Outcomes and Prognostic Markers in Extracorporeal Cardiopulmonary Resuscitation: 10-Year Experience from a Rural Tertiary Care Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
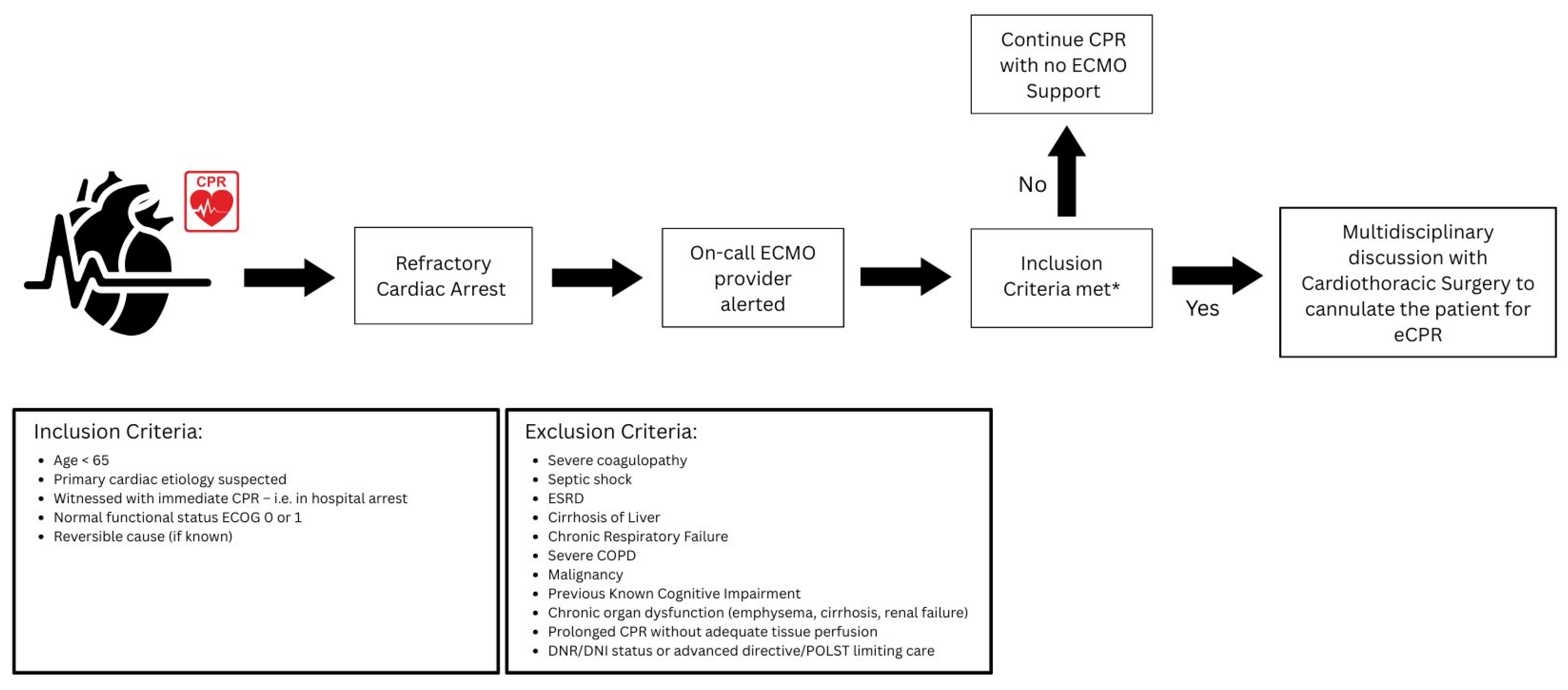
2.2. Patient Selection
2.3. Clinical Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHA | American Heart Association |
| BMI | Body Mass Index |
| CPC | Cerebral Performance Categories |
| eCPR | Extracorporeal Cardiopulmonary Resuscitation |
| ECMO | Extracorporeal Membrane Oxygenation |
| GNO | Good Neurological Outcomes |
| IQR | Interquartile Range |
| MAP | Mean Arterial Pressure |
| PNO | Poor Neurological Outcomes |
| ROSC | Return of Spontaneous Circulation |
References
- Meaney, P.A.; Bobrow, B.J.; Mancini, M.E.; Christenson, J.; de Caen, A.R.; Bhanji, F.; Abella, B.S.; Kleinman, M.E.; Edelson, D.P.; Berg, R.A.; et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation 2013, 128, 417–435, Erratum in Circulation 2013, 128, e120; Erratum in Circulation 2013, 128, e408. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322, Erratum in Circulation 2015, 131, e535; Erratum in Circulation 2016, 133, e417. [Google Scholar] [CrossRef] [PubMed]
- Sonneville, R.; Schmidt, M. Extracorporeal Cardiopulmonary Resuscitation for Adults with Refractory Out-of-Hospital Cardiac Arrest: Towards Better Neurological Outcomes. Circulation 2020, 141, 887–890. [Google Scholar] [CrossRef] [PubMed]
- Shanmugasundaram, M.; Lotun, K. Refractory Out of Hospital Cardiac Arrest. Curr. Cardiol. Rev. 2018, 14, 109–114. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thiagarajan, R.R.; Brogan, T.V.; Scheurer, M.A.; Laussen, P.C.; Rycus, P.T.; Bratton, S.L. Extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in adults. Ann. Thorac. Surg. 2009, 87, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Suverein, M.M.; Delnoij, T.S.R.; Lorusso, R.; Brandon Bravo Bruinsma, G.J.; Otterspoor, L.; Elzo Kraemer, C.V.; Vlaar, A.P.J.; van der Heijden, J.J.; Scholten, E.; den Uil, C.; et al. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2023, 388, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Yannopoulos, D.; Bartos, J.; Raveendran, G.; Walser, E.; Connett, J.; Murray, T.A.; Collins, G.; Zhang, L.; Kalra, R.; Kosmopoulos, M.; et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. Lancet 2020, 396, 1807–1816. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lavonas, E.J.; Akpunonu, P.D.; Arens, A.M.; Babu, K.M.; Cao, D.; Hoffman, R.S.; Hoyte, C.O.; Mazer-Amirshahi, M.E.; Stolbach, A.; St-Onge, M.; et al. 2023 American Heart Association Focused Update on the Management of Patients with Cardiac Arrest or Life-Threatening Toxicity Due to Poisoning: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2023, 148, e149–e184. [Google Scholar] [CrossRef] [PubMed]
