AI-Enhanced Predictive Modeling for Identifying Depression and Delirium in Cardiovascular Patients Scheduled for Cardiac Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dataset
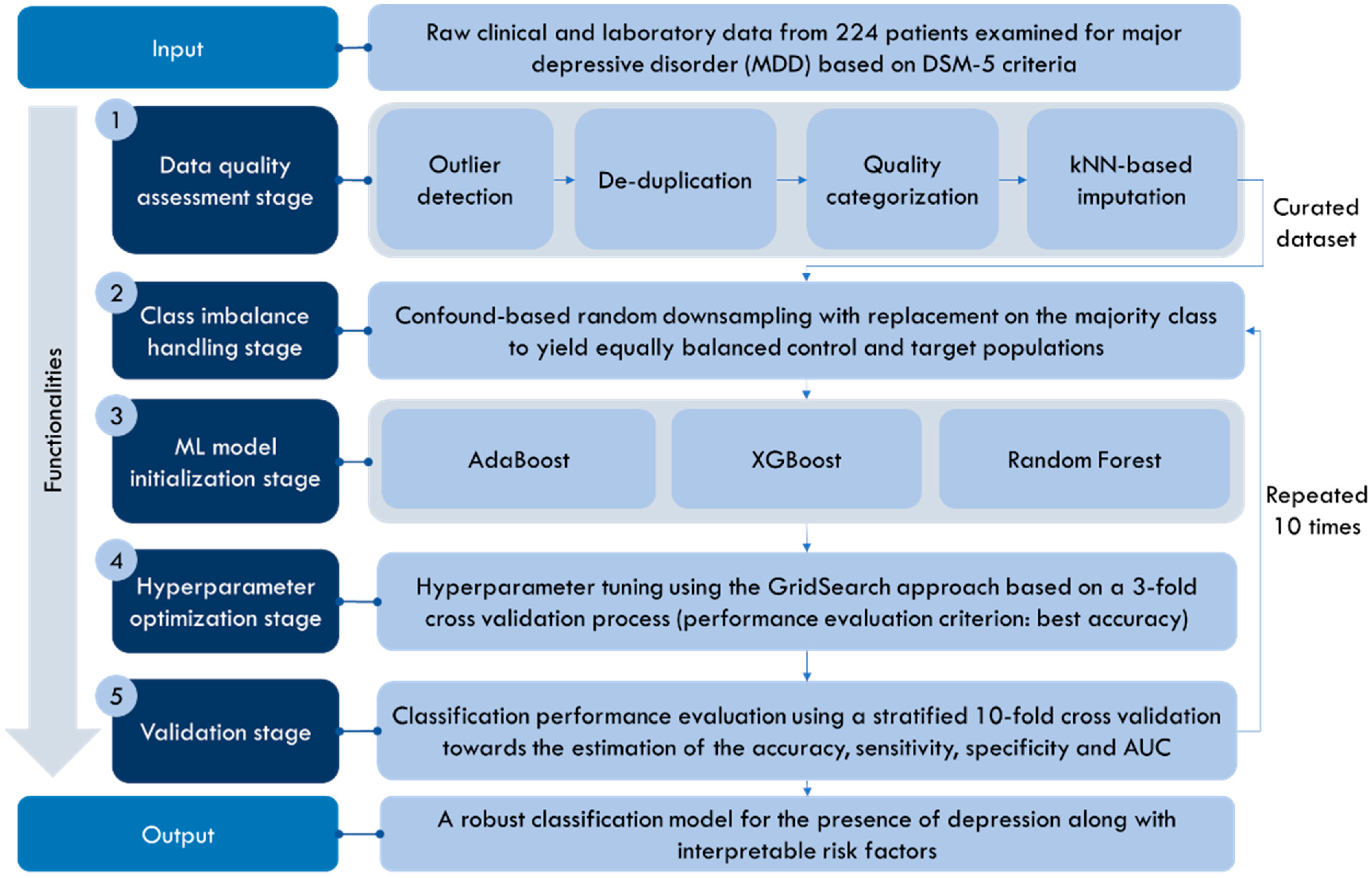
2.2. Proposed Workflow of Depression and Delirium Prediction
2.2.1. Data Quality Assessment (Data Curation) Stage
2.2.2. Class Imbalance Handling Stage
2.2.3. ML Model Initialization Stage
2.2.4. Hyperparameter Optimization Stage
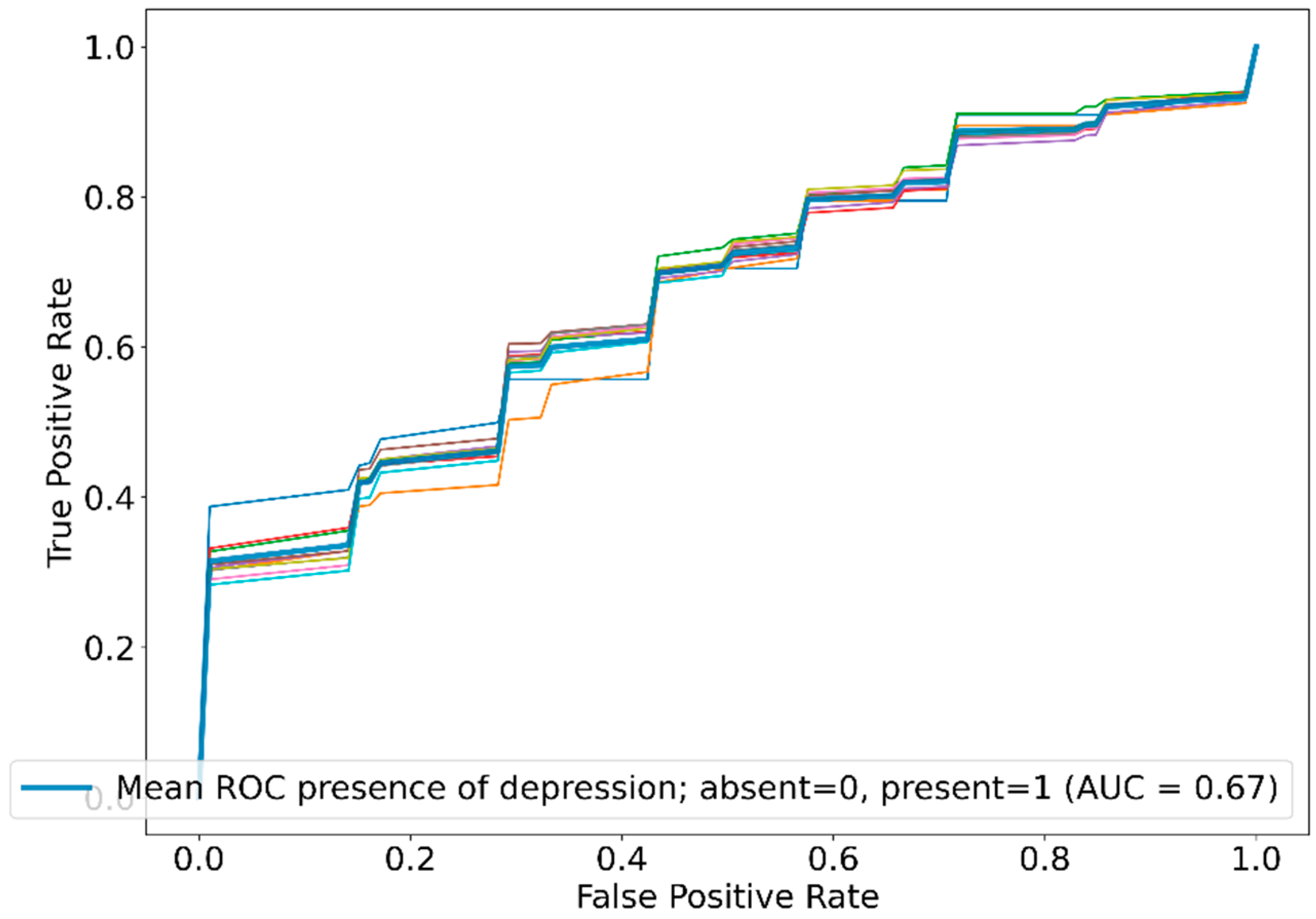
2.2.5. Validation Stage
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017, 135, e146–e603, Erratum in Circulation 2017, 136, e196. [Google Scholar] [CrossRef]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Liu, G.; Geng, Q. Associations of Cardiovascular Disease and Depression with Memory Related Disease: A Chinese National Prospective Cohort Study. J. Affect. Disord. 2020, 260, 11–17. [Google Scholar] [CrossRef]
- Graham, N.; Ward, J.; Mackay, D.; Pell, J.P.; Cavanagh, J.; Padmanabhan, S.; Smith, D.J. Impact of Major Depression on Cardiovascular Outcomes for Individuals with Hypertension: Prospective Survival Analysis in UK Biobank. BMJ Open 2019, 9, e024433. [Google Scholar] [CrossRef] [PubMed]
- Whooley, M.A.; Wong, J.M. Depression and Cardiovascular Disorders. Annu. Rev. Clin. Psychol. 2013, 9, 327–354. [Google Scholar] [CrossRef] [PubMed]
- Shao, M.; Lin, X.; Jiang, D.; Tian, H.; Xu, Y.; Wang, L.; Ji, F.; Zhou, C.; Song, X.; Zhuo, C. Depression and Cardiovascular Disease: Shared Molecular Mechanisms and Clinical Implications. Psychiatry Res. 2020, 285, 112802. [Google Scholar] [CrossRef] [PubMed]
