Comparative Morphometric Study of the Occipital Condyle in Class III and Class I Skeletal Malocclusion Patients
Abstract
1. Introduction
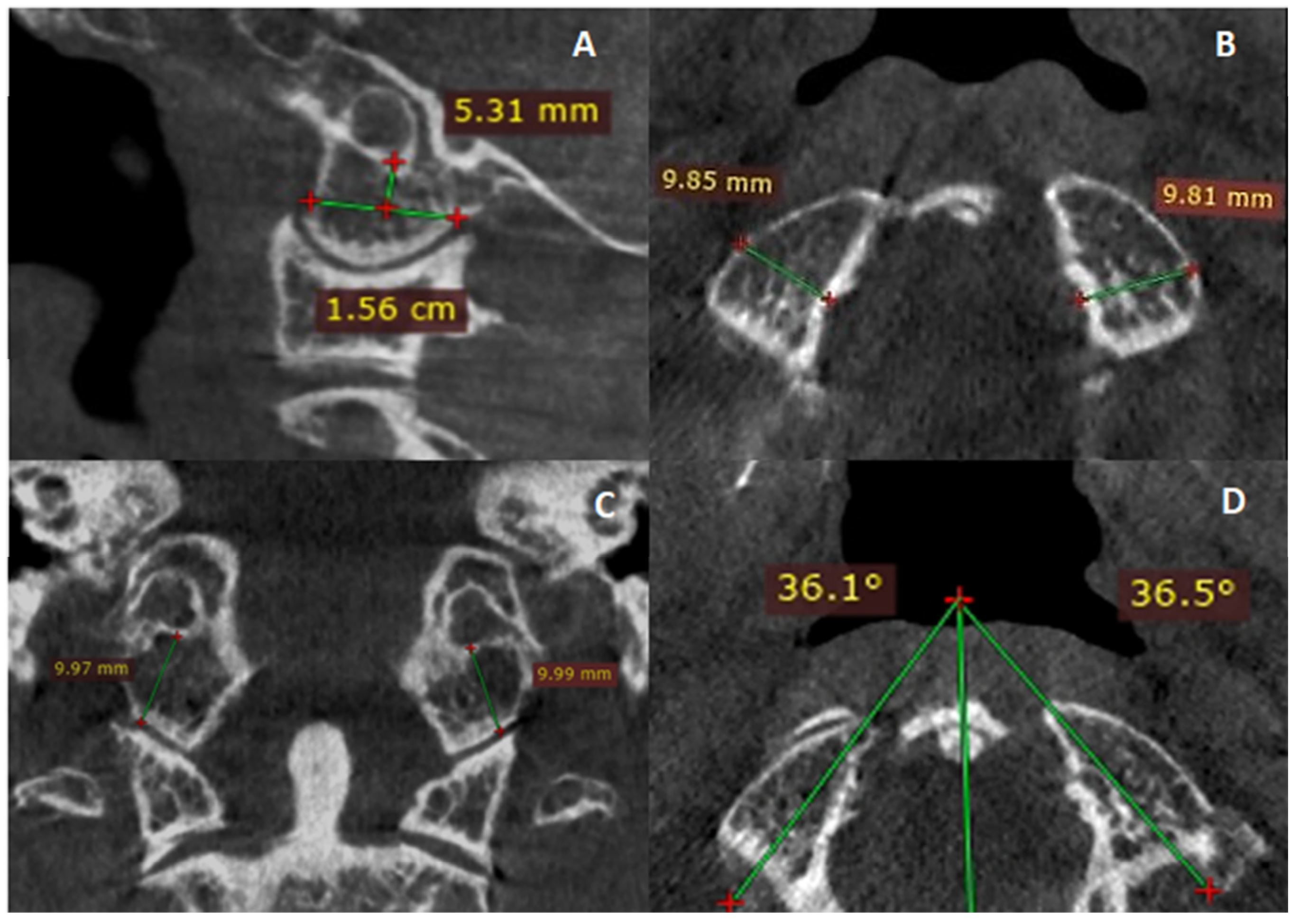
2. Materials and Methods
Statistical Analysis
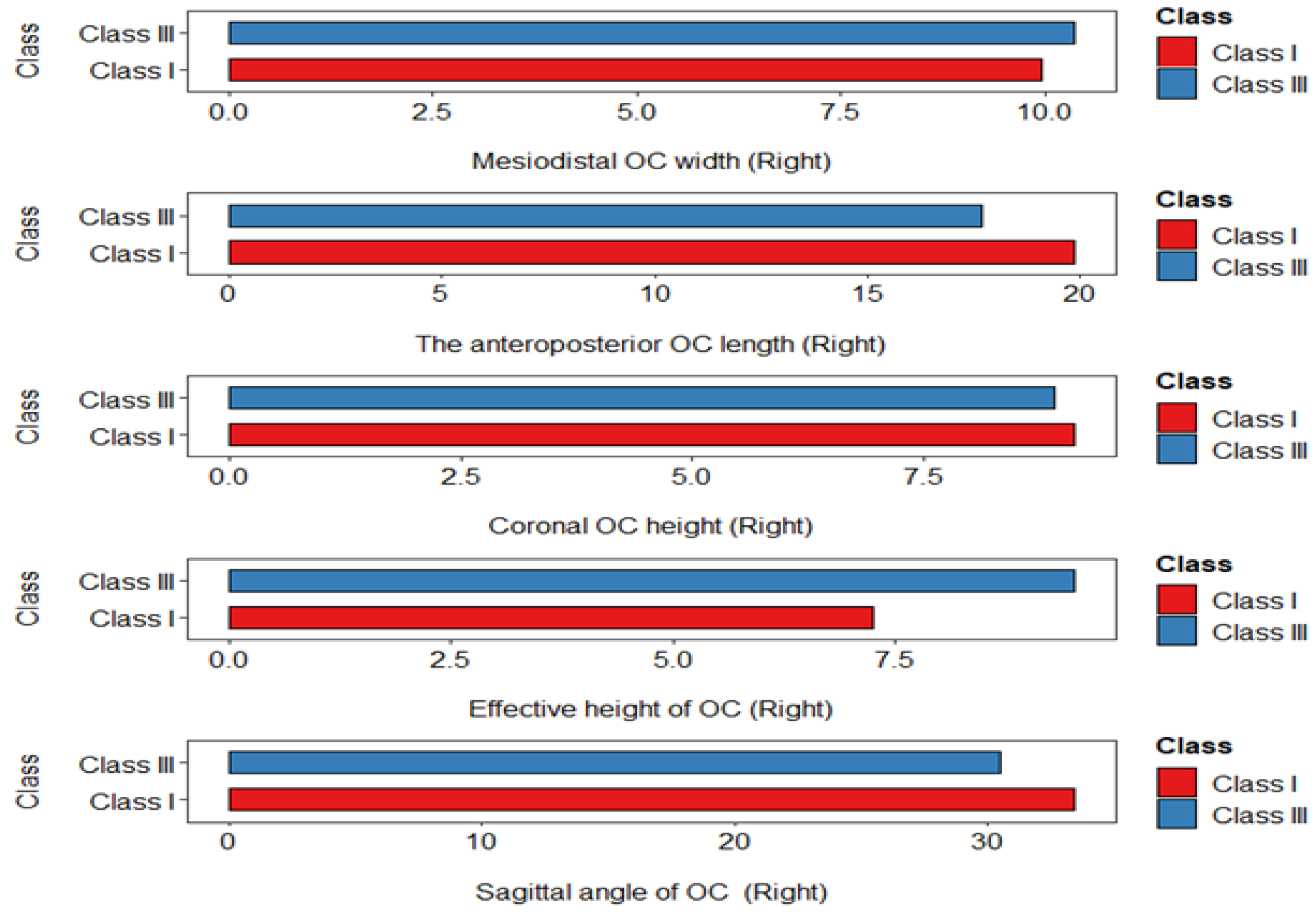
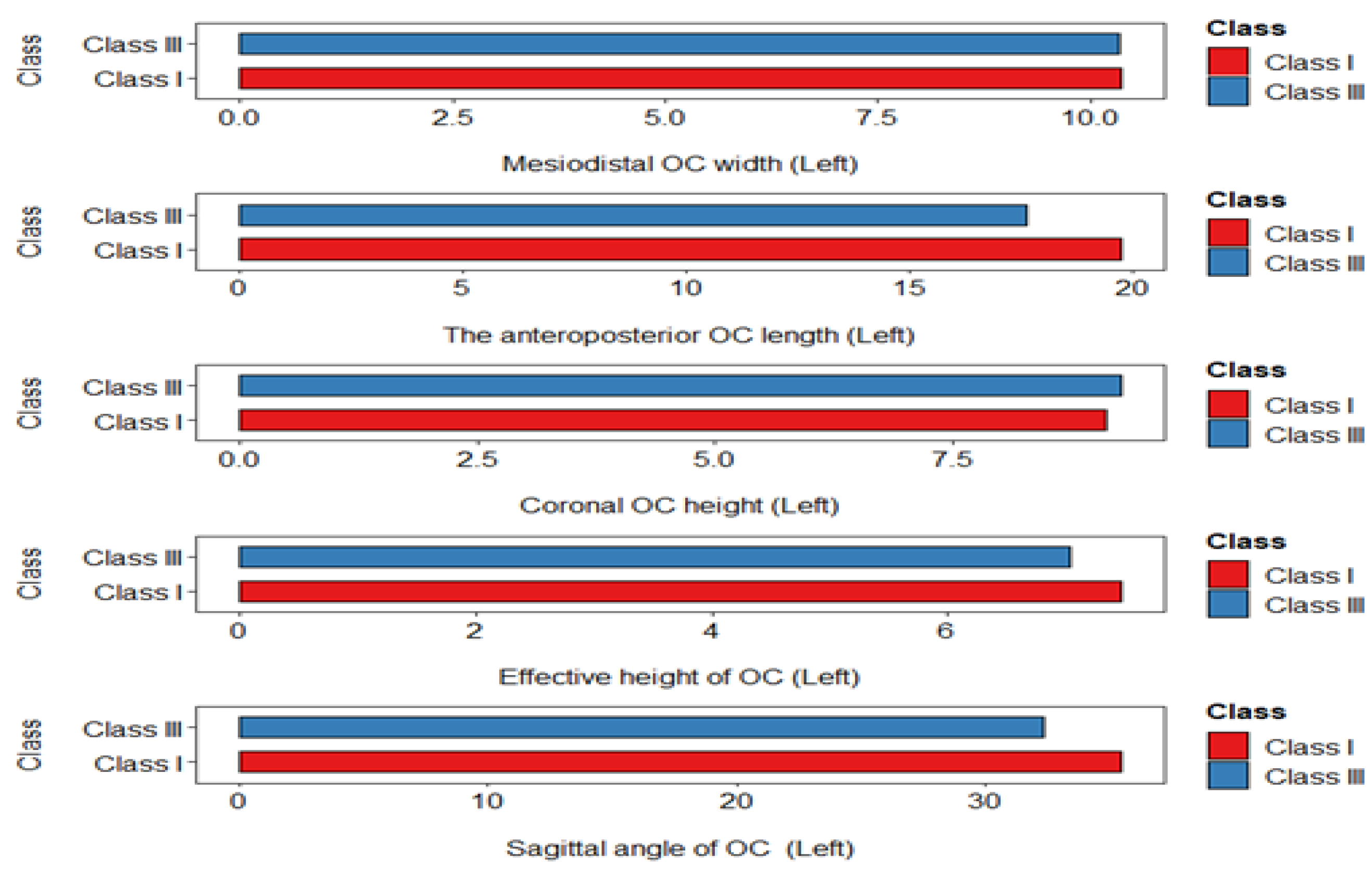
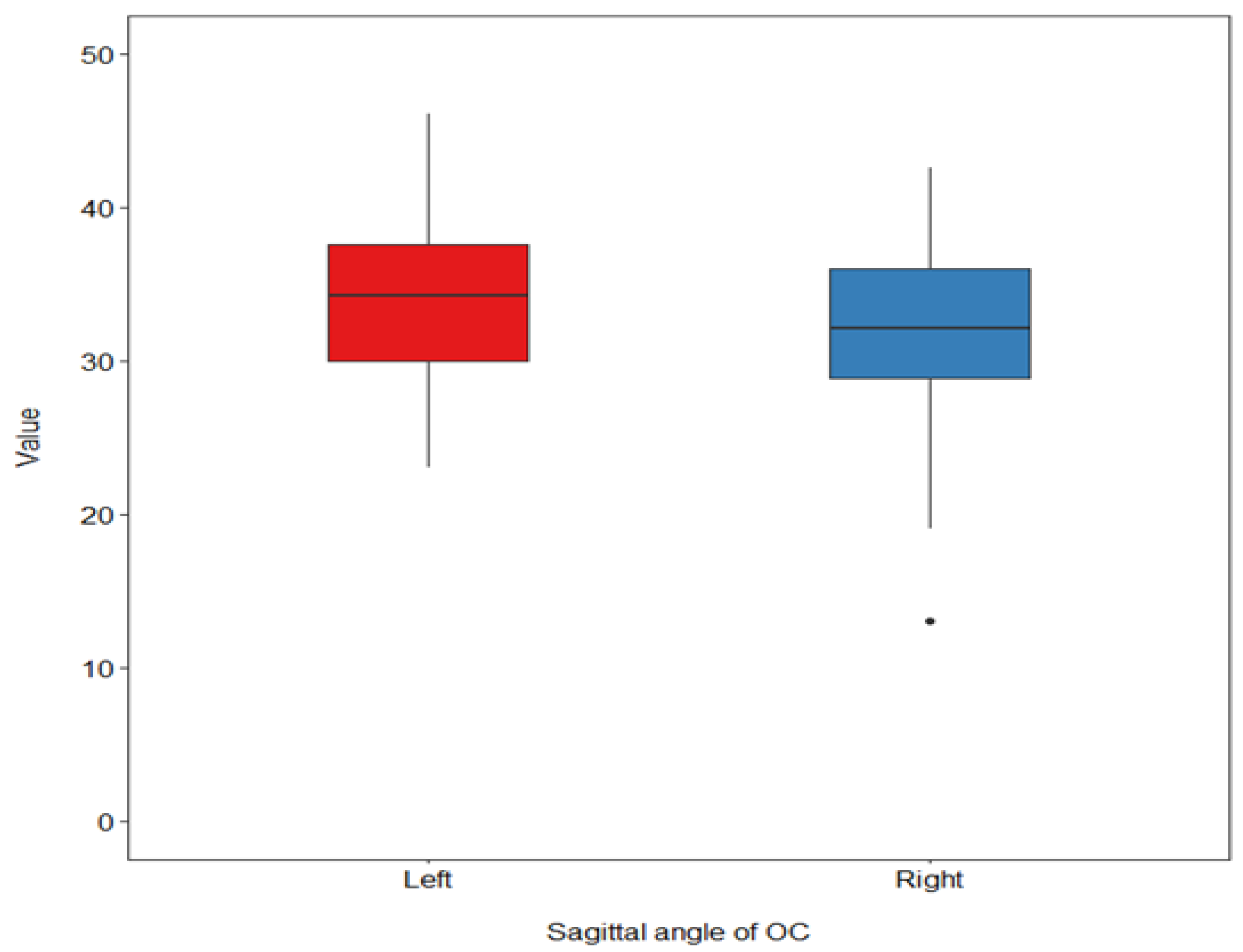
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Angle, E.H. Classification of malocclusion. Dent. Cosmos. 1899, 41, 350–375. [Google Scholar]
- Ngan, P.; Moon, W. Evolution of Class III treatment in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 22–36. [Google Scholar] [CrossRef] [PubMed]
- Standerwick, R.G.; Roberts, W.E. The aponeurotic tension model of craniofacial growth in man. Open Dent. J. 2009, 3, 100–113. [Google Scholar] [CrossRef] [PubMed]
- Thiesen, G.; Pletsch, G.; Zastrow, M.D.; Valle, C.V.M.D.; Valle-Corotti, K.M.D.; Patel, M.P.; Conti, P.C.R. Comparative analysis of the anterior and posterior length and deflection angle of the cranial base, in individuals with facial Pattern I, II and III. Dent. Press J. Orthod. 2013, 18, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Brodie, A.G., Jr. The behavior of the cranial base and its components as revealed by serial cephalometric roentgenograms. Angle Orthod. 1955, 25, 148–160. [Google Scholar]
- Kasai, K.; Moro, T.; Kanazawa, E.; Iwasawa, T. Relationship between cranial base and maxillofacial morphology. Eur. J. Orthod. 1995, 17, 403–410. [Google Scholar] [CrossRef]
- Smartt, J.M., Jr.; Elliott, R.M.; Reid, R.R.; Bartlett, S.P. Analysis of differences in the cranial base and facial skeleton of patients with lambdoid synostosis and deformational plagiocephaly. Plast. Reconstr. Surg. 2011, 127, 303–312. [Google Scholar] [CrossRef]
