Understanding Loss to Follow-Up in AMD Patients Receiving VEGF Inhibitor Therapy: Associated Factors and Underlying Reasons
Abstract
1. Introduction
2. Materials and Methods
- Initiation of anti-VEGF therapy (ranibizumab 0.5 mg, aflibercept 2 mg, brolucizumab 6 mg, or bevacizumab 1.25 mg) between 1 January 2010 and 1 January 2022;
- Treatment of wet AMD in accordance with the valid indication restrictions for this treatment;
- Administration of at least 1 intravitreal anti-VEGF injection;
- Minimum assessment period of 6 months since the first injection.
- Patients treated in interventional clinical trials;
- Patients who were administered other drugs (e.g., steroids) intravitreally;
- Intravitreal anti-VEGF treatment administered for reasons other than wet AMD (DME, RVO, proliferative diabetic retinopathy, visual impairment due to choroidal neovascularization of different etiology).
- Active subfoveal macular neovascularization (MNV) due to AMD;
- Baseline BCVA 20/25–20/200, in the case of a single seeing eye 20/25–20/320;
- Signs of MNV activity confirmed using optical coherence tomography (OCT) and/or fluorescein angiography (FAG) and/or optical coherence tomography angiography (OCT-A);
- In the case of active MNV with baseline BCVA worse than 20/200 or 20/320 in a single seeing eye, only off-label bevacizumab treatment was possible.
- (1)
- Deterioration (−6 to −14 letters)—this category represents a moderate decrease of visual acuity;
- (2)
- Improvement (+6 to +14 letters)—these patients have experienced a moderate gain in visual acuity, indicating a positive response to treatment;
- (3)
- Stabilization (+5 to −5 letters)—this category includes patients whose visual acuity has remained relatively stable, with minor gains or losses, where disease progression has been halted;
- (4)
- Super responders (+15 or more letters)—patients who have shown a significant improvement in BCVA, indicating a highly effective response to the anti-VEGF treatment;
- (5)
- Treatment failure (−15 or more letters)—this category represents a significant loss of BCVA, suggesting that the treatment has not been effective, or the disease has significantly progressed.
- (1)
- ≥70 letters (≥20/40);
- (2)
- ≥35 to ≤69 letters (20/200—20/50);
- (3)
- <35 letters (<20/200).
Statistical Analysis
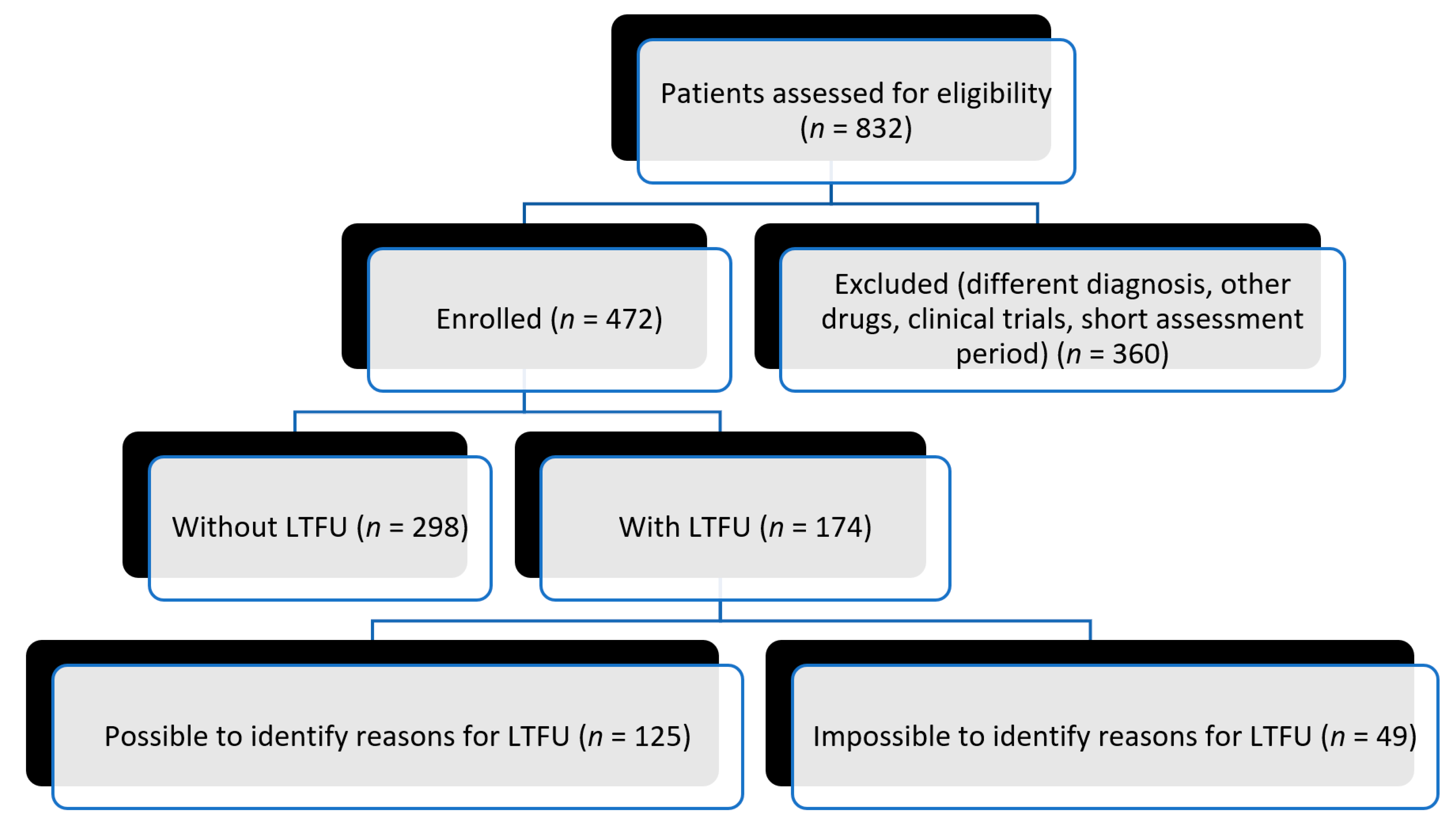
3. Results
3.1. Characteristics of the Population
3.2. Treatment
- 51.9% (two-hundred and forty-five patients) were treated with ranibizumab;
- 16.5% (seventy-eight patients) were treated with aflibercept;
- 1.5% (seven patients) were treated with bevacizumab;
- 1.7% (eight patients) were treated with brolucizumab.
