Incidental Calcifications of Carotid and Vertebral Arteries: Frequency and Associations in Pediatric Population
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bartstra, J.W.; van den Beukel, T.C.; Van Hecke, W.; Mali, W.P.T.M.; Spiering, W.; Koek, H.L.; Hendrikse, J.; de Jong, P.A.; den Harder, A.M. Intracranial Arterial Calcification: Prevalence, Risk Factors, and Consequences: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2020, 76, 1595–1604. [Google Scholar] [CrossRef] [PubMed]
- Olatunji, R.B.; Adekanmi, A.J.; Ogunseyinde, A.O. Intracranial Arterial Calcification in Black Africans with Acute Ischaemic Stroke. Cerebrovasc. Dis. Extra 2018, 8, 26–38. [Google Scholar] [CrossRef]
- Bos, D.; Portegies, M.L.; van der Lugt, A.; Bos, M.J.; Koudstaal, P.J.; Hofman, A.; Krestin, G.P.; Franco, O.H.; Vernooij, M.W.; Ikram, M.A. Intracranial carotid artery atherosclerosis and the risk of stroke in whites: The Rotterdam Study. JAMA Neurol. 2014, 71, 405–411. [Google Scholar] [CrossRef]
- Kamphuis, M.J.; van der Kamp, L.T.; Lette, E.; Rinkel, G.J.E.; Vergouwen, M.D.I.; van der Schaaf, I.C.; de Jong, P.A.; Ruigrok, Y.M. Intracranial arterial calcification in patients with unruptured and ruptured intracranial aneurysms. Eur. Radiol. 2024, 34, 7517–7525. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.; Lee, K.B.; Roh, H.; Ahn, M.Y.; Bae, H.J.; Lee, J.S.; Woo, H.Y.; Hwang, H.W. Intracranial arterial calcification can predict early vascular events after acute ischemic stroke. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2014, 23, e331–e337. [Google Scholar] [CrossRef] [PubMed]
- Cereda, A.; Franchina, A.G.; Tua, L.; Rocchetti, M.; Garattini, D.; D’Elia, E.; Lucreziotti, S. Coronary artery calcification as an incremental predictive risk: Research perspectives in primary prevention. J. Cardiol. 2025; advance online publication. [Google Scholar] [CrossRef]
- Hussein, H.M.; Zacharatos, H.; Cordina, S.; Lakshminarayan, K.; Ezzeddine, M.A. Intracranial vascular calcification is protective from vasospasm after aneurysmal subarachnoid hemorrhage. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2014, 23, 2687–2693. [Google Scholar] [CrossRef]
- Park, K.Y.; Chung, P.W.; Kim, Y.B.; Moon, H.S.; Suh, B.C.; Yoon, W.T. Increased pulsatility index is associated with intracranial arterial calcification. Eur. Neurol. 2013, 69, 83–88. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Mera, R.M.; Atahualpa Project Investigators. The Role of Brachial Pulse Pressure as an Indicator of Intracranial Atherosclerosis: The Atahualpa Project. High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2017, 24, 419–424. [Google Scholar] [CrossRef]