- Moyers, R. Etiologia da maloclusão. In Moyers RE. Ortodontia, 4th ed.; Guanabara Koogan: Rio de Janeiro, Brazil, 1991; pp. 212–237. [Google Scholar]
- Enlow, D. O processo do crescimento facial. In Crescimento Facial, 3rd ed.; Artes Médicas: São Paulo, Brazil, 1993; pp. 72–73. [Google Scholar]
- Enlow, D.H.; Moyers, R.E. Handbook of Facial Growth; WB Saunders Company: Philadelphia, PA, USA, 1982. [Google Scholar]
- Proff, P.; Will, F.; Bokan, I.; Fanghänel, J.; Gedrange, T. Cranial base features in skeletal Class III patients. Angle Orthod. 2008, 78, 433–439. [Google Scholar] [CrossRef]
- Marquez, I.M. Avaliaçäo do Padräo Facial, Preparo Ortodôntico e Capacidade do Tratamento Cirúrgico em Pacientes Classe III com Prognatismo Mandibular. Ph.D. Thesis, Universidade de São Paulo, Bauru, Brazil, 1994. [Google Scholar]
- Chin, A.; Perry, S.; Liao, C.; Yang, Y. The relationship between the cranial base and jaw base in a Chinese population. Head Face Med. 2014, 10, 31. [Google Scholar] [CrossRef]
- Sanborn, R.T. Differences between the facial skeletal patterns of Class III malocclusion and normal occlusion. Angle Orthod. 1955, 25, 208–222. [Google Scholar]
- Ferner, H.; Staubesand, J. Sobotta-Atlas de Anatomia Humana; Ed. Médica Panamericana: Madrid, Spain, 1984; p. 386. [Google Scholar]
- Ebraheim, N.A.; Lu, J.; Biyani, A.; Brown, J.A.; Yeasting, R.A. An anatomic study of the thickness of the occipital bone. Implications for occipitocervical instrumentation. Spine 1996, 21, 1725–1729; discussion 1729–1730. [Google Scholar] [CrossRef] [PubMed]
- Singh, O.; Joe, M.D. Anatomy, Head and Neck, Jugular Foramen; StatPearls Publishing LLC: Treasure Island, FL, USA, 2019. [Google Scholar]
