Sequential Comparison of Knee Muscle Strength after Anterior Cruciate Ligament Reconstruction between Hamstring Autograft and Tibialis Anterior Allograft: Propensity Score Matched Pair Analysis
Abstract
1. Introduction
2. Materials and Methods
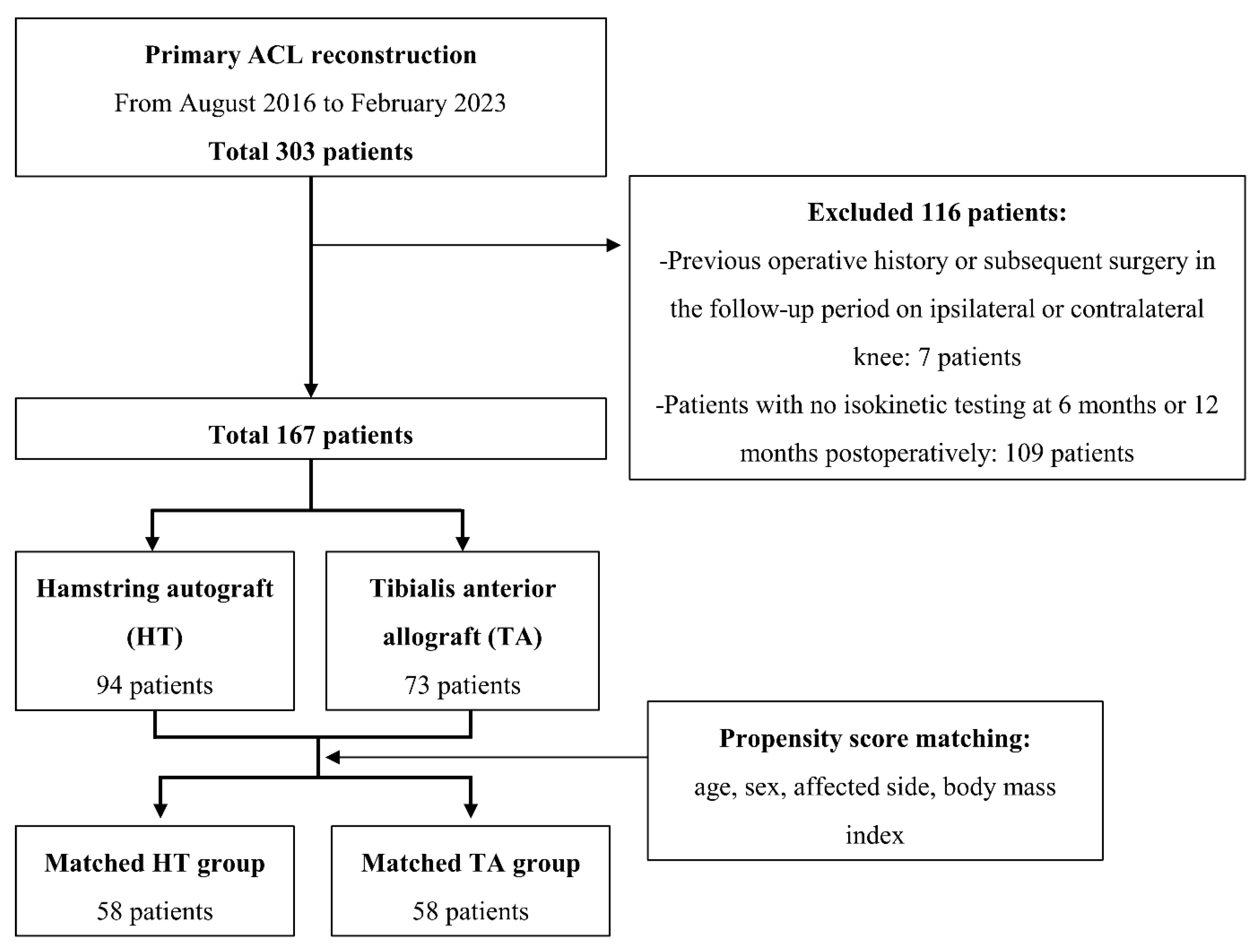
2.1. Patients
2.2. Surgical Procedures and Rehabilitation
2.3. Isokinetic Muscle Strength Testing
2.4. Clinical Outcome Assessment
2.5. Statistical Method
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sinding, K.S.; Nielsen, T.G.; Hvid, L.G.; Lind, M.; Dalgas, U. Effects of autograft types on muscle strength and functional capacity in patients having anterior cruciate ligament reconstruction: A randomized controlled trial. Sports Med. 2020, 50, 1393–1403. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Maradit Kremers, H.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Liukkonen, R.J.; Ponkilainen, V.T.; Reito, A. Revision rates after primary acl reconstruction performed between 1969 and 2018: A systematic review and metaregression analysis. Orthop J. Sports Med. 2022, 10, 23259671221110191. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Pareek, A.; Hewett, T.E.; Levy, B.A.; Dahm, D.L.; Stuart, M.J.; Krych, A.J. Long-term rate of graft failure after acl reconstruction: A geographic population cohort analysis. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Choi, C.H.; Yoo, J.H.; Jung, M.; Lee, T.H.; Choi, K.H.; Kim, S.H. The graft insertion length in the femoral tunnel during anterior cruciate ligament reconstruction with suspensory fixation and tibialis anterior allograft does not affect surgical outcomes but is negatively correlated with tunnel widening. Arthroscopy 2021, 37, 2903–2914.e2901. [Google Scholar] [CrossRef] [PubMed]
- Bourke, H.E.; Salmon, L.J.; Waller, A.; Patterson, V.; Pinczewski, L.A. Survival of the anterior cruciate ligament graft and the contralateral acl at a minimum of 15 years. Am. J. Sports Med. 2012, 40, 1985–1992. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Choi, C.H.; Jung, M.; Yoo, J.H.; Kwon, H.J.; Hong, Y.T.; Kim, S.H. Small intercondylar notch size is not associated with poor surgical outcomes of anatomical single-bundle anterior cruciate ligament reconstructions. Clin. Orthop. Surg. 2024, 16, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.H.; Lee, S.M.; Park, J.Y.; Lee, H.S.; Hwang, S.H. A comparison of results in older, middle-aged, and younger patients after primary anterior cruciate ligament reconstruction: Minimum 10-year follow-up. Clin. Orthop. Surg. 2024, 16, 57–65. [Google Scholar] [CrossRef]