- 25.6% (121 patients) had their treatment switched to a different anti-VEGF drug during the course of the study.
- In 2.8% (13 patients), each eye was treated with a different type of anti-VEGF drug without switch.
3.3. Loss to Follow-Up
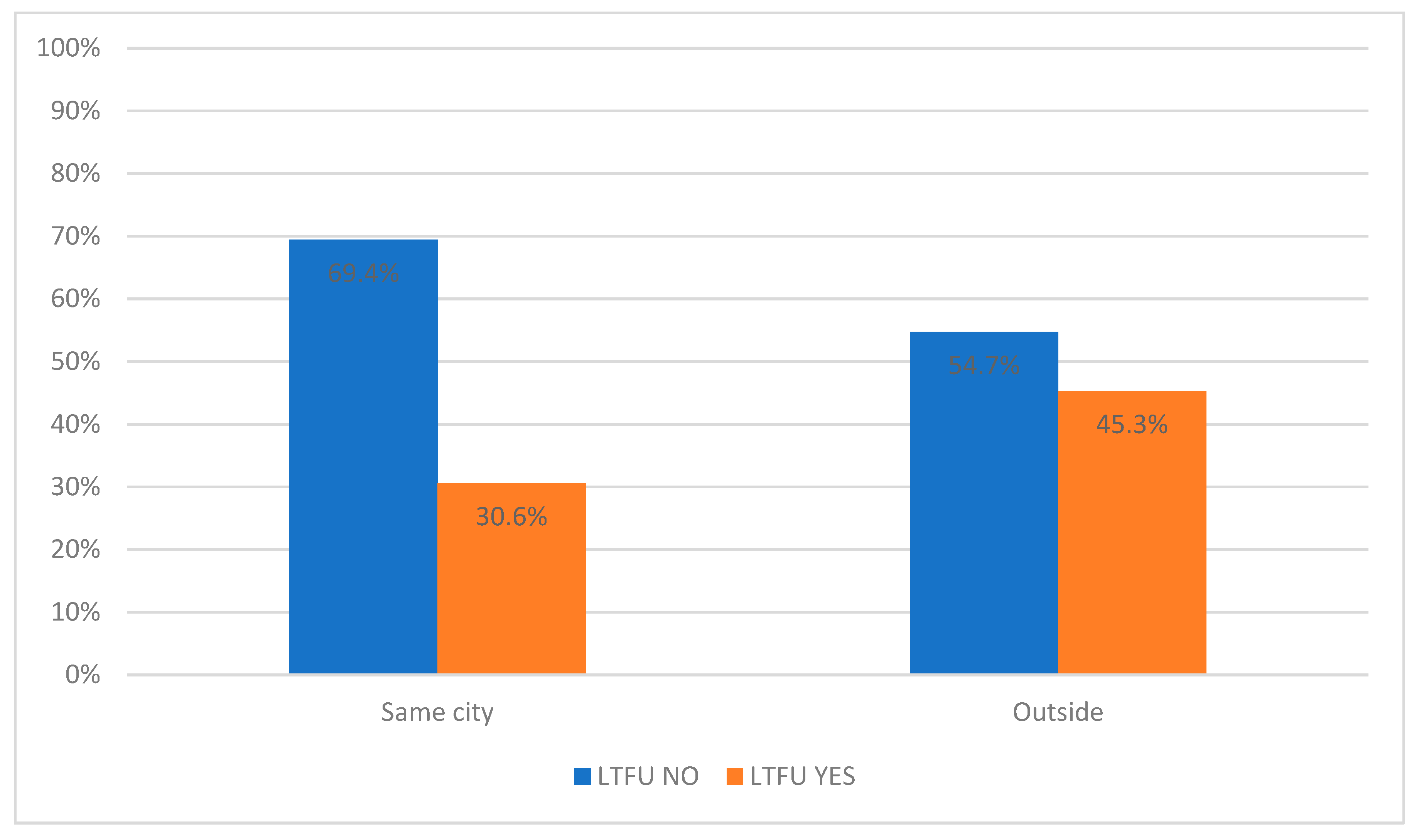