- Smucker, J.D.; Sasso, R.C. The evolution of spinal instrumentation for the management of occipital cervical and cervicothoracic junctional injuries. Spine 2006, 31, S44–S52; discussion S61. [Google Scholar] [CrossRef] [PubMed]
- Stock, G.H.; Vaccaro, A.R.; Brown, A.K.; Anderson, P.A. Contemporary posterior occipital fixation. J. Bone Jt. Surg. Am. 2006, 88, 1642–1649. [Google Scholar] [CrossRef] [PubMed]
- Bosco, A.; Venugopal, P.; Shetty, A.P.; Shanmuganathan, R.; Kanna, R.M. Morphometric evaluation of occipital condyles: Defining optimal trajectories and safe screw lengths for occipital condyle-based occipitocervical fixation in indian population. Asian Spine J. 2018, 12, 214–223. [Google Scholar] [CrossRef]
- Naderi, S.; Korman, E.; Citak, G.; Guvencer, M.; Arman, C.; Senoglu, M.; Tetik, S.; Arda, M.N. Morphometric analysis of human occipital condyle. Clin. Neurol. Neurosurg. 2005, 107, 191–199. [Google Scholar] [CrossRef]
- Uribe, J.S.; Ramos, E.; Vale, F. Feasibility of occipital condyle screw placement for occipitocervical fixation: A cadaveric study and description of a novel technique. J. Spinal Disord. Tech. 2008, 21, 540–546. [Google Scholar] [CrossRef]
- Sanggarnjanavanich, S.; Sekiya, T.; Nomura, Y.; Nakayama, T.; Hanada, N.; Nakamura, Y. Cranial-base morphology in adults with skeletal Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 82–91. [Google Scholar] [CrossRef]
- Srivastava, A.; Nanda, G.; Mahajan, R.; Nanda, A.; Mishra, N.; Karmaran, S.; Batra, S.; Chhabra, H.S. Computed tomography-based occipital condyle morphometry in an Indian population to assess the feasibility of condylar screws for occipitocervical fusion. Asian Spine J. 2017, 11, 847–853. [Google Scholar] [CrossRef]