- Arnold, M.P.; Calcei, J.G.; Vogel, N.; Magnussen, R.A.; Clatworthy, M.; Spalding, T.; Campbell, J.D.; Bergfeld, J.A.; Sherman, S.L. Acl study group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3871–3876. [Google Scholar] [CrossRef]
- Kaeding, C.C.; Pedroza, A.D.; Reinke, E.K.; Huston, L.J.; Spindler, K.P. Risk factors and predictors of subsequent acl injury in either knee after acl reconstruction: Prospective analysis of 2488 primary acl reconstructions from the moon cohort. Am. J. Sports Med. 2015, 43, 1583–1590. [Google Scholar] [CrossRef]
- Lamblin, C.J.; Waterman, B.R.; Lubowitz, J.H. Anterior cruciate ligament reconstruction with autografts compared with non-irradiated, non-chemically treated allografts. Arthroscopy 2013, 29, 1113–1122. [Google Scholar] [CrossRef]
- Mariscalco, M.W.; Magnussen, R.A.; Mehta, D.; Hewett, T.E.; Flanigan, D.C.; Kaeding, C.C. Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: A systematic review. Am. J. Sports Med. 2014, 42, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Tuca, M.; Valderrama, I.; Eriksson, K.; Tapasvi, S. Current trends in anterior cruciate ligament surgery. A worldwide benchmark study. J. ISAKOS 2023, 8, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Alomar, A.Z.; Baltow, B.; AlMogbil, I. Effect of anteromedial portal location on femoral tunnel inclination, length, and location in hamstring autograft-based single-bundle anterior cruciate ligament reconstruction: A prospective study. Knee Surg. Relat. Res. 2023, 35, 26. [Google Scholar] [CrossRef] [PubMed]
- Liau, Z.Q.G.; Ng, M.S.P.; Low, S.S.E.; Chin, B.Z.; Hui, J.H.P.; Kagda, F.H.Y. A novel practical method to predict anterior cruciate ligament hamstring graft size using preoperative mri. Knee Surg. Relat. Res. 2024, 36, 17. [Google Scholar] [CrossRef]
- Widner, M.; Dunleavy, M.; Lynch, S. Outcomes following acl reconstruction based on graft type: Are all grafts equivalent? Curr. Rev. Musculoskelet. Med. 2019, 12, 460–465. [Google Scholar] [CrossRef]
- McRae, S.; Leiter, J.; McCormack, R.; Old, J.; MacDonald, P. Ipsilateral versus contralateral hamstring grafts in anterior cruciate ligament reconstruction: A prospective randomized trial. Am. J. Sports Med. 2013, 41, 2492–2499. [Google Scholar] [CrossRef]
- Hardy, A.; Casabianca, L.; Andrieu, K.; Baverel, L.; Noailles, T. Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: Systematic review of literature. Orthop. Traumatol. Surg. Res. 2017, 103, S245–S248. [Google Scholar] [CrossRef]
