Zhang, L.; Hu, G.; Hu, G.; Sun, W. Pre-treatment Serum Lactate Dehydrogenase Predicts Distant Metastasis and Poor Survival in Nasopharyngeal Carcinoma. J. Cancer 2019, 10, 3657–3664. [Google Scholar] [CrossRef]
- Zhang, L.L.; Zhou, G.Q.; Li, Y.Y.; Tang, L.L.; Mao, Y.P.; Lin, A.H.; Ma, J.; Qi, Z.-Y.; Sun, Y. Combined prognostic value of pretreatment anemia and cervical node necrosis in patients with nasopharyngeal carcinoma receiving intensity-modulated radiotherapy: A large-scale retrospective study. Cancer Med. 2017, 6, 2822–2831. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, P.Y.; Su, Z.; Mao, Y.P.; Liu, Q.; Xie, F.Y. Prognostic value of ABO blood group in southern Chinese patients with established nasopharyngeal carcinoma. Br. J. Cancer 2013, 109, 2462–2466. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.J.; Khan, M.; Chatterjee, U.; Santhosh, S.; Hashmi, M.; Gill, J.; Yu, B.; Iovoli, A.; Farrugia, M.; Wooten, K.; et al. Association of Body Mass Index with Outcomes Among Patients with Head and Neck Cancer Treated with Chemoradiotherapy. JAMA Netw. Open 2023, 6, e2320513. [Google Scholar] [CrossRef]
- Tazzyman, S.; Lewis, C.E.; Murdoch, C. Neutrophils: Key mediators of tumour angiogenesis. Int. J. Exp. Pathol. 2009, 90, 222–231. [Google Scholar] [CrossRef]
- Treffers, L.W.; Hiemstra, I.H.; Kuijpers, T.W.; van den Berg, T.K.; Matlung, H.L. Neutrophils in cancer. Immunol. Rev. 2016, 273, 312–328. [Google Scholar] [CrossRef]
- Chraa, D.; Naim, A.; Olive, D.; Badou, A. T lymphocyte subsets in cancer immunity: Friends or foes. J. Leukoc. Biol. 2018, 105, 243–255. [Google Scholar] [CrossRef] [PubMed]
- Haemmerle, M.; Stone, R.L.; Menter, D.G.; Afshar-Kharghan, V.; Sood, A.K. The platelet lifeline to cancer: Challenges and opportunities. Cancer cell 2018, 33, 965–983. [Google Scholar] [CrossRef]
- Olingy, C.E.; Dinh, H.Q.; Hedrick, C.C. Monocyte heterogeneity and functions in cancer. J. Leukoc. Biol. 2019, 106, 309–322. [Google Scholar] [CrossRef]
- Tham, T.; Olson, C.; Khaymovich, J.; Herman, S.W.; Costantino, P.D. The lymphocyte-to-monocyte ratio as a prognostic indicator in head and neck cancer: A systematic review and meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2018, 275, 1663–1670. [Google Scholar] [CrossRef]
- Mascarella, M.A.; Mannard, E.; Silva, S.D.; Zeitouni, A. Neutrophil-to-lymphocyte ratio in head and neck cancer prognosis: A systematic review and meta-analysis. Head. Neck 2018, 40, 1091–1100. [Google Scholar] [CrossRef]
- Bardash, Y.; Olson, C.; Herman, W.; Khaymovich, J.; Costantino, P.; Tham, T. Platelet-Lymphocyte Ratio as a Predictor of Prognosis in Head and Neck Cancer: A Systematic Review and Meta-Analysis. Oncol. Res. Treat. 2019, 42, 665–677. [Google Scholar] [CrossRef] [PubMed]