- Degno, S.; Abrha, M.; Asmare, Y.; Muche, A. Anatomical variation in morphometry and morphology of the foramen magnum and occipital condyle in dried adult skulls. J. Craniofac. Surg. 2019, 30, 256–259. [Google Scholar] [CrossRef]
- Le, T.V.; Dakwar, E.; Hann, S.; Effio, E.; Baaj, A.A.; Martinez, C.; Vale, F.L.; Uribe, J.S. Computed tomography-based morphometric analysis of the human occipital condyle for occipital condyle-cervical fusion. J. Neurosurg. Spine 2011, 15, 328–331. [Google Scholar] [CrossRef]
- Gumussoy, I.; Duman, S.B. Morphometric analysis of occipital condyles using alternative imaging technique. Surg. Radiol. Anat. 2020, 42, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, C.; Giuntini, V.; Defraia, E.; Baccetti, T. Glenoid fossa position in Class III malocclusion associated with mandibular protrusion. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Kerr, W.J.S.; Philip Adams, C. Cranial base and jaw relationship. Am. J. Phys. Anthropol. 1988, 77, 213–220. [Google Scholar] [CrossRef]
- Chang, H.P.; Chou, T.M.; Hsieh, S.H.; Tseng, Y.C. Cranial-base morphology in children with class III malocclusion. Kaohsiung J. Med. Sci. 2005, 21, 159–165. [Google Scholar] [CrossRef]
- Singh, G.; McNamara, J.; Lozanoff, S. Finite element analysis of the cranial base in subjects with Class III malocclusion. Br. J. Orthod. 1997, 24, 103–112. [Google Scholar] [CrossRef]
- Horowitz, S.; Converse, J.; Gerstman, L. Craniofacial relationships in mandibular prognathism. Arch. Oral Biol. 1969, 14, 121–131. [Google Scholar] [CrossRef]
- Triwardhani, A.; Effendi, A.R.; Ardani, I.G.A.W.; Utami, R.N. Correlation between the Variation of Head Type and Malocclusion: A Scooping Review. J. Int. Oral Health 2023, 15, 8–14. [Google Scholar] [CrossRef]