- Gotovac, N.; Išgum, I.; Viergever, M.A.; Biessels, G.J.; Fajdić, J.; Velthuis, B.K.; Prokop, M. Calcium at the carotid siphon as an indicator of internal carotid artery stenosis. Eur. Radiol. 2013, 23, 1478–1486. [Google Scholar] [CrossRef]
- Baradaran, H.; Patel, P.; Gialdini, G.; Giambrone, A.; Lerario, M.P.; Navi, B.B.; Min, J.K.; Iadecola, C.; Kamel, H.; Gupta, A. Association between Intracranial Atherosclerotic Calcium Burden and Angiographic Luminal Stenosis Measurements. AJNR. Am. J. Neuroradiol. 2017, 38, 1723–1729. [Google Scholar] [CrossRef]
- Vos, A.; Kockelkoren, R.; de Vis, J.B.; van der Schouw, Y.T.; van der Schaaf, I.C.; Velthuis, B.K.; Mali, W.P.T.M.; de Jong, P.A.; DUST study group. Risk factors for atherosclerotic and medial arterial calcification of the intracranial internal carotid artery. Atherosclerosis 2018, 276, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Sanders-Taylor, C.; Kurbanov, A.; Cebula, H.; Leach, J.L.; Zuccarello, M.; Keller, J.T. The carotid siphon: A historic radiographic sign, not an anatomic classification. World Neurosurg. 2014, 82, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Koch, B.; Blackham, A.; Jones, B. Incidental internal carotid artery calcifications on temporal bone CT in children. Pediatr. Radiol. 2007, 37, 141–144. [Google Scholar] [CrossRef]
- Kobylinski, S. Häufigkeit und Lokalisation der Arterienverkalkungen im Kindesalter [Frequency and localisation of arterial calcifications during childhood (author’s transl)]. Zentralblatt Allg. Pathol. u. Pathol. Anat. 1974, 118, 196–202. [Google Scholar]
- Meyer, W.W.; Lind, J. Calcifications of the carotid siphon—A common finding in infancy and childhood. Arch. Dis. Child. 1972, 47, 355–363. [Google Scholar] [CrossRef]
- Wu, X.H.; Chen, X.Y.; Wang, L.J.; Wong, K.S. Intracranial Artery Calcification and Its Clinical Significance. J. Clin. Neurol. 2016, 12, 253–261. [Google Scholar] [CrossRef]
- Mak, H.K.; Wong, C.W.; Yau, K.K.; Wong, W.M.; Gu, J.; Khong, P.L.; Chan, B.P. Computed tomography evaluation of intracranial atherosclerosis in Chinese patients with transient ischemic attack or minor ischemic stroke—Its distribution and association with vascular risk factors. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2009, 18, 158–163. [Google Scholar] [CrossRef]