- Bargieł, W.; Cierpiszewska, K.; Maruszczak, K.; Pakuła, A.; Szwankowska, D.; Wrzesińska, A.; Gutowski, Ł.; Formanowicz, D. Recognized and Potentially New Biomarkers-Their Role in Diagnosis and Prognosis of Cardiovascular Disease. Medicina 2021, 57, 701. [Google Scholar] [CrossRef]
- Beurel, E.; Toups, M.; Nemeroff, C.B. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron 2020, 107, 234–256. [Google Scholar] [CrossRef]
- Melin, E.O.; Dereke, J.; Hillman, M. Higher Levels of the Soluble Receptor for Advanced Glycation End Products and Lower Levels of the Extracellular Newly Identified Receptor for Advanced Glycation End Products Were Associated with Lipid-Lowering Drugs in Patients with Type 1 Diabetes: A Comparative Cross-Sectional Study. Lipids Health Dis. 2020, 19, 223. [Google Scholar] [CrossRef]
- Kaźmierski, J.; Miler, P.; Pawlak, A.; Jerczyńska, H.; Nowakowska, K.; Walkiewicz, G.; Woźniak, K.; Krejca, M.; Wilczyński, M. Increased postoperative myeloperoxidase concentration associated with low baseline antioxidant capacity as the risk factor of delirium after cardiac surgery. Ann. Med. 2022, 54, 610–616. [Google Scholar] [CrossRef]
- Russell, S.; Novig, P. Artificial Intelligence: A Modern Approach; Pearson: Harlow, UK, 2020. [Google Scholar]
- Ghaderzadeh, M. Clinical decision support system for early detection of prostate cancer from benign hyperplasia of prostate. Stud. Health Technol. Inform. 2013, 192, 928. [Google Scholar] [PubMed]