- Kim, J.G.; Yang, S.J.; Lee, Y.S.; Shim, J.C.; Ra, H.J.; Choi, J.Y. The effects of hamstring harvesting on outcomes in anterior cruciate ligament-reconstructed patients: A comparative study between hamstring-harvested and -unharvested patients. Arthroscopy 2011, 27, 1226–1234. [Google Scholar] [CrossRef]
- Landes, S.; Nyland, J.; Elmlinger, B.; Tillett, E.; Caborn, D. Knee flexor strength after acl reconstruction: Comparison between hamstring autograft, tibialis anterior allograft, and non-injured controls. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 317–324. [Google Scholar] [CrossRef]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Hamstring strength recovery after hamstring tendon harvest for anterior cruciate ligament reconstruction: A comparison between graft types. Arthroscopy 2010, 26, 462–469. [Google Scholar] [CrossRef]
- Konrath, J.M.; Vertullo, C.J.; Kennedy, B.A.; Bush, H.S.; Barrett, R.S.; Lloyd, D.G. Morphologic characteristics and strength of the hamstring muscles remain altered at 2 years after use of a hamstring tendon graft in anterior cruciate ligament reconstruction. Am. J. Sports Med. 2016, 44, 2589–2598. [Google Scholar] [CrossRef]
- Li, S.; Su, W.; Zhao, J.; Xu, Y.; Bo, Z.; Ding, X.; Wei, Q. A meta-analysis of hamstring autografts versus bone-patellar tendon-bone autografts for reconstruction of the anterior cruciate ligament. Knee 2011, 18, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Cristiani, R.; Mikkelsen, C.; Wange, P.; Olsson, D.; Stålman, A.; Engström, B. Autograft type affects muscle strength and hop performance after acl reconstruction. A randomised controlled trial comparing patellar tendon and hamstring tendon autografts with standard or accelerated rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3025–3036. [Google Scholar] [CrossRef] [PubMed]
- Johnston, P.T.; Feller, J.A.; McClelland, J.A.; Webster, K.E. Strength deficits and flexion range of motion following primary anterior cruciate ligament reconstruction differ between quadriceps and hamstring autografts. J. ISAKOS 2021, 6, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Xergia, S.A.; McClelland, J.A.; Kvist, J.; Vasiliadis, H.S.; Georgoulis, A.D. The influence of graft choice on isokinetic muscle strength 4-24 months after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 768–780. [Google Scholar] [CrossRef]
- Ericsson, Y.B.; Roos, E.M.; Owman, H.; Dahlberg, L.E. Association between thigh muscle strength four years after partial meniscectomy and radiographic features of osteoarthritis 11 years later. BMC Musculoskelet. Disord. 2019, 20, 512. [Google Scholar] [CrossRef]