- Livingston, J.H.; Stivaros, S.; Warren, D.; Crow, Y.J. Intracranial calcification in childhood: A review of aetiologies and recognizable phenotypes. Dev. Med. Child Neurol. 2014, 56, 612–626. [Google Scholar] [CrossRef]
- Bergevin, M.A.; Daugherty, C.C.; Bove, K.E.; McAdams, A.J. The internal carotid artery siphon in children and adolescents. Hum. Pathol. 1991, 22, 603–606. [Google Scholar] [CrossRef]
- Ahmed, M.; McPherson, R.; Abruzzo, A.; Thomas, S.E.; Gorantla, V.R. Carotid Artery Calcification: What We Know So Far. Cureus 2021, 13, e18938. [Google Scholar] [CrossRef]
- Agacayak, K.S.; Guler, R.; Sezgin Karatas, P. Relation Between the Incidence of Carotid Artery Calcification and Systemic Diseases. Clin. Interv. Aging 2020, 15, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Gao, J.; Lv, Q.; Cai, H.; Wang, F.; Ye, R.; Liu, X. Calcification in Atherosclerotic Plaque Vulnerability: Friend or Foe? Front. Physiol. 2020, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, F.G.; Caschera, L.; Teixeira, S.R.; Viaene, A.N.; Pinelli, L.; Mankad, K.; Alves, C.A.P.F.; Ortiz-Gonzalez, X.R.; Andronikou, S.; Vossough, A. Intracranial calcifications in childhood: Part 2. Pediatr. Radiol. 2020, 50, 1448–1475. [Google Scholar] [CrossRef]
- Ptak, T.; Hunter, G.H.; Avakian, R.; Novelline, R.A. Clinical significance of cavernous carotid calcifications encountered on head computed tomography scans performed on patients seen in the emergency department. J. Comput. Assist. Tomogr. 2003, 27, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Katada, K.; Kanno, T.; Sano, H.; Shinomiya, Y.; Koga, S. Calcification of the vertebral artery. Am. J. Neuroradiol. 1983, 4, 450–453. [Google Scholar] [CrossRef]
- Peters, M.E.M.; de Brouwer, E.J.M.; Bartstra, J.W.; Mali, W.P.T.M.; Koek, H.L.; Rozemuller, A.J.M.; Baas, A.F.; de Jong, P.A. Mechanisms of calcification in Fahr disease and exposure of potential therapeutic targets. Neurol. Clin. Pract. 2020, 10, 449–457. [Google Scholar] [CrossRef]
- Naylor, R.; Rantner, B.; Ancetti, S.; de Borst, G.J.; De Carlo, M.; Halliday, A.; Kakkos, S.K.; Markus, H.S.; McCabe, D.J.H.; Sillesen, H.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2023 Clinical Practice Guidelines on the Management of Atherosclerotic Carotid and Vertebral Artery Disease. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2023, 65, 7–111. [Google Scholar] [CrossRef]