- Rezaei, T.; Jafari Khouzani, P.; Jafari Khouzani, S.; Moghadam Fard, A.; Rashidi, S.; Ghazalgoo, A.; Rezaei, M.; Farrokhi, M.; Moeini, A.; Foroutani, L.; et al. Integrating Artificial Intelligence into Telemedicine: Revolutionizing Healthcare Delivery. Kindle 2023, 3, 1–161. [Google Scholar]
- Beam, A.L.; Kohane, I.S. Big data and machine learning in health care. JAMA 2018, 319, 1317–1318. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, W.; Raghupathi, V. Big data analytics in healthcare: Promise and potential. Health Inform. Sci. Syst. 2014, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Na, K.-S.; Cho, S.-E.; Geem, Z.W.; Kim, Y.-K. Predicting Future Onset of Depression among Community Dwelling Adults in the Republic of Korea Using a Machine Learning Algorithm. Neurosci. Lett. 2020, 721, 134804. [Google Scholar] [CrossRef] [PubMed]
- Sau, A.; Bhakta, I. Predicting Anxiety and Depression in Elderly Patients Using Machine Learning Technology. Healthc. Technol. Lett. 2017, 4, 238–243. [Google Scholar] [CrossRef]
- Zulfiker, S.; Kabir, N.; Biswas, A.A.; Nazneen, T.; Uddin, M.S. An In-Depth Analysis of Machine Learning Approaches to Predict Depression. Curr. Res. Behav. Sci. 2021, 2, 100044. [Google Scholar] [CrossRef]
- Priya, A.; Garg, S.; Tigga, N.P. Predicting Anxiety, Depression and Stress in Modern Life Using Machine Learning Algorithms. Procedia Comput. Sci. 2020, 167, 1258–1267. [Google Scholar] [CrossRef]
- Sau, A.; Bhakta, I. Screening of Anxiety and Depression among Seafarers Using Machine Learning Technology. Inform. Med. Unlocked 2019, 16, 100228. [Google Scholar] [CrossRef]
