Ultrasound Elastography as a Diagnostic Tool for Peyronie’s Disease: A State-of-the-Art Review
Abstract
1. Introduction
1.1. Peyronie’s Disease (PD)
1.2. Elastography
1.3. The Aim of this Study
2. Relevant Sections
2.1. Strain Elastography
2.2. Transient Elastography
2.3. Acoustic Radiation Force Impulse
2.3.1. Point Shear-Wave Elastography (p-SWE)
2.3.2. Shear-Wave Elastography
2.3.3. Supersonic Shear Imaging
2.3.4. Vibro-Elastography and Vibro-Acoustography
2.4. Literature Review
2.4.1. Lahme et al. (2009) [38]
2.4.2. Morana et al. (2010) [39]
2.4.3. Riversi et al. (2012) [40]
2.4.4. Zhang et al. (2018) [41]
2.4.5. Trama et al. (2018) [42]
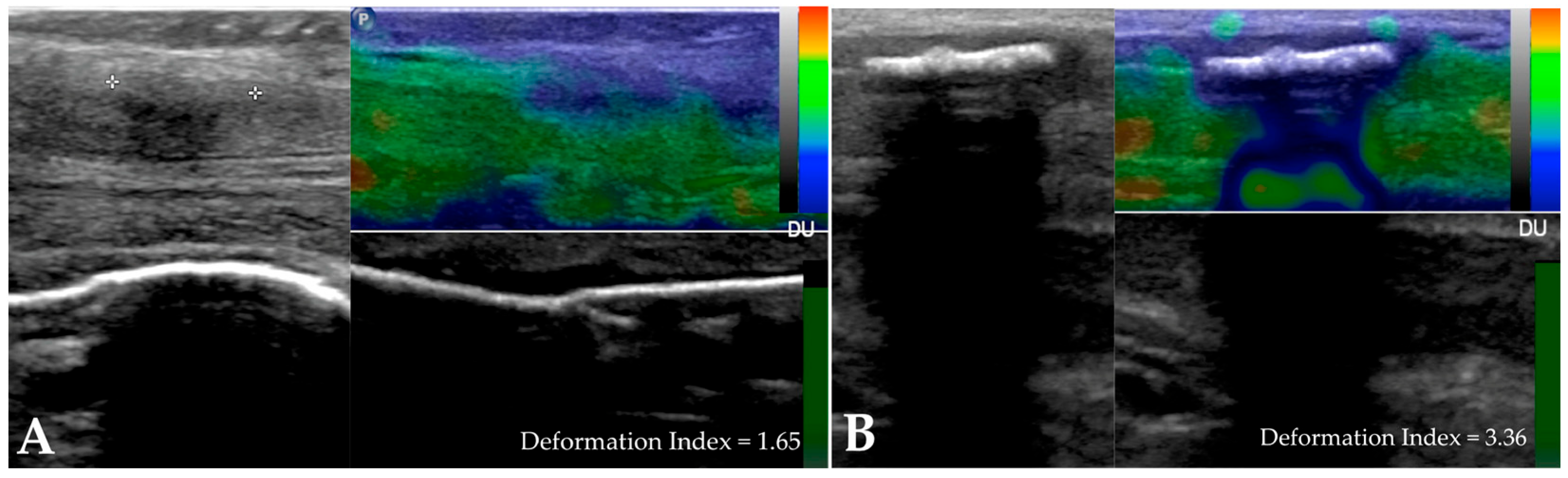
2.4.6. Tyloch et al. (2020) [43]
2.4.7. Trama et al. (2022) [44]
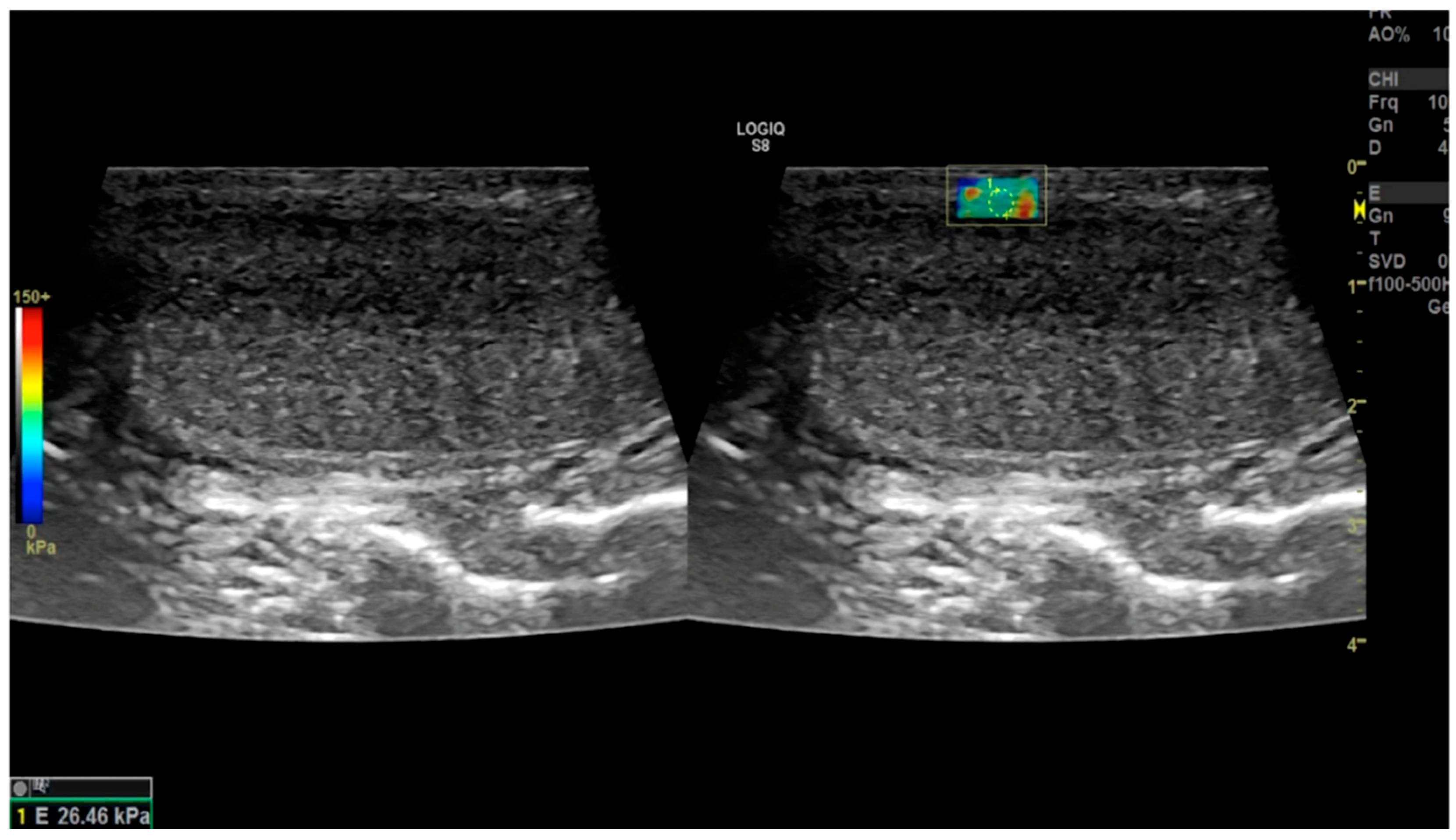
2.4.8. Zhao et al. (2024) [45]
2.4.9. Richards et al. (2014) [46]
2.4.10. Dhawan et al. (2022) [47]
2.4.11. Parmar et al. (2020) [37]
- -
- To assess the presence of concurrent ED to determine the need for a penile prosthesis for comprehensive treatment;
- -
- To determine whether plaques involve the neurovascular bundle or cavernosal artery, aiding in surgical preparation;
- -
- To conduct ultrasound assessments in the office, saving both time and money.