- Kantarcı, M.; Aydın, S.; Oğul, H.; Kızılgöz, V. New imaging techniques and trends in radiology. Diagn. Interv. Radiol. 2025; advance online publication. [Google Scholar] [CrossRef]




| Number and Percentage of Patients | ||
|---|---|---|
| Category 0 | No evidence of calcification | 201 (67%) |
| Category 1 | Unilateral suspicious calcification focus | 28 (9.3%) |
| Category 2 | Prominent calcifications on one or more images, ranging from a single hyperdense focal point to peripheral areas of calcification | 47 (15.6%) |
| Category 3 | Prominent foci of calcification in bilateral ICA or vertebral arteries | 24 (8.1%) |
| Intracranial Calcification | Etiologies | Anatomic Location/Calcification Pattern |
|---|---|---|
| Physiologic/Age-Related Intracranial Calcifications | Pineal gland, choroid plexus, falx cerebri, tentorium cerebelli, basal ganglia | |
| Genetic Syndromes/Developmental Disorders | Sturge–Weber syndrome | Gyriform design with twin lines; similar to a tram track |
| Tuberous sclerosis | Tubers that are subcortical and subependymal along the atrium and caudothalamic groove | |
| Neurofibromatosis | Choroid plexus calcifications in the latteral ventricles and cerebellar nodular calcifications | |
| Cockayne syndrome | Bilateral prominent or punctate calcifications at the level of the basal ganglia | |
| Krabbe disease | Corona radiata and internal capsule | |
| Pseudo-TORCH syndromes | Cortical bands, as well as in the thalamus, pons, and cerebellum | |
| Hyperphenylalaninemia | Basal ganglia | |
| Von Hippel–Lindau syndrome | Endolymphatic sac tumor | |
| Mitochondrial disorders | Dispersed or punctate in the thalamus and basal ganglia | |
| Fahr disease | Caudate, putamen, globus pallidus, thalamus, deep cortex, and dentate are all symmetrically involved | |
| Congenital Infection | Cytomegalovirus | The basal ganglia have mild punctate calcifications, and the periventricular region has thick, chunky calcifications |
| Herpes | Dispersed | |
| Toxoplasmosis | Nodular calcification is seen in the periventricular and cortical regions Curvilinear calcification is seen in the thalamus and basal ganglia | |
| Rubella | The periventricular region and basal ganglia | |
| Zika | Subcortical punctate calcifications | |
| Human Immunodeficiency Virus | Subcortical tissue and basal ganglia | |
| Acquired Infection | Neurocysticercosis | Calcific nodule within a calcified cyst |
| Mycobacterium tuberculosis | Central calcific tuberculomas | |
| Cryptococcus neoformans | Parenchymal and leptomeningeal punctate calcifications | |