- Moullas, A.T.; Palomo, J.M.; Gass, J.R.; Amberman, B.D.; White, J.; Gustovich, D. Nonsurgical treatment of a patient with a Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2006, 129, S111–S118. [Google Scholar] [CrossRef]
- Xue, F.; Wong, R.W.; Rabie, A.B. Genes, genetics, and Class III malocclusion. Orthod. Craniofac. Res. 2010, 13, 69–74. [Google Scholar] [CrossRef]
- Callewaert, F.; Sinnesael, M.; Gielen, E.; Boonen, S.; Vanderschueren, D. Skeletal sexual dimorphism: Relative contribution of sex steroids, GH-IGF1, and mechanical loading. J. Endocrinol. 2010, 207, 127–134. [Google Scholar] [CrossRef]
- Björk, A. Cranial base development: A follow-up x-ray study of the individual variation in growth occurring between the ages of 12 and 20 years and its relation to brain case and face development. Am. J. Orthod. 1955, 41, 198–225. [Google Scholar] [CrossRef]
- Bjork, A. The face in profile: An anthropological X-ray investigation on Swedish children and conscripts. Sven. Tandläk.-Tidskr. 1947, 40, 180. [Google Scholar]
- Ricketts, R.M. A foundation for cephalometric communication. Am. J. Orthod. 1960, 46, 330–357. [Google Scholar] [CrossRef]
- Mouakeh, M. Cephalometric evaluation of craniofacial pattern of Syrian children with Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 640–649. [Google Scholar] [CrossRef]
- Singh, G.D.; McNamara, J.A., Jr.; Lozanoff, S. Morphometry of the cranial base in subjects with Class III malocclusion. J. Dent. Res. 1997, 76, 694–703. [Google Scholar] [CrossRef]
- Kim, S.-J.; Lee, K.-J.; Lee, S.-H.; Baik, H.-S. Morphologic relationship between the cranial base and the mandible in patients with facial asymmetry and mandibular prognathism. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 330–340. [Google Scholar] [CrossRef]
