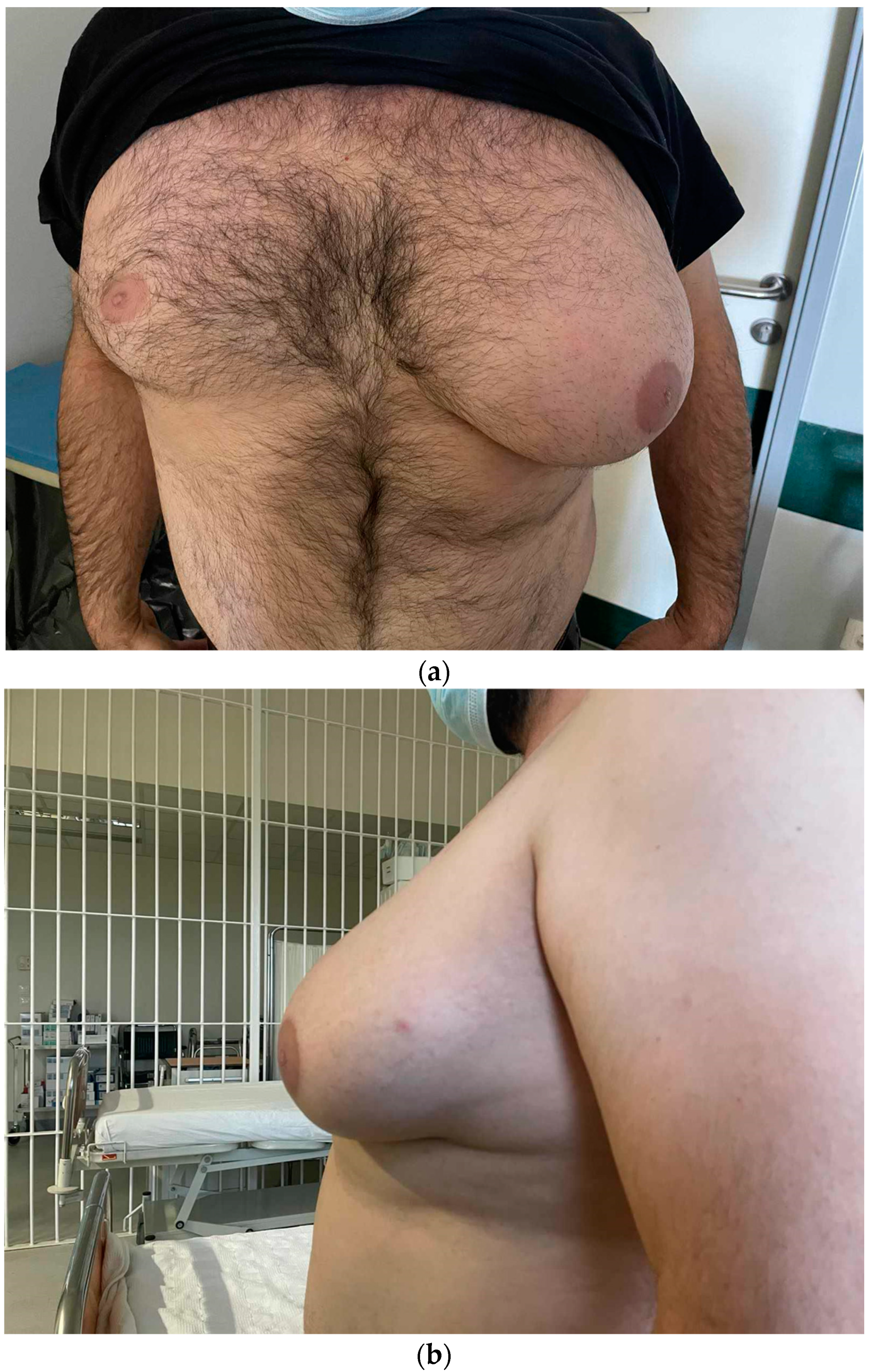
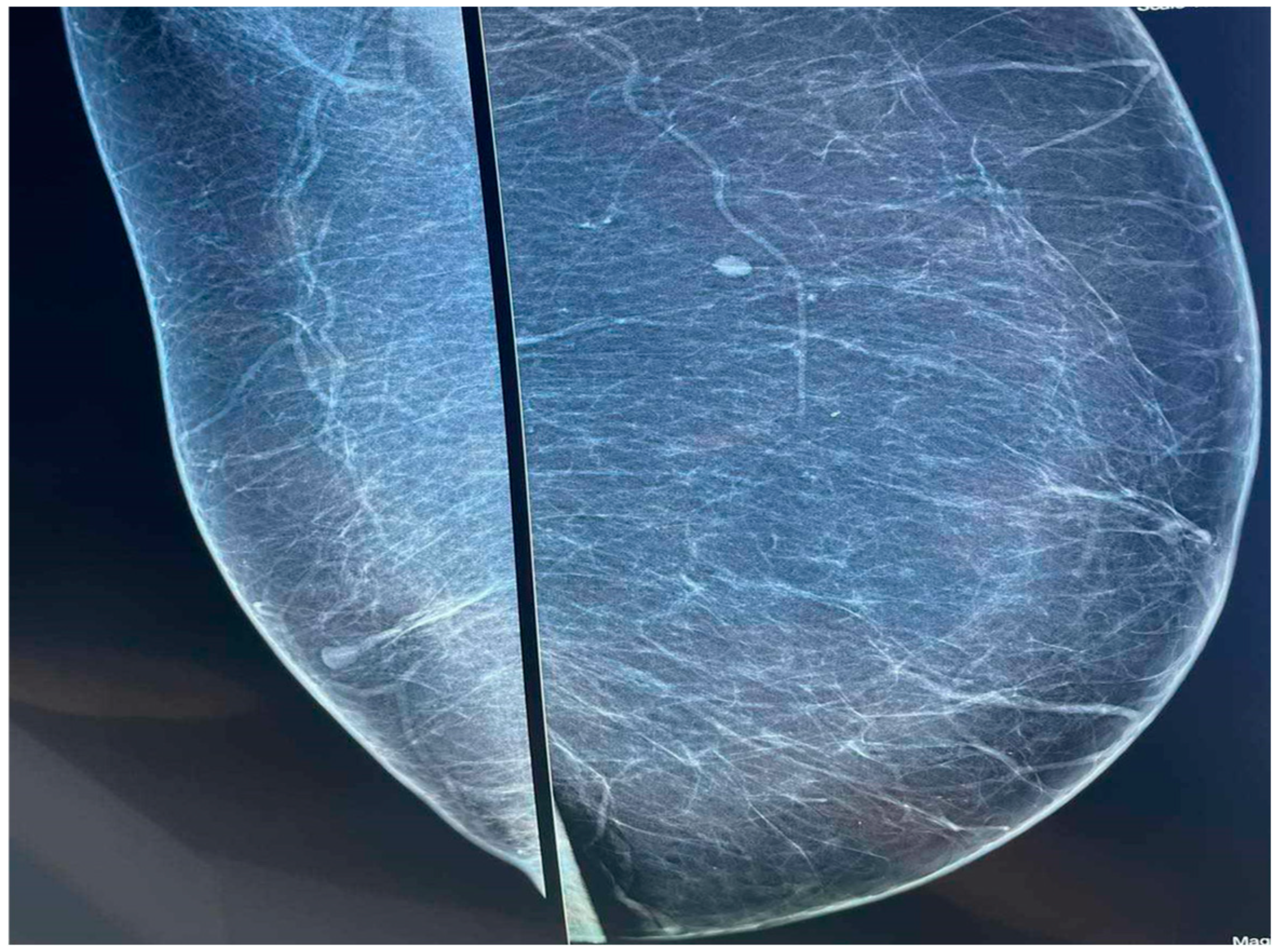
A Unique Case of Unilateral Pseudogynecomastia
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baumann, K. Gynecomastia—Conservative and Surgical Management. Breast Care 2018, 13, 419–424. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Polat, A.V.; Öztürk, M.; Çamlıdağ, İ.; Akyüz, B. Is gynecomastia related to the disease characteristics and prognosis in testicular germ cell tumor patients? Diagn. Interv. Radiol. 2019, 25, 189–194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hanneken, S.; Kruse, R.; Dall, P.; Ruzicka, T.; Neumann, N.J. Unilateral pseudogynecomastia: A novel work-related disease. Ann. Intern. Med. 2004, 140, W28. [Google Scholar] [PubMed]
- Mett, T.R.; Pfeiler, P.P.; Luketina, R.; Bingöl, A.S.; Krezdorn, N.; Vogt, P.M. Surgical treatment of gynaecomastia: A standard of care in plastic surgery. Eur. J. Plast. Surg. 2020, 43, 389–398. [Google Scholar] [CrossRef]
- Kornstein, A.N.; Cinelli, P.B. Inferior pedicle reduction technique for larger forms of gynecomastia. Aesthetic Plast. Surg. 1992, 16, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Spyropoulou, G.A.; Karamatsoukis, S.; Foroglou, P. Unilateral Pseudogynecomastia: An Occupational Hazard in Manual Metal-Pressing Factories? Aesthetic Plast. Surg. 2011, 35, 270–273. [Google Scholar] [CrossRef]
- Arnon, O.; Barnea, Y.; Zaretski, A.; Miller, E.; Leshem, D.; Weiss, J.; Amir, A.; Gur, E. Occupational Pseudogynecomastia: A New Etiology for Unilateral Gynecomastia. Plast. Reconstr. Surg. 2005, 115, 1e–4e. [Google Scholar] [CrossRef] [PubMed]
