Early-Stage Prototype Assessment of Cost-Effective Non-Intrusive Wearable Device for Instant Home Fetal Movement and Distress Detection: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
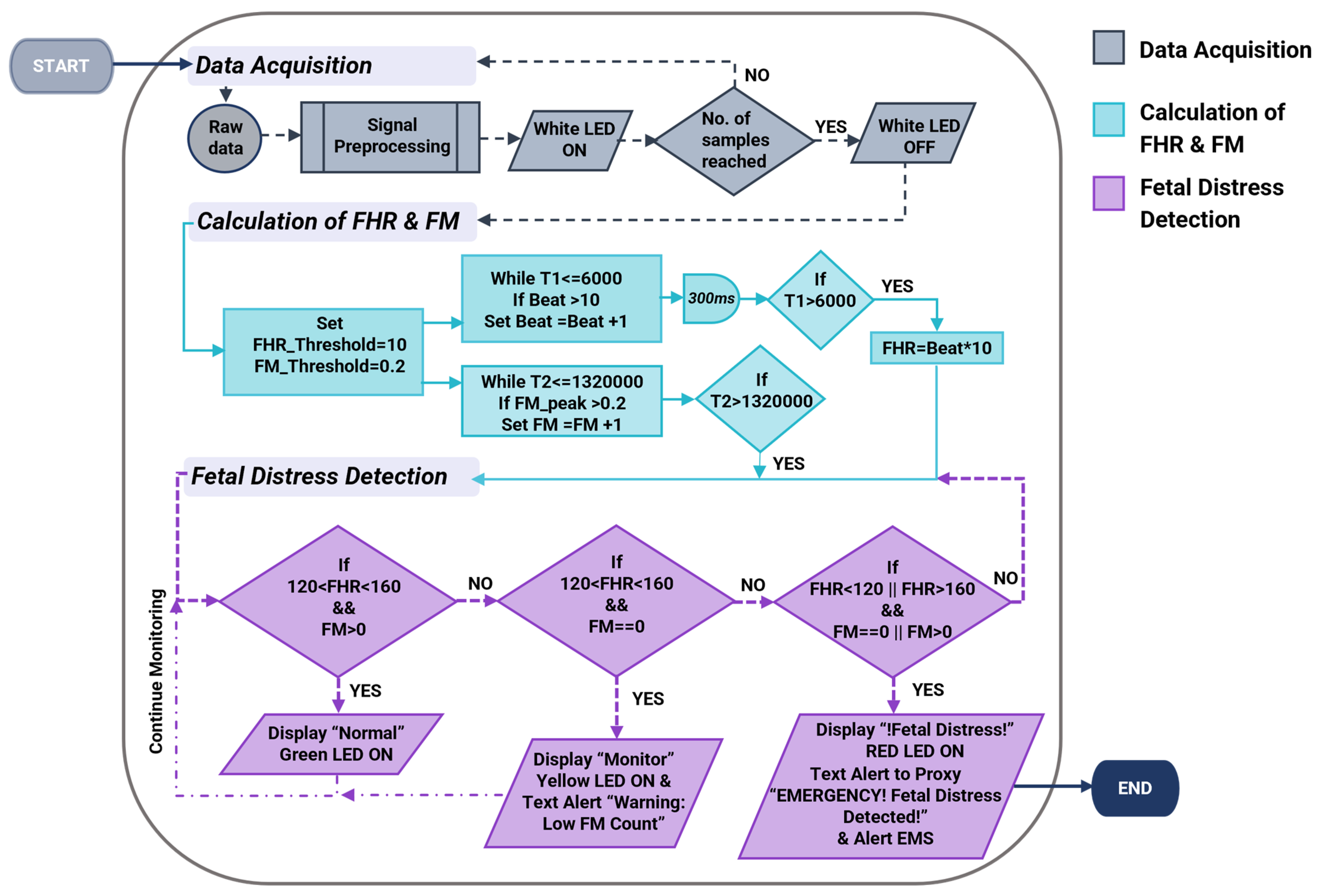
2.1. The Operational Algorithm
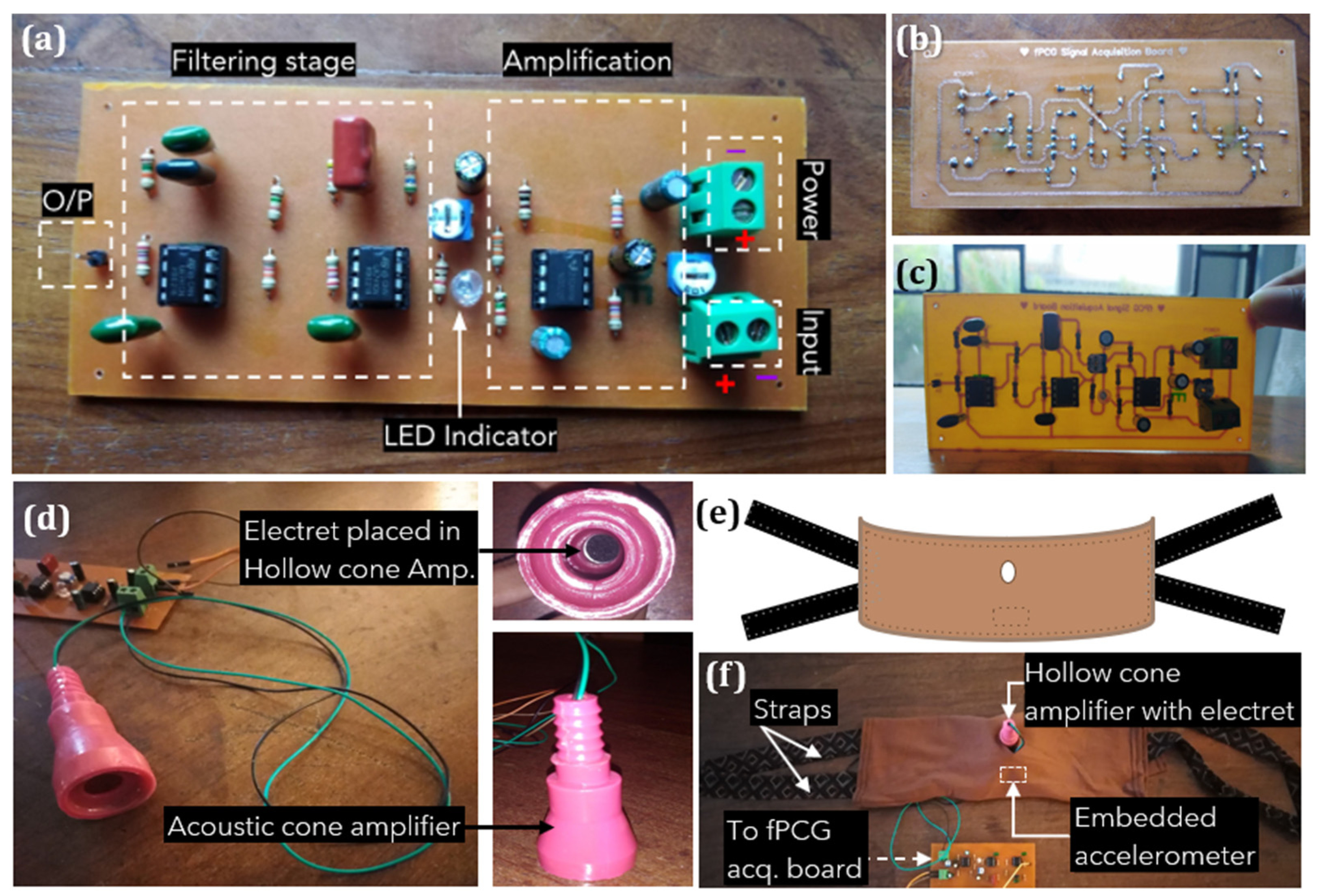
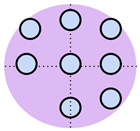
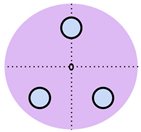
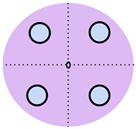
2.2. System Configuration
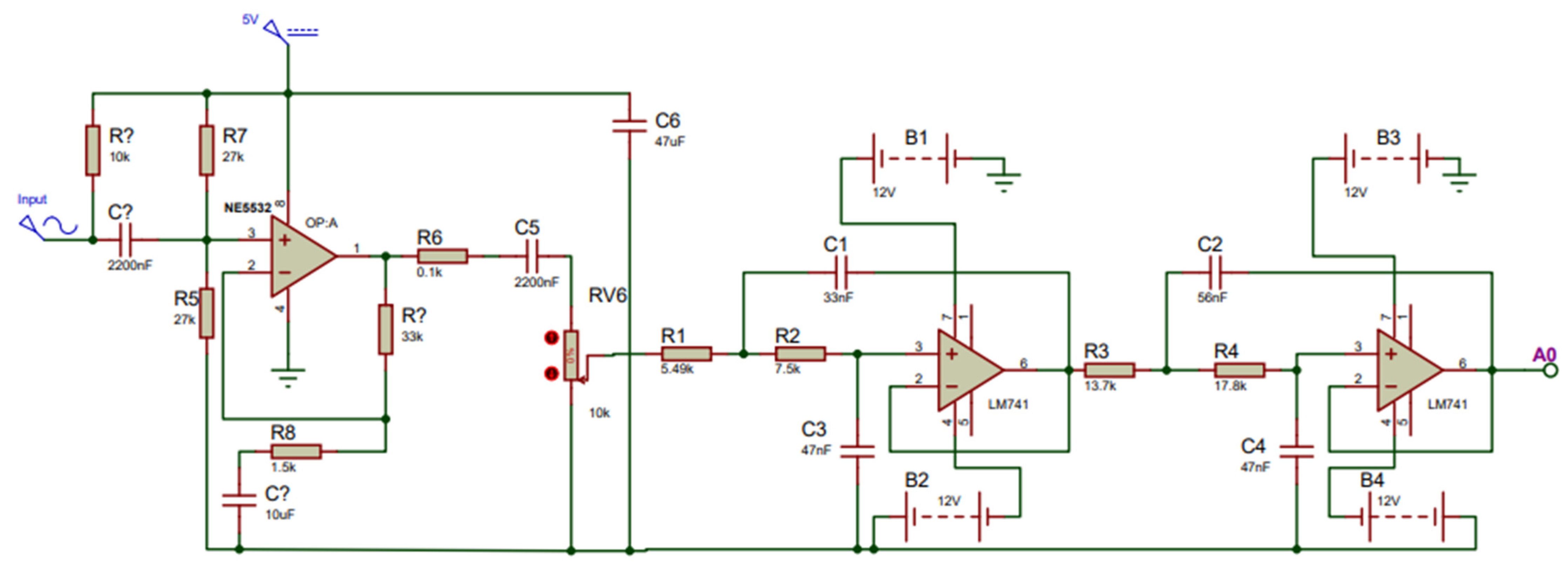
2.3. Development of the Fetal Phonocardiography (fPCG) Acquisition Board
2.4. Development of the Alarm System
3. Results and Discussion
3.1. Digital Signal Processing Algorithm for Calculating Fetal Movement