- Kluba, S.; Roßkopf, F.; Kraut, W.; Peters, J.P.; Calgeer, B.; Reinert, S.; Krimmel, M. Malocclusion in the primary dentition in children with and without deformational plagiocephaly. Clin. Oral. Investig. 2016, 20, 2395–2401. [Google Scholar] [CrossRef]
- Almeida, K.C.M.D.; Raveli, T.B.; Vieira, C.I.V.; Santos-Pinto, A.D.; Raveli, D.B. Influence of the cranial base flexion on Class I, II and III malocclusions: A systematic review. Dent. Press J. Orthod. 2017, 22, 56–66. [Google Scholar] [CrossRef]
- Dhopatkar, A.; Bhatia, S.; Rock, P. An Investigation Into the Relationship Between theCranial Base Angle and Malocclusion. Angle Orthod. 2002, 72, 456–463. [Google Scholar]
- Baumler, C.; Leboucq, N.; Captier, G. Mandibular asymmetry in plagiocephaly without synostosis. Rev. Stomatol. Chir. Maxillofac. 2007, 108, 424–430. [Google Scholar] [CrossRef]
- Hwang, S.W.; Gressot, L.V.; Chern, J.J.; Relyea, K.; Jea, A. Complications of occipital screw placement for occipitocervical fusion in children. J. Neurosurg. Pediatr. 2012, 9, 586–593. [Google Scholar] [CrossRef] [PubMed]
| Variable | Level | Class I n = 38 | Class III n = 38 | p |
|---|---|---|---|---|
| Gender (%) | Female | 19 (50.0) | 19 (50.0) | 1 |
| Male | 19 (50.0) | 19 (50.0) | ||
| Age (mean (SD)) | 22.45 (3.77) | 22.32 (5.08) | 0.898 |
| Class I | Class III | Mean Difference | p-Value | |
|---|---|---|---|---|
| Right | ||||
| OC-MDW | 9.96 (1.30) | 10.36 (1.32) | −0.4 | 0.190 |
| OC-SL | 19.84 (2.07) | 17.67 (2.48) | 2.17 | <0.001 |
| OC-CH | 9.12 (1.40) | 8.91 (1.81) | 0.21 | 0.570 |
| OC-EH | 7.25 (1.63) | 9.51 (12.05) | −2.26 | 0.250 |
| OC-SA | 33.42 (4.61) | 30.47 (6.10) | 2.95 | 0.020 |
| Left | ||||
| OC-MDW | 10.35 (1.43) | 10.33 (1.21) | 0.02 | 0.940 |
