Reliability and Radiographic Correlation of the Foot Posture Index-6: A Multi-Rater Analysis in Symptomatic and Asymptomatic Individuals
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. FPI-6 Measurements
2.3. Radiographic Measurements
2.4. Statistical Analysis
3. Results
3.1. Demographic Data
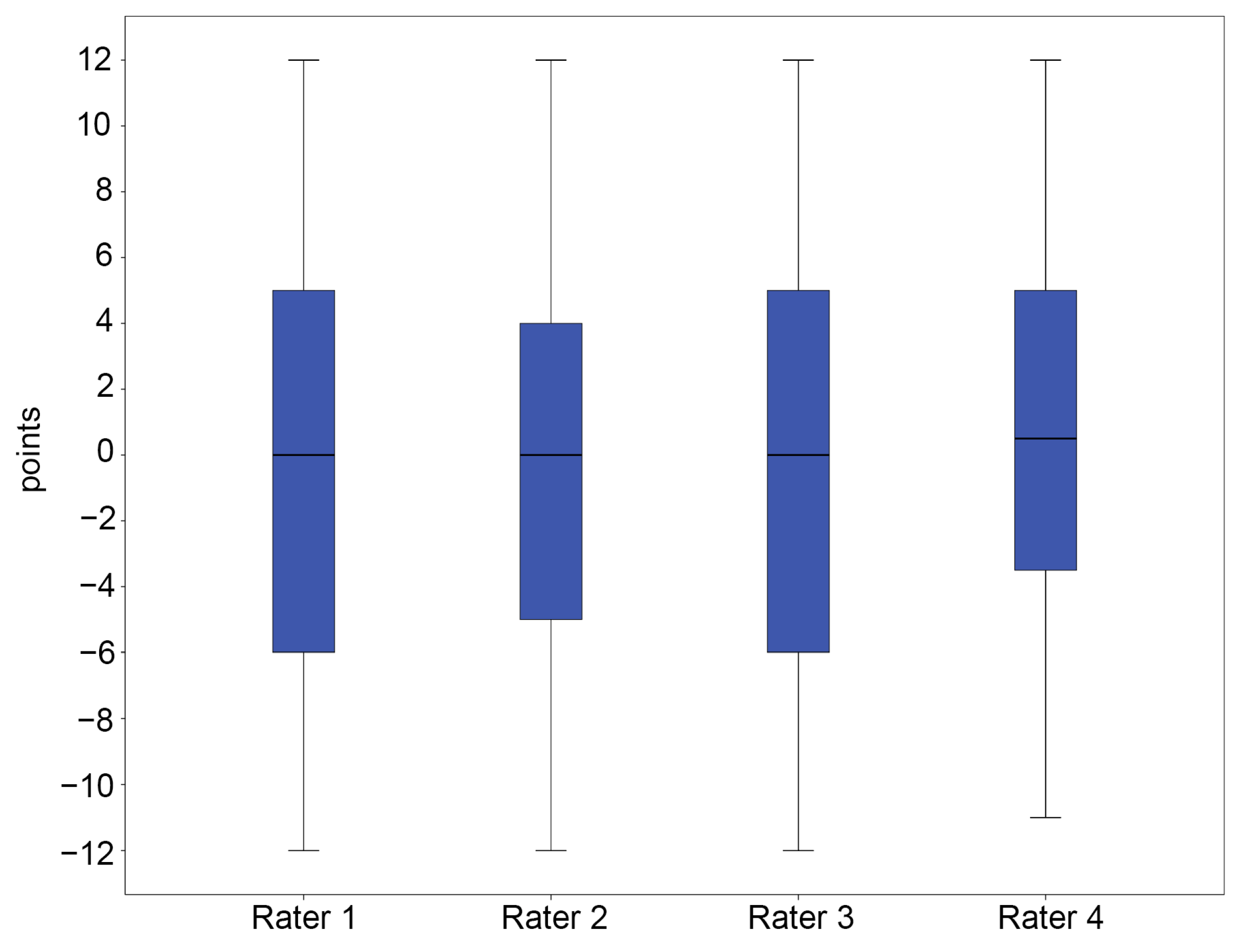
3.2. Reliability of the FPI-6
3.3. Results of the Radiographic Measurements
3.4. Correlation Between FPI-6 Scores and Radiographic Measurements
3.5. Distribution of the FPI-6 Scores According to Foot Pathology in Group B
4. Discussion
5. Limitations and Future Work
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FPI | foot posture index |
| OA | osteoarthritis |
| RA | rheumatoid foot arthritis |
| HV | hallux valgus |
| TCA | talocalcaneal angle |
| AP | anteroposterior |
| TNCA | talonavicular coverage angle |
| TMA | talo-first metatarsal angle |
| HAA | hindfoot alignment angle |
| CPA | calcaneal pitch angle |
| MA | Meary’s angle |
| ICC | intraclass correlation coefficient |
| CI | confidence interval |
References
- Barton, C.J.; Levinger, P.; Crossley, K.M.; Webster, K.E.; Menz, H.B. Relationships between the Foot Posture Index and foot kinematics during gait in individuals with and without patellofemoral pain syndrome. J. Foot Ankle Res. 2011, 4, 10. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.M.; Copper, A.W.; Scharfbillig, R.W.; Scutter, S.D.; Williams, M.T. Reliability of the Foot Posture Index and Traditional Measures of Foot Position. J. Am. Podiatr. Assoc. 2003, 93, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Redmond, A.C.; Crosbie, J.; Ouvrier, R.A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Teyhen, D.S.; Stoltenberg, B.E.; Eckard, T.G.; Doyle, P.M.; Boland, D.M.; Feldtmann, J.J.; McPoil, T.G.; Christie, D.S.; Molloy, J.M.; Goffar, S.L. Static foot posture associated with dynamic plantar pressure parameters. J. Orthop. Sports Phys. Ther. 2011, 41, 100–107. [Google Scholar] [CrossRef]
- Keenan, A.M.; Redmond, A.C.; Horton, M.; Conaghan, P.G.; Tennant, A. The Foot Posture Index: Rasch analysis of a novel, foot-specific outcome measure. Arch. Phys. Med. Rehabil. 2007, 88, 88–93. [Google Scholar] [CrossRef]
- Yates, B.; White, S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am. J. Sports Med. 2004, 32, 772–780. [Google Scholar] [CrossRef]
- Nubé, V.L.; Molyneaux, L.; Yue, D.K. Biomechanical Risk Factors Associated with Neuropathic Ulceration of the Hallux in People with Diabetes Mellitus. J. Am. Podiatr. Assoc. 2006, 96, 189–197. [Google Scholar] [CrossRef]
- Cornwall, M.W.; McPoil, T.G. Relationship between static foot posture and foot mobility. J. Foot Ankle Res. 2011, 4, 4. [Google Scholar] [CrossRef]