- Valero, C.; Pardo, L.; Sansa, A.; Garcia Lorenzo, J.; López, M.; Quer, M.; León, X. Prognostic capacity of Systemic Inflammation Response Index (SIRI) in patients with head and neck squamous cell carcinoma. Head. Neck 2020, 42, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-T.; Kuo, L.-T.; Weng, H.-H.; Hsu, C.-M.; Tsai, M.-S.; Chang, G.-H.; Lee, Y.-C.; Huang, E.I.; Tsai, Y.-T. Systemic Immun e–Inflammation Index as a Predictor for Head and Neck Cancer Prognosis: A Meta-Analysis. Front. Oncol. 2022, 12, 899518. [Google Scholar] [CrossRef] [PubMed]
- Yeh, P.; Chang, C.-M.; Liao, L.-J.; Wu, C.-Y.; Hsieh, C.-H.; Shueng, P.-W.; Cheng, P.-W.; Lo, W.-C. A predictive survival model for patients with stage IV oropharyngeal squamous cell carcinoma treated with chemoradiation. Eur. Arch. Oto-Rhino-Laryngol. 2024, 281, 369–377. [Google Scholar] [CrossRef]
- Gama, R.R.; Song, Y.; Zhang, Q.; Brown, M.C.; Wang, J.; Habbous, S.; Tong, L.; Huang, S.H.; O’Sullivan, B.; Waldron, J.; et al. Body mass index and prognosis in patients with head and neck cancer. Head. Neck 2017, 39, 1226–1233. [Google Scholar] [CrossRef]
- Hollander, D.d.; Kampman, E.; van Herpen, C.M.L. Pretreatment body mass index and head and neck cancer outcome: A review of the literature. Crit. Rev. Oncol. Hematol. 2015, 96, 328–338. [Google Scholar] [CrossRef]
- Lønbro, S.; Petersen, G.B.; Andersen, J.R.; Johansen, J. Prediction of critical weight loss during radiation treatment in head and neck cancer patients is dependent on BMI. Support. Care Cancer 2016, 24, 2101–2109. [Google Scholar] [CrossRef]
- Fattouh, M.; Chang, G.Y.; Ow, T.J.; Shifteh, K.; Rosenblatt, G.; Patel, V.M.; Smith, R.V.; Prystowsky, M.B.; Schlecht, N.F. Association between pretreatment obesity, sarcopenia, and survival in patients with head and neck cancer. Head. Neck 2019, 41, 707–714. [Google Scholar] [CrossRef]
- Du, Y.; Feng, R.; Chang, E.T.; Yin, L.; Huang, T.; Li, Y.; Zhou, X.; Huang, Y.; Zhou, F.; Su, C.; et al. Body mass index and body shape before treatment and nasopharyngeal carcinoma prognosis: A population-based patient cohort study in southern China. Int. J. Cancer 2023, 153, 290–301. [Google Scholar] [CrossRef]
- Jin, X.; Hu, R.; Guo, H.; Ding, C.; Pi, G.; Tian, M. Pretreatment Body Mass Index (BMI) as an Independent Prognostic Factor in Nasopharyngeal Carcinoma Survival: A Systematic Review and Meta-Analysis. Nutr. Cancer 2022, 74, 3457–3467. [Google Scholar] [CrossRef]
- Hedrick, C.C.; Malanchi, I. Neutrophils in cancer: Heterogeneous and multifaceted. Nat. Rev. Immunol. 2022, 22, 173–187. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, M. Role of platelets and platelet receptors in cancer metastasis. J. Hematol. Oncol. 2018, 11, 125. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Zhuang, L.; Shen, Y.; Geng, Y.; Yu, S.; Chen, H.; Liu, L.; Meng, Z.; Wang, P.; Chen, Z. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer 2016, 122, 2158–2167. [Google Scholar] [CrossRef]
- Lo, W.-C.; Chang, C.-M.; Wu, C.-Y.; Hsieh, C.-H.; Shueng, P.-W.; Cheng, P.-W.; Liao, L.-J. A predictive model for advanced oropharyngeal cancer patients treated with chemoradiation. BMC Cancer 2022, 22, 615. [Google Scholar] [CrossRef]