Sonoelastography
2.4.12. Simon et al. (2022) [48]
3. Discussion
4. Conclusions
5. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herati, A.S.; Pastuszak, A.W. The Genetic Basis of Peyronie’s Disease: A Review. Sex Med. Rev. 2016, 4, 85–94. [Google Scholar] [CrossRef]
- Bias, W.B.; Nyberg, L.M., Jr.; Hochberg, M.C.; Walsh, P.C.; Opitz, J.M. Peyronie’s disease: A newly recognized autosomal-dominant trait. Am. J. Med. Genet. 1982, 12, 227–235. [Google Scholar] [CrossRef] [PubMed]
- DiBenedetti, D.B.; Nguyen, D.; Zografos, L.; Ziemiecki, R.; Zhou, X. A Population-Based Study of Peyronie’s Disease: Prevalence and Treatment Patterns in the United States. Adv. Urol. 2011, 2011, 282503. [Google Scholar] [CrossRef] [PubMed]
- Stuntz, M.; Perlaky, A.; des Vignes, F.; Kyriakides, T.; Glass, D. The Prevalence of Peyronie’s Disease in the United States: A Population-Based Study. PLoS ONE 2016, 11, e0150157. [Google Scholar] [CrossRef] [PubMed]
- Bella, A.J.; Lee, J.C.; Grober, E.D.; Carrier, S.; Bénard, F.; Brock, G.B. 2018 Canadian Urological Association guideline for Peyronie’s disease and congenital penile curvature. Can. Urol. Assoc. J. 2018, 12, E197–E209. [Google Scholar] [CrossRef] [PubMed]
- Johnson, H.M.; Weerakoon, P.; Stricker, P.D. The incidence, aetiology, and presentation of Peyronie’s disease in Sydney, Australia. J. Sex. Disabil. 2002, 20, 109–116. [Google Scholar] [CrossRef]
- La Pera, G.; Pescatori, E.S.; Calabrese, M.; Boffini, A.; Colombo, F.; Andriani, E.; Natali, A.; Vaggi, L.; Catuogno, C.; Giustini, M.; et al. Peyronie’s disease: Prevalence and association with cigarette smoking. A multicenter population-based study in men aged 50–69 years. Eur Urol. 2001, 40, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, U.; Sommer, F.; Klotz, T.; Braun, M.; Reifenrath, B.; Engelmann, U. The prevalence of Peyronie’s disease: Results of a large survey. BJU Int. 2001, 88, 727–730. [Google Scholar] [CrossRef] [PubMed]
- Rhoden, E.L.; Teloken, C.; Ting, H.Y.; Lucas, M.L.; Teodósio da Ros, C.; Ary Vargas Souto, C. Prevalence of Peyronie’s disease in men over 50-y-old from Southern Brazil. Int. J. Impot. Res. 2001, 13, 291–293. [Google Scholar] [CrossRef]
- Shiraishi, K.; Shimabukuro, T.; Matsuyama, H. The prevalence of Peyronie’s disease in Japan: A study in men undergoing maintenance hemodialysis and routine health checks. J. Sex. Med. 2012, 9, 2716–2723. [Google Scholar] [CrossRef]
- Wong, A.; Tsang, S.S.; Ray, Y.M.O.; Chun, S.; Tsang, C.-F.; Ho, B.S.; Ng, A.T.; Tsu, J.H.; Lam, W. Mp33-12 Prevalence of Peyronie’s disease and its psychosexual impact in the chinese population: A large cohort population-based cross-sectional study. J. Urol. 2020, 203, e499. [Google Scholar]
- Kyei, M.Y.; Mensah, J.E.; Asante, E.; Bray, L.D.; Awuku-Asabre, J. Peyronie’s Disease in People of African Origin: A Mini Review. J. Gerontol. Aging Res. 2017, 1, 104. Available online: https://www.researchgate.net/publication/327751134_Peyronie%27s_Disease_in_People_of_African_origin_A._Mini_Review (accessed on 16 March 2024).