3.1.1. Fetal Movement Dataset
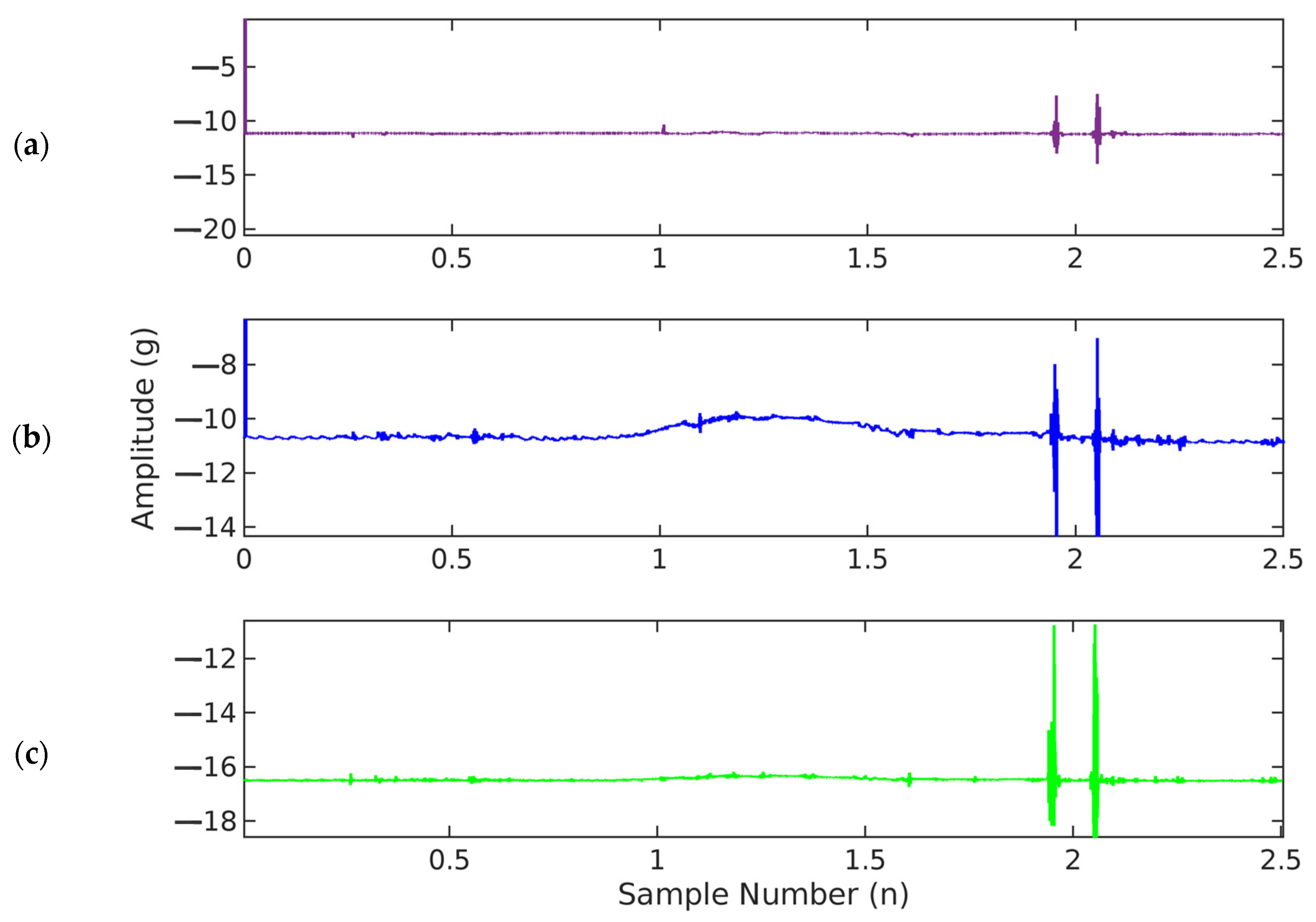
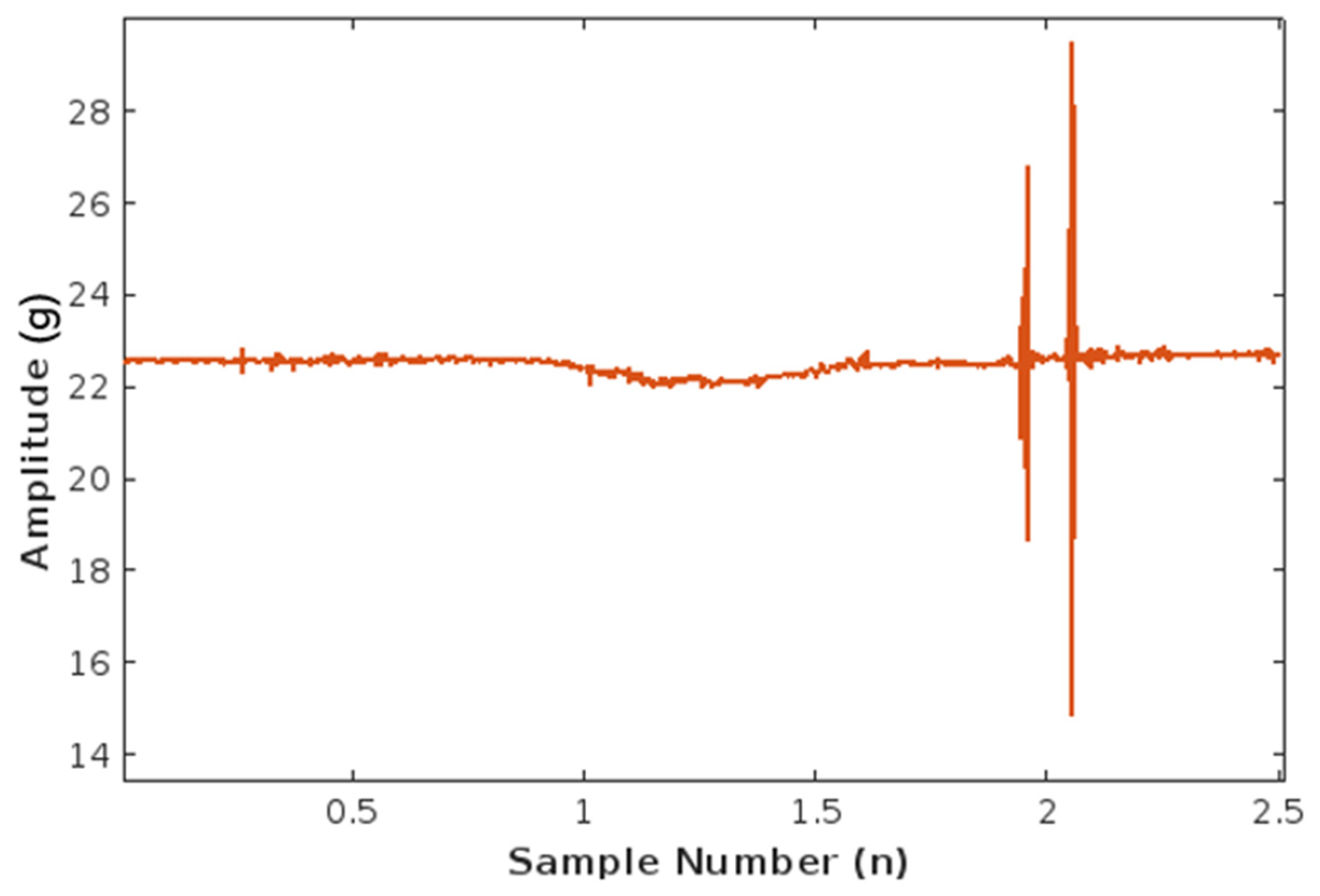
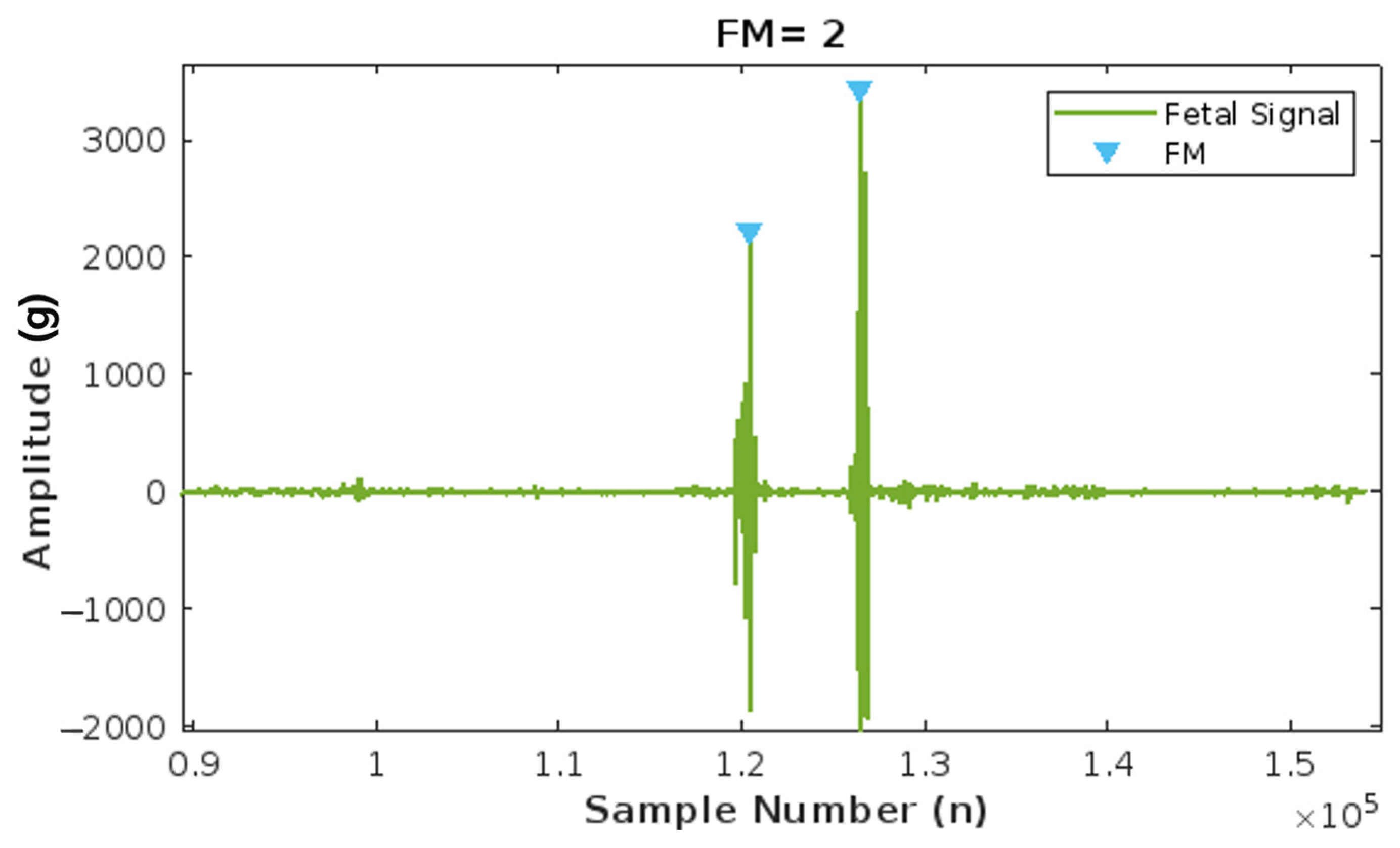
3.1.2. Fetal Movement (FM) Signal Visualization and Filtering
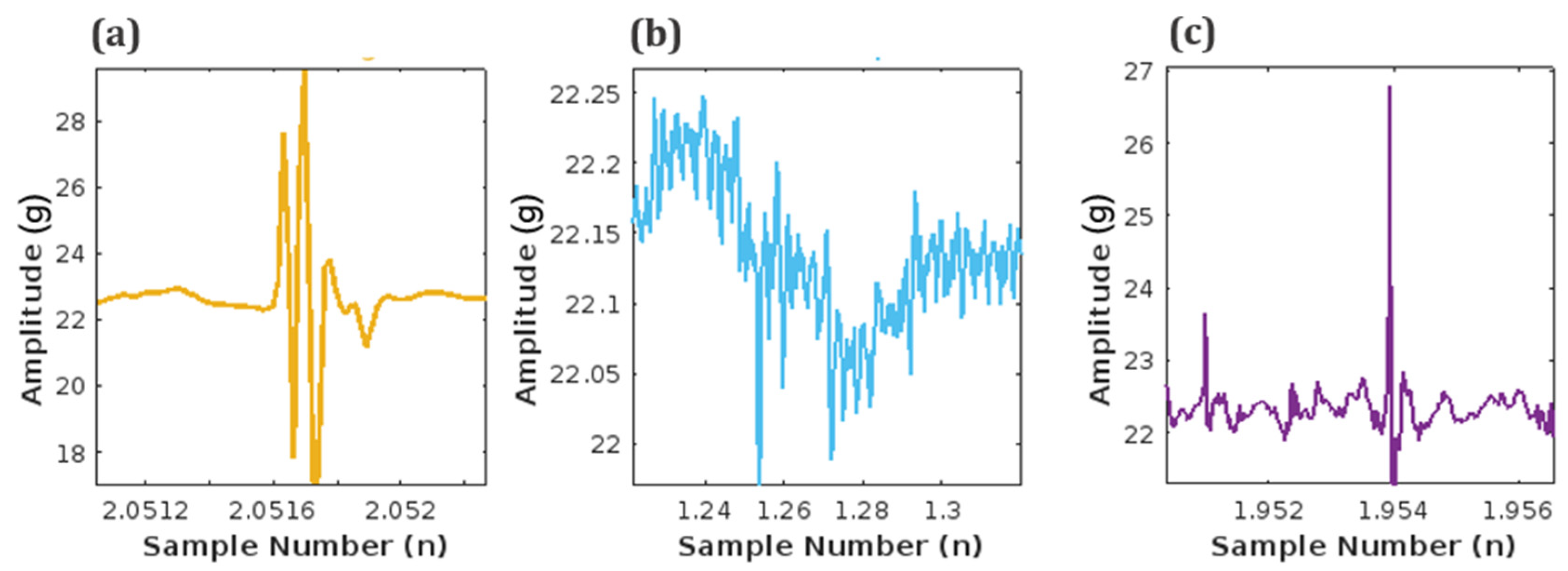
3.1.3. Fetal Movement (FM) Peak Detection
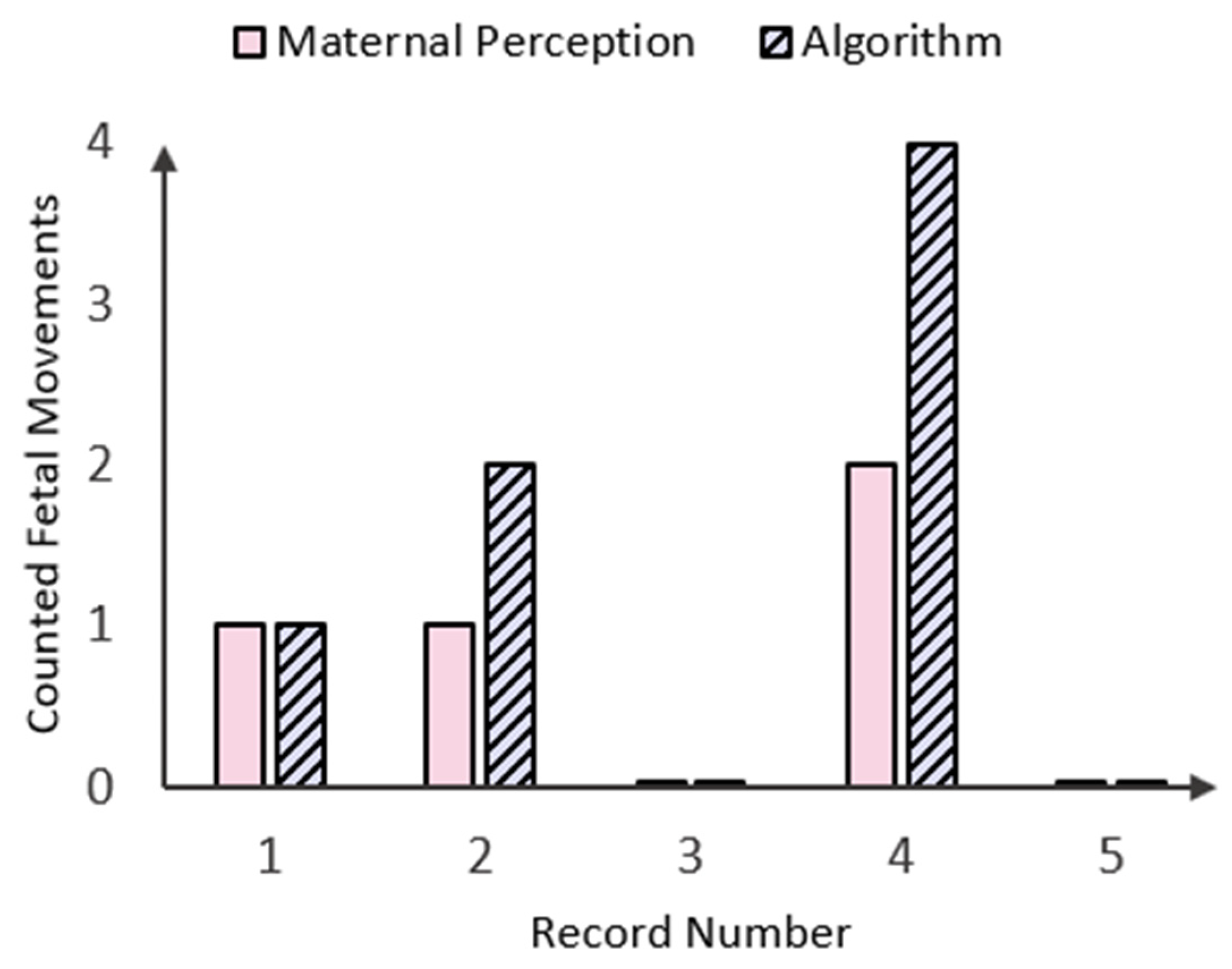
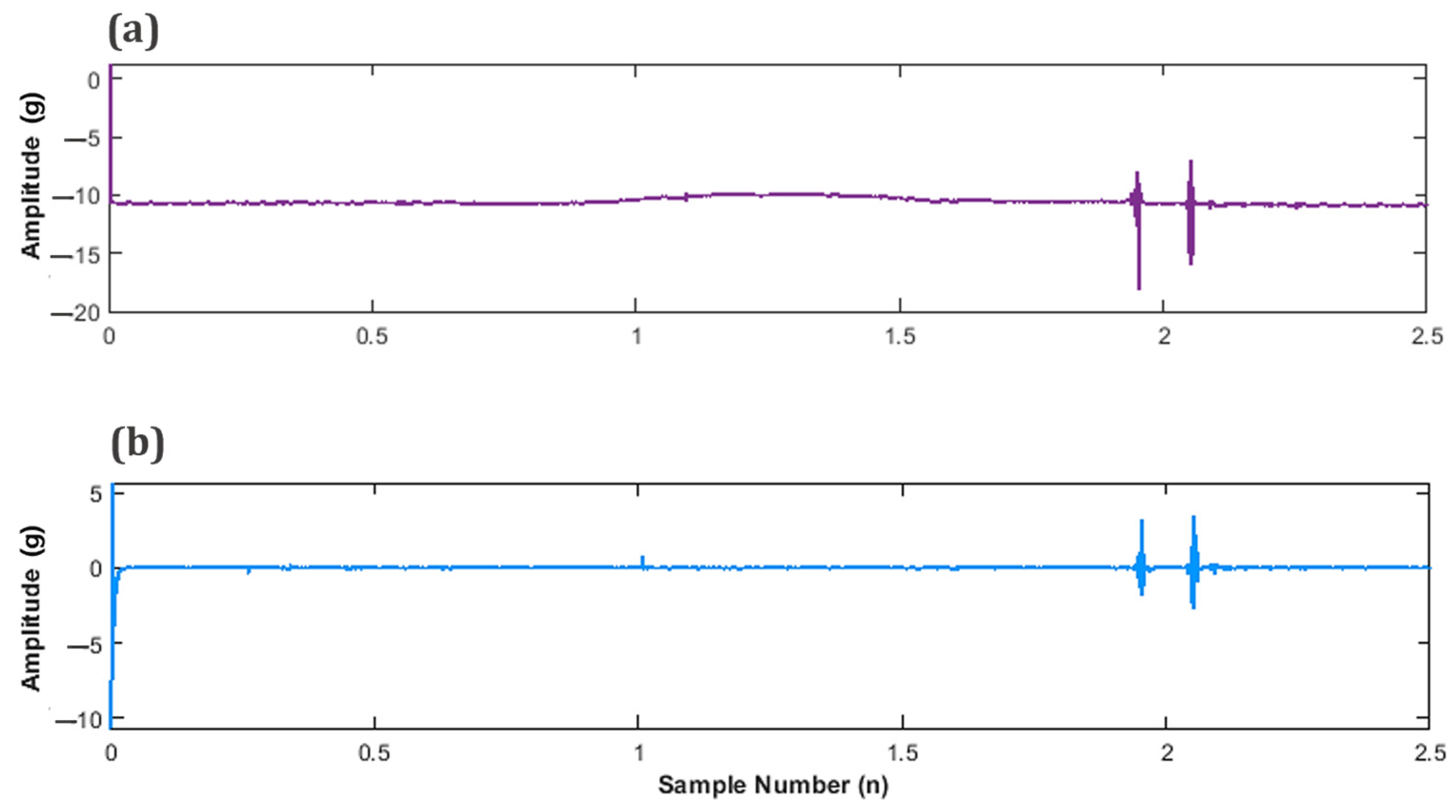
3.1.4. Fetal Movement (FM) Count Algorithm
3.2. Amplifier and Filter for Fetal Heart Rate Acquisition
3.3. Alarm System
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WebMD 1 in 4 U.S. Stillbirths Might Be Prevented. 2018. Available online: https://www.webmd.com/baby/news/20180119/1-in-4-us-stillbirths-might-be-prevented (accessed on 5 February 2024).