3.4. Commuting
3.5. Factors
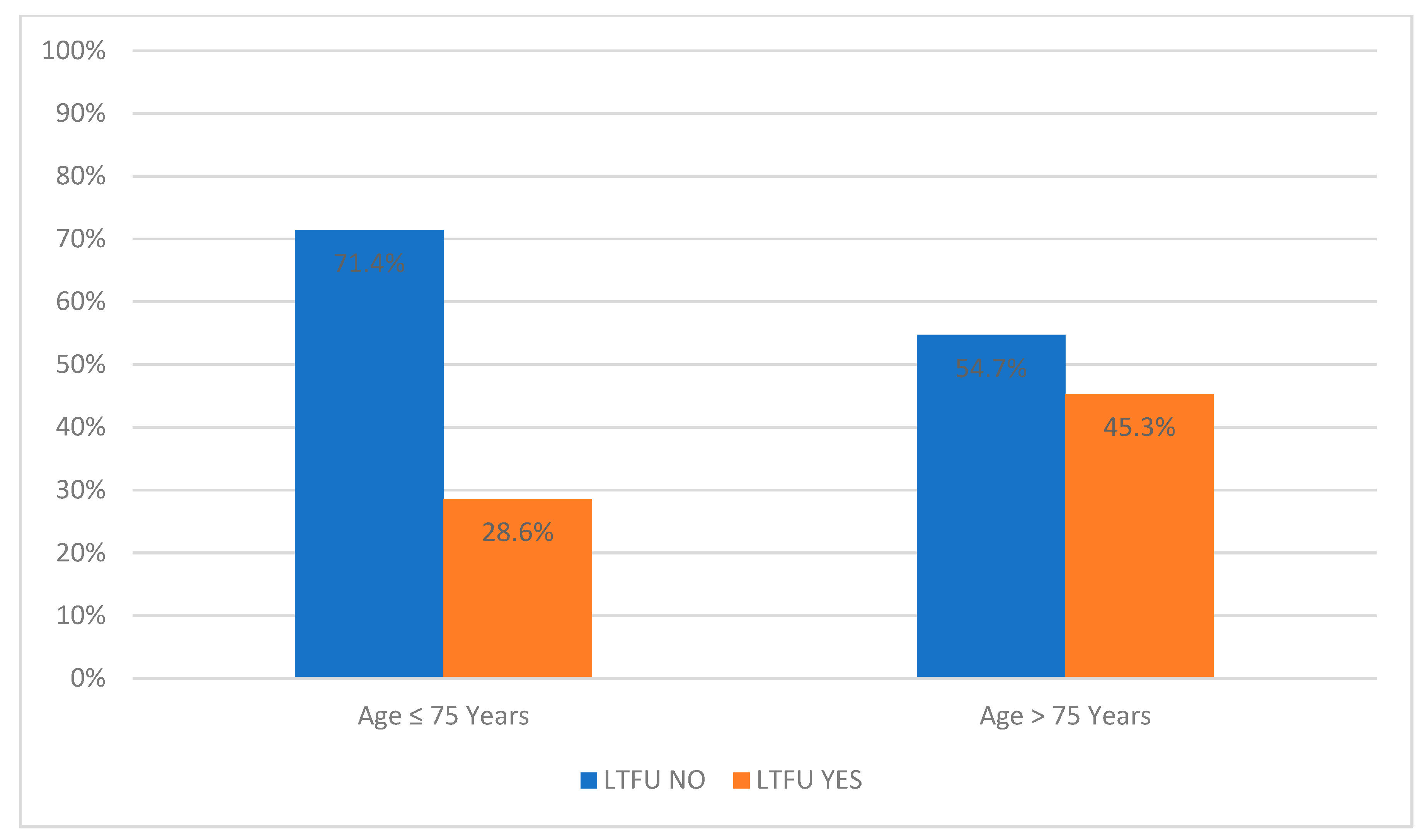
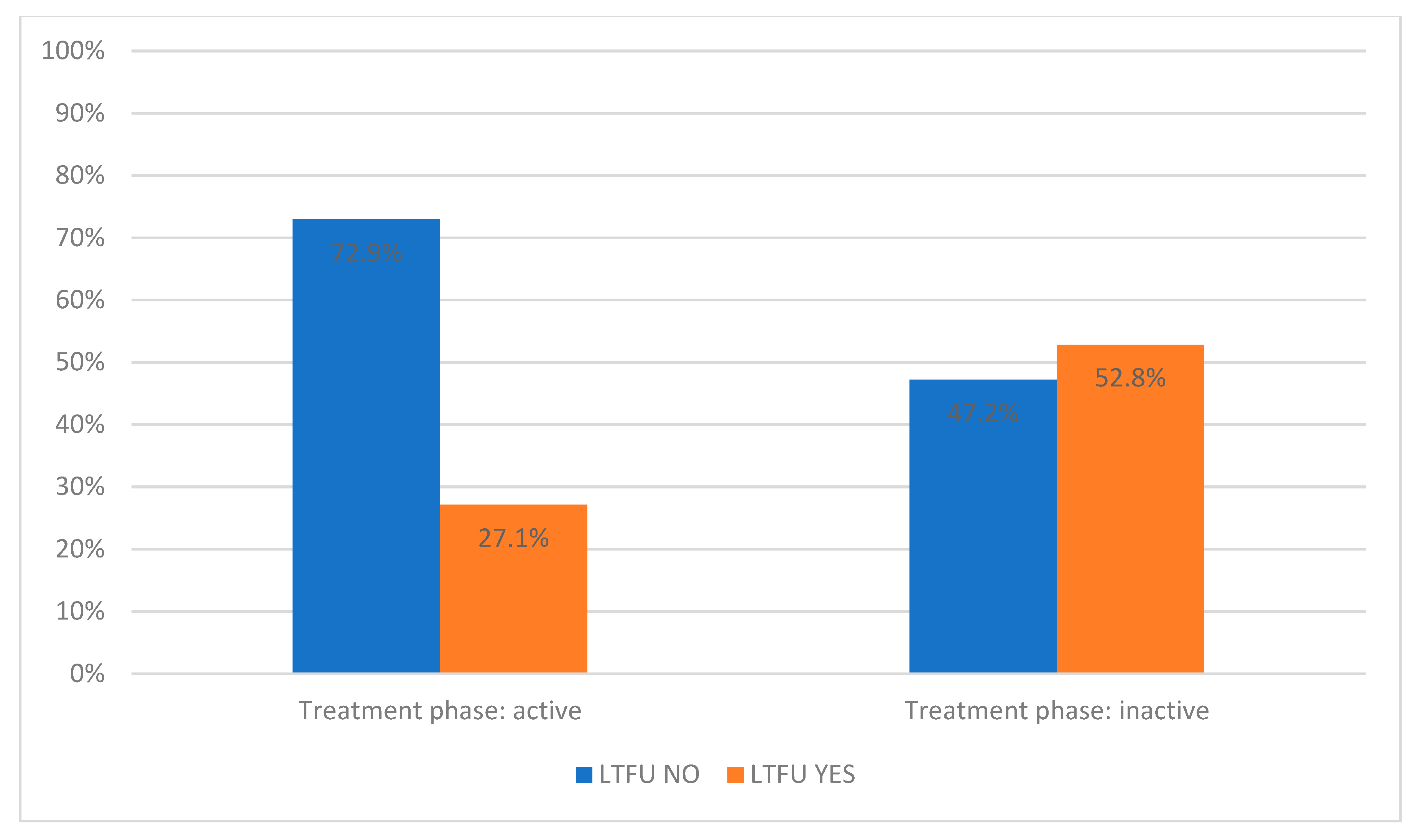
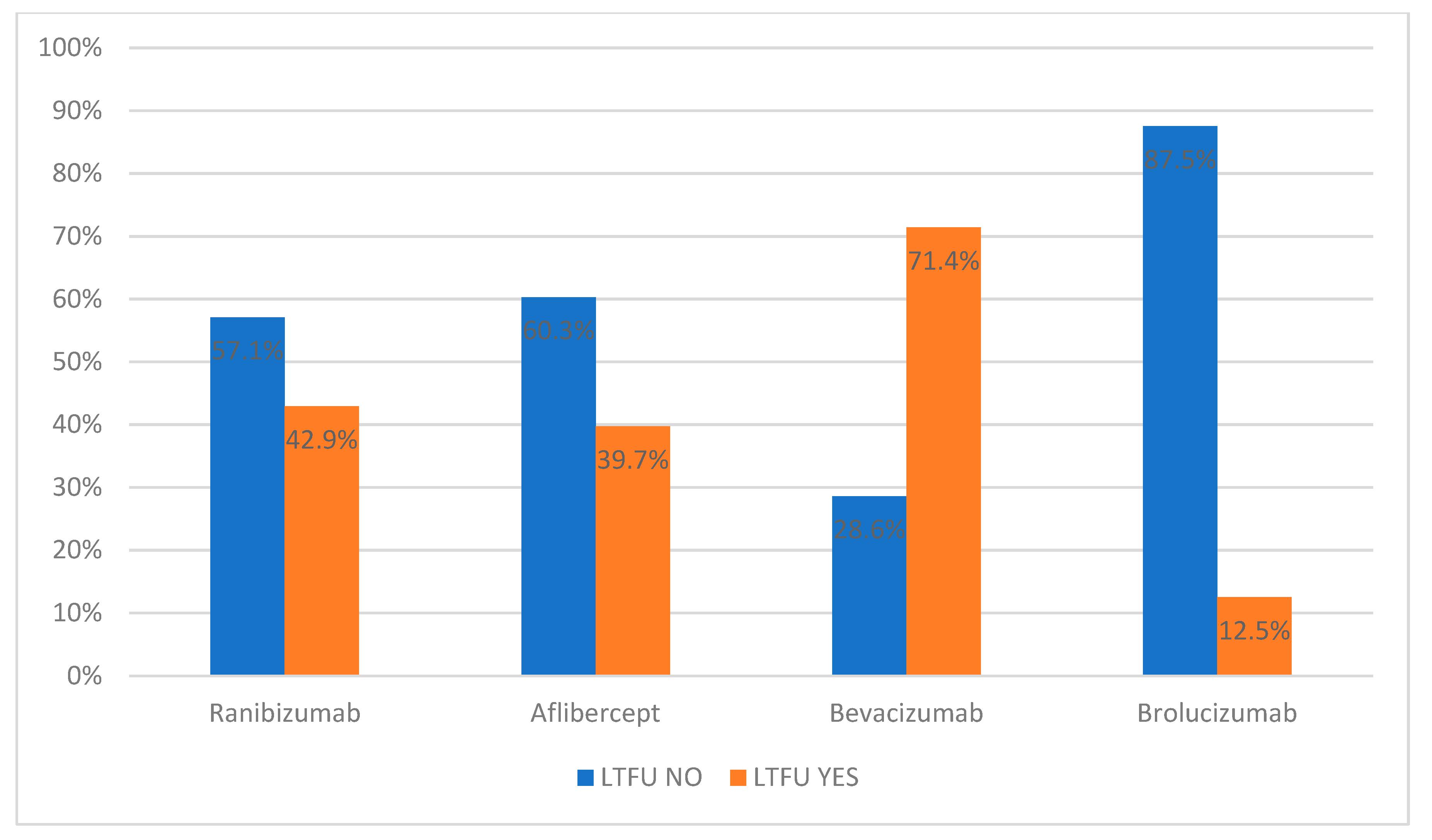
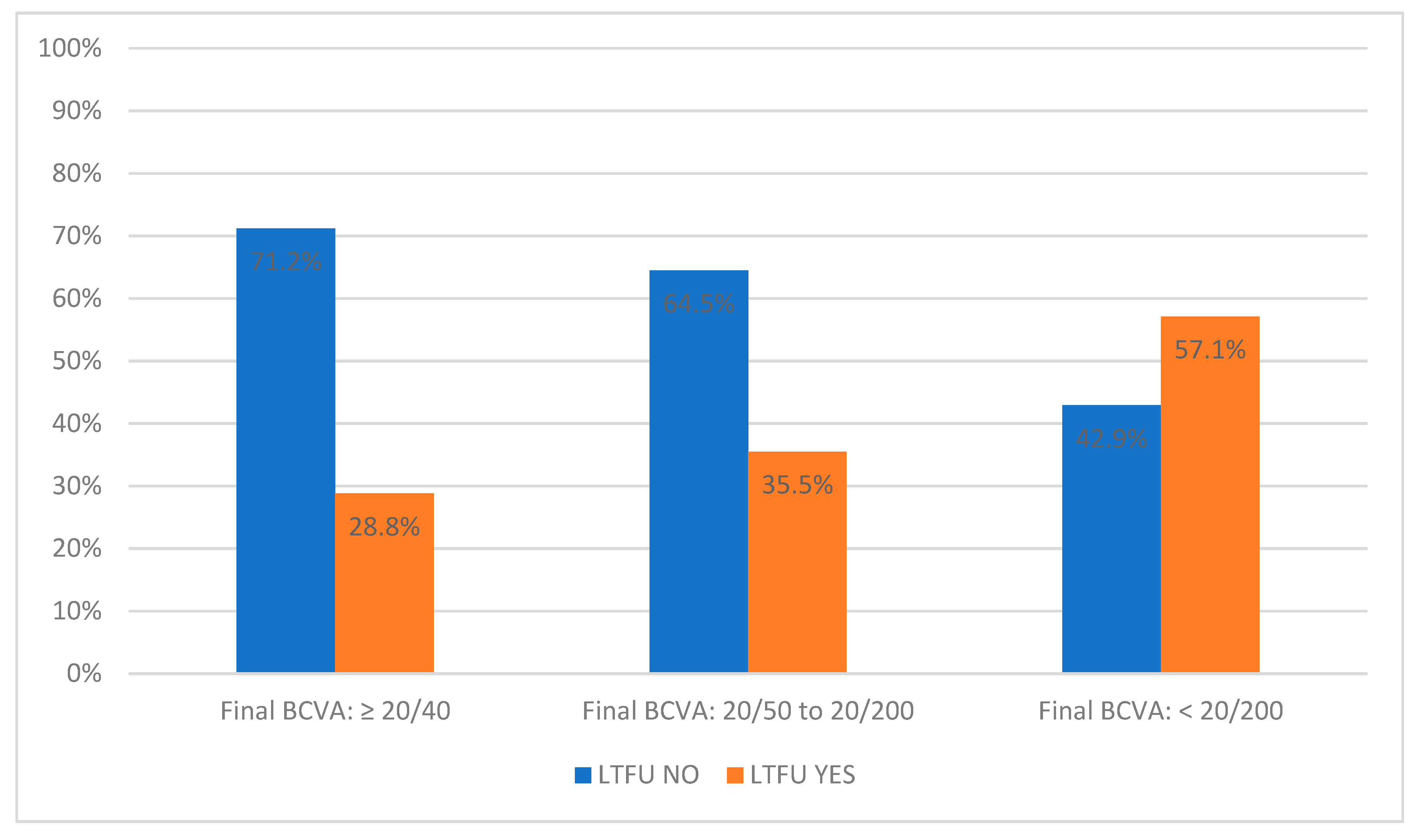
3.5.1. Significant Factors
3.5.2. Non-Significant Factors
3.5.3. Multivariate Regression