- Atasever Akkas, E.; Erdis, E.; Yucel, B. Prognostic value of the systemic immune-inflammation index, systemic inflammation response index, and prognostic nutritional index in head and neck cancer. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 3821–3830. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.-F.; Wu, C.-Y.; Lo, W.-C.; Chiu, Y.-L.; Shueng, P.-W.; Hsieh, C.-H.; Hsu, C.-X.; Kuo, D.-Y.; Hou, P.-Y.; Liao, L.-J. Postchemoradiotherapy systemic inflammation response index predicts treatment response and overall survival for patients with locally advanced nasopharyngeal cancer. J. Formos. Med. Assoc. 2023, 122, 1141–1149. [Google Scholar] [CrossRef]
- Yuan, X.; Yang, H.; Zeng, F.; Zhou, S.; Wu, S.; Yuan, Y.; Cui, L.; Feng, H.; Lin, D.; Chen, Z.; et al. Prognostic value of systemic inflammation response index in nasopharyngeal carcinoma with negative Epstein-Barr virus DNA. BMC Cancer 2022, 22, 858. [Google Scholar] [CrossRef]
- Miao, J.; Wang, L.; Ong, E.H.W.; Hu, C.; Lin, S.; Chen, X.; Chen, Y.; Zhong, Y.; Jin, F.; Lin, Q.; et al. Effects of induction chemotherapy on nutrition status in locally advanced nasopharyngeal carcinoma: A multicentre prospective study. J. Cachexia Sarcopenia Muscle 2023, 14, 815–825. [Google Scholar] [CrossRef]
- Jia, P.; Wu, X.; Shen, F.; Xu, G.; Xu, H.; Cong, M.; Song, C.; Shi, H. Nutritional status and its correlation to prognosis of nasopharyngeal carcinoma patients in different ages in China: A multicenter cohort study. Support. Care Cancer 2023, 31, 638. [Google Scholar] [CrossRef]
- Nishikawa, H.; Goto, M.; Fukunishi, S.; Asai, A.; Nishiguchi, S.; Higuchi, K. Cancer Cachexia: Its Mechanism and Clinical Significance. Int. J. Mol. Sci. 2021, 22, 8491. [Google Scholar] [CrossRef]
- Zhang, L.-L.; Xu, F.; Song, D.; Huang, M.-Y.; Huang, Y.-S.; Deng, Q.-L.; Li, Y.-Y.; Shao, J.-Y. Development of a Nomogram Model for Treatment of Nonmetastatic Nasopharyngeal Carcinoma. JAMA Netw. Open 2020, 3, e2029882. [Google Scholar] [CrossRef] [PubMed]
| N (%) or Mean ± SD or Median (Range, IQR) | ||
|---|---|---|
| Age (years) | 56.7 ± 11 (24–88) | |
| Gender | Male | 55 (90.16%) |
| Female | 6 (9.84%) | |
| Clinical T Classification | T1/T2/T3/T4 | 12 (19.67%)/7 (18.03%)/12 (19.67%)/30 (49.18%) |
| Clinical N Classification | N0/N1/N2/N3 | 5 (8.20%)/12 (19.67%)/9 (14.75%)/20 (32.79%) |
| Body Height (cm) | 166.7 ± 7.4 (149–189) | |
| Pretreatment BW (kg) | 69.6 ± 16.5 (43–146) | |
| Posttreatment BW (kg) | 62.2 ± 11.9 (41–107) | |
| Pretreatment BMI (kg/m2) | 24.9 ± 4.5 (16.38–40.87) | |
| Posttreatment BMI (kg/m2) | 62.2 ± 11.9 (41–107) | |
| Induction chemotherapy | With/Without | 37 (60.66%)/24 (39.34%) |
| Death within 5 years | 28 (45.90%) | |
| Disease Persistence | 28 (45.90%) | |
| Recurrence | Local/Regional/Distant | 12 (19.67%)/9 (14.75%)/24 (39.34%) |
| Follow-up duration (days) | 1716 ± 1096 (169–5281) | |
| Smoking status | Yes/No | 34 (55.74%)/27 (44.26%) |