- Fazel Zarandi, M.H.; Soltanzadeh, S.; Mohammadi, A.; Castillo, O. Designing a General Type-2 Fuzzy Expert System for Diagnosis of Depression. Appl. Soft Comput. 2019, 80, 329–341. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlingon, VA, USA, 2013. [Google Scholar]
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2001, 29, 1370–1379. [Google Scholar] [CrossRef]
- Kazmierski, J.; Kowman, M.; Banach, M.; Fendler, W.; Okonski, P.; Banys, A.; Jaszewski, R.; Rysz, J.; Sobow, T.; Kloszewska, I. The use of DSM-IV and ICD-10 criteria and diagnostic scales for delirium among cardiac surgery patients: Results from the IPDACS study. J. Neuropsychiatry Clin. Neurosci. 2010, 22, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Breitbart, W.; Rosenfeld, B.; Roth, A.; Smith, M.J.; Cohen, K.; Passik, S. The memorial delirium assessment scale. J. Pain Symptom Manag. 1997, 13, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Pezoulas, V.C.; Kourou, K.D.; Kalatzis, F.; Exarchos, T.P.; Venetsanopoulou, A.; Zampeli, E.; Gandolfo, S.; Skopouli, F.; De Vita, S.; Tzioufas, A.G.; et al. Medical Data Quality Assessment: On the Development of an Automated Framework for Medical Data Curation. Comput. Biol. Med. 2019, 107, 270–283. [Google Scholar] [CrossRef] [PubMed]
- Medical Data Sharing. Harmonization and Analytics—1st Edition. Available online: https://www.elsevier.com/books/medical-data-sharing-harmonization-and-analytics/pezoulas/978-0-12-816507-2 (accessed on 21 January 2021).