- Erol, S.; Orhan, E.; Sevin, A.; Erdoğan, B. Trauma: A New Pseudogynecomastia Cause. Aesthetic Plast. Surg. 2010, 34, 404–405. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.G.; Song, W.J.; Kim, C.H.; Kim, J.W.; Tark, M.S. Unilateral gynecomastia in a tennis player. Arch. Plast. Surg. 2012, 39, 675–678. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Braunstein, G.D. Gynecomastia. N. Engl. J. Med. 1993, 328, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Durkin, E.T.; Warner, T.F.; Nichol, P.F. Enlarging unilateral breast mass in an adolescent male: An unusual presentation of intraductal papilloma. J. Pediatr. Surg. 2011, 46, e33–e35. [Google Scholar] [CrossRef] [PubMed]
- Pellegrin, M.C.; Naviglio, S.; Cattaruzzi, E.; Barbi, E.; Ventura, A. A Teenager with Sudden Unilateral Breast Enlargement. J. Pediatr. 2017, 182, 394. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arredondo Montero, J.; Bronte Anaut, M.; Ayuso González, L.; Hernández-Martín, S.; Ruiz de Azúa-Ciria, Y. Unilateral Galactocele in a 2-Year-Old Boy: The Role of GATA-3. Indian J. Surg. 2023, 85, 1485–1487. [Google Scholar] [CrossRef]
- Laimon, W.; El-Hawary, A.; Aboelenin, H.; Elzohiri, M.; Abdelmaksoud, S.; Megahed, N.; Salem, N. Prepubertal gynecomastia is not always idiopathic: Case series and review of the literature. Eur. J. Pediatr. 2020, 180, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Hardy, K.L.; Stark, R.; Small, K.H.; Kenkel, J.M. An Alternative Treatment of Pseudogynecomastia in Male Patients After Massive Weight Loss. Aesthetic Surg. J. Open Forum 2020, 2, ojaa013. [Google Scholar] [CrossRef]