- Buldt, A.K.; Murley, G.S.; Levinger, P.; Menz, H.B.; Nester, C.J.; Landorf, K.B. Are clinical measures of foot posture and mobility associated with foot kinematics when walking? J. Foot Ankle Res. 2015, 8, 63. [Google Scholar] [CrossRef]
- Terada, M.; Wittwer, A.M.; Gribble, P.A. Intra-rater and inter-rater reliability of the five image-based criteria of the foot posture index-6. Int. J. Sports Phys. Ther. 2014, 9, 187–194. [Google Scholar]
- Cornwall, M.W.; McPoil, T.G.; Lebec, M.; Vicenzino, B.; Wilson, J. Reliability of the Modified Foot Posture Index. J. Am. Podiatr. Assoc. 2008, 98, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.D.; Kim, Y.M.; Kim, K.; Choi, M.S.; Lee, H.J. Reliability of the Foot Posture Index (FPI-6) for Assessment of Stroke Patients. J. Kor Phys. Ther. 2015, 27, 311–314. [Google Scholar] [CrossRef]
- Menz, H.B.; Munteanu, S.E. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J. Orthop. Sports Phys. Ther. 2005, 35, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Morrison, S.C.; Ferrari, J. Inter-rater reliability of the Foot Posture Index (FPI-6) in the assessment of the paediatric foot. J. Foot Ankle Res. 2009, 2, 26. [Google Scholar] [CrossRef]
- Lee, J.S.; Kim, K.B.; Jeong, J.O.; Kwon, N.Y.; Jeong, S.M. Correlation of foot posture index with plantar pressure and radiographic measurements in pediatric flatfoot. Ann. Rehabil. Med. 2015, 39, 10–17. [Google Scholar] [CrossRef]
- Zuil-Escobar, J.C.; Martínez-Cepa, C.B.; Martín-Urrialde, J.A.; Gómez-Conesa, A. Evaluating the medial longitudinal arch of the foot: Correlations, reliability, and accuracy in people with a low arch. Phys. Ther. 2019, 99, 364–372. [Google Scholar] [CrossRef]
- Perera, A.; Guha, A. Clinical and radiographic evaluation of the cavus foot: Surgical implications. Foot Ankle Clin. 2013, 18, 619–628. [Google Scholar] [CrossRef]
- Pagenstert, G.I.; Hintermann, B.; Barg, A.; Leumann, A.; Valderrabano, V. Realignment surgery as alternative treatment of varus and valgus ankle osteoarthritis. Clin. Orthop. Relat. Res. 2007, 462, 156–168. [Google Scholar] [CrossRef]
- Younger, A.S.; Sawatzky, B.; Dryden, P. Radiographic assessment of adult flatfoot. Foot Ankle Int. 2005, 26, 820–825. [Google Scholar] [CrossRef]
- van der Heijde, D.M.; van Leeuwen, M.A.; van Riel, P.L.; Koster, A.M.; van ‘t Hof, M.A.; van Rijswijk, M.H.; van de Putte, L.B. Biannual radiographic assessments of hands and feet in a three-year prospective followup of patients with early rheumatoid arthritis. Arthritis Rheum. 1992, 35, 26–34. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Jones, C.P. Hallux valgus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007, 28, 759–777. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.M.; Chung, C.Y.; Park, M.S.; Lee, S.H.; Cho, J.H.; Choi, I.H. Reliability and validity of radiographic measurements in hindfoot varus and valgus. J. Bone Joint Surg. Am. 2010, 92, 2319–2327. [Google Scholar] [CrossRef] [PubMed]