- Zhiguo, D.; Minrui, F. An Anomaly Detection Approach Based on Isolation Forest Algorithm for Streaming Data using Sliding Window. IFAC Proc. Vol. 2013, 46, 12–17. [Google Scholar]
- Zhang, S. Nearest Neighbor Selection for Iteratively KNN Imputation. J. Syst. Softw. 2012, 85, 2541–2552. [Google Scholar] [CrossRef]
- Schapire, R.E. Explaining AdaBoost. In Empirical Inference; Schölkopf, B., Luo, Z., Vovk, V., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 37–52. ISBN 978-3-642-41135-9. [Google Scholar]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the KDD’16: 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar] [CrossRef]
- Cutler, A.; Cutler, D.; Stevens, J. Random Forests. In Machine Learning—ML; Springer: Berlin/Heidelberg, Germany, 2011; Volume 45, pp. 157–176. ISBN 978-1-4419-9325-0. [Google Scholar]
- Bucala, R.; Cerami, A. Advanced glycosylation: Chemistry, biology, and implications for diabetes and aging. Adv. Pharmacol. 1992, 23, 1–34. [Google Scholar]
- Hudson, B.I.; Lippman, M.E. Targeting RAGE signaling in inflammatory disease. Annu. Rev. Med. 2018, 69, 349–364. [Google Scholar] [CrossRef]
- Kierdorf, K.; Fritz, G. RAGE regulation and signaling in inflammation and beyond. J. Leukoc. Biol. 2013, 94, 55–68. [Google Scholar] [CrossRef]
- Zhang, M.; Kho, A.L.; Anilkumar, N.; Chibber, R.; Pagano, P.J.; Shah, A.M.; Cave, A.C. Glycated proteins stimulate reactive oxygen species production in cardiac myocytes: Involvement of Nox 2 (gp91phox)-containing NADPH oxidase. Circulation 2006, 113, 1235–1243. [Google Scholar] [CrossRef] [PubMed]
- Persson, F.; Rossing, P.; Hovind, P. Endothelial dysfunction and inflammation predict development of diabetic nephropathy in the irbesartan in patients with type 2 diabetes and microalbuminuria (IRMA 2) study. Scand. J. Clin. Lab. Investig. 2008, 68, 731–738. [Google Scholar] [CrossRef]
- Reznikov, L.L.; Waksman, J.; Azam, T. Effect of advanced glycation end products on endotoxin-induced TNF-alpha, IL-1beta and IL-8 in human peripheral blood mononuclear cells. Clin. Nephrol. 2004, 61, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Stassen, M.; Müller, C.; Arnold, M. IL-9 and IL-13 production by activated mast cells is strongly enhanced in the presence of lipopolysaccharide: NF-kappa B is decisively involved in the expression of IL-9. J. Immunol. 2001, 166, 4391–4398. [Google Scholar] [CrossRef] [PubMed]
- Milne, G.L.; Musiek, E.S.; Morrow, J.D. F2-isoprostanes as markers of oxidative stress in vivo: An overview. Biomarkers 2005, 1, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Gracia, K.C.; Llanas-Cornejo, D.; Husi, H. CVD and Oxidative Stress. J. Clin. Med. 2017, 6, 22. [Google Scholar] [CrossRef]
- Mehta, J.L.; Saldeen, T.G.; Rand, K. Interactive role of infection, inflammation and traditional risk factors in atherosclerosis and coronary artery disease. J. Am. Coll. Cardiol. 1998, 31, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Black, C.N.; Bot, M.; Scheffer, P.G.; Cuijpers, P.; Penninx, B.W.J.H. Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology 2015, 51, 164–175. [Google Scholar] [CrossRef]
- Panth, N.; Paudel, K.R.; Parajuli, K. Reactive oxygen species: A key hallmark of cardiovascular disease. Adv. Med. 2016, 2016, 12. [Google Scholar] [CrossRef]
