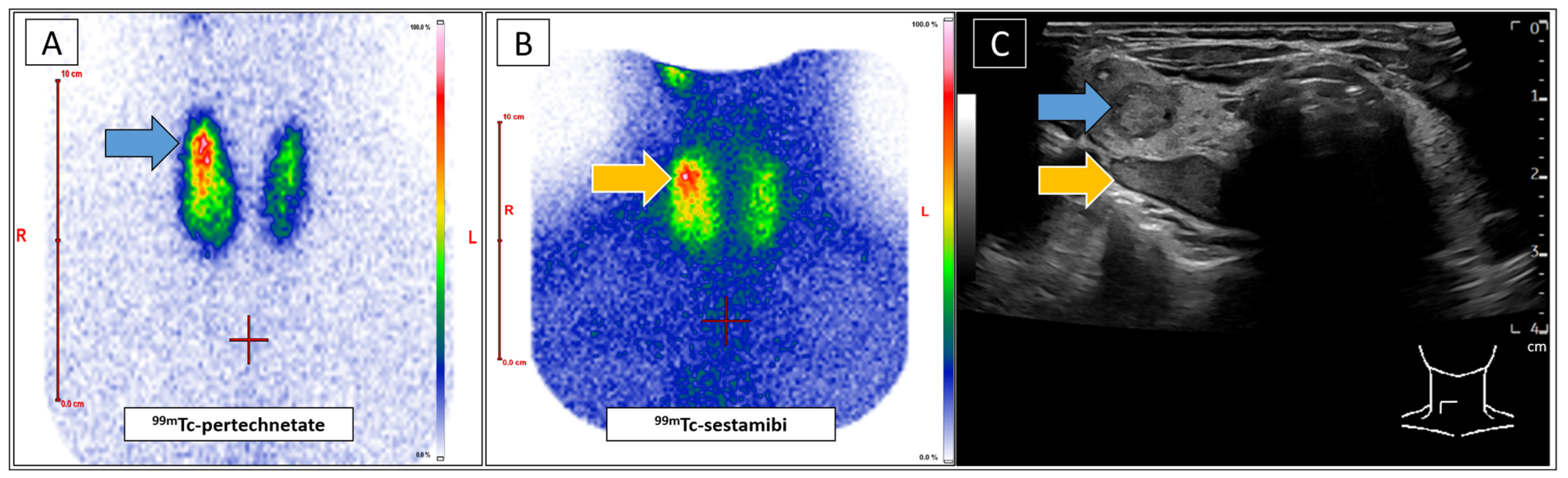
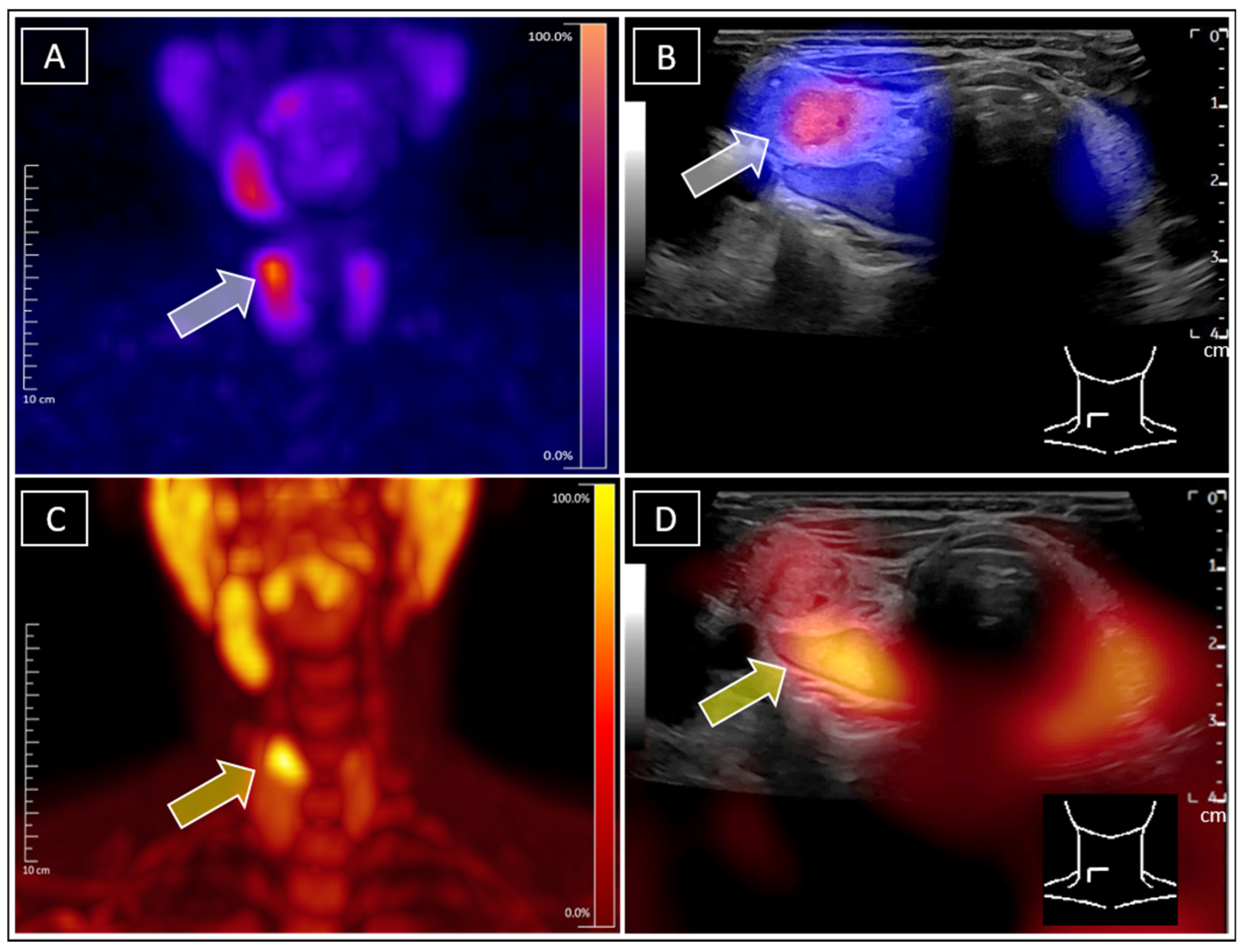
Simultaneous Identification of Tc-99m-Sestamibi-Positive Autonomous Thyroid Adenoma and Adjacent F-18-Ethylcholine-Positive Parathyroid Adenoma in Patient with Graves’ Disease Using Real-Time Ultrasound Fusion Imaging
Abstract
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hindie, E.; Ugur, O.; Fuster, D.; Odoherty, M.; Grassetto, G.; Urena, P.; Kettle, A.; Gulec, S.A.; Pons, F.; Rubello, D. 2009 EANM parathyroid guidelines. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 1201–1216. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Hanley, D.A.; Rizzoli, R.; Bollerslev, J.; Young, J.; Rejnmark, L.; Thakker, R.; Damour, P.; Paul, T.; Van Uum, S.; et al. Primary hyperparathyroidism: Review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int. 2017, 28, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Schweighofer-Zwink, G.; Hehenwarter, L.; Rendl, G.; Rettenbacher, L.; Langsteger, W.; Beheshti, M.; Pirich, C. Imaging of parathyroid adenomas with F-18 choline PET-CT. Wien. Med. Wochenschr. 2019, 169, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Leder, T.; Seifert, P.; Drescher, R.; Gühne, F.; Freesmeyer, M. Excellent Response to Multimodal Therapy Approach in Hyperfunctioning Metastatic Follicular Thyroid Carcinoma Diagnosed on 123 I-SPECT/Ultrasound Fusion Imaging. Clin. Nucl. Med. 2023, 48, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Bluemel, C.; Kirchner, P.; Kajdi, G.W.; Werner, R.A.; Herrmann, K. Localization of Parathyroid Adenoma With Real-Time Ultrasound: Freehand SPECT Fusion. Clin. Nucl. Med. 2016, 41, e141–e142. [Google Scholar] [CrossRef] [PubMed]
- Bluemel, C.; Safak, G.; Cramer, A.; Wöckel, A.; Gesierich, A.; Hartmann, E.; Schmid, J.-S.; Kaiser, F.; Buck, A.K.; Herrmann, K. Fusion of freehand SPECT and ultrasound: First experience in preoperative localization of sentinel lymph nodes. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 2304–2312. [Google Scholar] [CrossRef] [PubMed]