| OC-SL | 19.74 (1.94) | 17.65 (2.93) | 2.08 | <0.001 |
| OC-CH | 9.11 (1.09) | 9.27 (1.98) | −0.16 | 0.670 |
| OC-EH | 7.46 (1.60) | 7.04 (2.01) | 0.43 | 0.300 |
| OC-SA | 35.44 (4.43) | 32.32 (5.01) | 3.12 | 0.005 |
| Overall | |||
|---|---|---|---|
| Variable | Male n = 38 | Female n = 38 | p-Value |
| Right | |||
| OC-MDW | 9.86 (1.23) | 10.45 (1.35) | 0.048 |
| OC-SL | 18.31 (1.91) | 19.21 (2.96) | 0.120 |
| OC-CH | 8.99 (1.68) | 9.04 (1.56) | 0.904 |
| OC-EH | 8.96 (12.09) | 7.80 (1.86) | 0.560 |
| OC-SA | 33.23 (4.79) | 30.66 (6.05) | 0.043 |
| Left | |||
| OC-MDW | 10.07 (1.21) | 10.61 (1.37) | 0.075 |
| OC-SL | 18.30 (2.36) | 19.09 (2.95) | 0.203 |
| OC-CH | 9.14 (1.83) | 9.24 (1.32) | 0.792 |
| OC-EH | 6.94 (1.93) | 7.56 (1.66) | 0.139 |
| OC-SA | 34.37 (4.91) | 33.38 (5.02) | 0.390 |
| Class I | |||
| Variable | Male n = 19 | Female n = 19 | p-value |
| Right | |||
| OC-MDW | 9.44 (0.97) | 10.48 (1.40) | 0.011 |
| OC-SL | 19.09 (1.75) | 20.59 (2.13) | 0.024 |
| OC-CH | 9.04 (1.32) | 9.20 (1.51) | 0.720 |
| OC-EH | 6.75 (1.55) | 7.75 (1.60) | 0.057 |
| OC-SA | 33.78 (4.30) | 33.06 (4.99) | 0.634 |
| Left | |||
| OC-MDW | 9.95 (1.23) | 10.75 (1.53) | 0.083 |
| OC-SL | 19.22 (1.58) | 20.26 (2.16) | 0.100 |
| OC-CH | 9.03 (1.09) | 9.18 (1.11) | 0.674 |
| OC-EH | 7.55 (1.61) | 7.37 (1.63) | 0.740 |
| OC-SA | 36.47 (3.48) | 34.40 (5.10) | 0.152 |
| Class III | |||
| Variable | Male n = 19 | Female n = 19 | p-Value |
| Right | |||
| OC-MDW | 10.28 (1.34) | 10.43 (1.34) | 0.735 |
| OC-SL | 17.52 (1.78) | 17.82 (3.07) | 0.710 |
| OC-CH | 8.94 (2.01) | 8.87 (1.64) | 0.899 |
| OC-EH | 11.17 (16.97) | 7.85 (2.13) | 0.402 |
| OC-SA | 32.68 (5.29) | 28.26 (6.17) | 0.023 |
| Left | |||
| OC-MDW | 10.19 (1.22) | 10.46 (1.22) | 0.499 |