- Lorusso, R.; Whitman, G.; Milojevic, M.; Raffa, G.; McMullan, D.M.; Boeken, U.; Haft, J.; Bermudez, C.; Shah, A.; D’Alessandro, D.A. 2020 EACTS/ELSO/STS/AATS expert consensus on post-cardiotomy extracorporeal life support in adult patients. J. Thorac. Cardiovasc. Surg. 2021, 161, 1287–1331. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Cho, Y.H.; Yang, J.H.; Yang, J.H.; Chung, S.; Suh, G.Y.; Sung, K. Impact of age on the outcomes of extracorporeal cardiopulmonary resuscitation: Analysis using inverse probability of treatment weighting. Eur. J. Cardiothorac. Surg. 2021, 60, 1318–1324. [Google Scholar] [CrossRef] [PubMed]
- George, N.; Stephens, K.; Ball, E.; Crandall, C.; Ouchi, K.; Unruh, M.; Kamdar, N.; Myaskovsky, L. Extracorporeal Membrane Oxygenation for Cardiac Arrest: Does Age Matter? Crit. Care Med. 2024, 52, 20–30. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yu, H.Y.; Wang, C.H.; Chi, N.H.; Huang, S.C.; Chou, H.W.; Chou, N.K.; Chen, Y.S. Effect of interplay between age and low-flow duration on neurologic outcomes of extracorporeal cardiopulmonary resuscitation. Intensive Care Med. 2019, 45, 44–54. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bartos, J.A.; Grunau, B.; Carlson, C.; Duval, S.; Ripeckyj, A.; Kalra, R.; Raveendran, G.; John, R.; Conterato, M.; Frascone, R.J.; et al. Improved Survival with Extracorporeal Cardiopulmonary Resuscitation Despite Progressive Metabolic Derangement Associated with Prolonged Resuscitation. Circulation 2020, 141, 877–886. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kosmopoulos, M.; Kalra, R.; Alexy, T.; Gaisendrees, C.; Jaeger, D.; Chahine, J.; Voicu, S.; Tsangaris, A.; Gutierrez, A.B.; Elliott, A.; et al. The impact of BMI on arrest characteristics and survival of patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. Resuscitation 2023, 188, 109842. [Google Scholar] [CrossRef] [PubMed]
- Pai, C.H.; Hsu, J.C.; Lin, L.Y.; Wang, C.H.; Wei, L.Y.; Chi, N.H.; Huang, S.C.; Yu, H.Y.; Chou, N.K.; Hsu, R.B.; et al. Does obesity matter in patients receiving venoarterial extracorporeal membrane oxygenation? The U-shaped relationship between body mass index and mortality after extracorporeal cardiopulmonary resuscitation. Surgery 2025, 178, 108928. [Google Scholar] [CrossRef] [PubMed]
- Beni, C.E.; Rice-Townsend, S.E.; Esangbedo, I.D.; Jancelewicz, T.; Vogel, A.M.; Newton, C.; Boomer, L.; Rothstein, D.H. Outcome of Extracorporeal Cardiopulmonary Resuscitation in Pediatric Patients Without Congenital Cardiac Disease: Extracorporeal Life Support Organization Registry Study. Pediatr. Crit. Care Med. 2023, 24, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.I.; Ko, R.E.; Yang, J.H.; Cho, Y.H.; Ahn, J.; Ryu, J.A. Optimal Mean Arterial Pressure for Favorable Neurological Outcomes in Survivors after Extracorporeal Cardiopulmonary Resuscitation. J. Clin. Med. 2022, 11, 290. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ryu, J.A.; Chung, C.R.; Cho, Y.H.; Sung, K.; Jeon, K.; Suh, G.Y.; Park, T.K.; Lee, J.M.; Song, Y.B.; Hahn, J.Y.; et al. Neurologic Outcomes in Patients Who Undergo Extracorporeal Cardiopulmonary Resuscitation. Ann. Thorac. Surg. 2019, 108, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Debaty, G.; Babaz, V.; Durand, M.; Gaide-Chevronnay, L.; Fournel, E.; Blancher, M.; Bouvaist, H.; Chavanon, O.; Maignan, M.; Bouzat, P.; et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation 2017, 112, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ma, Q.; Zhang, H.; Liu, S.; Zheng, Y. Predictors of survival and neurologic outcome for adults with extracorporeal cardiopulmonary resuscitation: A systemic review and meta-analysis. Medicine 2018, 97, e13257. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Daou, O.; Winiszewski, H.; Besch, G.; Pili-Floury, S.; Belon, F.; Guillon, B.; Marx, T.; Chocron, S.; Capellier, G.; Perrotti, A.; et al. Initial pH and shockable rhythm are associated with favorable neurological outcome in cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. J. Thorac. Dis. 2020, 12, 849–857. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thevathasan, T.; Gregers, E.; Rasalingam Mørk, S.; Degbeon, S.; Linde, L.; Bønding Andreasen, J.; Smerup, M.; Eifer Møller, J.; Hassager, C.; Laugesen, H.; et al. Lactate and lactate clearance as predictors of one-year survival in extracorporeal cardiopulmonary resuscitation—An international, multicentre cohort study. Resuscitation 2024, 198, 110149. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Takayama, W.; Inoue, A.; Hifumi, T.; Sakamoto, T.; Kuroda, Y.; Otomo, Y.; Study of Advanced Life Support for Ventricular Fibrillation with Extracorporeal Circulation in Japan (SAVE-J II) Study Group. Impact of Lactate Clearance on Clinical and Neurological Outcomes of Patients with Out-of-Hospital Cardiac Arrest Treated with Extracorporeal Cardiopulmonary Resuscitation: A Secondary Data Analysis. Crit. Care Med. 2024, 52, e341–e350. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Namjouyan, K.; Mittal, A.; Gajkowski, E.; Carry, B.; Penupolu, S.; Young, A. Prognostic markers in patients who suffered cardiac arrest and underwent extracorporeal cardiopulmonary resuscitation: 10-year experience from a rural tertiary care center. CHEST 2023, 164, A1557. [Google Scholar] [CrossRef]
| Total Patients | 37 |
|---|---|
| Age, Median (IQR) | 58 (48, 65) |
| Male, n (%) | 24 (64.9%) |
| CPC Score | |
| Good Neurological Outcomes (CPC 1 &2) | 9 (24.3%) |
| Poor Neurological Outcomes (CPC 3,4 &5) | 28 (75.7%) |
| Mortality | |||
|---|---|---|---|
| No | Yes | p-Value | |
| (N = 12) | (N = 25) | ||
| Age, Median (IQR) | 46 (35, 53.5) | 61 (51, 72) | <0.01 1 |
| Male, n (%) | 8 (66.7%) | 16 (64.0%) | 0.87 2 |
| Poor Neurological Outcomes (N = 28) | Good Neurological Outcomes (N = 9) | Odds Ratio (95% Cl) | p-Value | |
|---|---|---|---|---|