- Lindsay, M.B.; Schain, D.M.; Grambsch, P.; Benson, R.C.; Beard, C.M.; Kurland, L.T. The incidence of Peyronie’s disease in Rochester, Minnesota, 1950 through 1984. J. Urol. 1991, 146, 1007–1009. [Google Scholar] [CrossRef]
- Tefekli, A.; Kandirali, E.; Erol, H.; Alp, T.; Köksal, T.; Kadioğlu, A. Peyronie’s disease in men under age 40: Characteristics and outcome. Int. J. Impot. Res. 2001, 13, 18–23. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Levine, L.A.; Estrada, C.R.; Storm, D.W.; Matkov, T.G. Peyronie disease in younger men: Characteristics and treatment results. J. Androl. 2003, 24, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Deveci, S.; Hopps, C.V.; O’Brien, K.; Parker, M.; Guhring, P.; Mulhall, J.P. Defining the clinical characteristics of Peyronie’s disease in young men. J. Sex. Med. 2007, 4, 485–490. [Google Scholar] [CrossRef]
- Cilio, S.; Fallara, G.; Capogrosso, P.; Candela, L.; Belladelli, F.; Pozzi, E.; Corsini, C.; Raffo, M.; Schifano, N.; Boeri, L.; et al. The symptomatic burden of Peyronie’s disease at presentation according to patient age: A critical analysis of the Peyronie’s disease questionnaire (PDQ) domains. Andrology 2023, 11, 501–507. [Google Scholar] [CrossRef]
- Paulis, G.; Cavallini, G.; Barletta, D.; Turchi, P.; Vitarelli, A.; Fabiani, A. Clinical and epidemiological characteristics of young patients with Peyronie’s disease: A retrospective study. Res. Rep. Urol. 2015, 7, 107–111. [Google Scholar]
- Hellstrom, W.J.; Bivalacqua, T.J. Peyronie’s disease: Etiology, medical, and surgical therapy. J. Androl. 2000, 21, 347–354. [Google Scholar] [CrossRef]
- Weidner, W.; Schroeder-Printzen, I.; Weiske, W.H.; Vosshenrich, R. Sexual dysfunction in Peyronie’s disease: An analysis of 222 patients without previous local plaque therapy. J. Urol. 1997, 157, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Romano, G.; Paulis, A. Prevalence, psychological impact, and risk factors of erectile dysfunction in patients with Peyronie’s disease: A retrospective analysis of 309 cases. Res. Rep. Urol. 2016, 8, 95–103. [Google Scholar]
- Nelson, C.J.; Diblasio, C.; Kendirci, M.; Hellstrom, W.; Guhring, P.; Mulhall, J.P. The Chronology of Depression and Distress in Men with Peyronie’s Disease. J. Sex. Med. 2008, 5, 1985–1990. [Google Scholar] [CrossRef] [PubMed]
- Kuja-Halkola, R.; Henningsohn, L.; D’Onofrio, B.M.; Mills, J.; Adolfsson, A.; Larsson, H.; Cederlöf, M. Mental Disorders in Peyronie’s Disease: A Swedish Cohort Study of 3.5 Million Men. J. Urol. 2021, 205, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Devine, C.J., Jr.; Somers, K.D.; Ladaga, L.E. Peyronie’s disease: Pathophysiology. Prog. Clin. Biol. Res. 1991, 370, 355–358. [Google Scholar] [PubMed]
- Devine, C.J.J.; Somers, K.D.; Jordan, G.H.; Schlossberg, S.M. Proposal: Trauma as a cause of Peyronie’s lesion. J. Urol. 1997, 157, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Jarow, J.P.; Lowe, F.C. Penile trauma: An etiologic factor in Peyronie’s disease and erectile dysfunction. J. Urol. 1997, 158, 1388–1390. [Google Scholar] [CrossRef] [PubMed]
- El-Sakka, A.I.; Salabas, E.; Dinçer, M.; Kadioglu, A. The pathophysiology of Peyronie’s disease. Arab J. Urol. 2013, 11, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Paulis, G.; Romano, G.; Paulis, L.; Barletta, D. Recent Pathophysiological Aspects of Peyronie’s Disease: Role of Free Radicals, Rationale, and Therapeutic Implications for Antioxidant Treatment-Literature Review. Adv. Urol. 2017, 2017, 4653512. [Google Scholar] [CrossRef]
- Paulis, G.; De Giorgio, G.; Paulis, L. Role of Oxidative Stress in Peyronie’s Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants. Int. J. Mol. Sci. 2022, 23, 15969. [Google Scholar] [CrossRef]