- Nosewicz, T.L.; Knupp, M.; Bolliger, L.; Hintermann, B. The reliability and validity of radiographic measurements for determining the three-dimensional position of the talus in varus and valgus osteoarthritic ankles. Skeletal Radiol. 2012, 41, 1567–1573. [Google Scholar] [CrossRef] [PubMed]
- Kido, M.; Ikoma, K.; Ikeda, R.; Hosokawa, T.; Hara, Y.; Imai, K.; Maki, M.; Ohashi, S.; Mikami, Y.; Kubo, T. Reproducibility of radiographic methods for assessing longitudinal tarsal axes Part 2: Severe cavus or flatfoot study. Foot 2020, 42, 101631. [Google Scholar] [CrossRef]
- Porteny, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 2nd ed.; Prentice Hall Health: Upper Saddle River, NJ, USA, 2000; p. 752. [Google Scholar]
- Burns, J.; Keenan, A.-M.; Redmond, A. Foot type and overuse injury in triathletes. J. Am. Podiatr. Assoc. 2005, 95, 235–241. [Google Scholar] [CrossRef]
- Cain, L.E.; Nicholson, L.L.; Adams, R.D.; Burns, J. Foot morphology and foot/ankle injury in indoor football. J. Sci. Med. Sport. 2007, 10, 311–319. [Google Scholar] [CrossRef]
- McLaughlin, P.; Vaughan, B.; Shanahan, J.; Martin, J.; Linger, G. Inexperienced examiners and the Foot Posture Index: A reliability study. Man. Ther. 2016, 26, 238–240. [Google Scholar] [CrossRef]
- Redmond, A. The Foot Posture Index: Easy Quantification of Standing Foot Posture: Six Item Version: FPI-6: User Guide and Manual; University of Leeds: Leeds, UK, 2005. [Google Scholar]
- Shibuya, N.; Jupiter, D.C.; Ciliberti, L.J., Jr.; VanBuren, V.; La Fontaine, J. Prevalence of podiatric medical problems in veterans versus nonveterans. J. Am. Podiatr. Assoc. 2011, 101, 323–330. [Google Scholar] [CrossRef]






| Group A (n = 40) | Group B (n = 60) | |
|---|---|---|
| Age, years | 23.8 ± 1.9 (21–28) | 61.9 ± 15.3 (9–83) |
| Sex, numbers | Male 40 | Male 24, Female 36 |
| Height, cm | 174.6 ± 4.7 (163.0–186.0) | 158.3 ± 8.9 (132.0–177.7) |
| Weight, kg | 72.6 ± 9.7 (48.6–100.9) | 65.5 ± 12.1 (30.6–89.9) |
| BMI, kg/m2 | 23.8 ± 3.2 (16.3–32.9) | 26.1 ± 4.2 (16.1–40.8) |
| Group A (n = 40) | Group B (n = 60) | |
|---|---|---|
| Rater 1 vs. Rater 2 | 0.787 | 0.938 |
| Rater 1 vs. Rater 3 | 0.583 | 0.962 |
| Rater 1 vs. Rater 4 | 0.471 | 0.809 |
| Rater 2 vs. Rater 3 | 0.637 | 0.938 |
| Rater 2 vs. Rater 4 | 0.535 | 0.772 |
| Rater 3 vs. Rater 4 | 0.601 | 0.824 |
| Total | 0.608 | 0.878 |
| AP TCA | TNCA | AP TMA | Lat TCA | CPA | MA | HAA | |
|---|---|---|---|---|---|---|---|
| FPI 1 | 0.136 | 0.620 * | 0.492 * | 0.399 * | −0.052 | 0.530 * | −0.713 * |
| FPI 2 | 0.109 | 0.602 * | 0.398 * | 0.317 * | −0.066 | 0.505 * | −0.738 * |
| FPI 3 | 0.127 | 0.583 ** | 0.339 ** | 0.356 ** | 0.002 | 0.467 * | −0.726 ** |
| FPI 4 | 0.072 | 0.573 ** | 0.358 ** | 0.323 ** | −0.052 | 0.485 ** | −0.748 ** |