| Vascular Malformations | Arteriovenous malformation | Punctate or curvilinear calcifications may be present |
| Cavernous malformation | Amorphous/punctate calcifications | |
| Developmental venous anomaly | Dystrophic calcifications | |
| Intra-Axial Neoplastic | Pilocytic Astrocytoma | Extensive calcification rarely occurs |
| Oligodendroglioma | Nodular and grouped | |
| Ganglioglioma | Calcific mural nodules | |
| Medulloblastoma | Dispersed foci or grouped | |
| Extra-Axial Neoplastic | Meningioma | Spherical and rim |
| Craniopharyngioma | Thin and peripheral | |
| Germ cell tumors | Heterogeneous | |
| Lipoma | Eggshell calcifications | |
| Intraventricular | Ependymoma | Point or mass-like |
| Central neurocytoma | Variable, ranging from small punctate foci to large calcifications | |
| Metabolic/Endocrine | Hypoparathyroidism | Basal ganglia |
| Inflammatory | Systemic lupus erythematosus | Most common in the cerebellum |
| Sarcoidosis | Cerebellum, hypothalamus, and suprasellar regions |
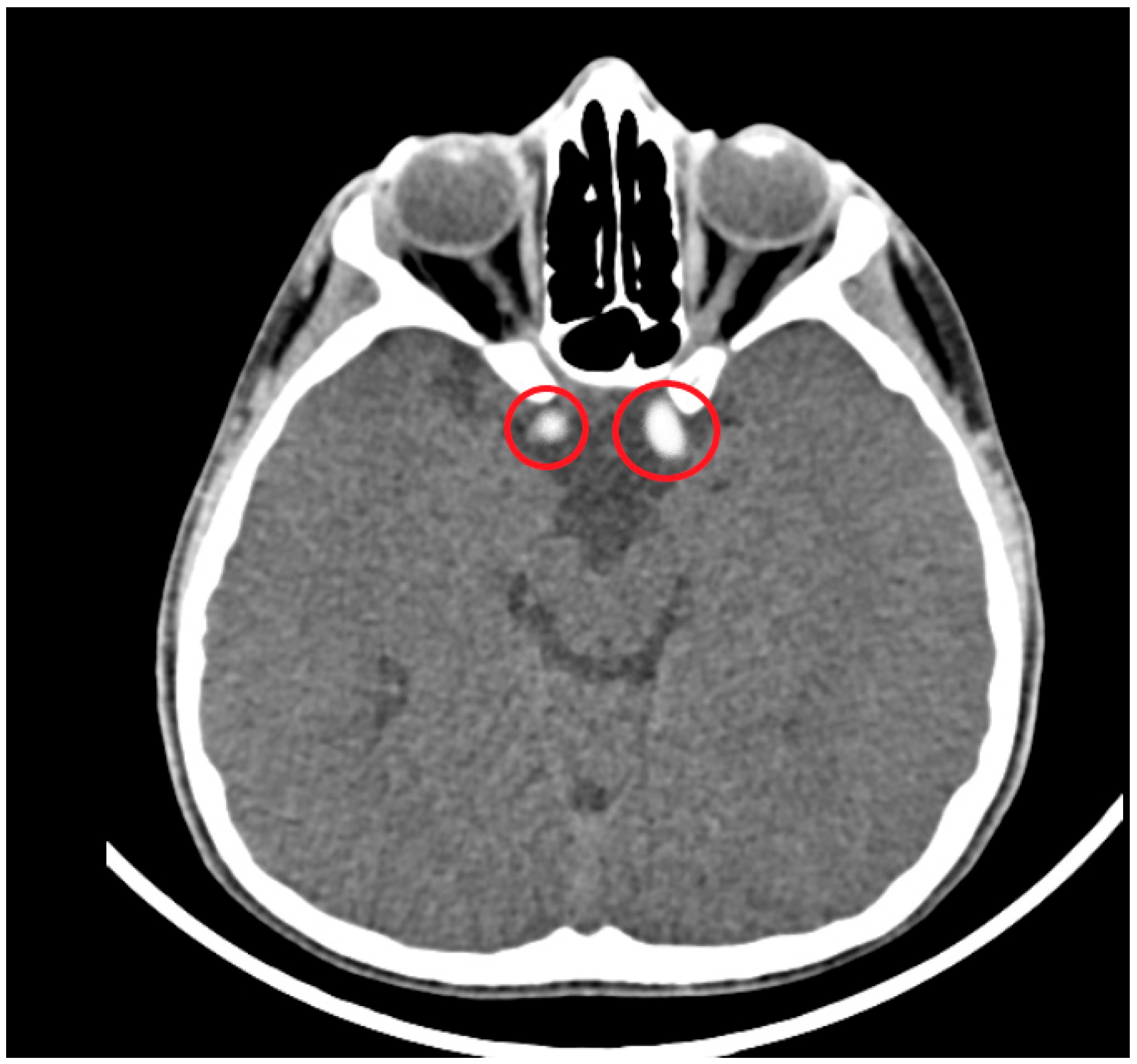
| Cervical | Petrous | Lacerum | Carotid Siphon | Supraclinoid | |
|---|---|---|---|---|---|
| ICA Calcifications | 7 (2.3%) | 7 (2.3%) | 6 (2%) | 31 (10.3%) | 31 (10.3%) |
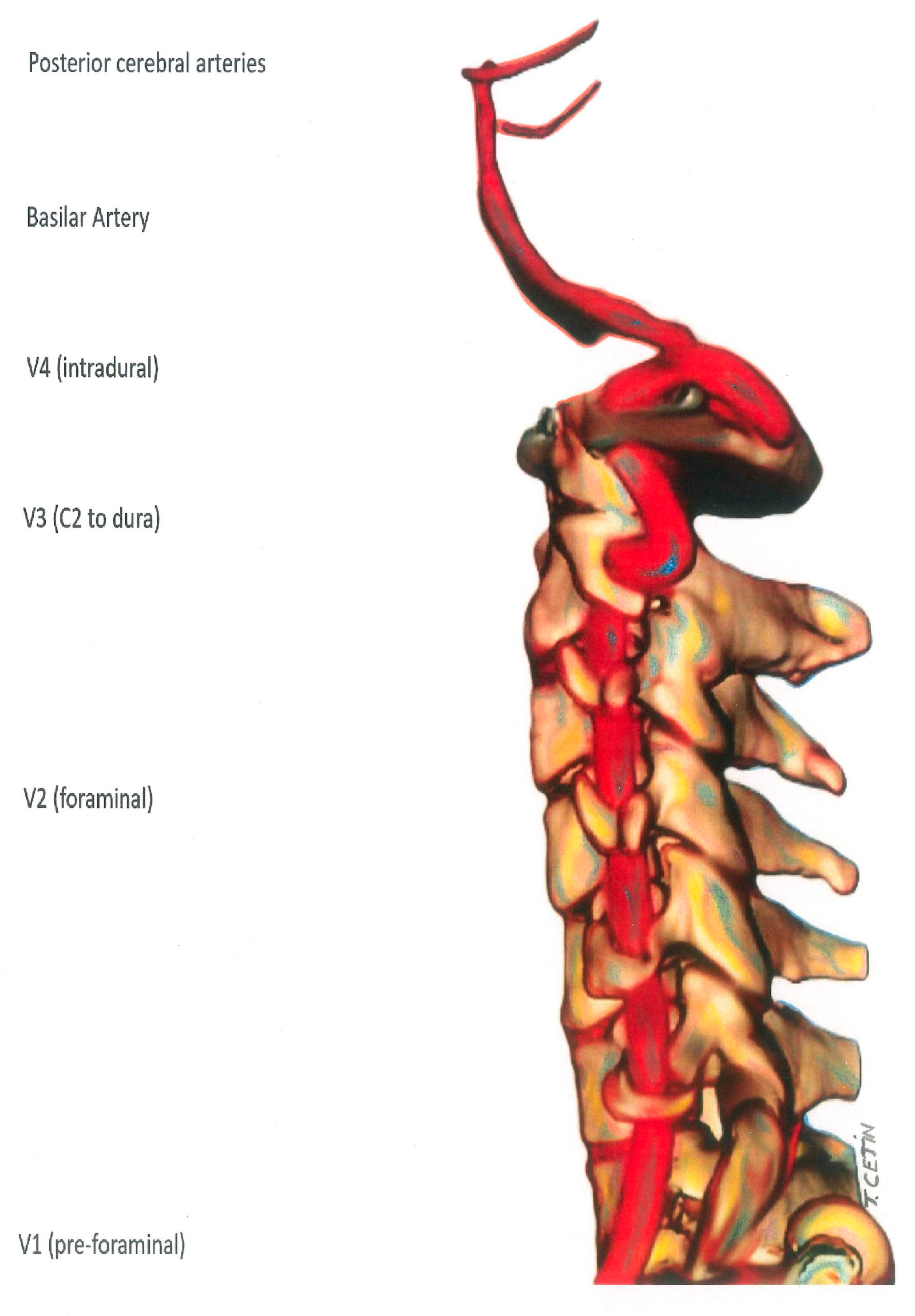
| V1 | V2 | V3 | V4 | |
|---|---|---|---|---|
| Vertebral Artery Calcifications | 1 (0.33%) | 1 (0.33%) | 0 | 15 (5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cetin, T.; Cinar, G.; Ucan, B.; Memis, F.; Irgul, B.; Aydin, S. Incidental Calcifications of Carotid and Vertebral Arteries: Frequency and Associations in Pediatric Population. Diagnostics 2025, 15, 1263. https://doi.org/10.3390/diagnostics15101263
Cetin T, Cinar G, Ucan B, Memis F, Irgul B, Aydin S. Incidental Calcifications of Carotid and Vertebral Arteries: Frequency and Associations in Pediatric Population. Diagnostics. 2025; 15(10):1263. https://doi.org/10.3390/diagnostics15101263
Chicago/Turabian StyleCetin, Turkhun, Gokce Cinar, Berna Ucan, Fulya Memis, Baris Irgul, and Sonay Aydin. 2025. "Incidental Calcifications of Carotid and Vertebral Arteries: Frequency and Associations in Pediatric Population" Diagnostics 15, no. 10: 1263. https://doi.org/10.3390/diagnostics15101263
APA StyleCetin, T., Cinar, G., Ucan, B., Memis, F., Irgul, B., & Aydin, S. (2025). Incidental Calcifications of Carotid and Vertebral Arteries: Frequency and Associations in Pediatric Population. Diagnostics, 15(10), 1263. https://doi.org/10.3390/diagnostics15101263