- Sikka, S.C.; Hellstrom, W.J. Role of oxidative stress and antioxidants in Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 353–360. [Google Scholar] [CrossRef]
- Paulis, G.; Brancato, T. Inflammatory mechanisms and oxidative stress in Peyronie’s disease: Therapeutic “rationale” and related emerging treatment strategies. Inflamm. Allergy Drug Targets 2012, 11, 48–57. [Google Scholar] [CrossRef]
- Davila, H.H.; Magee, T.R.; Vernet, D.; Rajfer, J.; Gonzalez-Cadavid, N.F. Gene transfer of inducible nitric oxide synthase complementary DNA regresses the fibrotic plaque in an animal model of Peyronie’s disease. Biol. Reprod. 2004, 71, 1568–1577. [Google Scholar] [CrossRef]
- Bivalacqua, T.J.; Champion, H.C.; Hellstrom, W.J. Implications of nitric oxide synthase isoforms in the pathophysiology of Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Cadavid, N.F.; Magee, T.R.; Ferrini, M.; Qian, A.; Vernet, D.; Rajfer, J. Gene expression in Peyronie’s disease. Int. J. Impot. Res. 2002, 14, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Kelâmi, A. Autophotography in evaluation of functional penile disorders. Urology 1983, 21, 628–629. [Google Scholar] [CrossRef] [PubMed]
- McCauley, J.F.; Dean, R.C. Diagnostic utility of penile ultrasound in Peyronie’s disease. World. J. Urol. 2020, 38, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Parmar, M.; Masterson, J.M.; Masterson, T.A., 3rd. The role of imaging in the diagnosis and management of Peyronie’s disease. Curr. Opin. Urol. 2020, 30, 283–289. [Google Scholar] [CrossRef]
- Lahme, S.; Zimmermanns, V.; Liske, P.; Ober, P. Real-Time Elastography (RTE) in Patients with Peyronie’s Disease: First Results of a New Imaging Technique for the Detection and Mesurement of Plaques. J. Urol. 2009, 181, 280. [Google Scholar] [CrossRef]
- Morana, C.; Loiero, G.; Sangiorgio, A.; Zani, T.; Catalano, G. Elastosonography in the Peyronie’s disease: Our preliminary experience. Arch. Ital. Urol. Androl. 2010, 82, 269–270. [Google Scholar]
- Riversi, V.; Tallis, V.; Trovatelli, S.; Belba, A.; Volterrani, L.; Iacoponi, F.; Ponchietti, R. Realtime-elastosonography of the penis in patients with Peyronie’s disease. Arch. Ital. Urol. Androl. 2012, 84, 174–177. [Google Scholar]
- Zhang, X.; Zhou, B.; Miranda, A.F.; Trost, L.W. A Novel Noninvasive Ultrasound Vibro-elastography Technique for Assessing Patients with Erectile Dysfunction and Peyronie Disease. Urology 2018, 116, 99–105. [Google Scholar] [CrossRef]
- Trama, F.; Riccardo, F.; Ruffo, A.; Celentano, G.; Romeo, G.; Russo, A. Elastosonographic Changes in Patients with Peyronie’s Disease, before and after Treatment with a Compound Based on Ecklonia bicyclis, Tribulus terrestris, and Water-Soluble Chitosan. OJU J. 2018, 8, 77–87. Available online: https://www.scirp.org/pdf/OJU_2018032914374831.pdf (accessed on 16 March 2024). [CrossRef]
- Tyloch, J.F.; Tyloch, D.J.; Adamowicz, J.; Warsiński, P.; Ostrowski, A.; Nowikiewicz, M.; Drewa, T. Application of three-dimensional ultrasonography (3D ultrasound) to pretreatment evaluation of plastic induration of the penis (Peyronie’s disease). Med. Ultrason. 2020, 22, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Trama, F.; Illiano, E.; Iacono, F.; Ruffo, A.; di Lauro, G.; Aveta, A.; Crocetto, F.; Manfredi, C.; Costantini, E. Use of penile shear wave elastosonography for the diagnosis of Peyronie’s Disease: A prospective case-control study. Basic Clin. Androl. 2022, 32, 15. [Google Scholar] [CrossRef]