- Väistö, O.; Toivanen, J.; Kannus, P.; Järvinen, M. Anterior knee pain and thigh muscle strength after intramedullary nailing of a tibial shaft fracture: An 8-year follow-up of 28 consecutive cases. J. Orthop. Trauma 2007, 21, 165–171. [Google Scholar] [CrossRef]
- Mizner, R.L.; Petterson, S.C.; Stevens, J.E.; Vandenborne, K.; Snyder-Mackler, L. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J. Bone Jt. Surg. Am. 2005, 87, 1047–1053. [Google Scholar] [CrossRef]
| Overall | Matched | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | HT (n = 73) | TA (n = 94) | p-Value | ASMD | HT (n = 58) | TA (n = 58) | p-Value | ASMD |
| Age | 23.0 (20.0, 33.0) | 26.0 (20.0, 38.0) | 0.300 | 0.194 | 23.00 (20.0, 35.0) | 24.00 (19.0, 34.0) | 0.598 | 0.006 |
| BMI | 24.11 (22.55, 25.96) | 24.70 (22.39, 27.39) | 0.309 | 0.190 | 24.39 (22.6, 26.2) | 24.47 (22.4, 26.8) | 0.474 | 0.026 |
| Sex | 0.012 | 0.405 | >0.999 | <0.001 | ||||
| Male | 62 (84.9) | 64 (68.1) | 49 (84.5) | 49 (84.5) | ||||
| Female | 11 (15.1) | 30 (31.9) | 9 (15.5) | 9 (15.5) | ||||
| Affected side | 0.718 | 0.056 | 0.695 | 0.069 | ||||
| Right | 36 (49.3) | 49 (52.1) | 28 (48.3) | 30 (51.7) | ||||
| Left | 37 (50.7) | 45 (47.9) | 30 (51.7) | 28 (48.3) | ||||
| 6 Months Post Operation | 12 Months Post Operation | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | HT Group | TA Group | p-Value | Effect Size | HT Group | TA Group | p-Value | Effect Size |
| Extensor 60°/s | ||||||||
| Peak torque LSI | 67.4 ± 22.8 | 64.6 ± 22.1 | 0.468 | 0.124 | 80.3 ± 20.4 | 75.6 ± 18.8 | 0.168 | 0.240 |
| Total work LSI | 65.6 ± 22.1 | 65.6 ± 22.8 | 0.997 | 0.001 | 79.8 ± 19.3 | 77.3 ± 19.0 | 0.454 | 0.131 |
| Average power LSI | 67.9 ± 21.7 | 66.3 ± 18.3 | 0.945 | 0.080 | 79.0 ± 19.3 | 76.5 ± 18.4 | 0.470 | 0.133 |
| Flexor 60°/s | ||||||||
| Peak torque LSI | 71.6 ± 22.8 | 76.3 ± 21.9 | 0.210 | 0.210 | 80.6 ± 19.0 | 86.4 ± 19.3 | 0.116 | 0.303 |
| Total work LSI | 67.1 ± 25.9 | 67.5 ± 21.4 | 0.934 | 0.016 | 74.4 ± 19.6 | 84.2 ± 24.8 | 0.020 * | 0.438 |
| Average power LSI | 72.1 ± 22.6 | 75.1 ± 23.3 | 0.400 | 0.131 | 76.3 ± 17.3 | 85.3 ± 21.5 | 0.029 * | 0.461 |
| Extensor 180°/s | ||||||||
| Peak torque LSI | 70.0 ± 19.1 | 72.2 ± 20.3 | 0.546 | 0.112 | 82.0 ± 17.1 | 81.3 ± 20.7 | 0.840 | 0.037 |
| Total work LSI | 68.3 ± 20.4 | 70.7 ± 22.7 | 0.548 | 0.111 | 80.5 ± 17.3 | 82.0 ± 22.1 | 0.654 | 0.076 |
| Average power LSI | 67.2 ± 21.0 | 69.9 ± 21.6 | 0.481 | 0.127 | 81.2 ± 18.2 | 81.0 ± 22.2 | 0.947 | 0.010 |