| OC-SL | 17.38 (2.67) | 17.92 (3.21) | 0.579 |
| OC-CH | 9.24 (2.38) | 9.29 (1.54) | 0.947 |
| OC-EH | 6.33 (2.07) | 7.74 (1.71) | 0.028 |
| OC-SA | 32.26 (5.29) | 32.37 (4.87) | 0.949 |
| Variable | Right | Left | p-Value |
|---|---|---|---|
| OC-MDW | 10.16 (1.32) | 10.34 (1.32) | 0.195 |
| OC-SL | 18.76 (2.52) | 18.70 (2.68) | 0.817 |
| OC-CH | 9.01 (1.61) | 9.19 (1.59) | 0.185 |
| OC-EH | 8.38 (8.61) | 7.25 (1.81) | 0.247 |
| OC-SA | 31.95 (5.57) | 33.88 (4.96) | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gumussoy, I.; Duman, S.B.; Miloglu, O.; Demirsoy, M.S.; Dogan, A.; Abdelkarim, A.Z.; Guller, M.T. Comparative Morphometric Study of the Occipital Condyle in Class III and Class I Skeletal Malocclusion Patients. Diagnostics 2024, 14, 2688. https://doi.org/10.3390/diagnostics14232688
Gumussoy I, Duman SB, Miloglu O, Demirsoy MS, Dogan A, Abdelkarim AZ, Guller MT. Comparative Morphometric Study of the Occipital Condyle in Class III and Class I Skeletal Malocclusion Patients. Diagnostics. 2024; 14(23):2688. https://doi.org/10.3390/diagnostics14232688
Chicago/Turabian StyleGumussoy, Ismail, Suayip Burak Duman, Ozkan Miloglu, Mustafa Sami Demirsoy, Ayhan Dogan, Ahmed Z. Abdelkarim, and Mustafa Taha Guller. 2024. "Comparative Morphometric Study of the Occipital Condyle in Class III and Class I Skeletal Malocclusion Patients" Diagnostics 14, no. 23: 2688. https://doi.org/10.3390/diagnostics14232688
APA StyleGumussoy, I., Duman, S. B., Miloglu, O., Demirsoy, M. S., Dogan, A., Abdelkarim, A. Z., & Guller, M. T. (2024). Comparative Morphometric Study of the Occipital Condyle in Class III and Class I Skeletal Malocclusion Patients. Diagnostics, 14(23), 2688. https://doi.org/10.3390/diagnostics14232688