- Family Health Bureau Sri Lanka National Statistics 2020. Available online: https://fhb.health.gov.lk/index.php/en/statistics (accessed on 5 February 2024).
- UNICEF DATA A Neglected Tragedy: The Global Burden of Stillbirths. 2020. Available online: https://data.unicef.org/resources/a-neglected-tragedy-stillbirth-estimates-report/ (accessed on 24 March 2024).
- Gravett, C.; Eckert, L.O.; Gravett, M.G.; Dudley, D.J.; Stringer, E.M.; Mujobu, T.B.M.; Lyabis, O.; Kochhar, S.; Swamy, G.K. Non-Reassuring Fetal Status: Case Definition & Guidelines for Data Collection, Analysis, and Presentation of Immunization Safety Data. Vaccine 2016, 34, 6084–6092. [Google Scholar] [CrossRef]
- Stacey, T.; Thompson, J.M.D.; Mitchell, E.A.; Ekeroma, A.; Zuccollo, J.; McCowan, L.M.E. Maternal Perception of Fetal Activity and Late Stillbirth Risk: Findings from the Auckland Stillbirth Study. Birth 2011, 38, 311–316. [Google Scholar] [CrossRef]
- NHS Stillbirth—What Happens If Your Unborn Baby Dies. 2021. Available online: https://www.nhs.uk/conditions/stillbirth/what-happens/#:~:text=Stillbirth-,What%20happens%20if%20your%20unborn%20baby%20dies,-%2D (accessed on 5 February 2024).
- Monasta, L.; Giangreco, M.; Ancona, E.; Barbone, F.; Bet, E.; Boschian-Bailo, P.; Cacciaguerra, G.; Cagnacci, A.; Canton, M.; Casarotto, M.; et al. Retrospective Study 2005–2015 of All Cases of Fetal Death