- Gusenoff, J.A.; Coon, D.; Rubin, J.P. Pseudogynecomastia after massive weight loss: Detectability of technique, patient satisfaction, and classification. Plast. Reconstr. Surg. 2008, 122, 1301–1311. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.Y.; Park, S.J.; Kim, S.Y.; Kim, B.J. Efficacy and Safety of Cold-Induced Noninvasive Targeted Fat Reduction in Pseudogynecomastia. Ann. Dermatol. 2022, 34, 412–418. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kountouri, I.; Katsarelas, I.; Kokkali, E.; Giotas, A.; Gkogkos, C.; Chatzinas, D.; Nachopoulos, P.; Faseki, A.; Panagiotou, A.; Polychronidis, A.; et al. A Unique Case of Unilateral Pseudogynecomastia. Diagnostics 2024, 14, 2058. https://doi.org/10.3390/diagnostics14182058
Kountouri I, Katsarelas I, Kokkali E, Giotas A, Gkogkos C, Chatzinas D, Nachopoulos P, Faseki A, Panagiotou A, Polychronidis A, et al. A Unique Case of Unilateral Pseudogynecomastia. Diagnostics. 2024; 14(18):2058. https://doi.org/10.3390/diagnostics14182058
Chicago/Turabian StyleKountouri, Ismini, Ioannis Katsarelas, Eftychia Kokkali, Amyntas Giotas, Christos Gkogkos, Dimitrios Chatzinas, Panagiotis Nachopoulos, Afroditi Faseki, Alexandra Panagiotou, Athanasios Polychronidis, and et al. 2024. "A Unique Case of Unilateral Pseudogynecomastia" Diagnostics 14, no. 18: 2058. https://doi.org/10.3390/diagnostics14182058
APA StyleKountouri, I., Katsarelas, I., Kokkali, E., Giotas, A., Gkogkos, C., Chatzinas, D., Nachopoulos, P., Faseki, A., Panagiotou, A., Polychronidis, A., Chandolias, M., Gkiatas, N., Manolakaki, D., & Dimasis, P. (2024). A Unique Case of Unilateral Pseudogynecomastia. Diagnostics, 14(18), 2058. https://doi.org/10.3390/diagnostics14182058