- Kazmierski, J.; Banys, A.; Latek, J.; Bourke, J.; Jaszewski, R. Cortisol levels and neuropsychiatric diagnosis as markers of postoperative delirium: A prospective cohort study. Crit. Care. 2013, 17, R38. [Google Scholar] [CrossRef]
- Saveanu, R.V.; Nemeroff, C.B. Etiology of depression: Genetic and environmental factors. Psychiatr. Clin. N. Am. 2012, 35, 51–71. [Google Scholar] [CrossRef] [PubMed]
- Al Rifai, M.; Schneider, A.L.; Alonso, A.; Maruthur, N.; Parrinello, C.M.; Astor, B.C.; Hoogeveen, R.C.; Soliman, E.Z.; Chen, L.Y.; Ballantyne, C.M.; et al. sRAGE, inflammation, and risk of atrial fibrillation: Results from the Atherosclerosis Risk in Communities (ARIC) Study. J. Diabetes Complicat. 2015, 29, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Feng, J.Z.; Qiu, Y.H.; Yu, F.B.; Zhang, J.Z.; Zhou, W.; Yu, F.; Wang, G.K.; An, L.N.; Ni, F.H. Activation of receptor for advanced glycation end products contributes to aortic remodeling and endothelial dysfunction in sinoaortic denervated rats. Atherosclerosis 2013, 229, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Bu, D.X.; Hudson, B.I. Vascular and inflammatory stresses mediate atherosclerosis via RAGE and its ligands in apoE-/- mice. J. Clin. Investig. 2008, 118, 183–194. [Google Scholar]
- Falcone, C.; Emanuele, E.; D’angelo, A.; Buzzi, M.P.; Belvito, C.; Cuccia, M.; Geroldi, D. Plasma Levels of Soluble Receptor for Advanced Glycation End Products and Coronary Artery Disease in Nondiabetic Men. Arter. Thromb. Vasc. Biol. 2005, 25, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Prasad, K. Low levels of serum soluble receptors for advanced glycation end products, biomarkers for disease state: Myth or reality. Int. J. Angiol. 2014, 23, 11–16. [Google Scholar] [CrossRef]
- Reichert, S.; Triebert, U.; Santos, A.N.; Hofmann, B.; Schaller, H.G.; Schlitt, A.; Schulz, S. Soluble form of receptor for advanced glycation end products and incidence of new cardiovascular events among patients with cardiovascular disease. Atherosclerosis 2017, 266, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.C.; Shiu, S.W.; Chow, W.S.; Leng, L.; Bucala, R.; Betteridge, D.J. Association between serum levels of soluble receptor for advanced glycation end products and circulating advanced glycation end products in type 2 diabetes. Diabetologia 2006, 49, 2756–2762. [Google Scholar] [CrossRef]
- Dozio, E.; Caldiroli, L.; Molinari, P.; Castellano, G.; Delfrate, N.W.; Romanelli, M.M.C.; Vettoretti, S. Accelerated AGEing: The Impact of Advanced Glycation End Products on the Prognosis of Chronic Kidney Disease. Antioxidants 2023, 12, 584. [Google Scholar] [CrossRef]
- Santilli, F.; Bucciarelli, L.; Noto, D.; Cefalù, A.B.; Davì, V.; Ferrante, E.; Pettinella, C.; Averna, M.R.; Ciabattoni, G.; Davì, G. Decreased plasma soluble RAGE in patients with hypercholesterolemia: Effects of statins. Free Radic. Biol. Med. 2007, 43, 1255–1262. [Google Scholar] [CrossRef]
- Geroldi, D.; Falcone, C.; Emanuele, E.; D’Angelo, A.; Calcagnino, M.; Buzzi, M.P.; A Scioli, G.; Fogari, R. Decreased plasma levels of soluble receptor for advanced glycation end-products in patients with essential hypertension. J. Hypertens. 2005, 23, 1725–1729. [Google Scholar] [CrossRef] [PubMed]