- Zhao, S.; Wu, X.; Zhang, Y.; Zhang, C. Role of Shear Wave Elastography in the Diagnosis of Peyronie Disease. J. Ultrasound Med. 2024, 43, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Richards, G.; Goldenberg, E.; Pek, H.; Gilbert, B.R. Penile sonoelastography for the localization of a non-palpable, non-sonographically visualized lesion in a patient with penile curvature from Peyronie’s disease. J. Sex. Med. 2014, 11, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, S.; Dhok, A.; Phatak, S.; Mitra, K.; Ansari, A. Peyronie’s Disease Presenting as Curvature of the Penis: A Case Report. Cureus 2022, 14, e32055. [Google Scholar] [CrossRef] [PubMed]
- Simon, V.; Dudea, S.M.; Crisan, N.; Stanca, V.D.; Dudea-Simon, M.; Andras, I.; Mihaly, Z.A.; Coman, I. Elastography in the Urological Practice: Urinary and Male Genital Tract, Prostate Excluded-Review. Diagnostics 2022, 12, 1727. [Google Scholar] [CrossRef] [PubMed]
- Shiina, T.; Nightingale, K.R.; Palmeri, M.L.; Hall, T.J.; Bamber, J.C.; Barr, R.G.; Castera, L.; Choi, B.I.; Chou, Y.H.; Cosgrove, D.; et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: Basic principles and terminology. Ultrasound Med. Biol. 2015, 41, 1126–1147. [Google Scholar] [CrossRef] [PubMed]
- Ophir, J.; Mehta, D. Elimination of diffraction error in acoustic attenuation estimation via axial beam translation. Ultrason. Imaging 1988, 10, 139–152. [Google Scholar] [CrossRef]
- Sigrist, R.M.S.; Liau, J.; Kaffas, A.E.; Chammas, M.C.; Willmann, J.K. Ultrasound Elastography: Review of Techniques and Clinical Applications. Theranostics 2017, 7, 1303–1329. [Google Scholar] [CrossRef]
- Ozturk, A.; Grajo, J.R.; Dhyani, M.; Anthony, B.W.; Samir, A.E. Principles of ultrasound elastography. Abdom. Radiol. 2018, 43, 773–785. [Google Scholar] [CrossRef]
- Gennisson, J.L.; Deffieux, T.; Fink, M.; Tanter, M. Ultrasound elastography: Principles and techniques. Diagn. Interv. Imaging 2013, 94, 487–495. [Google Scholar]
- Cui, X.W.; Li, K.N.; Yi, A.J.; Wang, B.; Wei, Q.; Wu, G.G.; Dietrich, C.F. Ultrasound elastography. Endosc. Ultrasound 2022, 11, 252–274. [Google Scholar] [CrossRef]
- Kwon, S.J.; Jeong, M.K. Advances in ultrasound elasticity imaging. Biomed. Eng. Lett. 2017, 7, 71–79. [Google Scholar] [CrossRef]
- Ophir, J.; Céspedes, I.; Ponnekanti, H.; Yazdi, Y.; Li, X. Elastography: A quantitative method for imaging the elasticity of biological tissues. Ultrason. Imaging 1991, 13, 111–134. [Google Scholar] [CrossRef]
- Sandrin, L.; Fourquet, B.; Hasquenoph, J.M.; Yon, S.; Fournier, C.; Mal, F.; Christidis, C.; Ziol, M.; Poulet, B.; Kazemi, F.; et al. Transient elastography: A new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med. Biol. 2003, 29, 1705–1713. [Google Scholar] [CrossRef] [PubMed]
- Arndt, R.; Schmidt, S.; Loddenkemper, C.; Grünbaum, M.; Zidek, W.; van der Giet, M.; Westhoff, T.H. Noninvasive evaluation of renal allograft fibrosis by transient elastography—A pilot study. Transpl. Int. 2010, 23, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Sommerer, C.; Scharf, M.; Seitz, C.; Millonig, G.; Seitz, H.K.; Zeier, M.; Mueller, S. Assessment of renal allograft fibrosis by transient elastography. Transpl. Int. 2013, 26, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Lukenda, V.; Mikolasevic, I.; Racki, S.; Jelic, I.; Stimac, D.; Orlic, L. Transient elastography: A new noninvasive diagnostic tool for assessment of chronic allograft nephropathy. Int. Urol. Nephrol. 2014, 46, 1435–1440. [Google Scholar] [CrossRef]
- Lee, Y.J. Shear Wave Elastography: A Reliable and Outperforming Diagnostic Tool for Liver Fibrosis Assessment in Chronic Hepatitis. A Literature Review. Available online: https://www.konicaminolta.jp/healthcare/products/us/aixplorer/pdf/whitepaper_liver-fibrosis-literature-review_eng.pdf (accessed on 16 March 2024).