- de Bree, R.; Pouw, B.; Heuveling, D.A.; Castelijns, J. Fusion of Freehand SPECT and Ultrasound to Perform Ultrasound-Guided Fine-Needle Aspiration Cytology of Sentinel Nodes in Head and Neck Cancer. AJNR Am. J. Neuroradiol. 2015, 36, 2153–2158. [Google Scholar] [CrossRef] [PubMed]
- Okur, A.; Hennersperger, C.; Runyan, B.; Gardiazabal, J.; Keicher, M.; Paepke, S.; Wendler, T.; Navab, N. FhSPECT-US guided needle biopsy of sentinel lymph nodes in the axilla: Is it feasible? Med. Image Comput. Comput. Assist. Interv. 2014, 17, 577–584. [Google Scholar] [PubMed]
- Giovanella, L.; Campenni, A.; Tuncel, M.; Ovcaricek, P.P. Integrated Diagnostics of Thyroid Nodules. Cancers 2024, 16, 311. [Google Scholar] [CrossRef] [PubMed]
- Hoang, T.D.; Jani, A.G.; Mai, V.Q.; Tuamokumo, F.O.; Shakir, M.K. Associations of Serum Ionized Calcium, Phosphate, and Pth Levels with Parathyroid Scan in Primary Hyperparathyroidism. Endocr. Pract. 2019, 25, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Krcalova, E.; Horacek, J.; Novakova, E.; Cvejn, M.; Lazarakova, D.; Mikulecky, R.; Maslo, J.; Cepkova, J.; Tilser, J.; Dolezal, J. Dual Tracer 99mTc-Pertechnetate/99mTc-MIBI Dual-Time-Point SPECT/CT Parathyroid Gland Assessment Regarding to Parathyroid Gland Size and Biochemical Parameters–Two Years Single Imaging Centre Experience. Acta Med. 2019, 62, 1–5. [Google Scholar]
- Westerdahl, J.; Bergenfelz, A. Sestamibi scan-directed parathyroid surgery: Potentially high failure rate without measurement of intraoperative parathyroid hormone. World J. Surg. 2004, 28, 1132–1138. [Google Scholar] [CrossRef] [PubMed]
- Fakhran, S.; Branstetter, B.F.; Pryma, D.A. Parathyroid imaging. Neuroimaging Clin. N. Am. 2008, 18, 537–549. [Google Scholar] [CrossRef] [PubMed]
- Zielke, A.; Smaxwil, C.A. Current approach in cases of persistence and recurrence of primary hyperparathyroidism. Chirurgie 2023, 94, 595–601. [Google Scholar] [CrossRef]