- Miniati, M.; Monti, S.; Basta, G.; Cocci, F.; Fornai, E.; Bottai, M. Soluble receptor for advanced glycation end products in COPD: Relationship with emphysema and chronic cor pulmonale: A case-control study. Respir. Res. 2011, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Emanuele, E.; D’Angelo, A.; Tomaino, C.; Binetti, G.; Ghidoni, R.; Politi, P.; Bernardi, L.; Maletta, R.; Bruni, A.C.; Geroldi, D. Circulating levels of soluble receptor for advanced glycation end products in Alzheimer’s disease and vascular dementia. Arch. Neurol. 2005, 62, 1734–1736. [Google Scholar] [CrossRef] [PubMed]
- Crawford, A.A.; Soderberg, S.; Kirschbaum, C.; Murphy, L.; Eliasson, M.; Ebrahim, S.; Smith, G.D.; Olsson, T.; Sattar, N.; Lawlor, D.A.; et al. Morning plasma cortisol as a cardiovascular risk factor: Findings from prospective cohort and Mendelian randomization studies. Eur. J. Endocrinol. 2019, 181, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Gehi, A.; Haas, D.; Pipkin, S.; Whooley, M.A. Depression and medication adherence in outpatients with coronary heart disease. Arch. Intern. Med. 2005, 165, 2508–2513. [Google Scholar] [CrossRef]
- Sherwood, A.; Blumenthal, J.A.; Trivedi, R.; Johnson, K.S.; O’Connor, C.M.; Adams, K.F.; Dupree, C.S.; Waugh, R.A.; Bensimhon, D.R.; Gaulden, L.; et al. Relationship of depression to death or hospitalization in patients with heart failure. Arch. Intern. Med. 2007, 167, 367–373. [Google Scholar] [CrossRef]
- Müller-Tasch, T.; Peters-Klimm, F.; Schellberg, D.; Holzapfel, N.; Barth, A.; Jünger, J.; Szecsenyi, J.; Herzog, W. Depression Is a Major Determinant of Quality of Life in Patients With Chronic Systolic Heart Failure in General Practice. J. Card. Fail. 2007, 13, 818–824. [Google Scholar] [CrossRef]
- Kazmierski, J.; Kowman, M.; Banach, M.; Fendler, W.; Okonski, P.; Banys, A.; Jaszewski, R.; Rysz, J.; Mikhailidis, D.P.; Sobow, T.; et al. Incidence and predictors of delirium after cardiac surgery: Results from The IPDACS Study. J. Psychosom. Res. 2010, 69, 179–185. [Google Scholar] [CrossRef]
- Kaźmierski, J.; Miler, P.; Pawlak, A.; Jerczyńska, H.; Woźniak, J.; Frankowska, E.; Brzezińska, A.; Woźniak, K.; Krejca, M.; Wilczyński, M. Elevated Monocyte Chemoattractant Protein-1 as the Independent Risk Factor of Delirium after Cardiac Surgery. A Prospective Cohort Study. J. Clin. Med. 2021, 10, 1587. [Google Scholar] [CrossRef]


| Characteristic | Mean or N | SD or % |
|---|---|---|
| Age (years) | 66.66 | 7.06 |
| Gender (Male) | 171 | 80% |
| Education (years) | 11.53 | 3.37 |
| Weight (kg) | 81.69 | 12.38 |
| Height (cm) | 170.22 | 8.20 |
| Presence of anxiety disorders | 14 | 7% |
| Alcohol addiction | 17 | 8% |
| Diabetes | 74 | 34% |
| Hypertension | 176 | 82% |
| Peripheral arterial disease | 31 | 14% |
| Vascular diseases of the CNS | 24 | 11% |
| Other diseases of the CNS (epilepsy or head injuries) | 8 | 4% |
| Asthma | 7 | 3% |
| Chronic obstructive pulmonary disease | 14 | 7% |
| Smoking tobacco | 94 | 44% |
| Anemia (Hb 10 mg/dL for female; 12 mg/dL for male) | 32 | 15% |
| Creatinine > 1.2 mg/dL | 31 | 14% |
| Atrial fibrillation | 28 | 13% |
| Pacemaker | 4 | 2% |
| Significant ventricular arrhythmias | 2 | 1% |
| Ejection fraction % | 51.61 | 10% |
| CCS score | 2.39 | 0.74 |
| NYHA grade | 2.17 | 0.70 |