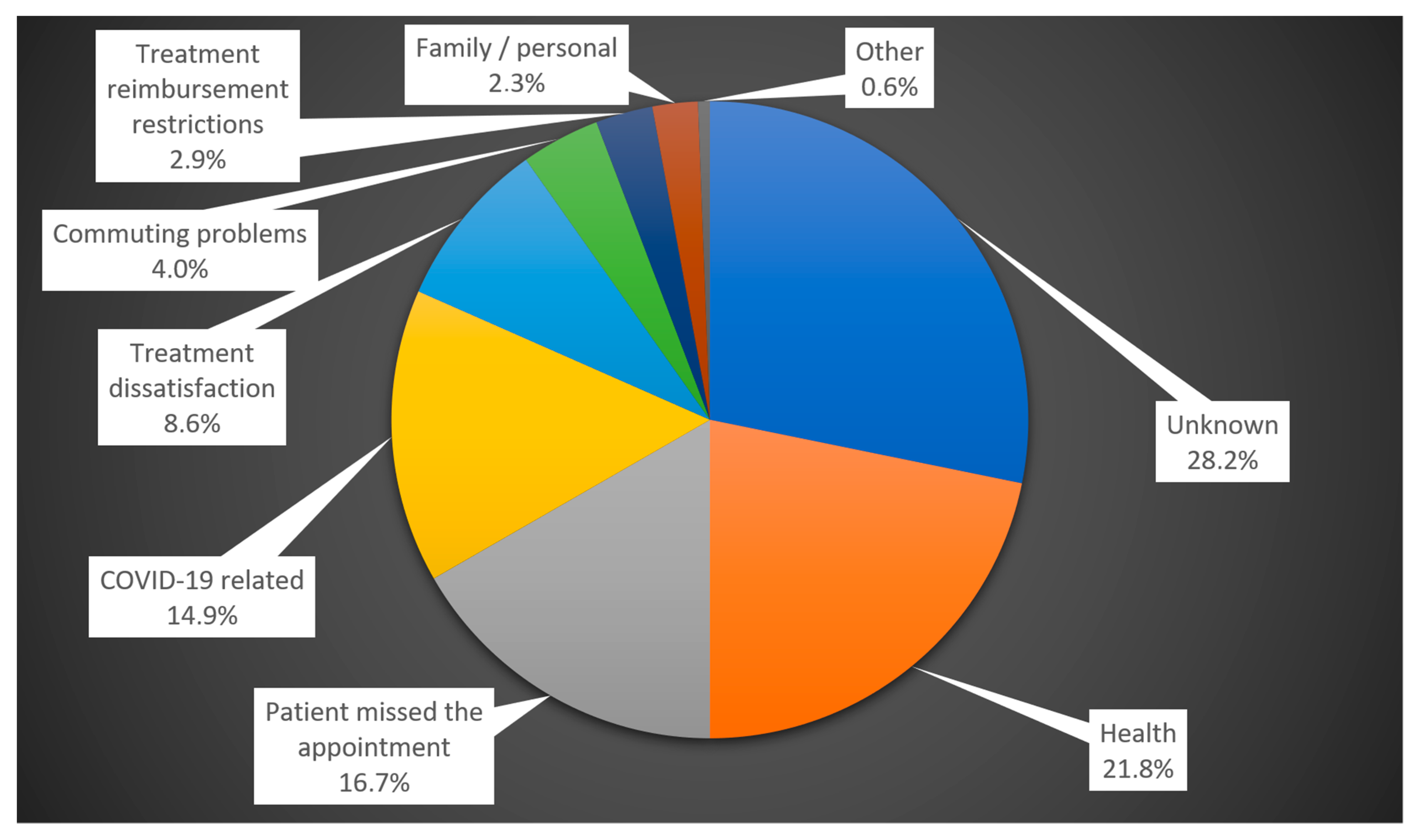
3.6. Underlying Reasons
3.6.1. Overview
3.6.2. Common Reasons for LTFU
3.6.3. Treatment Dissatisfaction
- Perceived insufficient effect of the treatment (1 patient);
- Fatigue from repeated and frequent visits (1 patient);
- Pain during application (1 patient);
- Long waiting times for application (2 patients);
- Loss of motivation for treatment (1 patient);
- No change in visual acuity (2 patients);
- The mental demands of the treatment (1 patient);
- Inability to see the purpose or benefit of the treatment (1 patient).