| FPI 5 | 0.166 | 0.686 ** | 0.438 ** | 0.318 ** | −0.263 ** | 0.658 ** | −0.664 ** |
| FPI 6 | 0.168 | 0.597 ** | 0.503 ** | 0.346 ** | −0.095 | 0.512 ** | −0.658 ** |
| Total FPI-6 | 0.140 | 0.665 ** | 0.453 ** | 0.369 ** | −0.096 | 0.570 ** | −0.773 ** |
| AP TCA | TNCA | AP TMA | Lat TCA | CPA | MA | HAA | |
|---|---|---|---|---|---|---|---|
| FPI 1 | −0.086 | 0.381 * | 0.048 | −0.255 | −0.337 * | 0.328 * | −0.267 |
| FPI 2 | 0.031 | 0.159 | −0.164 | −0.124 | −0.097 | 0.114 | −0.134 |
| FPI 3 | −0.100 | 0.206 | 0.060 | −0.326 * | −0.369 * | 0.281 | −0.177 |
| FPI 4 | −0.091 | 0.320 * | 0.027 | −0.091 | −0.148 | 0.217 | −0.171 |
| FPI 5 | −0.095 | 0.130 | −0.176 | −0.021 | −0.144 | 0.228 | −0.213 |
| FPI 6 | 0.046 | 0.560 ** | 0.198 | −0.337 * | −0.487 ** | 0.518 ** | −0.268 |
| Total FPI-6 | −0.156 | 0.258 | 0.139 | −0.101 | −0.200 | 0.172 | −0.374 * |
| AP TCA | TNCA | AP TMA | Lat TCA | CPA | MA | HAA | |
|---|---|---|---|---|---|---|---|
| FPI 1 | 0.160 | 0.713 ** | 0.500 ** | 0.455 ** | −0.138 | 0.605 ** | −0.801 ** |
| FPI 2 | 0.136 | 0.705 ** | 0.591 ** | 0.465 ** | −0.168 | 0.601 ** | −0.765 ** |
| FPI 3 | 0.122 | 0.672 ** | 0.456 ** | 0.391 ** | −0.127 | 0.556 ** | −0.780 ** |
| FPI 4 | 0.143 | 0.629 ** | 0.388 ** | 0.404 ** | −0.065 | 0.514 ** | −0.761 ** |
| FPI 5 | 0.080 | 0.641 ** | 0.421 ** | 0.355 ** | −0.133 | 0.526 ** | −0.777 ** |
| FPI 6 | 0.192 | 0.712 ** | 0.469 ** | 0.480 ** | −0.247 | 0.678 ** | −0.716 ** |
| Total FPI-6 | 0.237 | 0.664 ** | 0.542 ** | 0.492 ** | −0.033 | 0.544 ** | −0.712 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyung, M.G.; Cho, Y.J.; Lee, J.H.; Shin, M.S.; Park, J.H.; Lee, D.Y. Reliability and Radiographic Correlation of the Foot Posture Index-6: A Multi-Rater Analysis in Symptomatic and Asymptomatic Individuals. Diagnostics 2025, 15, 1214. https://doi.org/10.3390/diagnostics15101214
Kyung MG, Cho YJ, Lee JH, Shin MS, Park JH, Lee DY. Reliability and Radiographic Correlation of the Foot Posture Index-6: A Multi-Rater Analysis in Symptomatic and Asymptomatic Individuals. Diagnostics. 2025; 15(10):1214. https://doi.org/10.3390/diagnostics15101214
Chicago/Turabian StyleKyung, Min Gyu, Yun Jae Cho, Jae Hee Lee, Min Seok Shin, Jay Hoon Park, and Dong Yeon Lee. 2025. "Reliability and Radiographic Correlation of the Foot Posture Index-6: A Multi-Rater Analysis in Symptomatic and Asymptomatic Individuals" Diagnostics 15, no. 10: 1214. https://doi.org/10.3390/diagnostics15101214
APA StyleKyung, M. G., Cho, Y. J., Lee, J. H., Shin, M. S., Park, J. H., & Lee, D. Y. (2025). Reliability and Radiographic Correlation of the Foot Posture Index-6: A Multi-Rater Analysis in Symptomatic and Asymptomatic Individuals. Diagnostics, 15(10), 1214. https://doi.org/10.3390/diagnostics15101214