| ECOG performance status | 0/1/2/4 | 30 (49.18%)/29 (47.54%)/1 (1.64%)/1 (1.64%) |
| Hypertension | Yes/No | 5 (8.20%)/56 (91.80%) |
| Diabetes | Yes/No | 2 (3.28%)/59 (96.72%) |
| Hepatitis B | Yes/No | 3 (4.92%)/58 (95.08%) |
| Coronary artery disease | Yes/No | 2 (3.28%)/59 (96.72%) |
| Variables | Dichotomized Units | OS | DSS | DFS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95%CI | p-Value | HR | 95%CI | p-Value | HR | 95%CI | p-Value | |||||
| Gender | Female vs. male | 1.611 | 0.382 | 6.800 | 0.516 | 1.548 | 0.366 | 6.547 | 0.552 | 3.083 | 1.346 | 0.413 | 4.389 |
| Age | <53 vs. ≥53 | 1.747 | 0.742 | 4.116 | 0.202 | 1.389 | 0.607 | 3.177 | 0.437 | 1.423 | 0.711 | 2.849 | 0.319 |
| Pretreatment BMI (kg/m2) | <22.48 vs. ≥22.48 | 0.430 | 0.204 | 0.906 | 0.026 | 0.462 | 0.216 | 0.989 | 0.047 | 0.533 | 0.272 | 1.043 | 0.066 |
| Posttreatment BMI (kg/m2) | <21.6 vs. ≥21.6 | 0.380 | 0.175 | 0.826 | 0.015 | 0.339 | 0.152 | 0.757 | 0.008 | 0.353 | 0.180 | 0.693 | 0.002 |
| Δ BMI (kg/m2) | <−1.93 vs. ≥−1.93 | 0.634 | 0.292 | 1.378 | 0.250 | 0.570 | 0.255 | 1.272 | 0.170 | 0.443 | 0.213 | 0.921 | 0.029 |
| T status | T1&T2 vs. T3&T4 | 2.880 | 0.996 | 8.328 | 0.051 | 0.275 | 0.948 | 7.980 | 0.063 | 1.657 | 0.776 | 3.536 | 0.192 |
| N status | N0-1 vs. N2 vs. N3 | 0.681 | 0.445 | 1.019 | 0.062 | 0.653 | 0.433 | 0.985 | 0.042 | 0.723 | 0.502 | 1.040 | 0.080 |
| Pretreatment Hb (gm/dL) | <16 vs. ≥16 | 0.513 | 0.194 | 1.353 | 0.117 | 0.638 | 0.220 | 1.851 | 0.408 | 0.800 | 0.311 | 2.060 | 0.644 |
| Posttreatment Hb (gm/dL) | <11.2 vs. ≥11.2 | 0.582 | 0.276 | 1.225 | 0.154 | 0.724 | 0.339 | 1.544 | 0.403 | 0.948 | 0.488 | 1.842 | 0.875 |
| Δ Hb (gm/dL) | <−2.9 vs. ≥−2.9 | 0.684 | 0.326 | 1.436 | 0.316 | 0.548 | 0.256 | 1.172 | 0.121 | 0.598 | 0.310 | 1.154 | 0.125 |
| Pretreatment LMR | <3.6 vs. ≥3.6 | 0.456 | 0.210 | 0.990 | 0.047 | 0.410 | 0.184 | 0.914 | 0.029 | 0.553 | 0.286 | 1.070 | 0.078 |
| Posttreatment LMR | <1.3 vs. ≥1.3 | 0.485 | 0.213 | 1.104 | 0.085 | 0.458 | 0.200 | 1.049 | 0.065 | 0.493 | 0.231 | 1.054 | 0.068 |
| Δ LMR | <−2.98 vs. ≥−2.98 | 1.414 | 0.601 | 3.327 | 0.728 | 2.072 | 0.784 | 5.475 | 0.142 | 1.369 | 0.659 | 2.843 | 0.400 |
| Pretreatment PLR | <1.3 vs. ≥1.3 | 1.748 | 0.741 | 4.210 | 0.202 | 1.661 | 0.701 | 3.938 | 0.249 | 1.362 | 0.680 | 2.728 | 0.383 |
| Posttreatment PLR | <4 vs. ≥4 | 1.557 | 0.704 | 3.446 | 0.275 | 1.631 | 0.732 | 3.636 | 0.232 | 1.892 | 0.944 | 3.794 | 0.072 |
| Δ PLR | <0.54 vs. ≥0.54 | 1.829 | 0.775 | 4.314 | 0.168 | 1.739 | 0.733 | 4.126 | 0.209 | 1.856 | 0.843 | 4.083 | 0.124 |
| Pretreatment NLR | <2.8 vs. ≥2.8 | 2.575 | 1.134 | 5.851 | 0.024 | 2.953 | 1.248 | 6.988 | 0.014 | 2.725 | 1.355 | 5.481 | 0.005 |
| Posttreatment NLR | <4.8 vs. ≥4.8 | 1.312 | 0.622 | 2.767 | 0.476 | 2.953 | 1.248 | 6.988 | 0.618 | 1.881 | 0.973 | 3.638 | 0.060 |
| Δ NLR | <0.86 vs. ≥0.86 | 0.771 | 0.366 | 1.625 | 0.495 | 0.714 | 0.333 | 1.528 | 0.385 | 0.809 | 0.420 | 1.559 | 0.527 |