3.6.4. Commuting Problems
3.6.5. Less Common Reasons for LTFU
4. Discussion
4.1. Significant Findings
4.2. Age
4.3. Treatment Phase
4.4. Best-Corrected Visual Acuity
4.5. Type of Anti-VEGF Drug
4.6. Treatment Switch
4.7. Commuting Distance and the Need for an Escort during Commuting
4.8. Reasons for LTFU from a Patient’s Perspective
5. Study’s Limitations
6. Brief Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Okada, M.; Wong, T.Y.; Mitchell, P.; Eldem, B.; Talks, S.J.; Tariq, A.; Daien, V.; Rodriguez, F.J.; Gale, R.; Barratt, J.; et al. Defining Nonadherence and Non-Persistence to Anti-Vascular Endothelial Growth Factor Therapies in Neovascular Age-Related Macular Degeneration. JAMA Ophthalmol. 2021, 139, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Obeid, A.; Gao, X.; Ali, F.S.; Aderman, C.M.; Shahlaee, A.; Adam, M.K.; Kasi, S.K.; Hyman, L.; Ho, A.C.; Hsu, J. Loss to Follow-up Among Patients with Neovascular Age-Related Macular Degeneration Who Received Intravitreal Anti-Vascular Endothelial Growth Factor Injections. JAMA Ophthalmol. 2018, 136, 1251–1259. [Google Scholar] [CrossRef]
- American Academy of Ophthalmology. 2021–2022 Basic and Clinical Science Course, Section 12: Retina and Vitreous; American Academy of Ophthalmology: San Francisco, CA, USA, 2021; ISBN 978-1-68104-450-7. [Google Scholar]
- Wong, T.Y.; Chakravarthy, U.; Klein, R.; Mitchell, P.; Zlateva, G.; Buggage, R.; Fahrbach, K.; Probst, C.; Sledge, I. The Natural History and Prognosis of Neovascular Age-Related Macular Degeneration: A Systematic Review of the Literature and Meta-Analysis. Ophthalmology 2008, 115, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Stattin, M.; Ahmed, D.; Graf, A.; Haas, A.-M.; Kickinger, S.; Jacob, M.; Krepler, K.; Ansari-Shahrezaei, S. The Effect of Treatment Discontinuation During the COVID-19 Pandemic on Visual Acuity in Exudative Neovascular Age-Related Macular Degeneration: 1-Year Results. Ophthalmol. Ther. 2021, 10, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Saleh, O.A.; Jammal, H.; Alqudah, N.; Alqudah, A.; Abu-Yaghi, N. Clinical Experience in the Administration of Intravitreal Injection Therapy at a Tertiary University Hospital in Jordan During the COVID-19 Lockdown. Clin. Ophthalmol. Auckl. NZ 2020, 14, 2473–2480. [Google Scholar] [CrossRef] [PubMed]
- Stone, L.G.; Grinton, M.E.; Talks, J.S. Delayed Follow-up of Medical Retina Patients Due to COVID-19: Impact on Disease Activity and Visual Acuity. Graefes Arch. Clin. Exp. Ophthalmol. 2021, 259, 1773–1780. [Google Scholar] [CrossRef]
- Khurana, R.N.; Li, C.; Lum, F. Loss to Follow-up in Patients with Neovascular Age-Related Macular Degeneration Treated with Anti-VEGF Therapy in the United States in the IRIS® Registry. Ophthalmology 2023, 130, 672–683. [Google Scholar] [CrossRef]
- Müller, S.; Ehlken, C.; Bauer-Steinhusen, U.; Lechtenfeld, W.; Hasanbasic, Z.; Agostini, H.; Wilke, T. Treatment of Age-Related Neovascular Macular Degeneration: The Patient’s Perspective. Graefes Arch. Clin. Exp. Ophthalmol. 2017, 255, 2237–2246. [Google Scholar] [CrossRef]
- Muste, J.C.; Russell, M.W.; Iyer, A.I.; Singh, R.P. Interventions to Reduce Loss to Follow up in Common Retinal Pathology: A Systematic Review. Eur. J. Ophthalmol. 2023, 33, 1513–1516. [Google Scholar] [CrossRef]
- Lalwani, G.A.; Rosenfeld, P.J.; Fung, A.E.; Dubovy, S.R.; Michels, S.; Feuer, W.; Davis, J.L.; Flynn, H.W.; Esquiabro, M. A Variable-Dosing Regimen with Intravitreal Ranibizumab for Neovascular Age-Related Macular Degeneration: Year 2 of the PrONTO Study. Am. J. Ophthalmol. 2009, 148, 43–58.e1. [Google Scholar] [CrossRef]
- Wykoff, C.C.; Croft, D.E.; Brown, D.M.; Wang, R.; Payne, J.F.; Clark, L.; Abdelfattah, N.S.; Sadda, S.R.; TREX-AMD Study Group. Prospective Trial of Treat-and-Extend versus Monthly Dosing for Neovascular Age-Related Macular Degeneration: TREX-AMD 1-Year Results. Ophthalmology 2015, 122, 2514–2522. [Google Scholar] [CrossRef]
- Early Treatment Diabetic Retinopathy Study Research Group. Early Treatment Diabetic Retinopathy Study Design and Baseline Patient Characteristics. ETDRS Report Number 7. Ophthalmology 1991, 98, 741–756. [Google Scholar] [CrossRef]
- Brown, D.M.; Michels, M.; Kaiser, P.K.; Heier, J.S.; Sy, J.P.; Ianchulev, T.; ANCHOR Study Group. Ranibizumab versus Verteporfin Photodynamic Therapy for Neovascular Age-Related Macular Degeneration: Two-Year Results of the ANCHOR Study. Ophthalmology 2009, 116, 57–65.e5. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y.; MARINA Study Group. Ranibizumab for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.-F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal Aflibercept (VEGF Trap-Eye) in Wet Age-Related Macular Degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [CrossRef] [PubMed]
- Westborg, I.; Rosso, A. Risk Factors for Discontinuation of Treatment for Neovascular Age-Related Macular Degeneration. Ophthalmic Epidemiol. 2018, 25, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Bobykin, E.V. The influence of patient compliance with antiangiogenic therapy on its efficacy for neovascular age-related macular degeneration. Vestn. Oftalmol. 2014, 130, 88–96. [Google Scholar]
- Subhi, Y.; Sørensen, T.L. Neovascular Age-Related Macular Degeneration in the Very Old (≥90 Years): Epidemiology, Adherence to Treatment, and Comparison of Efficacy. J. Ophthalmol. 2017, 2017, 7194927. [Google Scholar] [CrossRef] [PubMed]
- Wintergerst, M.W.M.; Bouws, J.; Loss, J.; Heimes, B.; Pauleikhoff, D.; Holz, F.G.; Finger, R.P. Reasons for delayed and discontinued therapy in age-related macular degeneration. Ophthalmol. Z. Dtsch. Ophthalmol. Ges. 2018, 115, 1035–1041. [Google Scholar] [CrossRef]
- EMA. Eylea. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/eylea (accessed on 7 October 2023).
- EMA. Beovu. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/beovu (accessed on 7 October 2023).
- EMA. Lucentis. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/lucentis (accessed on 7 October 2023).
- Ministerstvo Zdravotnictva Slovenskej Republiky. Zoznam Kategorizovanych Liekov. Available online: https://www.health.gov.sk/?zoznam-kategorizovanych-liekov (accessed on 26 September 2023).