Occurred at ≥23 Gestational Weeks, in Friuli Venezia Giulia, Italy. BMC Pregnancy Childbirth 2020, 20, 384. [Google Scholar] [CrossRef] [PubMed]
- Layden, E.A.; Thomson, A.J.; Owen, P.; Madhra, M.; Magowan, B. (Eds.) Monitoring of the Fetus in Labour. In Clinical Obstetrics and Gynaecology; Elsevier: Edinburgh, Scotland, 2023; ISBN 978-0-7020-8514-7. [Google Scholar]
- Kwon, J.Y.; Park, I.Y. Fetal Heart Rate Monitoring: From Doppler to Computerized Analysis. Obstet. Gynecol. Sci. 2016, 59, 79. [Google Scholar] [CrossRef] [PubMed]
- Degani, N.; Sikich, N. Caesarean Delivery Rate Review: An Evidence-Based Analysis. Ont. Health Technol. Assess. Ser. 2015, 15, 1–58. [Google Scholar]
- Alfirevic, Z.; Gyte, G.M.; Cuthbert, A.; Devane, D. Continuous Cardiotocography (CTG) as a Form of Electronic Fetal Monitoring (EFM) for Fetal Assessment during Labour. Cochrane Database Syst. Rev. 2017, 2019, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Kumari, M.; Abraham, A.; Abraham, K.; Navaneethan, P.; Karuppusami, R.; Sridhar, S.; Regi, A. Intrapartum Electronic Fetal Monitoring and Perinatal Outcomes: Analysis of Components of Fetal Heart Rate Pattern. Curr. Med. Issues 2023, 21, 26. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration Ultrasound Imaging. 2024. Available online: https://www.fda.gov/radiation-emitting-products/medical-imaging/ultrasound-imaging (accessed on 5 February 2024).