- Dong, Z.; Kim, J.; Huang, C.; Lowerison, M.R.; Lok, U.W.; Chen, S.; Song, P. Three-Dimensional Shear Wave Elastography Using a 2D Row Column Addressing (RCA) Array. BME Front. 2022, 2022, 9879632. [Google Scholar] [CrossRef]
- Cantisani, V.; David, E.; Grazhdani, H.; Rubini, A.; Radzina, M.; Dietrich, C.F.; Durante, C.; Lamartina, L.; Grani, G.; Valeria, A.; et al. Prospective Evaluation of Semiquantitative Strain Ratio and Quantitative 2D Ultrasound Shear Wave Elastography (SWE) in Association with TIRADS Classification for Thyroid Nodule Characterization. Ultraschall Med. 2019, 40, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Veyrieres, J.B.; Albarel, F.; Lombard, J.V.; Berbis, J.; Sebag, F.; Oliver, C.; Petit, P. A threshold value in Shear Wave elastography to rule out malignant thyroid nodules: A reality? Eur. J. Radiol. 2012, 81, 3965–3972. [Google Scholar] [CrossRef] [PubMed]
- Tanter, M.; Bercoff, J.; Athanasiou, A.; Deffieux, T.; Gennisson, J.L.; Montaldo, G.; Muller, M.; Tardivon, A.; Fink, M. Quantitative assessment of breast lesion viscoelasticity: Initial clinical results using supersonic shear imaging. Ultrasound Med. Biol. 2008, 34, 1373–1386. [Google Scholar] [CrossRef] [PubMed]
- Rivaz, H.; Rohling, R. A hand-held probe for vibro-elastography. Med. Image Comput. Comput. Assist. Interv. 2005, 8, 613–620. [Google Scholar]
- Fatemi, M.; Greenleaf, J.F. Ultrasound-stimulated vibro-acoustic spectrography. Science 1998, 280, 82–85. [Google Scholar] [CrossRef]
- Mitri, F.G.; Davis, B.J.; Urban, M.W.; Alizad, A.; Greenleaf, J.F.; Lischer, G.H.; Wilson, T.M.; Fatemi, M. Vibro-acoustography imaging of permanent prostate brachytherapy seeds in an excised human prostate–preliminary results and technical feasibility. Ultrasonics 2009, 49, 389–394. [Google Scholar] [CrossRef][Green Version]
- Urban, M.W.; Chalek, C.; Kinnick, R.R.; Kinter, T.M.; Haider, B.; Greenleaf, J.F.; Thomenius, K.E.; Fatemi, M. Implementation of vibro-acoustography on a clinical ultrasound system. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2011, 58, 1169–1181. [Google Scholar] [CrossRef]
- Alizad, A.; Whaley, D.H.; Urban, M.W.; Carter, R.E.; Kinnick, R.R.; Greenleaf, J.F.; Fatemi, M. Breast vibro-acoustography: Initial results show promise. Breast Cancer Res. 2012, 14, R128. [Google Scholar] [CrossRef]
- Nelson, C.J.; Mulhall, J.P. Psychological impact of Peyronie’s disease: A review. J. Sex. Med. 2013, 10, 653–660. [Google Scholar] [CrossRef]
- Chung, E.; Clendinning, E.; Lessard, L.; Brock, G. Five-year follow-up of Peyronie’s graft surgery: Outcomes and patient satisfaction. J. Sex. Med. 2011, 8, 594–600. [Google Scholar] [CrossRef]
- Bercoff, J.; Chaffai, S.; Tanter, M.; Sandrin, L.; Catheline, S.; Fink, M.; Gennisson, J.L.; Meunier, M. In vivo breast tumor detection using transient elastography. Ultrasound Med. Biol. 2003, 29, 1387–1396. [Google Scholar] [CrossRef] [PubMed]
- Adhoute, X.; Foucher, J.; Laharie, D.; Terrebonne, E.; Vergniol, J.; Castéra, L.; Lovato, B.; Chanteloup, E.; Merrouche, W.; Couzigou, P.; et al. Diagnosis of liver fibrosis using FibroScan and other noninvasive methods in patients with hemochromatosis: A prospective study. Gastroenterol. Clin. Biol. 2008, 32, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.; Nguyen, M.; Ju, I.; Brancatisano, A.; Ryan, B.; van der Poorten, D. Utility of Fibroscan XL to assess the severity of non-alcoholic fatty liver disease in patients undergoing bariatric surgery. Sci. Rep. 2021, 11, 14006. [Google Scholar] [CrossRef] [PubMed]