- de Koekkoek-Doll, P.K.; Maas, M.; Vogel, W.; Castelijns, J.; Smit, L.; Zavrakidis, I.; Beets-Tan, R.; Brekel, M.V.D. Real-Time Ultrasound Image Fusion with FDG-PET/CT to Perform Fused Image-Guided Fine-Needle Aspiration in Neck Nodes: Feasibility and Diagnostic Value. AJNR Am. J. Neuroradiol. 2021, 42, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Winkens, T.; Seifert, P.; Hollenbach, C.; Kühnel, C.; Gühne, F.; Freesmeyer, M. The FUSION iENA Study: Comparison of I-124-PET/US Fusion Imaging with Conventional Diagnostics for the Functional Assessment of Thyroid Nodules by Multiple Observers. Nuklearmedizin 2019, 58, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Gühne, F.; Mothes, H.; Freesmeyer, M. Allocation of parathyroid adenoma and suspicious thyroid nodule by real-time (99m)Tc-MIBI SPECT/US fusion imaging. Endocrine 2016, 54, 560–561. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leder, T.; Seifert, P.; Gühne, F.; Freesmeyer, M. Simultaneous Identification of Tc-99m-Sestamibi-Positive Autonomous Thyroid Adenoma and Adjacent F-18-Ethylcholine-Positive Parathyroid Adenoma in Patient with Graves’ Disease Using Real-Time Ultrasound Fusion Imaging. Diagnostics 2025, 15, 1262. https://doi.org/10.3390/diagnostics15101262
Leder T, Seifert P, Gühne F, Freesmeyer M. Simultaneous Identification of Tc-99m-Sestamibi-Positive Autonomous Thyroid Adenoma and Adjacent F-18-Ethylcholine-Positive Parathyroid Adenoma in Patient with Graves’ Disease Using Real-Time Ultrasound Fusion Imaging. Diagnostics. 2025; 15(10):1262. https://doi.org/10.3390/diagnostics15101262
Chicago/Turabian StyleLeder, Theresa, Philipp Seifert, Falk Gühne, and Martin Freesmeyer. 2025. "Simultaneous Identification of Tc-99m-Sestamibi-Positive Autonomous Thyroid Adenoma and Adjacent F-18-Ethylcholine-Positive Parathyroid Adenoma in Patient with Graves’ Disease Using Real-Time Ultrasound Fusion Imaging" Diagnostics 15, no. 10: 1262. https://doi.org/10.3390/diagnostics15101262
APA StyleLeder, T., Seifert, P., Gühne, F., & Freesmeyer, M. (2025). Simultaneous Identification of Tc-99m-Sestamibi-Positive Autonomous Thyroid Adenoma and Adjacent F-18-Ethylcholine-Positive Parathyroid Adenoma in Patient with Graves’ Disease Using Real-Time Ultrasound Fusion Imaging. Diagnostics, 15(10), 1262. https://doi.org/10.3390/diagnostics15101262