- Mhajna, M.; Schwartz, N.; Levit-Rosen, L.; Warsof, S.; Lipschuetz, M.; Jakobs, M.; Rychik, J.; Sohn, C.; Yagel, S. Wireless, Remote Solution for Home Fetal and Maternal Heart Rate Monitoring. Am. J. Obstet. Gynecol. MFM 2020, 2, 100101. [Google Scholar] [CrossRef]
- Delay, U.; Nawarathne, T.; Dissanayake, S.; Gunarathne, S.; Withanage, T.; Godaliyadda, R.; Rathnayake, C.; Ekanayake, P.; Wijayakulasooriya, J. Novel Non-Invasive in-House Fabricated Wearable System with a Hybrid Algorithm for Fetal Movement Recognition. PLoS ONE 2021, 16, e0254560. [Google Scholar] [CrossRef]
- Lai, J.; Woodward, R.; Alexandrov, Y.; Ain Munnee, Q.; Lees, C.C.; Vaidyanathan, R.; Nowlan, N.C. Performance of a Wearable Acoustic System for Fetal Movement Discrimination. PLoS ONE 2018, 13, e0195728. [Google Scholar] [CrossRef]
- Yuan, L.; Yuan, Y.; Zhou, Z.; Bai, Y.; Wu, S. A Fetal ECG Monitoring System Based on the Android Smartphone. Sensors 2019, 19, 446. [Google Scholar] [CrossRef] [PubMed]
- Abeywardhana, S.A.Y.; Subhashini, H.A.A.; Wasalaarachchi, W.A.W.S.; Wimalarathna, G.H.I.; Ekanayake, M.P.B.; Godaliyadda, G.M.R.I.; Wijayakulasooriya, J.V.; Rathnayake, R.M.C.J. Time Domain Analysis for Fetal Movement Detection Using Accelerometer Data. In Proceedings of the 2018 IEEE Region 10 Humanitarian Technology Conference (R10-HTC), Malambe, Sri Lanka, 6–8 December 2018; pp. 1–5. [Google Scholar]
- Yang, C.; Antoine, C.; Young, B.K.; Tavassolian, N. A Pilot Study on Fetal Heart Rate Extraction from Wearable Abdominal Inertial Sensors. IEEE Sens. J. 2019, 19, 10773–10781. [Google Scholar] [CrossRef]
- Khandoker, A.; Ibrahim, E.; Oshio, S.; Kimura, Y. Validation of Beat by Beat Fetal Heart Signals Acquired from Four-Channel Fetal Phonocardiogram with Fetal Electrocardiogram in Healthy Late Pregnancy. Sci. Rep. 2018, 8, 13635. [Google Scholar] [CrossRef]
- Boeing, J.; Gatlin, T.; Hendler, E.; Hyde, E. Fetal Heart Rate Monitor for Resource-Limited Settings; Mechanical and Biomedical Engineering; University of Michigan: Ann Arbor, MI, USA, 2012. [Google Scholar]
- Wei, J.; Wang, Z.; Xing, X. A Wireless High-Sensitivity Fetal Heart Sound Monitoring System. Sensors 2020, 21, 193. [Google Scholar] [CrossRef] [PubMed]
- Hema, L.K.; Amalna; Anil, A.; Kanya. Pregnant Women Health Monitoring System Using Embedded System. IOP Conf. Ser. Mater. Sci. Eng. 2020, 993, 012078. [Google Scholar] [CrossRef]
- Abdhul Rahuman, M.A.; Kahatapitiya, N.S.; Amarakoon, V.N.; Wijenayake, U.; Silva, B.N.; Jeon, M.; Kim, J.; Ravichandran, N.K.; Wijesinghe, R.E. Recent Technological Progress of Fiber-Optical Sensors for Bio-Mechatronics Applications. Technologies 2023, 11, 157. [Google Scholar] [CrossRef]
- Abeywardena, C.L.; Vanheusden, F.J.; Walker, K.F.; Arm, R.; Zhang, Q. Fetal Movement Counting Using Optical Fibre Sensors. Sensors 2020, 21, 48. [Google Scholar] [CrossRef] [PubMed]
- Charlier, P.; De Jonckheere, J.; Zhao, X. Fetal Movement Acceleration Data 2019. Available online: https://zenodo.org/doi/10.5281/zenodo.3544630 (accessed on 28 July 2024).
- Liang, S.; Peng, J.; Xu, Y.; Ye, H. Passive Fetal Movement Recognition Approaches Using Hyperparameter Tuned LightGBM Model and Bayesian Optimization. Comput. Intell. Neurosci. 2021, 2021, 6252362. [Google Scholar] [CrossRef] [PubMed]
- Qin, M.; Xu, Y.; Liang, Y.; Sun, T. A Wearable Fetal Movement Detection System for Pregnant Women. Front. Med. 2023, 10, 1160373. [Google Scholar] [CrossRef]
- Mesbah, M.; Khlif, M.S.; Layeghy, S.; East, C.E.; Dong, S.; Brodtmann, A.; Colditz, P.B.; Boashash, B. Automatic Fetal Movement Recognition from Multi-Channel Accelerometry Data. Comput. Methods Programs Biomed. 2021, 210, 106377. [Google Scholar] [CrossRef]
- Pildner Von Steinburg, S.; Boulesteix, A.-L.; Lederer, C.; Grunow, S.; Schiermeier, S.; Hatzmann, W.; Schneider, K.-T.M.; Daumer, M. What Is the “Normal” Fetal Heart Rate? PeerJ 2013, 1, e82. [Google Scholar] [CrossRef] [PubMed]
- Saastad, E.; Winje, B.A.; Stray Pedersen, B.; Frøen, J.F. Fetal Movement Counting Improved Identification of Fetal Growth Restriction and Perinatal Outcomes—A Multi-Centre, Randomized, Controlled Trial. PLoS ONE 2011, 6, e28482. [Google Scholar] [CrossRef]
- Labcenter Electronics Proteus 2024. Available online: https://www.labcenter.com/ (accessed on 24 March 2024).