- Sandrin, L.; Tanter, M.; Catheline, S.; Fink, M. Shear modulus imaging with 2-D transient elastography. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2002, 49, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Tanter, M.; Bercoff, J.; Sandrin, L.; Fink, M. Ultrafast compound imaging for 2-D motion vector estimation: Application to transient elastography. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2002, 49, 1363–1374. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, M.; Gallotti, A.; Mucelli, R.P. Tissue quantification with acoustic radiation force impulse imaging: Measurement repeatability and normal values in the healthy liver. AJR Am. J. Roentgenol. 2010, 195, 132–136. [Google Scholar] [CrossRef]
- Bota, S.; Herkner, H.; Sporea, I.; Salzl, P.; Sirli, R.; Neghina, A.M.; Peck-Radosavljevic, M. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int. 2013, 33, 1138–1147. [Google Scholar] [CrossRef] [PubMed]
- Ferraioli, G.; Tinelli, C.; Lissandrin, R.; Zicchetti, M.; Bernuzzi, S.; Salvaneschi, L.; Filice, C. Elastography Study Group Ultrasound point shear wave elastography assessment of liver and spleen stiffness: Effect of training on repeatability of measurements. Eur. Radiol. 2014, 24, 1283–1289. [Google Scholar] [CrossRef]
- Ferraioli, G.; Parekh, P.; Levitov, A.B.; Filice, C. Shear wave elastography for evaluation of liver fibrosis. J. Ultrasound Med. 2014, 33, 197–203. [Google Scholar] [CrossRef]
- Cassinotto, C.; Lapuyade, B.; Mouries, A.; Hiriart, J.B.; Vergniol, J.; Gaye, D.; Castain, C.; Le Bail, B.; Chermak, F.; Foucher, J.; et al. Non-invasive assessment of liver fibrosis with impulse elastography: Comparison of Supersonic Shear Imaging with ARFI and FibroScan®. J. Hepatol. 2014, 61, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Andresen, R.; Wegner, H.E.; Miller, K.; Banzer, D. Imaging modalities in Peyronie’s disease. An intrapersonal comparison of ultrasound sonography, X-ray in mammography technique, computerized tomography, and nuclear magnetic resonance in 20 patients. Eur. Urol. 1998, 34, 128–135. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paulis, G.; De Giorgio, G.; Paulis, A. Ultrasound Elastography as a Diagnostic Tool for Peyronie’s Disease: A State-of-the-Art Review. Diagnostics 2024, 14, 665. https://doi.org/10.3390/diagnostics14060665
Paulis G, De Giorgio G, Paulis A. Ultrasound Elastography as a Diagnostic Tool for Peyronie’s Disease: A State-of-the-Art Review. Diagnostics. 2024; 14(6):665. https://doi.org/10.3390/diagnostics14060665
Chicago/Turabian StylePaulis, Gianni, Giovanni De Giorgio, and Andrea Paulis. 2024. "Ultrasound Elastography as a Diagnostic Tool for Peyronie’s Disease: A State-of-the-Art Review" Diagnostics 14, no. 6: 665. https://doi.org/10.3390/diagnostics14060665
APA StylePaulis, G., De Giorgio, G., & Paulis, A. (2024). Ultrasound Elastography as a Diagnostic Tool for Peyronie’s Disease: A State-of-the-Art Review. Diagnostics, 14(6), 665. https://doi.org/10.3390/diagnostics14060665