| Duration of cardiac arrest less than 15 min, n (%) | 5/23 (21.7%) | 4/7 (57.1%) | 4.80 (0.80–28.90) | 0.09 1 |
| Duration of cardiac arrest in minutes, Median (IQR) | 60 (15, 60) | 10 (10, 2) | N/A | 0.01 2 |
| Time on ECMO in days, Median (IQR) | 1.9 (0.5, 7.8) | 4.8 (1.8, 7.9) | N/A | 0.35 2 |
| Mortality | Age Adjusted | ||||||
|---|---|---|---|---|---|---|---|
| Total | No | Yes | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| (N = 37) | (N = 9) | (N = 28) | |||||
| Non-shockable rhythm, n (%) | 18 (50.0%) | 2 (22.2%) | 16 (59.3%) | 5.09 (0.89–29.26) | 0.07 1 | 3.79 (0.60–23.75) | 0.07 1 |
| Missing | 1 | 0 | 1 | ||||
| Obese, n (%) | 25 (67.6%) | 3 (33.3%) | 22 (78.6%) | 7.33 (1.40–38.33) | 0.02 1 | 12.13 (1.57–93.46) | 0.02 1 |
| MAP in first 6 h, Median (IQR) | 62.5 (54.0, 70.0) | 70 (65, 80) | 60 (50, 65) | <0.02 2 | |||
| Missing | 1 | 0 | 1 | ||||
| MAP in first 6 h < 65, n (%) | 20 (55.6%) | 0 (0.0%) | 20 (74.1%) | N/A | <0.01 1 | N/A | 0.93 1 |
| Missing | 1 | 0 | 1 | ||||
| Peak lactate in 24 h, Median (IQR) | 9.2 (6.5, 14.0) | 6.9 (3.6, 9.0) | 11.2 (7.2, 14.7) | 0.06 2 | |||
| Missing | 4 | 0 | 4 | ||||
| Peak lactate in 24 h > 10, n (%) | 16 (48.5%) | 2 (22.2%) | 14 (58.3%) | 4.90 (0.84–28.72) | 0.08 1 | 6.97 (0.91–53.52) | 0.06 1 |
| Missing | 4 | 0 | 4 | ||||
| Need for RRT, n (%) | 16 (47.1%) | 4 (44.4%) | 12 (48.0%) | 1.15 (0.25–5.34) | 0.80 1 | 1.19 (0.23–6.26) | 0.84 1 |
| Missing | 3 | 0 | 3 | ||||
| Blood transfusion, Median (IQR) | 6 (0, 16) | 6 (5, 17) | 6 (0, 16) | 0.55 2 | |||
| Blood transfusion > 10, n (%) | 13 (35.1%) | 3 (33.3%) | 10 (35.7%) | 1.11 (0.23–5.43) | 0.90 1 | 0.84 (0.15–4.81) | 0.85 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Namjouyan, K.; Mittal, A.; Gajkowski, E.; Young, A.; Penupolu, S.; Carry, B. Outcomes and Prognostic Markers in Extracorporeal Cardiopulmonary Resuscitation: 10-Year Experience from a Rural Tertiary Care Center. Diagnostics 2025, 15, 1275. https://doi.org/10.3390/diagnostics15101275
Namjouyan K, Mittal A, Gajkowski E, Young A, Penupolu S, Carry B. Outcomes and Prognostic Markers in Extracorporeal Cardiopulmonary Resuscitation: 10-Year Experience from a Rural Tertiary Care Center. Diagnostics. 2025; 15(10):1275. https://doi.org/10.3390/diagnostics15101275
Chicago/Turabian StyleNamjouyan, Kamran, Aastha Mittal, Evan Gajkowski, Amanda Young, Sudheer Penupolu, and Brendan Carry. 2025. "Outcomes and Prognostic Markers in Extracorporeal Cardiopulmonary Resuscitation: 10-Year Experience from a Rural Tertiary Care Center" Diagnostics 15, no. 10: 1275. https://doi.org/10.3390/diagnostics15101275
APA StyleNamjouyan, K., Mittal, A., Gajkowski, E., Young, A., Penupolu, S., & Carry, B. (2025). Outcomes and Prognostic Markers in Extracorporeal Cardiopulmonary Resuscitation: 10-Year Experience from a Rural Tertiary Care Center. Diagnostics, 15(10), 1275. https://doi.org/10.3390/diagnostics15101275