| Clock drawing test (points) | 5.79 | 2.40 |
| Mini-Mental State Examination (points) | 27.60 | 2.10 |
| Antioxidant activity (mM) before surgery | 2.30 | 1.12 |
| Superoxide dismutase (U/mL) before surgery | 3.00 | 1.58 |
| sRAGE (ng/mL) before surgery | 1.02 | 0.74 |
| MPO (ng/mL) before surgery | 321.54 | 238.98 |
| MCP-1 (ng/mL) before surgery | 423.17 | 184.46 |
| hsCRP (ug/mL) before surgery | 10.67 | 23.14 |
| Urea (mmol/L) before surgery | 6.81 | 2.07 |
| Creatinine (mcmol/L) before surgery | 88.55 | 23.80 |
| Intraoperative circulatory support | 57 | 27% |
| Intraoperative resuscitation | 3 | 1% |
| Intraoperative steroid use | 2 | 1% |
| Postoperatively (pCO2 ≥45 mmHg) | 50 | 23% |
| Postoperatively (pO2 ≤ 60 mmHg) | 31 | 14% |
| Postoperative hyperthermia | 23 | 11% |
| Massive postoperative transfusion (>4 units) | 11 | 5% |
| Plasma transfusion (≥1 unit) | 35 | 16% |
| Reoperation | 13 | 6% |
| Urgent postoperative angioplasty | 1 | 0% |
| Length of stay in the ICU (days) | 3.71 | 2.24 |
| Hospitalization time (days) | 12.83 | 6.98 |
| ECC; in case of no (surgery OPCAB) | 165 | 77% |
| The highest MDAS score | 7.72 | 4.59 |
| Delirium diagnosis | 61 | 34% |
| Day after surgery at which delirium was diagnosed | 28 | 13% |
| Presence of depression | 34 | 16% |
| Biomarker | Correlation Coefficient | p-Value |
|---|---|---|
| MPO (ng/mL) | 0.14 | 0.29 |
| Antioxidant activity (mM) | −0.11 | 0.40 |
| Superoxide dismutase (U/mL) | −0.11 | 0.25 |
| sRAGE (ng/mL) | 0.32 | 0.04 |
| MCP-1 (ng/mL) | 0.06 | 0.62 |
| hsCRP (ug/mL) | 0.08 | 0.54 |
| Classifier | Accuracy | Sensitivity | Specificity | AUC | |
|---|---|---|---|---|---|
| Depression | RF | 0.614 | 0.701 | 0.528 | 0.671 |
| GBT | 0.565 | 0.598 | 0.532 | 0.571 | |
| XGBoost | 0.558 | 0.610 | 0.505 | 0.582 | |
| AdaBoost | 0.542 | 0.715 | 0.367 | 0.599 | |
| Delirium | GBT | 0.722 | 0.719 | 0.723 | 0.781 |
| RF | 0.709 | 0.757 | 0.657 | 0.787 | |
| XGBoost | 0.669 | 0.670 | 0.664 | 0.744 | |
| AdaBoost | 0.583 | 0.920 | 0.245 | 0.727 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowakowska, K.; Sakellarios, A.; Kaźmierski, J.; Fotiadis, D.I.; Pezoulas, V.C. AI-Enhanced Predictive Modeling for Identifying Depression and Delirium in Cardiovascular Patients Scheduled for Cardiac Surgery. Diagnostics 2024, 14, 67. https://doi.org/10.3390/diagnostics14010067
Nowakowska K, Sakellarios A, Kaźmierski J, Fotiadis DI, Pezoulas VC. AI-Enhanced Predictive Modeling for Identifying Depression and Delirium in Cardiovascular Patients Scheduled for Cardiac Surgery. Diagnostics. 2024; 14(1):67. https://doi.org/10.3390/diagnostics14010067
Chicago/Turabian StyleNowakowska, Karina, Antonis Sakellarios, Jakub Kaźmierski, Dimitrios I. Fotiadis, and Vasileios C. Pezoulas. 2024. "AI-Enhanced Predictive Modeling for Identifying Depression and Delirium in Cardiovascular Patients Scheduled for Cardiac Surgery" Diagnostics 14, no. 1: 67. https://doi.org/10.3390/diagnostics14010067
APA StyleNowakowska, K., Sakellarios, A., Kaźmierski, J., Fotiadis, D. I., & Pezoulas, V. C. (2024). AI-Enhanced Predictive Modeling for Identifying Depression and Delirium in Cardiovascular Patients Scheduled for Cardiac Surgery. Diagnostics, 14(1), 67. https://doi.org/10.3390/diagnostics14010067