- SoundJay Heartbeat Sound Effects—Wav MP3 Download 2023. Available online: https://www.soundjay.com/heartbeat-sound-effect.html (accessed on 24 March 2024).
- Ahmad, H.A.B.; El-Badawy, I.M.; Singh, O.P.; Hisham, R.B.; Malarvili, M.B. Fetal Heart Rate Monitoring Device Using Condenser Microphone Sensor: Validation and Comparison to Standard Devices. Technol. Health Care 2018, 26, 573–579. [Google Scholar] [CrossRef]






| Sensor and Electrode Configuration | Monitoring (Method, Sensors, Gw) | Algorithm and Signal Acquisition Techniques Used | Data Processing | Ref. |
|---|---|---|---|---|
 |
| Construction of mECG template through maternal QRST peak detection and mECG cancellation. fs = 120 Hz | Offline | [14] |
 |
| Hybrid algorithm (High pass filtering, segmentation, STFT, with CNN architecture) fs = 280 Hz | Offline | [15] |
 |
| Segmentation (Comb-notch filtering), Signal matching and Discrimination using PCA. | Offline (IMU and analog data on SD card) | [16] |
 |
| Baseline drift and mean value cancellation. FastICA algorithm (fECG extraction), sample entropy (signal location). fs = 250 Hz | Real-time via Bluetooth and Cloud storage | [17] |
 |
| Fast ICA algorithm (removes breathing artifacts and extract fECG). | Offline | [18] |
 |
| Prefiltered with zero-phase IIR filter CWT for processing and averaging algorithm for fusion. fs = 250 Hz | Offline | [19] |
 |
| Decomposition technique using Eigen vectors (to separate into different sound components) Denoising using WTST-NST. fs = 100 Hz | Offline | [20] |
 |
| Butterworth filter for sharpening sound attenuation in analog pre-amplification process. | Offline | [21] |
| Record Number (n) | Axis | Mean Value | Standard Deviation | Number of Samples (n) | Total Time Length (min) |
|---|---|---|---|---|---|
| Record 1 | X | −11.1521 | 0.0706 | 154,100 | 5.14 |
| Y | −10.5529 | 0.2797 | |||
| Z | −16.4638 | 0.0880 | |||
| Record 2 | X | −11.8295 | 0.0521 | 450,663 | 15.02 |
| Y | −10.5699 | 0.0983 | |||
| Z | −16.4497 | 0.0324 | |||
| Record 3 | X | −11.0093 | 0.0190 | 451,049 | 15.03 |
| Y | −9.3378 | 0.0417 | |||
| Z | −16.1127 | 0.0302 | |||
| Record 4 | X | −13.5053 | 0.1141 | 451,421 | 15.05 |
| Y | −10.2576 | 0.0671 | |||
| Z | −15.9186 | 0.0600 | |||
| Record 5 | X | −10.2336 | 0.0705 | 451,609 | 15.05 |
| Y | −10.3554 | 0.0720 | |||
| Z | −16.3136 | 0.0547 |
| Components | Variable | Expected Results | Final Outcome |
|---|---|---|---|
| Initiation | Initialization of system | White LED ON, LCD displays “Initialising” | White LED ON Displays: “Fetal Monitor Initialising…” |
| Alarm System | Reassuring Fetal Status | Green LED ON FHR and FM within normal range. | FHR = 140 BPM FM = ACT Displays: “Normal” Green LED ON |
| Low Fetal Movement count | Yellow LED On Warning Text: Low FM Count | FHR = 140 BPM FM = LOW Displays: “Monitor” Texts to Proxy: “Warning: Low Fetal Movement count” Yellow LED ON | |
| Non reassuring fetal status | Red LED ON FHR and FM outside normal range: Fetal distress | FHR = 162 BPM or 116 BPM FM= ACT or LOW Displays: “! Fetal Distress!” Texts to Proxy: “EMERGENCY: Fetal Distress Detected!” Red LED ON |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamed, H.; Kathriarachchi, S.K.; Kahatapitiya, N.S.; Silva, B.N.; Kalupahana, D.; Edirisinghe, S.; Wijenayake, U.; Ravichandran, N.K.; Wijesinghe, R.E. Early-Stage Prototype Assessment of Cost-Effective Non-Intrusive Wearable Device for Instant Home Fetal Movement and Distress Detection: A Pilot Study. Diagnostics 2024, 14, 1938. https://doi.org/10.3390/diagnostics14171938
Mohamed H, Kathriarachchi SK, Kahatapitiya NS, Silva BN, Kalupahana D, Edirisinghe S, Wijenayake U, Ravichandran NK, Wijesinghe RE. Early-Stage Prototype Assessment of Cost-Effective Non-Intrusive Wearable Device for Instant Home Fetal Movement and Distress Detection: A Pilot Study. Diagnostics. 2024; 14(17):1938. https://doi.org/10.3390/diagnostics14171938
Chicago/Turabian StyleMohamed, Hana, Suresh Kalum Kathriarachchi, Nipun Shantha Kahatapitiya, Bhagya Nathali Silva, Deshan Kalupahana, Sajith Edirisinghe, Udaya Wijenayake, Naresh Kumar Ravichandran, and Ruchire Eranga Wijesinghe. 2024. "Early-Stage Prototype Assessment of Cost-Effective Non-Intrusive Wearable Device for Instant Home Fetal Movement and Distress Detection: A Pilot Study" Diagnostics 14, no. 17: 1938. https://doi.org/10.3390/diagnostics14171938
APA StyleMohamed, H., Kathriarachchi, S. K., Kahatapitiya, N. S., Silva, B. N., Kalupahana, D., Edirisinghe, S., Wijenayake, U., Ravichandran, N. K., & Wijesinghe, R. E. (2024). Early-Stage Prototype Assessment of Cost-Effective Non-Intrusive Wearable Device for Instant Home Fetal Movement and Distress Detection: A Pilot Study. Diagnostics, 14(17), 1938. https://doi.org/10.3390/diagnostics14171938