| Flexor 180°/s | ||||||||
| Peak torque LSI | 79.1 ± 22.3 | 77.2 ± 19.3 | 0.632 | 0.091 | 84.1 ± 17.2 | 87.2 ± 17.1 | 0.246 | 0.181 |
| Total work LSI | 73.2 ± 26.0 | 71.9 ± 26.4 | 0.791 | 0.050 | 76.7 ± 21.1 | 85.8 ± 23.6 | 0.027 * | 0.407 |
| Average power LSI | 74.2 ± 24.4 | 72.0 ± 25.1 | 0.655 | 0.089 | 78.1 ± 19.2 | 87.1 ± 22.1 | 0.045 * | 0.435 |
| Variables | HT Group | TA Group | p-Value | Effect Size |
|---|---|---|---|---|
| VAS | 14.3 ± 17.6 | 11.4 ± 9.9 | 0.313 | 0.203 |
| Lysholm knee score | 84.9 ± 11.6 | 85.8 ± 14.8 | 0.737 | 0.068 |
| IKDC subjective score | 75.8 ± 17.3 | 74.7 ± 16.9 | 0.679 | 0.064 |
| Preinjury Tegner activity score | 6.0 ± 1.9 | 5.5 ± 2.0 | 0.150 | 0.256 |
| Tegner activity score | 3.4 ± 1.6 | 3.7 ± 1.8 | 0.303 | 0.176 |
| Return to activity rate | 11 (19.0) | 10 (17.2) | 1.000 | |
| Near return to activity rate | 23 (39.7) | 20 (34.5) | 0.701 | |
| Lachman test grade, 0/1/2/3 | 34/19/5/0 | 29/22/7/0 | 0.519 | |
| Pivot shift grade, 0/1/2/3 | 47/10/1/0 | 42/14/2/0 | 0.527 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, S.-H.; Choi, C.H.; Kim, S.-H.; Chung, K.; Moon, H.-S.; Sim, W.; Jung, M. Sequential Comparison of Knee Muscle Strength after Anterior Cruciate Ligament Reconstruction between Hamstring Autograft and Tibialis Anterior Allograft: Propensity Score Matched Pair Analysis. Diagnostics 2024, 14, 1478. https://doi.org/10.3390/diagnostics14141478
Jung S-H, Choi CH, Kim S-H, Chung K, Moon H-S, Sim W, Jung M. Sequential Comparison of Knee Muscle Strength after Anterior Cruciate Ligament Reconstruction between Hamstring Autograft and Tibialis Anterior Allograft: Propensity Score Matched Pair Analysis. Diagnostics. 2024; 14(14):1478. https://doi.org/10.3390/diagnostics14141478
Chicago/Turabian StyleJung, Se-Han, Chong Hyuk Choi, Sung-Hwan Kim, Kwangho Chung, Hyun-Soo Moon, Woongseob Sim, and Min Jung. 2024. "Sequential Comparison of Knee Muscle Strength after Anterior Cruciate Ligament Reconstruction between Hamstring Autograft and Tibialis Anterior Allograft: Propensity Score Matched Pair Analysis" Diagnostics 14, no. 14: 1478. https://doi.org/10.3390/diagnostics14141478
APA StyleJung, S.-H., Choi, C. H., Kim, S.-H., Chung, K., Moon, H.-S., Sim, W., & Jung, M. (2024). Sequential Comparison of Knee Muscle Strength after Anterior Cruciate Ligament Reconstruction between Hamstring Autograft and Tibialis Anterior Allograft: Propensity Score Matched Pair Analysis. Diagnostics, 14(14), 1478. https://doi.org/10.3390/diagnostics14141478