| Pretreatment SII | <826 vs. ≥826 | 2.533 | 1.185 | 5.412 | 0.016 | 2.799 | 1.280 | 6.118 | 0.010 | 2.699 | 1.385 | 5.257 | 0.004 |
| Posttreatment SII | <582 vs. ≥582 | 1.655 | 0.699 | 3.920 | 0.252 | 1.588 | 0.667 | 3.782 | 0.296 | 2.052 | 0.897 | 4.692 | 0.089 |
| Δ SII | <372 vs. ≥372 | 0.340 | 0.103 | 1.127 | 0.078 | 0.352 | 0.106 | 1.170 | 0.089 | 0.636 | 0.277 | 1.457 | 0.284 |
| Pretreatment SIRI | <125 vs. ≥125 | 2.260 | 1.056 | 4.838 | 0.036 | 2.935 | 1.315 | 6.552 | 0.009 | 2.558 | 1.297 | 5.044 | 0.007 |
| Posttreatment SIRI | <124 vs. ≥124 | 0.804 | 0.382 | 1.691 | 0.565 | 0.751 | 0.352 | 1.600 | 0.458 | 0.980 | 0.501 | 1.916 | 0.953 |
| Δ SIRI | <148 vs. ≥148 | 2.299 | 0.970 | 5.449 | 0.059 | 2.435 | 1.021 | 5.805 | 0.045 | 2.451 | 1.108 | 5.425 | 0.027 |
| Induction chemotherapy | No vs. Yes | 1.134 | 0.523 | 2.459 | 0.751 | 1.257 | 0.564 | 2.800 | 0.576 | 0.775 | 0.398 | 1.507 | 0.452 |
| ECOG performance status | 0–1 vs. 2–4 | 1.703 | 0.403 | 7.200 | 0.469 | 1.759 | 0.415 | 7.453 | 0.443 | 2.174 | 0.513 | 9.214 | 0.292 |
| Variables | Dichotomized Units | OS | DSS | DFS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95%CI | p-Value | HR | 95%CI | p-Value | HR | 95%CI | p-Value | |||||
| Posttreatment BMI (kg/m2) | <21.6 vs. ≥21.6 | 0.368 | 0.169 | 0.801 | 0.012 | 0.333 | 0.148 | 0.746 | 0.008 | 0.274 | 0.132 | 0.569 | 0.001 |
| Δ BMI (kg/m2) | <−1.93 vs. ≥−1.93 | 0.268 | 0.118 | 0.609 | 0.002 | ||||||||
| Pretreatment SIRI | <125 vs. ≥125 | 2.841 | 1.256 | 6.429 | 0.012 | 3.541 | 1.717 | 7.304 | 0.001 | ||||
| Disease Persistence/Recurrence (n = 36) | None (n = 25) | p-Value | ||
|---|---|---|---|---|
| Nomogram score | <92.5 | 15 (100%) | 0 (0%) | <0.001 |
| ≥92.5 | 21 (45.65%) | 25 (54.35%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeh, P.; Chang, C.-M.; Liao, L.-J.; Wu, C.-Y.; Hsieh, C.-H.; Shueng, P.-W.; Cheng, P.-W.; Lo, W.-C. Nomogram-Based Prediction of Survival in Stage IV Nasopharyngeal Carcinoma: A Retrospective Single-Center Study. Diagnostics 2025, 15, 1309. https://doi.org/10.3390/diagnostics15111309
Yeh P, Chang C-M, Liao L-J, Wu C-Y, Hsieh C-H, Shueng P-W, Cheng P-W, Lo W-C. Nomogram-Based Prediction of Survival in Stage IV Nasopharyngeal Carcinoma: A Retrospective Single-Center Study. Diagnostics. 2025; 15(11):1309. https://doi.org/10.3390/diagnostics15111309
Chicago/Turabian StyleYeh, Peng, Chih-Ming Chang, Li-Jen Liao, Chia-Yun Wu, Chen-Hsi Hsieh, Pei-Wei Shueng, Po-Wen Cheng, and Wu-Chia Lo. 2025. "Nomogram-Based Prediction of Survival in Stage IV Nasopharyngeal Carcinoma: A Retrospective Single-Center Study" Diagnostics 15, no. 11: 1309. https://doi.org/10.3390/diagnostics15111309
APA StyleYeh, P., Chang, C.-M., Liao, L.-J., Wu, C.-Y., Hsieh, C.-H., Shueng, P.-W., Cheng, P.-W., & Lo, W.-C. (2025). Nomogram-Based Prediction of Survival in Stage IV Nasopharyngeal Carcinoma: A Retrospective Single-Center Study. Diagnostics, 15(11), 1309. https://doi.org/10.3390/diagnostics15111309