- Ehlken, C.; Helms, M.; Böhringer, D.; Agostini, H.T.; Stahl, A. Association of Treatment Adherence with Real-Life VA Outcomes in AMD, DME, and BRVO Patients. Clin. Ophthalmol. Auckl. NZ 2018, 12, 13–20. [Google Scholar] [CrossRef]
- Rasmussen, A.; Sander, B.; Larsen, M.; Brandi, S.; Fuchs, J.; Hansen, L.H.; Lund-Andersen, H. Neovascular Age-Related Macular Degeneration Treated with Ranibizumab or Aflibercept in the Same Large Clinical Setting: Visual Outcome and Number of Injections. Acta Ophthalmol. 2017, 95, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Krivosic, V.; Philippakis, E.; Couturier, A.; Dupas, B.; Erginay, A.; Desmettre, T.; Streho, M.; Bonnin, S.; Mane, V.; Jouvaud, S.; et al. A “fast track” to improve management of neovascular age related macular degeneration. J. Fr. Ophtalmol. 2017, 40, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Oishi, A.; Mandai, M.; Nishida, A.; Hata, M.; Matsuki, T.; Kurimoto, Y. Remission and Dropout Rate of Anti-VEGF Therapy for Age-Related Macular Degeneration. Eur. J. Ophthalmol. 2011, 21, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Droege, K.M.; Muether, P.S.; Hermann, M.M.; Caramoy, A.; Viebahn, U.; Kirchhof, B.; Fauser, S. Adherence to Ranibizumab Treatment for Neovascular Age-Related Macular Degeneration in Real Life. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 1281–1284. [Google Scholar] [CrossRef]
- Sii, S.; Aspinall, P.; Borooah, S.; Dhillon, B. Exploring Factors Predicting Changes in Patients’ Expectations and Psychosocial Issues during the Course of Treatment with Intravitreal Injections for Wet Age-Related Macular Degeneration. Eye Lond. Engl. 2018, 32, 673–678. [Google Scholar] [CrossRef]
- Polat, O.; İnan, S.; Özcan, S.; Doğan, M.; Küsbeci, T.; Yavaş, G.F.; İnan, Ü.Ü. Factors Affecting Compliance to Intravitreal Anti-Vascular Endothelial Growth Factor Therapy in Patients with Age-Related Macular Degeneration. Turk. J. Ophthalmol. 2017, 47, 205–210. [Google Scholar] [CrossRef]
- Vaze, A.; Fraser-Bell, S.; Gillies, M. Reasons for Discontinuation of Intravitreal Vascular Endothelial Growth Factor Inhibitors in Neovascular Age-Related Macular Degeneration. Retina 2014, 34, 1774–1778. [Google Scholar] [CrossRef]
- Nunes, R.P.; Nóbrega, M.J.; De Novelli, F.J.; Coral, S.A.; Berti, T.B.; Missen, M.M.D.; Correa, M.C. Causes of Interruption of Bevacizumab Therapy in Age-Related Macular Degeneration. Arq. Bras. Oftalmol. 2010, 73, 146–149. [Google Scholar] [CrossRef]
- EMA. Avastin. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/avastin (accessed on 7 October 2023).
- Hanemoto, T.; Hikichi, Y.; Kikuchi, N.; Kozawa, T. The Impact of Different Anti-Vascular Endothelial Growth Factor Treatment Regimens on Reducing Burden for Caregivers and Patients with Wet Age-Related Macular Degeneration in a Single-Center Real-World Japanese Setting. PLoS ONE 2017, 12, e0189035. [Google Scholar] [CrossRef]
- Yang, K.-B.; Feng, H.; Zhang, H. Effects of the COVID-19 Pandemic on Anti-Vascular Endothelial Growth Factor Treatment in China. Front. Med. 2020, 7, 576275. [Google Scholar] [CrossRef]
- Sindal, M.D.; Chhabra, K.; Khanna, V. Profile of Patients Receiving Intravitreal Anti-Vascular Endothelial Growth Factor Injections during COVID-19-Related Lockdown. Indian J. Ophthalmol. 2021, 69, 730–733. [Google Scholar] [CrossRef] [PubMed]
- Soares, R.R.; Mellen, P.; Garrigan, H.; Obeid, A.; Wibbelsman, T.D.; Borkar, D.; Ho, A.C.; Hsu, J. Outcomes of Eyes Lost to Follow-up with Neovascular Age-Related Macular Degeneration Receiving Intravitreal Anti-Vascular Endothelial Growth Factor. Ophthalmol. Retina 2020, 4, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.-B.; Liu, L.; Feng, H.; Li, J.; Liu, Z.-L.; Liu, H.-N.; Zhang, H. Outcomes of Eyes Lost to Follow-Up in Patients with Central Retinal Vein Occlusion Who Are Receiving Anti-Vascular Endothelial Growth Factor Treatment. Ther. Clin. Risk Manag. 2021, 17, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Gomi, F.; Toyoda, R.; Yoon, A.H.; Imai, K. Factors of Anti-Vascular Endothelial Growth Factor Therapy Withdrawal in Patients with Neovascular Age-Related Macular Degeneration: Implications for Improving Patient Adherence. J. Clin. Med. 2021, 10, 3106. [Google Scholar] [CrossRef]
- Okada, M.; Mitchell, P.; Finger, R.P.; Eldem, B.; Talks, S.J.; Hirst, C.; Paladini, L.; Barratt, J.; Wong, T.Y.; Loewenstein, A. Nonadherence or Non-Persistence to Intravitreal Injection Therapy for Neovascular Age-Related Macular Degeneration: A Mixed-Methods Systematic Review. Ophthalmology 2021, 128, 234–247. [Google Scholar] [CrossRef]
| Factor | LTFU NO | LTFU YES | Significance |
|---|---|---|---|
| Sex | Men: 118 (63.4% of all men) | Men: 68 (36.6% of all men) | p = 0.923 (NS) |
| Women: 180 (62.9% of all women) | Women: 106 (37.1% of all women) | ||
| Age | 75.0 (69.0–80.0) | 77.0 (71.0–83.0) | p = 0.003 |
| Age above/under 75 years | ≤75 years: 170 (71.4%) | ≤75 years: 68 (28.6%) | p < 0.001 |
| >75 years: 128 (54.7%) | >75 years: 106 (45.3%) | ||
| Patient’s residence in the same city as the application center/outside | Same city: 172 (69.4%) | Same city: 76 (30.6%) | p = 0.004 |
| Outside: 126 (56.3%) | Outside: 98 (43.7%) | ||
| Commuting distance (km) | 10.0 (10.0–40.0) | 22.0 (10.0–54.0) | p = 0.004 |
| Escort needed when commuting | Yes: 72 (49.0%) | Yes: 75 (51.0%) | p < 0.001 |
| No: 162 (83.9%) | No: 31 (16.1%) | ||
| Unknown: 64 (48.5%) | Unknown: 68 (51.5%) |
| Factor | LTFU NO | LTFU YES | Significance |
|---|---|---|---|
| Treatment phase | Active: 213 (72.9%) | Active: 79 (27.1%) | p < 0.001 |
| Inactive: 85 (47.2%) | Inactive: 95 (52.8%) | ||
| Length of follow-up (months) | 47.0 (26.0–68.3) | 42.5 (16.0–72.3) | p = 0.228 (NS) |
| Time since last injection (days) | 0.0 (0.0–199.5) | 207.5 (0.0–1048.3) | p < 0.001 |
| Anti-VEGF drug (non-switched patients) * | Ranibizumab: 140 (57.1%) | Ranibizumab: 105 (42.9%) | p = 0.001 |
| Aflibercept: 47 (60.3%) | Aflibercept: 31 (39.7%) | ||
| Bevacizumab: 2 (28.6%) | Bevacizumab: 5 (71.4%) | ||
| Brolucizumab: 7 (87.5%) | Brolucizumab: 1 (12.5%) | ||
| Switch of therapy | Yes: 91 (75.2%) | Yes: 30 (24.8%) | p = 0.001 |
| No: 207 (59.0%) | No: 144 (41.0%) | ||
| Bilateral anti-VEGF | Yes: 91 (68.4%) | Yes: 42 (31.6%) | p = 0.140 (NS) |
| No: 207 (61.1%) | No: 132 (38.9%) |
| Factor | LTFU NO | LTFU YES | Significance |
|---|---|---|---|
| Baseline BCVA (first treated eye) | 60.0 (50.0–70.0) | 55.0 (37.8–68.3) | p = 0.004 |
| Final BCVA (first treated eye) | 64.0 (40.8–74.0) | 44.5 (26.0–72.0) | p < 0.001 |
| BCVA change (first treated eye) | +1.0 (−13.0–10.3) | −2.0 (−20.0–7.0) | p = 0.017 |
| Baseline BCVA (second treated eye in bilateral treatment) | 70.0 (58.0–76.5) | 66.5 (57.0–73.3) | p = 0.097 (NS) |
| Final BCVA (second treated eye in bilateral treatment) | 70.0 (55.0–77.0) | 66.5 (49.0–72.0) | p = 0.078 (NS) |
| BCVA change (second treated eye in bilateral treatment) | +0.0 (−7.3–7.0) | −1.0 (−13.0–5.0) | p = 0.531 (NS) |
| Final BCVA (in bilateral treatment, the better-seeing eye) | 69.0 (53.0–75.0) | 57.5 (30.0–73.0) | p < 0.001 |
| BCVA change (in bilateral treatment, the better-seeing eye) | +4.0 (−7.0–11.0) | +0.0 (−13.3–8.3) | p = 0.015 |
| Final BCVA—categories (in bilateral treatment, the better-seeing eye) | ≥20/40: 141 (71.2%) | ≥20/40: 57 (28.8%) | p < 0.001 |
| ≥20/200 to ≤20/50: 118 (64.5%) | ≥20/200 to ≤20/50: 65 (35.5%) | ||
| <20/200: 39 (42.9%) | <20/200: 52 (57.1%) | ||
| Final BCVA of the treated eye versus the other | Worse: 126 (59.2%) | Worse: 87 (40.8%) | p = 0.316 (NS) |
| Same: 29 (61.7%) | Same: 18 (38.3%) | ||
| Better: 58 (65.2%) | Better: 31 (34.8%) | ||
| BCVA change—categories (first treated eye) | Treatment failure: 67 (54.5%) | Treatment failure: 56 (45.5%) | p = 0.137 (NS) |
| Deterioration: 30 (65.2%) | Deterioration: 16 (34.8%) | ||
| Stabilization: 84 (62.7%) | Stabilization: 50 (37.3%) | ||
| Improvement: 65 (67.7%) | Improvement: 31 (32.3%) | ||
| Super responders: 52 (71.2%) | Super responders: 21 (28.8%) |
| Parameter | B +/− S.E. | Wald Score | Exp(B) (95% CI) | Significance |
|---|---|---|---|---|
| Escort needed when commuting NO | - | 1 | p < 0.001 | |
| Escort needed when commuting YES | 1.778 ± 0.266 | 44.704 | 5.915 (3.513–9.960) | p < 0.001 |
| Escort needed when commuting UNKNOWN | 1.596 ± 0.270 | 34.976 | 4.935 (2.907–8.375) | p < 0.001 |
| Treatment phase ACTIVE | - | 1 | p < 0.001 | |
| Treatment phase INACTIVE | 1.109 ± 0.217 | 26.130 | 3.030 (1.981–4.635) | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kusenda, P.; Caprnda, M.; Gabrielova, Z.; Kukova, N.; Pavlovic, S.; Stefanickova, J. Understanding Loss to Follow-Up in AMD Patients Receiving VEGF Inhibitor Therapy: Associated Factors and Underlying Reasons. Diagnostics 2024, 14, 400. https://doi.org/10.3390/diagnostics14040400
Kusenda P, Caprnda M, Gabrielova Z, Kukova N, Pavlovic S, Stefanickova J. Understanding Loss to Follow-Up in AMD Patients Receiving VEGF Inhibitor Therapy: Associated Factors and Underlying Reasons. Diagnostics. 2024; 14(4):400. https://doi.org/10.3390/diagnostics14040400
Chicago/Turabian StyleKusenda, Pavol, Martin Caprnda, Zuzana Gabrielova, Natalia Kukova, Samuel Pavlovic, and Jana Stefanickova. 2024. "Understanding Loss to Follow-Up in AMD Patients Receiving VEGF Inhibitor Therapy: Associated Factors and Underlying Reasons" Diagnostics 14, no. 4: 400. https://doi.org/10.3390/diagnostics14040400
APA StyleKusenda, P., Caprnda, M., Gabrielova, Z., Kukova, N., Pavlovic, S., & Stefanickova, J. (2024). Understanding Loss to Follow-Up in AMD Patients Receiving VEGF Inhibitor Therapy: Associated Factors and Underlying Reasons. Diagnostics, 14(4), 400. https://doi.org/10.3390/diagnostics14040400






